Abstract
Isolated minor non-specific ST-segment and T-wave (NSSTA), minor and major electrocardiographic (ECG) abnormalities are established, independent risk markers for incident cardiovascular events. Their association with subclinical atherosclerosis has been postulated but is not clearly defined. The aim of this study is to define the association between ECG abnormalities and measures of subclinical atherosclerosis. We studied participants from MESA, a multi-ethnic sample of men and women aged 45–84 and free of clinical cardiovascular disease at enrollment. Baseline examination included measurement of traditional risk factors, resting 12-lead electrocardiograms, coronary artery calcium (CAC) measurement and common carotid intima-media thickness (CCIMT). Electrocardiograms were coded using Novacode criteria and were defined as having either minor abnormalities (e.g., minor non-specific STTA, first degree atrioventricular block, and QRS axis deviations) or major abnormalities (e.g., pathologic Q waves, major ST-segment and T-wave abnormalities, significant dysrhythmias and conduction system delays). Multivariable logistic and linear regressions were used to determine the cross-sectional associations of ECG abnormalities with CAC and common carotid-IMT. Among 6710 participants, 52.7% were women, with a mean age of 62 years. After multivariable-adjustment, isolated minor STTA, minor and major ECG abnormalities were not associated with the presence of CAC (>0) among men (OR 1.04, 95% CI 0.81–1.33; 1.10, 0.91–1.32; and 1.03, 0.81–1.31, respectively) or women (1.01, 0.82–1.24; 1.04, 0.87–1.23; and 0.94, 0.73–1.22, respectively). Lack of association remained consistent when using both log CAC and CC-IMT as continuous variables. ECG abnormalities are not associated with markers of subclinical atherosclerosis in a large multi-ethnic cohort.
INTRODUCTION
A large number of prospective epidemiologic studies have established an association between isolated minor non-specific ST segment and T wave (NSSTTA), minor and major electrocardiographic (ECG) abnormalities and incident clinical coronary heart disease (CHD) events, independent of traditional coronary risk factors.1–6 The prevalence of minor ECG abnormalities is substantially higher than major abnormalities and increases markedly with older age.6–9 The mechanism by which minor ECG abnormalities, the majority of which are isolated non-specific STTA, increase risk is unclear. Several investigators3,10–12 have postulated that they may represent subclinical coronary atherosclerosis, but this is unconfirmed and there have been few studies to date examining this association. The MESA cohort is a large, multi-ethnic sample tracked with high quality ECG’s, as well as coronary artery calcium (CAC) and carotid intimamedia thickness (C-IMT) (two widely used measures of subclinical CVD that are known to be highly correlated with coronary atherosclerosis and prospectively associated with incident CHD events)13–17 that is ideally suited to examine the association of ECG abnormalities with subclinical atherosclerosis. Further elucidation of the association between these important ECG abnormalities and subclinical cardiac disease will help shed light on the mechanism through which they confer increased risk for CVD and CHD.
METHODS
The MESA cohort was initiated to investigate the prevalence, correlates, and progression of subclinical CVD. (i.e. disease detected by non-invasive means before it has manifested in clinical signs and symptoms). Details about the study design have previously been published.18 Briefly, between July 2000 and August 2002, 6814 men and women aged 45 to 84 years old, self-identified as white, black, Hispanic, or Chinese and free of clinically apparent CVD were recruited from portions of 6 US communities: Baltimore City and Baltimore County, Maryland; Chicago, Ill; Forsyth County, North Carolina; Los Angeles County, California; Northern Manhattan and the Bronx, New York; and St. Paul, Minn. Each field site recruited from locally available sources, which included lists of residents, lists of dwellings, and telephone exchanges. The institutional review boards at all participating centers approved the study, and all participants gave informed consent.
Participants underwent an extensive baseline evaluation, including an initial standardized questionnaire. Measurements of height, weight, body mass index, anthropometric data, and blood pressure were measured as well. Total and high-density lipoprotein cholesterol, triglycerides, and glucose levels were measured from blood samples obtained after a 12-hour fast. Low-density lipoprotein cholesterol was calculated with the Friedewald equation.19 Diabetes was defined as fasting glucose 126 mg/dL or use of hypoglycemic medication.
For electrocardiography, three 12-lead recordings are obtained using a Marquette MAC-PC instrument (Marquette Electronics, Milwaukee, Wisconsin) and read using both Minnesota Code (MC)20 and Novacode criteria (NC)21. Readings are performed centrally at the EPICARE reading center, Wake Forest University. Major ECG abnormalities were defined by the presence of 1 or more of the following findings: ventricular conduction defect (NC 3.1, 3.2 or 3.3), major Q wave (NC 5.1, 5.2, or 5.3), minor Q, QS waves with ST-T abnormalities (NC 5.4), isolated ST-T wave abnormalities (NC 5.5 or 5.6), left ventricular hypertrophy (NC 6.1.1), atrial fibrillation (NC 1.5.1, 1.5.2, or 1.5.3) or first degree atrio-ventricular block (NC 2.1). Minor ECG abnormalities were defined by the presence of 1 or more of the following findings: Minor Q, QS waves (NC 5.7), high R waves(NC 6.1.0), minor isolated ST-T abnormalities(NC 5.8), ST elevation (MC 9-2), incomplete right bundle branch block (NC 3.4.1), long QT Interval (qti1 >=110, where qti1 = qtdur1* (hr + 100) / 656), short PR segment (< 120 ms), left axis deviation (>= −90, <= −30), or right axis deviation(>=120, <=210). Isolated minor STTA (NC 5.8) were included, a priori, in a separate analysis as they represented a large percentage of the minor ECG abnormalities. Participants with major ECG abnormalities were excluded from the analyses examining minor ECG abnormalities and isolated minor STTA.
CAC was measured with either electron-beam computed tomography or multidetector computed tomography at 3 field centers and these scans were read independently at a centralized reading center. The amount of calcium was quantified with the Agatston scoring method.22 Interobserver agreement and intraobserver agreement were found to be very high (kappa =0.93 and 0.90, respectively). Coronary artery calcification was defined as being present (CAC+) if the calcium score was >0.23
Trained technicians in each field center performed B-mode ultrasonography of the right and left near and far walls of the internal carotid and common carotid arteries. An ultrasound reading center (Department of Radiology, Tufts–New England Medical Center, Boston, Massachusetts) measured maximal IMT of the common carotid artery defined as the mean of the maximal IMT of the near and far wall on both the left and right sides, and it was measured at mm proximal to the common carotid bulb.18 Internal Carotid IMT was not included in the present analysis due missing data.
All analyses were performed using SAS version 9.1 (SAS Institute, Cary, NC). Baseline characteristics were compared, after stratification by sex, between participants using chi-square tests for categorical variables and t-tests or Wilcoxon rank-sum tests for continuous variables, as appropriate. To determine the cross-sectional association of ECG abnormalities with CAC+ (defined as CAC > 0), logistic regression models were fitted with the presence of CAC as the dependent variable and the presence of ECG abnormalities as the independent variable. To analyze the presence and extent of CAC, and given the large number of zero values and highly skewed distribution, we used mixed models to analyze CAC presence and ln (CAC + 1). For the association of ECG abnormalities with common carotid IMT, we used linear regression models with mean maximal CC-IMT as the dependent variable and ECG abnormalities as the independent variables. All regression models were adjusted for age, sex, and race initially; further adjustment for demographic and clinical covariates (age, smoking status, systolic blood pressure, blood pressure med, total cholesterol, high-density lipoprotein, cholesterol med, diabetes, body mass index was performed. To test for interaction of abnormal ECGs and age, we examined both age-stratified (< 65 years vs. > 65 years) models, as well as multiplicative interaction terms in the same models. In secondary analyses we also examined sex/race-specific analyses to determine whether the pattern of associations was consistent across all sex/race groups. A p-value <0.05 was considered statistically significant.
RESULTS
The study sample consisted of 6710 subjects, of whom 52.7% were women, with a mean age of 62 years; 856 (12.8%) participants had major ECG abnormalities and were excluded from the minor ECG category leaving 5848 participants for inclusion in the minor and isolated minor NSTTA ECG analyses. Baseline characteristics of the study cohort stratified by sex are shown in Table 1.
Table 1.
Baseline Characteristics of Male and Female Participants in the Multi-Ethnic Study of Atherosclerosis (MESA)
| Variable | Men (N=3171) |
Women (N=3539) |
|---|---|---|
| Age (years) | 62.2 ± 10.2 | 62.1 ± 10.3 |
| Systolic Blood Pressure (mm Hg) | 126.0 ± 19.3 | 127.1 ±23.2 |
| Total Cholesterol (mg/dl) | 188.1 ± 34.9 | 199.5 ± 35.6 |
| High-density Lipoprotein Cholesterol (mg/dl) |
45.0 ± 11.8 | 56.2 ± 15.3 |
| Triglycerides (mg/dl) | 135.5 ± 95.6 | 128.3 ± 82.5 |
| Creatinine (mg/dl) | 1.07 ± 0.32 | 0.85 ± 0.20 |
| Lipid-Lowering Medication | 16.2 % | 16.1 % |
| Current Smoker | 14.5 % | 11.7 % |
| Hypertension* | 42.9 % | 46.7 % |
| Antihypertensive therapy | 30.8 % | 35.3 % |
| Diabetes Mellitus† | 14.1 % | 11.4 % |
| Family History of Heart Attack | 39.2 % | 45.9 % |
| Body mass index (kg/m2) | 27.9 ± 4.4 | 28.7 ± 6.2 |
Hypertension defined per JNC-VII criteria(SBP ≥140, DBP ≥90 or being treated)
Defined according to American Diabetes Association guidelines based on fasting glucose > 126 mg/dL or use of hypoglycemic medication
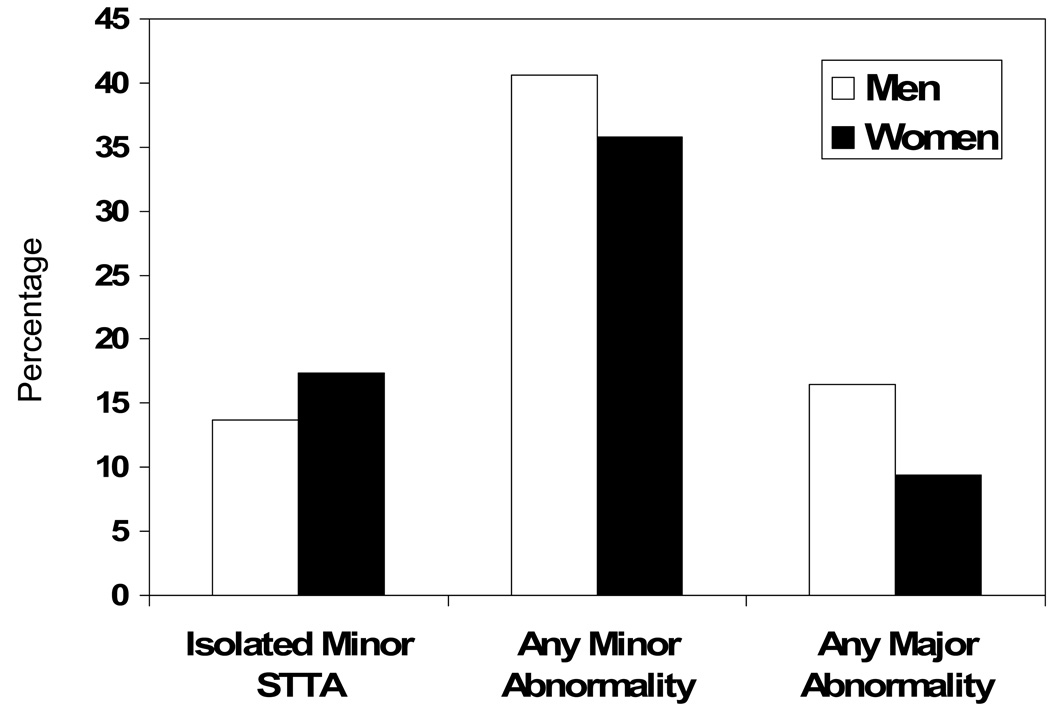
Table 2 displays the proportion of participants, stratified by sex, across the three measures of subclinical atherosclerosis; CAC > 0, Log CAC if CAC > 0, and common carotid-IMT. Figure 1 displays the proportion of participants, stratified by sex, across ECG abnormalities (isolated minor STTA, minor and major). The prevalence of ECG abnormalities and burden of subclinical athersclerosis differed significantly between men and women.
Table 2.
Levels of Coronary Artery Calcium and Common Carotid Intima-Media Thickness by sex in the Multi-Ethnic Study of Atherosclerosis (N=6710)
| MEN(n=3171) | WOMEN(n=3539) | p-value | |
|---|---|---|---|
| Common Carotid IMT, mm | 0.89 ± 0.20 | 0.85 ± 0.18 | <0.001 |
| Coronary Artery Calcium >0 | 61.2 % | 39.9 % | <0.001 |
| Median CAC, if CAC > 0 | 111.6 | 60.5 | <0.001 |
Figure 1.
Prevalence of selected ECG abnormalities by sex in MESA (n=6710).
As shown in Table 3, isolated minor STTA, minor and major ECG abnormalities were not significantly associated with CAC presence or extent in the entire cohort after multivariable adjustment. There was no evidence for interaction between ECG abnormalities and age. In secondary analyses we examined these associations within individual sex-race subgroups. These findings were also consistent across all sex and race strata, with the exception of Chinese and Hispanic men, even after adjustment for multiple potential confounders. Among Chinese men, minor ECG abnormalities were significantly associated with the presence of CAC in both age-adjusted and multivariable adjusted models. Isolated NSSTTA and major ECG abnormalities in Chinese men were associated with CAC+ in age-adjusted models, with borderline significance after multivariable adjustment. Among Hispanic men, there was an association between major ECG abnormalities and the extent of CAC after log transformation in both age-adjusted and multivariable-adjusted analyses.
Table 3.
Age-adjusted and multivariable-adjusted association of electrocardiographic abnormalities with Coronary Artery Calcium and Common Carotid Intima-Media Thickness
| Age-Adjusted | Multivariable-Adjusted | ||||||
|---|---|---|---|---|---|---|---|
| CAC > 0 | N | Odds Ratio | Confidence Interval |
P- value |
Odds Ratio | Confidence Interval |
p- value |
| MEN | |||||||
| Isolated Minor NSTTA | 2647 | 1.18 | 0.93–1.50 | 0.18 | 1.04 | 0.81–1.33 | 0.78 |
| Any Minor ECG abnormality | 2647 | 1.21 | 1.01–1.44 | 0.04 | 1.10 | 0.91–1.32 | 0.33 |
| Any Major ECG abnormality | 3171 | 1.12 | 0.92–1.45 | 0.23 | 1.03 | 0.81–1.31 | 0.79 |
| WOMEN | |||||||
| Isolated Minor NSTTA | 3207 | 1.09 | 0.89–1.33 | 0.42 | 1.01 | 0.82–1.24 | 0.92 |
| Any Minor ECG abnormality | 3207 | 1.16 | 0.98–1.37 | 0.08 | 1.04 | 0.87–1.23 | 0.67 |
| Any Major ECG abnormality | 3539 | 1.07 | 0.83–1.38 | 0.58 | 0.94 | 0.73–1.22 | 0.64 |
| Log CAC |
Parameter estimate |
Confidence Interval |
p- value |
Parameter Estimate |
Confidence Interval |
p- value |
|
| MEN | |||||||
| Isolated Minor NSTTA | 1564 | −0.10 | −0.33–0.13 | 0.39 | −0.15 | −0.38–0.08 | 0.20 |
| Any Minor ECG abnormality | 1564 | 0.12 | −0.06–0.29 | 0.19 | 0.05 | −0.12–0.23 | 0.55 |
| Any Major ECG abnormality | 1940 | 0.17 | −0.03–0.36 | 0.10 | 0.08 | −0.12–0.27 | 0.44 |
| WOMEN | |||||||
| Isolated Minor NSTTA | 1235 | −0.01 | −0.23–0.21 | 0.94 | −0.07 | −0.29–0.16 | 0.55 |
| Any Minor ECG abnormality | 1235 | 0.06 | −0.13–0.25 | 0.53 | −0.01 | −0.20–0.18 | 0.89 |
| Any Major ECG abnormality | 1411 | 0.18 | −0.08–0.44 | 1.8 | 0.12 | −0.14–0.38 | 0.38 |
| CC-IMT(mm) |
Parameter Estimate |
Confidence Interval |
p- value |
Parameter estimate |
Confidence Interval |
p- value |
|
| MEN | |||||||
| Isolated Minor NSTTA | 2647 | 0.011 | −0.008–0.03 | 0.26 | −0.007 | −0.02–0.01 | 0.44 |
| Any Minor ECG abnormality | 2647 | 0.028 | 0.014–0.042 | 0.0001 | 0.015 | 0.001–0.029 | 0.03 |
| Any Major ECG abnormality | 3171 | 0.006 | −0.1–0.02 | 0.49 | −0.008 | −0.25–0.009 | 0.36 |
| WOMEN | |||||||
| Isolated Minor NSSTTA | 3207 | 0.006 | −0.009–0.02 | 0.45 | −0.004 | −0.018–0.01 | 0.60 |
| Any Minor ECG abnormality | 3207 | 0.008 | −0.004–0.019 | 0.21 | −0.003 | −0.014–0.009 | 0.063 |
| Any Major ECG abnormality | 3539 | 0.02 | 0.001–0.39 | 0.03 | 0.008 | −0.01–0.03 | 0.40 |
All regression models were adjusted for age, sex, and race initially; further adjustment for demographic and clinical covariates (age, smoking status, systolic blood pressure (SBP), blood pressure (BP) med, total cholesterol (TC), high-density lipoprotein (HDL), cholesterol med, diabetes (DM), body mass index (BMI)) was performed. ECG = electrocardiographic, CAC = coronary artery calcium, CC-IMT = common carotid intima-media thickness NSSTTA = non-specific ST segment and T wave abnormalities
As shown in Table 3, isolated minor STTA, minor and major ECG abnormalities were not significantly associated with CC-IMT, with the exception of minor ECG abnormalities among men. This relationship was significantly attenuated, however, after adjustment for multiple confounders. There was no evidence for interaction between ECG abnormalities and age. In secondary analyses we examined these associations within individual sex-race subgroups. As demonstrated in the secondary CAC analyses, there was no significant association in any of the sex and race strata except for Chinese men. Among Chinese men with minor ECG abnormalities there was a significant association with extent of CC-IMT, even after adjustment for confounders.
DISCUSSION
In this cross-sectional analysis of a large, multi-ethnic sample composed of men and women aged 45–84, isolated minor NSSTA, minor and major ECG abnormalities were not associated with the presence of subclinical atherosclerosis as indicated by the presence of CAC (Agatston score >0), the extent of CAC among those with CAC, or the amount of common carotid IMT.
The lack of association between ECG abnormalities and subclinical atherosclerosis was observed fairly consistently across all sex and ethnic subgroups, in both age and multivariable adjusted models. Exceptions to this finding include CC-IMT among men with minor ECG abnormalities, extent of CAC among Hispanic men with major ECG abnormalities and Chinese men, among whom the presence of minor ECG changes was significantly associated with the presence of coronary calcification and degree of CC-IMT even after multivariable-adjusted models.
To our knowledge this is the largest study to examine the cross-sectional association of ECG abnormalities with subclinical atherosclerosis. Moreover, it is the first study to examine common carotid IMT, in addition to CAC, as a marker of subclinical atherosclerosis in an ECG study. Newman et al24 studied a sub-cohort of 414 individuals from the Cardiovascular Health Study who were free of clinical CVD at a mean age of 80 years. Major ECG abnormalities were not associated with the presence and extent of CAC in this sample of very old individuals subject to survival bias, with a very high prevalence of CAC despite the lack of clinical manifestations of CVD. Mohlencamp et al25 examined the association of multiple different automated ECG abnormalities (eg. left ventricular hypertrophy, T wave abnormality and major ECG findings) with CAC in an all white population of 4814 subjects aged 45–75 stratified by presence and absence of CVD. Among those patients without established CVD, only left ventricular hypertrophy (p=.025) remained significantly associated with CAC after multivariable analyses. This study however, was conducted in an all white cohort with automated ECG’s (as opposed to Minnesota or Novacoding) and its results cannot be generalized widely. Thus, previous studies suggest that ECG abnormalities have no association with CAC but have been hindered by smaller study samples and lack of age and ethnic diversity. Our study benefited from the large, multi-ethnic group of middle-age and older men and women participants of MESA with standardized ECG analyses and multiple high quality measures of subclinical atherosclerosis that make this cohort uniquely suited to examine the cross-sectional association of ECG changes with markers of subclinical atherosclerosis.
Given the consistent lack of association between ECG abnormalities and subclinical atherosclerosis across all age and race subgroups (with the exceptions noted above) and after multivariable adjustment models within this cohort, we believe subclinical atherosclerosis is less likely to be the underlying mechanism for these ECG abnormalities. We recently reported that26 the presence of isolated NSSTA in an older population from the Cardiovascular Health Study more than doubled the risk for CHD death (primarily as a result of increased arrhythmic death) in models adjusting for clinical covariates, the presence of subclinical disease and left ventricular mass index. These findings, when taken together with our conclusions, suggest that isolated minor NSSTA as well as minor ECG changes may be more associated with primary arrhythmic death as opposed to ischemic death. Given the cross-sectional nature of our observations, however, we believe further longitudinal investigation is warranted into subclinical atherosclerosis as well as alternative hypotheses (eg. left ventricular mass/hypertrophy, arrythmogenic substrates, and autonomic dysfunction) to explain the origins of these ECG abnormalities. We believe a more thorough understanding of the mechanisms through which these ECG changes are associated with clinical outcomes may allow clinicians and patients to focus preventive efforts and treatment strategies.
The mechanism underlying the observed association between ECG abnormalities and presence of subclinical atherosclerosis in isolated sex and race subgroups is unclear at present. Data are sparse regarding the prevalence and prognosis of ECG abnormalities in these populations. It is known that among non-white ethnicities there is a lower rate of CAC progression over time.27 Chinese men and women, however, tend to have both a lower rate of incident CAC+ as well as CAC progression27,28 over time, as compared with white men and women. Despite the lower rate of progression among non-white ethnicities, presence of CAC remains a significant predictor of incident clinical CHD events in all sex and race subgroups14. Postulated mechanisms for this ethnic disparity in the association between ECG abnormalities and subclinical atherosclerosis in our study include unmeasured confounders or mediators specific to the sex-race subgroup, sampling bias in the recruitment process or simply chance. Further investigation into the prevalence, prognosis and mechanisms of ECG abnormalities in sex-race specific subgroups is warranted.
Potential limitations of this study include problems inherent to CAC and carotid-IMT as surrogates for atherosclerosis. Even though coronary calcification is a well-documented tool for assessing subclinical atherosclerosis and correlates well with the degree of plaque burden, it is only a surrogate and is not currently the gold standard for assessment of atherosclerosis. Moreover, in the future, dichotomous cutpoints for assessment of the presence and extent of CAC will likely be replaced by age-specific cutpoints, such as the 90th percentile for age and sex, and Agatston scoring will likely be replaced by calcium mass, but the current study represents the state of the art. Carotid-IMT, which has also been shown to be a powerful marker of subclinical atherosclerosis and predictive of incident coronary events,13,15,17 was recently shown to be inferior to CAC as a predictor of subsequent CHD events.29 However, the additive utility of CC-IMT to CAC as a predictor of subclinical atherosclerosis and CHD risk has never been examined. Major and minor ECG changes make up a relatively heterogeneous group of abnormalities and specific abnormalities (eg. major STTA, minor NSTTA) may be more directly related to subclinical atherosclerosis. In secondary analyses, however, we examined multiple specific ECG abnormalities within the major and minor classification and found no significant association with both CAC and CC-IMT. Finally, the cross-sectional nature of the analyses precludes determination of the direction of association between these ECG abnormalities and subclinical atherosclerosis. Nevertheless, the clinical applications of this study are still valid as the everyday clinician is more concerned with the potential cross-sectional association between these easily identifiable ECG abnormalities and the presence of subclinical atherosclerosis, as opposed to their longitudinal association over time.
ACKNOWLEDGEMENTS
This research was supported by contracts N01-HC-95159 through N01-HC-95165 and N01-HC-95169 from the National Heart, Lung, and Blood Institute. The authors thank the other investigators, the staff, and the participants of the MESA study for their valuable contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONFLICTS OF INTEREST: none
References
- 1.The pooling project research group. Relationship of blood pressure, serum cholesterol, smoking habit, relative weight and ECG abnormalities to incidence of major coronary events: final report of the pooling project. J Chronic Dis. 1978;31:201–306. doi: 10.1016/0021-9681(78)90073-5. [DOI] [PubMed] [Google Scholar]
- 2.Daviglus ML, Liao Y, Greenland P, Dyer AR, Liu K, Xie X, Huang CF, Prineas RJ, Stamler J. Association of nonspecific minor ST-T abnormalities with cardiovascular mortality: the Chicago Western Electric Study. JAMA. 1999;281:530–536. doi: 10.1001/jama.281.6.530. [DOI] [PubMed] [Google Scholar]
- 3.Dekker JM, Schouten EG, Klootwijk P, Pool J, Kromhout D. ST Segment and T Wave Characteristics as Indicators of Coronary Heart Disease Risk: The Zutphen Study. J Am Coll Cardiol. 1995;25:1321–1322. doi: 10.1016/0735-1097(95)00017-X. [DOI] [PubMed] [Google Scholar]
- 4.Kannel WB. Common electrocardiographic markers for subsequent clinical coronary events. Circulation. 1987;75:II25–II127. [PubMed] [Google Scholar]
- 5.Liao Y, Liu K, Dyer AR, Schoenberger JA, Shekelle RB, Colette P, Stamler J. Major and minor electrocardiographic abnormalities and risk of death from coronary heart disease, cardiovascular diseases and all causes in men and women. J Am Coll Cardiol. 1988;12:1494–1500. doi: 10.1016/s0735-1097(88)80016-0. [DOI] [PubMed] [Google Scholar]
- 6.Sutherland SE, Gazes PC, Keil JE, Gilbert GE, Knapp RG. Electrocardiographic abnormalities and 30-year mortality among white and black men of the Charleston Heart Study. Circulation. 1993;88:2685–2692. doi: 10.1161/01.cir.88.6.2685. [DOI] [PubMed] [Google Scholar]
- 7.Vitelli LL, Crow RS, Shahar E, Hutchinson RG, Rautaharju PM, Folsom AR. Electrocardiographic findings in a healthy biracial population. Atherosclerosis Risk in Communities (ARIC) Study Investigators. Am J of Cardiol. 1998;81:453–459. doi: 10.1016/s0002-9149(97)00937-5. [DOI] [PubMed] [Google Scholar]
- 8.De Bacquer D, De Backer G, Kornitzer M. Prevalences of ECG findings in large population based samples of men and women. Heart (British Cardiac Society) 2000;84:625–633. doi: 10.1136/heart.84.6.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The West of Scotland Coronary Prevention Study Group. Baseline risk factors and their association with outcome in the West of Scotland Coronary Prevention Study. Am J Cardiol. 1997;79:756–762. doi: 10.1016/s0002-9149(96)00863-6. [DOI] [PubMed] [Google Scholar]
- 10.Kannel WB, Anderson K, McGee DL, Degatano LS, Stampfer MJ. Nonspecific electrocardiographic abnormality as a predictor of coronary heart disease: the Framingham Study. Am Heart J. 1987;113:370–376. doi: 10.1016/0002-8703(87)90280-8. [DOI] [PubMed] [Google Scholar]
- 11.Kumar A, Lloyd-Jones DM. Clinical significance of minor nonspecific ST-segment and T-wave abnormalities in asymptomatic subjects: a systematic review. Cardiol Rev. 2007;15:133–142. doi: 10.1097/01.crd.0000249382.65955.14. [DOI] [PubMed] [Google Scholar]
- 12.Short D. Clinical significance of minor ST-T depression in resting electrocardiogram. Br Heart J. 1972;34:377–382. doi: 10.1136/hrt.34.4.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chambless LE, Folsom AR, Davis V, Sharrett R, Heiss G, Sorlie P, Szklo M, Howard G, Evans GW. Risk factors for progression of common carotid atherosclerosis: the Atherosclerosis Risk in Communities Study, 1987–1998. Am J Epidemiol. 2002;155:38–47. doi: 10.1093/aje/155.1.38. [DOI] [PubMed] [Google Scholar]
- 14.Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, Liu K, Shea S, Szklo M, Bluemke DA, O'Leary DH, Tracy R, Watson K, Wong ND, Kronmal RA. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358:1336–1345. doi: 10.1056/NEJMoa072100. [DOI] [PubMed] [Google Scholar]
- 15.Hodis HN, Mack WJ, LaBree L, Selzer RH, Liu CR, Liu CH, Azen SP. The role of carotid arterial intima-media thickness in predicting clinical coronary events. Ann Intern Med. 1998;128:262–269. doi: 10.7326/0003-4819-128-4-199802150-00002. [DOI] [PubMed] [Google Scholar]
- 16.Kondos GT, Hoff JA, Sevrukov A, et al. Electron-beam tomography coronary artery calcium and cardiac events. Circulation. 2003;107:2571–2576. doi: 10.1161/01.CIR.0000068341.61180.55. [DOI] [PubMed] [Google Scholar]
- 17.O'Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK, Jr. Cardiovascular Health Study Collaborative Research Group. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. N Engl J Med. 1999;340:14–22. doi: 10.1056/NEJM199901073400103. [DOI] [PubMed] [Google Scholar]
- 18.Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, Greenland P, Jacob DR, Jr., Kronmal R, Liu K, Nelson JC, O'Leary D, Saad MF, Shea S, Szklo M, Tracy RP. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 19.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 20.Prineas RJCR, Blackburn H. The Minnesota Code Manual of Electrocardiographic Findings: Standards and Procedures for Measurement and Classification. Boston, MA: John Wright - PSG, Inc.; 1982. [Google Scholar]
- 21.Rautaharju PM, Park LP, Chaitman BR, Rautaharju F, Zhang ZM. The Novacode criteria for classification of ECG abnormalities and their clinically significant progression and regression. J Electrocardiol. 1998;31:157–187. [PubMed] [Google Scholar]
- 22.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–832. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 23.Bild DE, Detrano R, Peterson D, Guerci A, Liu K, Shahar E, Ouyang P, Jackson S, Saad MF. Ethnic differences in coronary calcification: the Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2005;111:1313–1320. doi: 10.1161/01.CIR.0000157730.94423.4B. [DOI] [PubMed] [Google Scholar]
- 24.Newman AB, Naydeck BL, Sutton-Tyrrell K, Edmundowicz D, O'Leary D, Kronmal R, Burke GL, Kuller LH. Relationship between coronary artery calcification and other measures of subclinical cardiovascular disease in older adults. Arterioscler Thromb Vasc Biol. 2002;22:1674–1679. doi: 10.1161/01.atv.0000033540.89672.24. [DOI] [PubMed] [Google Scholar]
- 25.Mohlenkamp S. Subclinical coronary atherosclerosis and resting ECG abnormalities in an unselected general populaiton. Atherosclerosis. 2008;196:786–794. doi: 10.1016/j.atherosclerosis.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 26.Kumar A, Prineas RJ, Arnold AM, Psaty BM, Furberg CD, Robbins J, Lloyd-Jones DM. Prevalence, prognosis, and implications of isolated minor nonspecific ST-segment and T-wave abnormalities in older adults: Cardiovascular Health Study. Circulation. 2008;118:2790–2796. doi: 10.1161/CIRCULATIONAHA.108.772541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kronmal RA, McClelland RL, Detrano R, Shea S, Lima JA, Cushman M, Bild DE, Burke GL. Risk factors for the progression of coronary artery calcification in asymptomatic subjects: results from the Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2007;115:2722–2730. doi: 10.1161/CIRCULATIONAHA.106.674143. [DOI] [PubMed] [Google Scholar]
- 28.McClelland RL, Chung H, Detrano R, Post W, Kronmal RA. Distribution of coronary artery calcium by race, gender, and age: results from the Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2006;113:30–37. doi: 10.1161/CIRCULATIONAHA.105.580696. [DOI] [PubMed] [Google Scholar]
- 29.Folsom AR, Kronmal RA, Detrano RC, O'Leary DH, Bild DE, Bluemke DA, Budoff MJ, Liu K, Shea S, Szklo M, Tracy RP, Watson KE, Burke GL. Coronary artery calcification compared with carotid intima-media thickness in the prediction of cardiovascular disease incidence: the Multi-Ethnic Study of Atherosclerosis (MESA) Arch Intern Med. 2008;168:1333–1339. doi: 10.1001/archinte.168.12.1333. [DOI] [PMC free article] [PubMed] [Google Scholar]