Cryptococcosis is now the commonest cause of adult meningitis in much of Southern and East Africa [1]. Despite currently available antifungal therapies, acute mortality ranges from 30 to over 50% in published series [2, 3]. The result is that cryptococcal infection accounts for 10-20 % of mortality in HIV-infected cohorts from Sub Saharan Africa [1], and recently published estimates by Park et al (AIDS 20th February 2009, issue 23, 525-30) place the overall toll at an estimated 504,000 deaths in sub-saharan Africa annually [4].
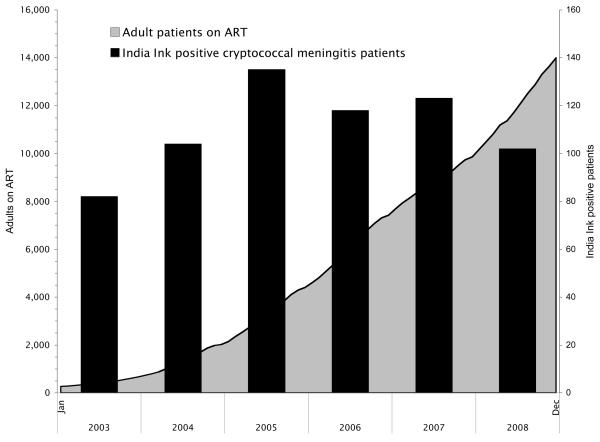
As part of an ongoing programme of work aimed at improving management of cryptococcal meningitis, we have prospectively monitored the number of new India Ink positive cases of cryptococcal meningitis diagnosed at GF Jooste Hospital, Cape Town, South Africa, for the last 6 years (2003-8). This is a public sector adult hospital serving a population of 1.3 million (including a large part of Khayelitsha township, population 500,000, with HIV antenatal seroprevalence of 32.7% in 2006 [5]). During this period, the area served by the hospital, and referral patterns for patients, have not changed. Antiretroviral therapy (ART) access has been substantially increased in the public sector clinics in the hospital's referral area from 660 adult patients on ART at the end of 2003 to 13,985 by the end of 2008, based on figures from the provincial reporting system described elsewhere [6]. It is estimated that 60% of adults with new World Health Organization (WHO) stage IV HIV disease in this setting are now accessing ART [6]. But despite this increase in the proportion of eligible patients receiving ART, the absolute number of patients with advanced disease not accessing treatment has remained constant or increased in recent years, due to the evolution of the epidemic [6]. This is in keeping with our finding that there has been no reduction in the number of new India Ink positive cases of cryptococcal meningitis presenting to our hospital over this period (Figure 1).
Figure 1.
Number of adult patients on anti-retroviral therapy (ART) in the hospital referral area, and the number of patients with India Ink positive cryptococcal meningitis presenting to the hospital by year, 2003-2008.
There has been a major effort to expand access to ART throughout sub-Saharan Africa over recent years. However despite implementation of successful treatment programmes, in many settings the numbers of people progressing to advanced immunosuppression exceeds the capacity of ART programmes, and large numbers patients presenting to health services with advanced HIV and opportunistic infections die without accessing ART. The result is that the “treatment gap” is not narrowed, and AIDS-related illness such as cryptococcal meningitis and the associated mortality are not reduced.
This is illustrated by the fact that, in the Western Cape Province, where GF Jooste hospital is located, the proportion of adult patients starting ART with CD4 counts below 50 cells/μl has fallen from 51.3% in 2001 to 21.5% in 2005 in line with increased access to care [6], while the absolute numbers of patients in this category has increased. Furthermore, unpublished aggregate data from the laboratory information system in the Province, further demonstrates that, irrespective of ART, the absolute numbers of all adult patients known to the health care system with CD4 counts below 100 cells/μl is increasing year-on-year (personal communication, Meg Osler, Provincial Government of Western Cape).
As these large numbers of patients with low CD4 counts not yet accessing ART remain at high risk of opportunistic infection, the burden of cryptococcal meningitis is likely to continue undiminished in many areas, despite increasing access to ART. These data reinforce the urgent need to improve the acute management of cryptococcal meningitis, and to facilitate earlier diagnosis and treatment, especially now that access to ART offers the possibility of a good long term prognosis, provided patients survive the acute cryptococcal infection [7]. This needs to be specifically addressed as an integral part of the response to the HIV epidemic in Africa, along with earlier HIV diagnosis and access to ART.
Acknowledgements
JNJ and GM are supported by the Wellcome Trust, London, UK.
Footnotes
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Jarvis JN, Harrison TS. HIV-associated cryptococcal meningitis. Aids. 2007;21:2119–2129. doi: 10.1097/QAD.0b013e3282a4a64d. [DOI] [PubMed] [Google Scholar]
- 2.Bicanic T, Meintjes G, Wood R, Hayes M, Rebe K, Bekker LG, Harrison T. Fungal burden, early fungicidal activity, and outcome in cryptococcal meningitis in antiretroviral-naive or antiretroviral-experienced patients treated with amphotericin B or fluconazole. Clin Infect Dis. 2007;45:76–80. doi: 10.1086/518607. [DOI] [PubMed] [Google Scholar]
- 3.Kambugu A, Meya DB, Rhein J, O'Brien M, Janoff EN, Ronald AR, et al. Outcomes of cryptococcal meningitis in Uganda before and after the availability of highly active antiretroviral therapy. Clin Infect Dis. 2008;46:1694–1701. doi: 10.1086/587667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Park BJ, Wannemuehler KA, Marston BJ, Govender N, Pappas PG, Chiller TM. Estimation of the current global burden of cryptococcal meningitis among persons living with HIV/AIDS. Aids. 2009;23:525–530. doi: 10.1097/QAD.0b013e328322ffac. [DOI] [PubMed] [Google Scholar]
- 5.Western Cape HIV Antenatal sero-prevalence survey in South Africa: 2007. Department of Health; South Africa: 2007. [Google Scholar]
- 6.Boulle A, Bock P, Osler M, Cohen K, Channing L, Hilderbrand K, et al. Antiretroviral therapy and early mortality in South Africa. Bull World Health Organ. 2008;86:678–687. doi: 10.2471/BLT.07.045294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bicanic T, Wood R, Meintjes G, Rebe K, Brouwer A, Loyse A, et al. High-dose amphotericin B with flucytosine for the treatment of cryptococcal meningitis in HIV-infected patients: a randomized trial. Clin Infect Dis. 2008;47:123–130. doi: 10.1086/588792. [DOI] [PubMed] [Google Scholar]