Abstract
PURPOSE
To identify whether parental history of myopia and/or parent-reported children’s visual activity levels can predict juvenile-onset myopia.
METHODS
Survey-based data from Orinda Longitudinal Study of Myopia subjects from 1989 to 2001 were used to predict future myopia. Univariate and multiple logistic regression analyses were performed, and receiver operator characteristic (ROC) curves were generated. Differences among the areas under the ROC curves were compared using the method of multiple comparison with the best.
RESULTS
Of the 514 children eligible for this analysis, 111 (21.6%) became myopic. Differences in the third grade between eventual myopes and nonmyopes were seen for the number of myopic parents (P < 0.001) and for the number of sports and outdoor activity hours per week (11.65 ± 6.97 hours for nonmyopes vs. 7.98 ± 6.54 hours for future myopes, P < 0.001). Analysis of the areas under the ROC curves showed three variables with a predictive value better than chance: the number of myopic parents, the number of sports and outdoor activity hours per week, and the number of reading hours per week. After controlling for sports and outdoor hours per week and parental myopia history, reading hours per week was no longer a statistically significant factor. The area under the curve for the parental myopia history and sports and outdoor activities model was 0.73. A significant interaction in the logistic model showed a differential effect of sport and outdoor activity hours per week based on a child’s number of myopic parents.
CONCLUSIONS
Parental history of myopia was an important predictor in univariate and multivariate models, with a differential effect of sports and outdoor activity hours per week based on the number of myopic parents. Lower amounts of sports and outdoor activity increased the odds of becoming myopic in those children with two myopic parents more than in those children with either zero or one myopic parent. The chance of becoming myopic for children with no myopic parents appears lowest in the children with the highest amount of sports and outdoor activity, compared with those with two myopic parents.
The prevalence of myopia has been estimated at roughly 25% of adults in the United States, with associated costs of examination and treatment in excess of $4.6 billion.1,2 These prevalence estimates are now dated and may not in fact reflect the actual prevalence among American children currently. For example, a report from Beaver Dam on longitudinal refractive error changes over a 10-year period showed an increase in the prevalence of myopia among more recent birth cohorts.3 The prevalence of myopia is higher in East Asia, particularly as reported for Singapore, Taiwan, and Hong Kong.4–7 Considering myopia’s high prevalence and costs, being able to slow or stop myopia progression and ultimately prevent the occurrence of myopia is important.
Studies focusing on reducing the progression of myopia have had limited success. Trials using progressive addition lenses,8 bifocals,9 and rigid gas permeable contact lenses10 found small, statistically significant reductions in myopic progression when compared to relevant control groups.
Pharmacologic agents are an alternative treatment. Atropine has been one of the primary pharmacologic treatments for slowing the progression of myopia. Although 1% atropine appears to be the most effective in slowing progression, with smaller effects seen with decreasing concentrations of atropine,11,12 the side effects may make its widespread use problematic. For instance, photophobia complaints remained high (22%) in the 0.5% atropine group at 3 months in a study by Shih et al.12 Recent papers from the United States and East Asia showed that the use of pirenzepine slows the progression of myopia approximately 50% over a 1-year period in the United States (reduced myopia progression by approximately 0.25 D compared with the control group) and by 50% in East Asia in the group using pirenzepine twice daily compared with the control group.13,14 These results indicate the same, weak effect for myopia reduction as that produced by 0.25% and 0.1% atropine. Optimally, a treatment that could prevent myopia will be given to individuals at greatest risk of becoming myopic. To do so, it is necessary to identify those factors that differentiate the premyopic child from the rest.
Studies evaluating the association between myopia and near work produce inconsistent results with regard to the impact of near work. Results have also been inconsistent depending on the near work measurement method. For example, Saw et al.15 found no significant association between myopia and near work, as measured by the number of hours of reading per week, unless the subjects were divided into groups of high myopes, low myopes, and nonmyopes, whereas the number of books read per week was significantly associated with being myopic. Angle and Wissmann16 found that near work accounted for a statistically significant amount of the variance in a regression model of refractive error, but the correlation was extremely low (r2 = 0.07). In a previous cross-sectional analysis of a subset of our cohort, near work was associated with children’s myopia, even after adjustment for parental history of myopia and school achievement.17
Goss18 postulated that one potential cause of myopia development in relation to near work was hyperopic defocus from poor accommodation (i.e., a high lag of accommodation). There is conflicting evidence for this idea. The theory has been tested by the COMET (Correction of Myopia Evaluation Trial)8 and Fulk et al.9 using bifocal progressive lenses to slow the progression of myopia. As noted earlier, the effect in these trials was modest and seemed to be driven by the larger treatment effect in the high lagging, esophoric myopes. In a recent paper, Mutti et al.19 evaluated accommodative lag before and after the onset of myopia and found that for a 4 D Badal accommodative stimulus, no significant increases in lag were seen before the onset of myopia or in the year of onset. Significant increases were only seen after myopia onset. This is in contrast to results presented by Gwiazda et al.20 who found that accommodative lag was elevated in children who became myopic 2 years, but not 1 year, before onset compared with emmetropes. These results suggest that accommodative lag may not be predictive of the onset of myopia, though recent work shows that there may be an association between accommodative factors and myopia progression.21
In our first paper looking at the ocular components and their ability to predict myopia in the Orinda Longitudinal Study of Myopia, we determined that the third grade sphere component of the cycloplegic refractive error had 86.7% sensitivity and 73.3% specificity for the identification of myopia when a cutoff of +0.75 D in the third-grade was used.22 We expanded on this single variable prediction to create a model using sphere, axial length, and corneal power to calculate the probability of becoming myopic. Factors beyond the physical characteristics of the eyes, in particular parental history of myopia and the amount of near work, may extend this predictive model. The purpose of this study was to determine the ability of nonocular variables to predict future myopia, specifically self-reported parental history of myopia and parental report of children’s time participating in near work and physical activities outside of school.
METHODS
Data are drawn from the Orinda Longitudinal Study of Myopia, a cohort study of school-aged children recruited at selected ages and seen annually during school grades 1 through 8. Parents and children were provided an explanation of the study, and the parents gave consent for their children’s participation. The study adhered to the tenets of the Declaration of Helsinki, and the study protocol was approved by the University of California, Berkeley’s Committee for the Protection of Human Subjects. The children were observed for a variable number of years, depending on their age at entry into the study. The children included in this analysis were third-grade subjects examined between 1989 and 2001 and found to be nonmyopic in the right eye in the third grade. Myopia was defined as at least −0.75 D of myopia in both the horizontal and vertical meridians on cycloplegic autorefraction. Corneal anesthesia was used to minimize the discomfort from the cycloplegic drops. One drop of 0.5% proparacaine was followed by 2 drops of 1% tropicamide, 5 minutes apart, for cycloplegia. Measurements were made 25 minutes after initial drop instillation.
As discussed previously,22 we found a lack of differentiation among first graders with respect to their ocular components. Third grade values allow for some differentiation, whereas the children are still young enough for the prediction of future myopia to be meaningful. To maintain consistency and allow for comparisons to the ocular component-based analysis, we present prediction of myopia based on values in subjects in the third grade. A new case was defined when a subject in fourth or subsequent grades had −0.75 D or more myopia on cycloplegic autorefraction in both meridians. This definition was chosen as −0.75 D of myopia is a clinically significant cutoff for providing a spectacle prescription, −0.75 D of myopia is likely to create symptoms of distance blur, and −0.75 D of myopia is clearly beyond the measurement error of the autorefractors used to measure refractive error.
Parents provided information through a survey on parental myopia and the number of hours per week of near work a child performed. On the baseline medical history form, one parent provided both parents’ years of birth, whether they wore spectacles or contact lenses, and, if so, the age when they were first prescribed spectacles, and how they primarily used the spectacles at the time of the survey (distance, near, or both). A parent was considered myopic if he or she used the spectacles primarily for distance or for both distance and near and had first been prescribed spectacles before the age of 17 years. This cutoff had a relatively high sensitivity and specificity (76% and 74%, respectively) in a validation study conducted by Walline et al.23 Parents completed an annual survey form that asked the following question: “During the school year, how many hours per week (outside of regular school hours) would you estimate this child performs the following activities (please fill in every blank; check none, if it is ‘0’ hours per week)?” The activities listed were: “Studies or reads for school assignments; reads for fun (pleasure); watches television; uses a computer/plays video games; and engages in outdoor and/or sports activities.” Activity hours per week for these analyses were obtained from the form completed by the parent during the child’s third grade school year. A cumulative near work exposure variable of diopter-hours was calculated.17,24,25 Diopter-hours is defined as (3 × hours of reading + 3 × hours of studying + 2 × video/computer hours + hours of watching television).
Statistical Methods
The average number of hours per week spent in activities in the third grade (age, 8–9 years) was estimated for both future myopes and nonmyopes, and statistically significant mean differences between the two groups were identified through t-tests. The relationship between the number of myopic parents and the onset of myopia was assessed with a χ2 test. All near activity and parental history variables were used as predictors in univariate logistic regression to estimate the odds ratios for future myopia. The number of myopic parents was modeled as a discrete variable of no, one, or two myopic parents. Multiple logistic regressions were performed for statistically significant variables from the univariate models. Optimally, relative risk would be used to characterize the risk of myopia, but given the logistic analysis used in the study, we present odds ratios (OR) with accompanying 95% confidence intervals (CI).
Based on our prior findings and issues surrounding model assumptions, we chose logistic regression to build predictive models. The assumptions for the logistic model are met, whereas the categorical nature of the parental history variables made the other models (canonical discriminant and quadratic discriminant analysis) incompatible. As in our previous paper, we used the receiver operating characteristic (ROC) curves associated with the logistic models as measures of the models’ predictive ability. The area under an ROC curve (θ) is the probability that, for a randomly selected pair of future-myopic and remained-nonmyopic individuals, the predictive model correctly ranks the individuals in terms of their likelihood of future disease.26,27 For example, suppose that a higher score from a predictive model means that a person is more likely to become myopic. If x is the value of the predictive model for a child who remains nonmyopic and y is the value of the predictive model for a future myopic child, then the area under the ROC curve associated with the model is an estimate of the chance that x < y. If the area under the curve is 0.75—for example, then a randomly selected individual from the remained nonmyopic group has a predictive test value, x, that is smaller than the value, y, of the future myopic individual 75% of the time, on average. The area under the empiric ROC curve plot is an unbiased estimate of P(x < y), which equates to the Mann-Whitney version of the two-sample rank-sum statistic of Wilcoxon.28,29 The area under the curve is compared statistically to 0.50, which is the value representing chance discrimination between the myopic and nonmyopic individuals. Multiple comparisons with the best methods were applied based on the work of Hsu30 to compare each method of prediction with the best of the other models of prediction using the area under the curve.
RESULTS
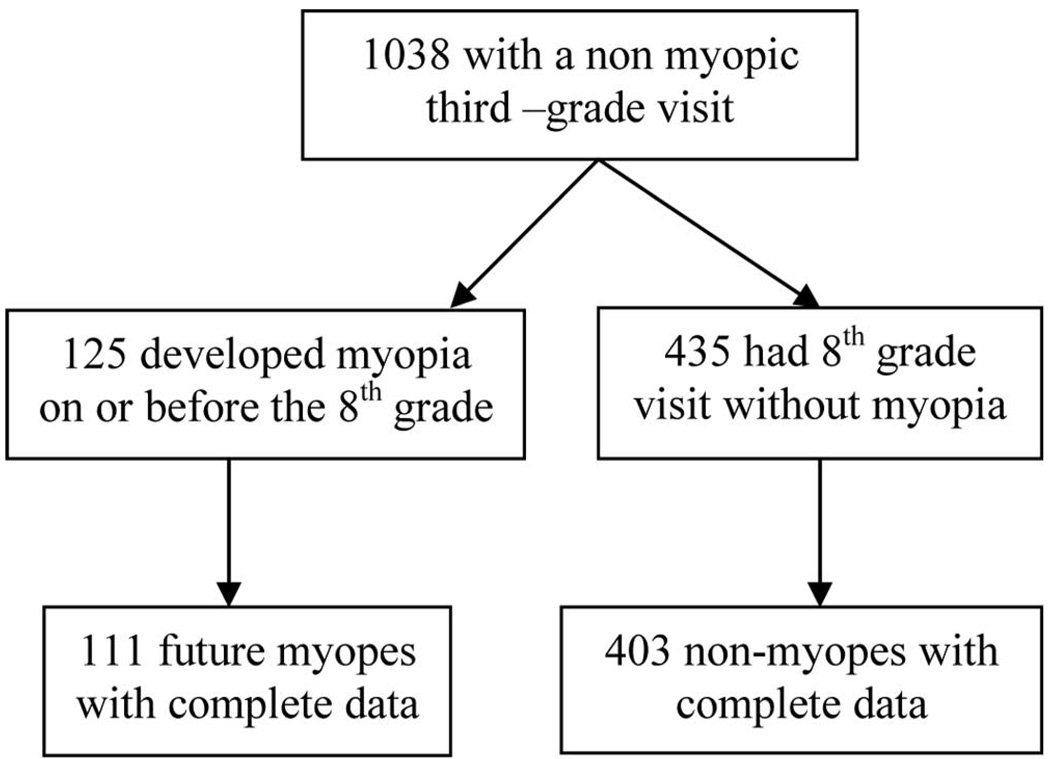
Figure 1 shows the flow diagram that resulted in the subjects who were eligible for the final analysis (i.e., those who had complete data for the variables of interest; refractive error, activity levels, and parental myopia) and sufficient follow-up. Overall, 514 subjects of 1038 with a third-grade visit (49.5%) had complete data and sufficient follow-up (i.e., either became myopic or were seen through eighth grade). The largest percentage of subjects who were excluded from the analyses did not have the opportunity for an eighth grade visit because the study closed before the subjects reached that grade (74%). Approximately 25% of the subjects without complete follow-up were in fourth grade when the study ended, approximately 25% were in the fifth grade and 25% were in the sixth grade. Half of the data among the remaining subjects lost to follow-up (23/46 subjects) was missing because of a missing activity variable.
FIGURE 1.
Description of which subjects were excluded and the reason for exclusion.
Table 1 shows a comparison of those with complete data to all those subjects with a third-grade visit who were not eligible for inclusion in the dataset because of incomplete follow-up or sufficient follow-up, but a missing variable of interest. In a comparison of parental history of myopia between these two groups, there were no statistically significant differences. Cycloplegic sphere was significantly different between the two groups, but the difference of 0.21 D is probably not clinically significant. Hours of watching television and hours of computer/video games were statistically significant, both being less than 1 hour per week different between the included subjects and those ineligible for inclusion. Hours of sports and outdoor activities were significantly different; the subjects with complete data had, on average, slightly more than 1 hour per week more of sports and outdoor activities.
TABLE 1.
Comparisons of Subjects with Complete Data and Subjects with Incomplete Data, Including Those with Insufficient Follow-up
| Not Complete |
Complete |
||||
|---|---|---|---|---|---|
| n | Mean ± SD | n | Mean ± STD | P | |
| Variable | |||||
| Cycloplegic sphere | 524 | 1.11 ± 0.62 | 514 | 0.89 ± 0.72 | <0.0001 |
| Corneal power | 523 | 43.71 ± 1.40 | 514 | 43.72 ± 1.40 | 0.88 |
| Axial length | 523 | 22.79 ± 0.66 | 514 | 22.87 ± 0.68 | 0.08 |
| Hours of reading | 481 | 3.85 ± 3.31 | 514 | 4.18 ± 3.52 | 0.14 |
| Hours of studying | 480 | 4.46 ± 2.86 | 514 | 4.51 ± 3.97 | 0.82 |
| Hours of sports/outdoor activities | 472 | 9.59 ± 7.11 | 514 | 10.86 ± 7.04 | 0.005 |
| Hours of watching TV | 478 | 7.54 ± 5.02 | 514 | 8.28 ± 5.56 | 0.03 |
| Hours of computer/video games | 467 | 3.01 ± 3.22 | 514 | 2.47 ± 2.83 | 0.005 |
| Diopter hours | 466 | 38.62 ± 18.29 | 514 | 39.28 ± 19.90 | 0.59 |
| Number of myopic parents | |||||
| Zero | 136 (50.9%) | 131 (49.1%) | 0.59 | ||
| One | 235 (48.6%) | 249 (51.4%) | |||
| Two | 116 (46.4%) | 134 (53.6%) | |||
Of the 514 eligible children, 111 (21.6%) became myopic by the eighth grade. The average age at the third-grade visit was 8.63 ± 0.39 years, and the average age at onset of myopia was 11.4 ± 1.5 years. The mean (± SD) of refractive error and activity hours in the third grade by child’s future myopia status, as well as the odds ratio, accompanying 95% confidence interval (CI), and probability are presented in Table 2. Of the activity variables, the number of hours of sports and outdoor activity per week in third grade was the only variable significantly associated with future myopia. The nonmyopic child participated in an average of 11.65 ± 6.97 hours per week of sports and outdoor activity, whereas the future myopic child participated in an average of 7.98 ± 6.54 hours per week (OR = 0.91, 95% CI = 0.87 – 0.94).
TABLE 2.
Univariate Results for Refractive Error, Activities, and Parental History for Child Myopia Status
| Variable in Third Grade | Remained Not Myopic* (n = 403) | Future Myopic* (n = 111) |
P | Odds Ratio | 95% CI |
|---|---|---|---|---|---|
| Cycloplegic sphere | 1.05 ± 0.71 | 0.32 ± 0.39 | <0.001† | 0.03 | 0.01–0.06 |
| Corneal power | 43.62 ± 1.39 | 44.09 ± 1.41 | 0.002† | 1.27 | 1.09–1.47 |
| Axial length | 22.81 ± 0.69 | 2308 ± 0.61 | <0.001† | 1.82 | 1.32–2.50 |
| Hours of sports/outdoor activity | 11.65 ± 6.97 | 7.98 ± 6.54 | <0.001† | 0.91 | 0.87–0.94 |
| Hours of reading | 4.06 ± 3.48 | 4.61 ± 3.66 | 0.14† | 1.04 | 0.99–1.10 |
| Hours of TV | 8.46 ± 5.66 | 7.63 ± 5.17 | 0.17† | 0.97 | 0.93–1.01 |
| Hours of studying | 4.56 ± 3.97 | 4.32 ± 4.00 | 0.58† | 0.98 | 0.93–1.04 |
| Hours of computer/video games | 2.45 ± 2.81 | 2.52 ± 2.92 | 0.81† | 1.01 | 0.94–1.09 |
| Diopter hours | 39.22 ± 19.67 | 39.49 ± 20.79 | 0.90† | 1.00 | 0.99–1.01 |
| Father myopic | 43.9% | 64.0% | <0.001‡ | 2.27 | 1.47–3.50 |
| Mother myopic | 47.6% | 69.4% | <0.001‡ | 2.49 | 1.59–3.90 |
| Number of myopic parents | |||||
| Zero | 29.3% | 11.7% | <0.001‡ | Reference | |
| One | 49.9% | 43.2% | <0.001‡ | 2.17 | 1.13–4.17 |
| Two | 20.8% | 45.0% | <0.001‡ | 5.40 | 2.76–10.57 |
Mean ± SD for continuous variables, percentages for categorical variables.
t-Test.
χ2 test.
Table 2 also presents parental myopia data. Among children who remained nonmyopic, approximately 48% had a myopic mother, whereas 69% of the children who became myopic had a myopic mother (P < 0.001). Similarly, among children who remained nonmyopic, 44% had a myopic father, whereas 64% of the children who become myopic had a myopic father (P < 0.001). The number of myopic parents was associated with children’s future myopia. Among children who remained nonmyopic, almost 21% had two myopic parents, whereas 45% of the future myopes had two myopic parents (P < 0.001). Compared with the reference group (children with no myopic parents), the odds ratios for future myopia were significant: 2.17 and 5.40 for children with one or two myopic parents, respectively.
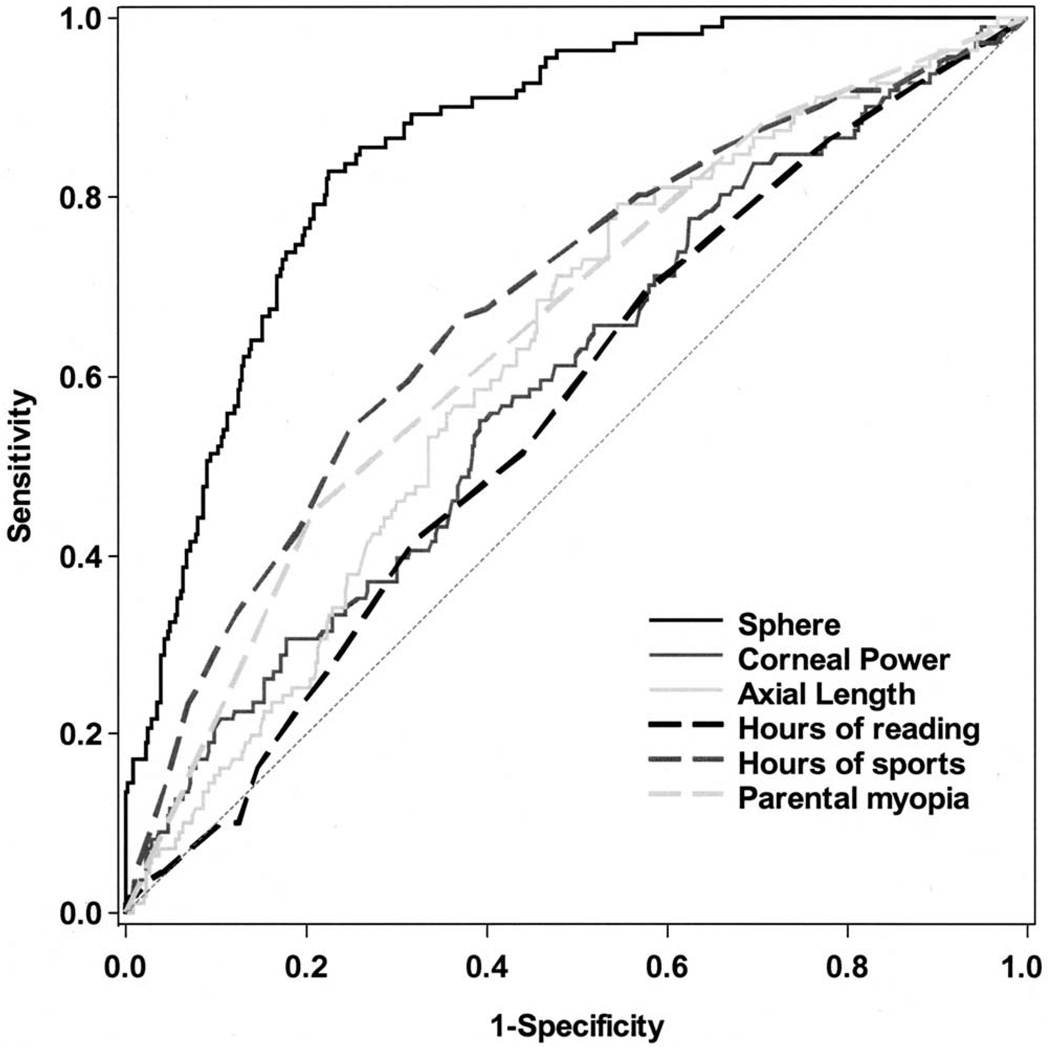
The areas under the ROC curves (AUC) associated with univariate logistic predictive models of future myopia are presented in Table 3. Variables from our previous model22 (mean sphere, axial length, and corneal power) are included, with mean sphere having the largest AUC (0.86), with number of hours per week of sports and outdoor activities and number of myopic parents being the next closest variables (0.68 and 0.66, respectively). The remainder of the activities had AUCs between 0.50 and 0.57. Of these, only hours per week spent reading had a statistically significant AUC. The confidence intervals of all the other activities’ AUCs included 0.50, indicating a predictive value no different from chance. Figure 2 provides plots of the ROC curves for those variables with statistically significant AUC estimates. In the plot, parental history of myopia was represented by number of myopic parents (i.e., no, one, or two myopic parents).
TABLE 3.
AUC Associated with Predictive Models Computed Using Univariate Logistic Regression Predicting Future Myopia
| Variable | AUC | SE | 95% CI |
|---|---|---|---|
| Cycloplegic sphere | 0.86 | 0.02 | 0.83–0.89 |
| Corneal power | 0.59 | 0.03 | 0.54–0.64 |
| Axial length | 0.62 | 0.03 | 0.58–0.67 |
| Hours of sports/outdoor activity | 0.68 | 0.03 | 0.64–0.73 |
| Number of myopic parents | 0.66 | 0.03 | 0.61–0.70 |
| Hours of reading | 0.56 | 0.03 | 0.51–0.61 |
| Hours of TV | 0.54 | 0.03 | 0.49–0.59 |
| Hours of studying | 0.54 | 0.03 | 0.49–0.59 |
| Diopter hours | 0.50 | 0.03 | 0.45–0.55 |
| Computer/video games hours | 0.50 | 0.03 | 0.45–0.55 |
FIGURE 2.
ROC curves associated with sphere, axial length, corneal power, sports and outdoor hours, reading hours, and parental myopia.
To assess how well information available in the third grade could anticipate onset of myopia, multivariate logistic models were fitted. The task was to determine the predictive ability of parental history of myopia and parental report of children’s reading hours per week and hours per week of sports and outdoor activity. The predictor set was restricted to these three variables because they were the only ones that showed statistically significant differences between myopes and nonmyopes in the univariate analyses, or, in the case of reading hours per week, had an AUC significantly greater than 0.50, as summarized in Tables 2 and 3.
The multivariate logistic analysis used all three significant variables from the univariate analyses, and reading hours per week was not statistically significant (Table 4). When reading hours per week was removed from the predictor set, the number of myopic parents and hours per week of sports and outdoor activity both continued to be significantly associated with future myopia. There was no statistically significant difference between the two AUCs (AUC ± SE: model with reading = 0.73 ± 0.03, model without reading = 0.73 ± 0.03). The logistic model including only sport and outdoor activity hours per week and parental myopia was selected as the best model because it was statistically equivalent to the alternative, but was a more parsimonious model. Models including gender and the interactions of gender and parental myopia and the interaction of gender and sports and outdoor activity hours per week were also constructed. Gender was not statistically significant in any of these models (data not shown).
TABLE 4.
Logistic Model Showing Results of Inclusion of All Significant Variables from the AUC Models Adjusted for Other Variables
| Variable | OR (95% CI) | P |
|---|---|---|
| Model 1 | ||
| Number of myopic parents | ||
| One | 2.05 (1.05–3.98) | 0.03 |
| Two | 4.92 (2.48–9.77) | <0.0001 |
| Sports/outdoors hours | 0.91 (0.87–0.95) | <0.0001 |
| Reading hours | 1.03 (0.98–1.10) | 0.26 |
| Model 2 | ||
| Number of myopic parents | ||
| One | 2.08 (1.07–4.05) | 0.03 |
| Two | 5.07 (2.56–10.05) | <0.0001 |
| Sports/outdoors hours | 0.91 (0.87–0.95) | <0.0001 |
The correlation between sports and outdoor activity hours per week and reading hours per week was not significant (r = 0.01, P = 0.80), indicating that sports and outdoor activity hours per week were not simply reducing the effect of reading hours per week due to correlation between the two variables. To explore further the effects of parental history of myopia and activity levels on future myopia and to assess a potential effect modification between sports and outdoor activities and reading, we performed a sequence of nine logistic regressions using the following predictors: the number of reading hours per week, the number of sports and outdoor activity hours per week, the number of myopic parents, and the pair-wise interactions among these three factors. Hours of reading per week was not significant in any models tested, nor were there any statistically significant interactions with reading hours per week and parental myopia history or reading hours per week and sports and outdoor activity hours; however, sports and outdoor activity hours per week, parental myopia history, and their interaction were statistically significant effects in all models tested.
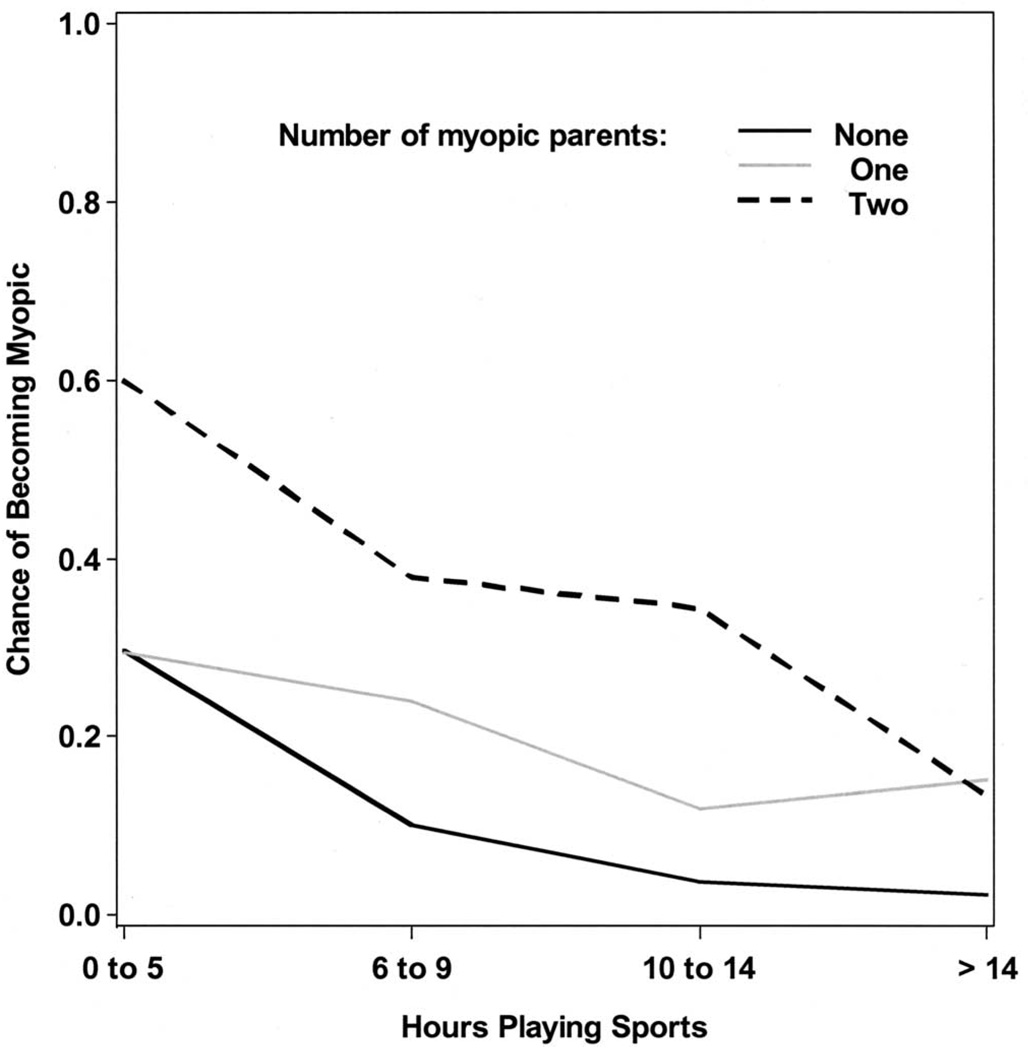
The interaction between sports and outdoor activity hours per week and number of myopic parents was explored through trends in the observed data. For each level of parental history of myopia, Figure 3 presents the observed chance of becoming myopic as a function of sports and outdoor activity hours per week. For these estimates, subjects were grouped according to their level of sports and outdoor activity hours per week using the variable’s quartiles. For the middle 50% of the sports and outdoor activity range, the graph shows that the chance of future myopia in subjects with one myopic parent is between that associated with no and two myopic parents. At the lowest quartile, those children with one myopic parent appeared to have a chance of becoming myopic similar to the children with no myopic parents, with the observed chance of myopia being highest among children with two myopic parents and a low level of sports and outdoor activities. At the highest quartile, those children with two myopic parents appeared to have a chance of becoming myopic similar to those children with one myopic parent, whereas those with no myopic parents and high sports and outdoor activity levels had a very low observed chance of myopia. Which parent (mother or father) was myopic had no effect (data not shown). The average number of hours per week of sports and outdoor activity was also compared to the hours per week of reading stratified at the median hour of reading. The same effect was seen within both strata, with the odds associated with a 1-unit increase in hours per week of sports and outdoor activity, yielding an odds ratio of 0.90 in each level.
FIGURE 3.
Probability of myopia by quartile of sports and outdoor activity hours per week and the number of myopic parents.
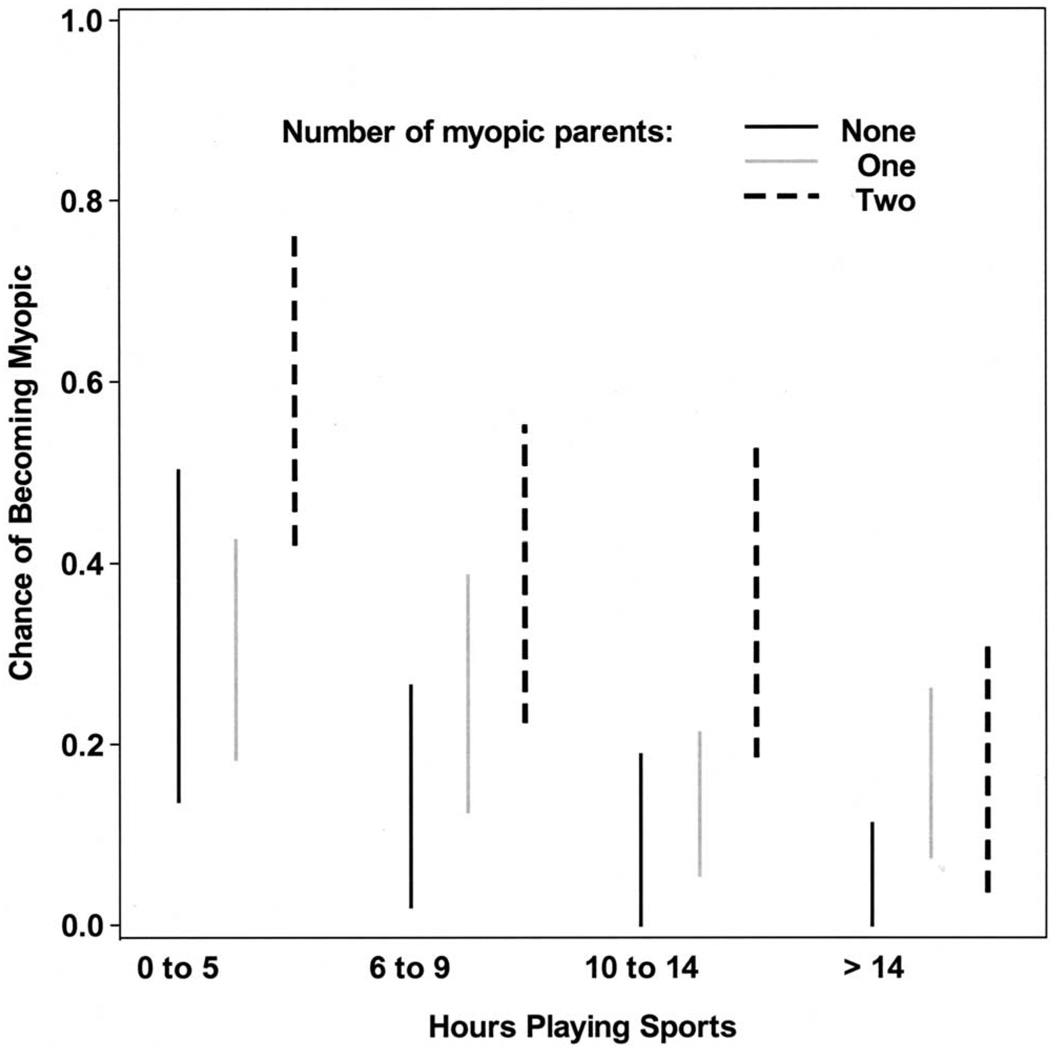
The width of the confidence interval for each estimate of the probability of myopia is shown in Figure 4. Table 5 shows the distribution of subjects in the sports and outdoor activity quartiles as a function of the number of myopic parents (χ2 test P = 0.05). Although there is variation in the proportion of subjects in each category, there are no categories with an extremely low percentage of subjects.
FIGURE 4.
Width of the 95% CI associated with the probability of myopia among the levels of sports and outdoor activity stratified by number of myopic parents.
TABLE 5.
Distribution of Parental Myopia among the Quartiles of Sports and Outdoor Activity Participation
| Sports/Outdoor Activity Groups |
No Myopic Parents |
One Myopic Parent |
Two Myopic Parents |
|---|---|---|---|
| 0 to 5 hours | 27 (21%) | 61 (24%) | 35 (26%) |
| 6 to 9 hours | 30 (23%) | 46 (18%) | 37 (28%) |
| 10 to 14 hours | 27 (21%) | 76 (31%) | 32 (24%) |
| More than 14 hours | 47 (36%) | 66 (27%) | 30 (22%) |
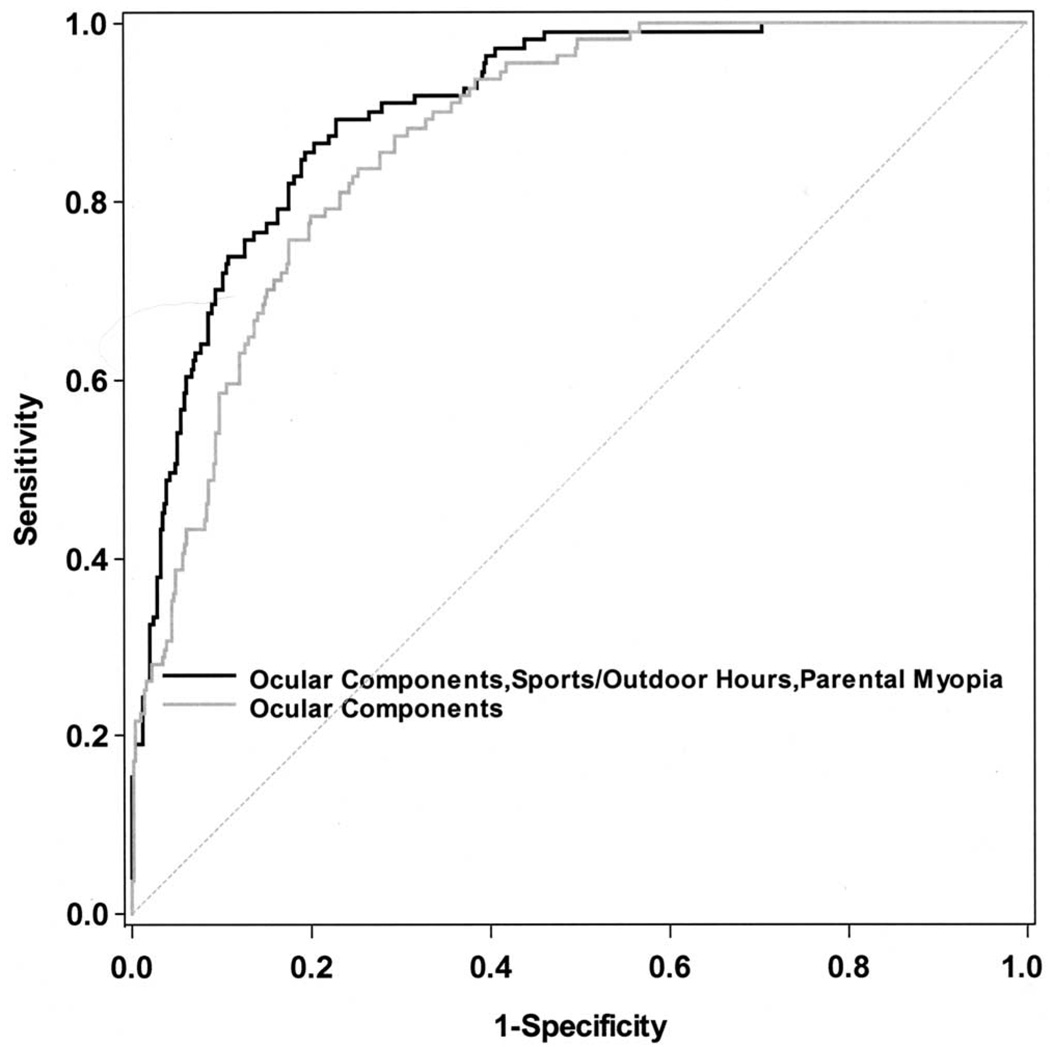
To integrate the results of the model of parental myopia and sports and outdoor activity with our previous work, we show in Table 6 the ROC curve results of three different models: the sports and outdoor activity-by-parents interaction model described herein; a model containing cycloplegic sphere, axial length, and corneal power, which is the best model from our previous work; and a model combining the ocular components with the predictors of the sports and outdoor activity-by-parents interaction. (The results of the multiple comparison of the best [MCB] analysis [difference, lower and upper bounds] are also presented in Table 6). In terms of predictive ability, the ocular components model is a better model than the model of sports and outdoor activity hours, parental myopia, and the interaction; however, the ocular components model was significantly improved by adding sports and outdoor activity hours per week, parental myopia, and the interaction between the two (lower bound = 0, indicating this is the preferred model). Figure 5 provides the ROC curve model that predicts future myopia as a function of cycloplegic sphere, axial length, corneal power, sports and outdoor activity hours per week, parental history of myopia, and the interaction of these two variables.
TABLE 6.
AUC Estimates for Models
| Logistic Regression Model Terms | AUC | SE | Difference* | 95% CI |
|---|---|---|---|---|
| Sports/outdoor activity hours, number of myopic parents, and sports* myopic parents interaction |
0.75 | 0.03 | −0.15 | −0.20-0 |
| Sphere, axial length, corneal power | 0.87 | 0.02 | −0.03 | −0.05-0 |
| Sphere, axial length, corneal power, sports/outdoor activity hours, number of myopic parents, and sports* myopic parents interaction |
0.90 | 0.02 | 0.03 | 0–0.05 |
Difference between AUC and the best of the remaining AUCs using the multiple comparison of the best analysis.
FIGURE 5.
ROC curve for a model using sphere, axial length, corneal power, number of myopic parents, sports and outdoor activity hours, and interaction of myopic parent number and sports and outdoor activity hours compared with a model including only sphere, axial length, and corneal power.
To assess the robustness of our model, we revisited the analysis using all subjects with a third-grade visit. We used a discrete time hazard model31 to conduct a survival analysis applying the models as presented in Table 6. The results from the survival analysis were consistent with the logistic regression models (data not shown). Because the logistic model is consistent with the optimal model from our original predictors paper, we present only the results of the logistic model.
DISCUSSION
Analysis of the development of myopia based on values of parental history and activities outside of school showed that a lower level of sports and outdoor activity and having myopic parents were the best nonocular predictors of future myopia in the premyopic third grader. This is another confirmation of results seen for the important role of parental myopia history.17,24,25,32,33 Attempts to evaluate reading hours from several different angles did not produce a significant effect for this activity. The number of hours of reading per week was not a significant factor in the logistic models, but, because it performed slightly better than chance in the ROC model and because of its prominence as a potential risk factor, we evaluated it with multivariate modeling to assess its impact after other variables were controlled for and to assess potential interactions. Controlling for gender of the subject did not affect the results. This is in contrast with the results of Pärssinen and Lyyra,34 who evaluated factors associated with myopic progression in a clinical trial of myopic children. They assessed hours of near work, defined as reading and other unspecified close work, and the number of hours spent on sports and outdoor activities. Models were built separately for boys and girls, with slight differences in the statistically significant variables in the analysis of variance models. In boys, near work was not significantly related to the progression of myopia, but the number of sports and outdoor activity hours was inversely related (P < 0.01). For girls, reading and the number of hours of near work were associated with myopia progression (P < 0.05), but sports and outdoor activity hours were not.
Exposure to distant stimuli has an asymmetric effect with 2 to 3 hours of normal vision neutralizing the effects of 9 to 12 hours of hyperopic defocus from minus lens treatment in tree shrew.35 These results could be translated to the human experience, in that it may not be the reading time (i.e., the potential exposure to hyperopic defocus), that the children experience that is relevant to their risk of eventual myopia but the amount of distance activity in which they are engaged. A recent study of the impact of defocus in the presence of hyperopic defocus in the tree shrew may have relevance to the results of the current study.36 The animals were presented with a visual stimulus that was at least 1 m away. Fifty percent of the eyes that were wearing a lens that created myopic defocus were able to block the development of myopia. The greatest deterrent to myopia in the presence of hyperopic defocus was a plano lens. These results indicate that perhaps distance clarity is a more effective cue in the mammalian eye than is defocus. The risk from any potential “grow” signal may not be relevant if there is a sufficient “stop” signal to counteract it. The hours of sports and outdoor activity per week may provide this stop signal; however, given the nature of childhood (i.e., intermittent glancing around and refocusing), the source of the “go” signal in humans is equivocal. To apply this finding to the development of human refractive error, an understanding of how the timing of alterations in chicks might correspond to defocus timing in humans is needed. The application of plus at near in bifocals has not been as effective in children as would have been predicted from animal experimentation. Children experiencing myopic defocus at distance from undercorrection had faster progression of myopia rather than slower.37 The importance of hyperopic defocus before myopia onset may also be questioned.19
In searching for a possible explanation about what kind of effect sports and outdoor activity could have, the question arises as to whether it may exert an influence over refractive error by nonvisual means (e.g., increased blood flow) that has inhibitory effects on ocular growth. Lovasik et al.38 found that exercise seemed to cause little change in choroidal blood flow. Other studies have reported that choroidal blood flow did not seem to have a role in axial elongation but may just be the result of the eye growing longer.39 This evidence would imply that the effect of blood flow is not a reasonable avenue to pursue.
Confounding effects must also be considered. Myopia has been associated with other characteristics such as IQ40–42 and personality.43,44 Perhaps increased sports and outdoor activity can be a surrogate for a more extroverted personality with a particular school achievement profile that is protective against myopia. Sports and psychology research involves determination of the dimensions that produce high-caliber athletes45 or relates physical activity to the behavior and mood of schoolchildren and teens.46–49 Extroversion was found more frequently in endurance athletes than in those subjects who did not exercise. Those who engage in endurance sports have higher levels of extroversion than regular participants in exercise.50 Eysenck et al.51 indicate that sports participants’ tendency toward extroversion is well documented, independent of the level at which they participate, but stress that the literature on the topic is of poor quality. They stress, like others in the field, that both personality and sport are multidimensional concepts with uncertainty within the respective fields about the best way to measure them and categorize.51,52
Likewise, there is no body of literature addressing the relation between intelligence and sport participation and most of the studies tend to deal with academic performance rather than intelligence, per se. For example one study looking at sports participation and academic activity found no significant difference in grade point average between those who participated in more hours of sports per week and those who spent less time,46 whereas another study found that high-level exercisers had higher grade point averages than low-level exercisers.49 Another study reported that children who spent at least 1 to 2 hours a week in sports and 1 to 2 hours a week in other activities (e.g., music, clubs) had higher odds of studying more than 3 hours a week.47 Future studies of the effects of sports and outdoor activity on myopia should include assessment of these potential confounding covariates.
It must be noted that although it could be the effect of sports on myopia development, we are unable to attribute it directly to sports. The question, as written, asks about the number of hours per week that the subject spends in sports and outdoor activities. It is possible that the effect may represent participation in outdoor activities rather than sports.
In assessing these results, it is possible that using a parental questionnaire asking about the number of hours per week that a child spends in various activities may present difficulties. The reliability of the visual activity questionnaire is not well established. The questionnaire may not be seeking the most appropriate information to target the amount of near work or other activities actually completed. For example, estimates of sports and outdoor activity hours may be more accurate. Because they transport children to and from sporting activities, parents may have a better estimate of the time spent in sporting activities than of how the child spends his or her indoor time in various activities. A previous study showed that the results of our questionnaire compare favorably with a more detailed questionnaire developed and used in Singapore.17 Similar results for the effect of outdoor activities in a cross-sectional study were also reported recently by the Sydney Myopia Study, which reported a significant association between myopia and outdoor leisure activities (OR = 0.77, 95% CI = 0.66–0.91; Rose KA et al. IOVS 2006;47:ARVO E-Abstract 5453). A possible solution to the problem of using a questionnaire to assess activity is to use the experience-sampling method (ESM).53 This technique has been used in a sample of children from the Contact Lenses and Myopia Progression (CLAMP) Study54 and is currently being used in the Study of the Progression of Nearsightedness (SPAN), to evaluate near work as a risk factor for adult myopic progression.55
We may also be seeing an effect of missing data. If the subjects who were not observed through the eighth grade were more or less likely to become myopic than those subjects with complete follow-up, our estimates could be biased. In a previous study, we evaluated the number of visits across refractive error groups (myopes, emmetropes, emmetropizing hyperopes, and persistent hyperopes) and found that emmetropes had fewer visits on average than did the other groups.56 The emmetropes were also significantly older than the other groups at baseline, which we believe is due to the design of the study allowing staggered entry and our imposition of a limit on the enrollment of younger children in the later years of the study. The primary reason for incomplete data was the study’s investigator-imposed end rather than subject withdrawal. The study ended before the subjects with incomplete data had the opportunity to have their final visits in the eighth grade—that is, the subjects did not withdraw because of risk factors for development of myopia. Although this may have affected the number of myopes we were able to study, it should not create an outcome-related bias among the subjects who did not have the opportunity to complete the study compared with subjects with complete data. There are a few variables that are significantly different between the subjects with complete and incomplete data (Table 1). Results of a survival analysis including censored data were consistent with the results reported herein. There was a statistically significant difference in the parent-reported average number of sport and outdoor activity hours in the third grade between those with complete follow-up and those without complete follow-up (10.86 h/wk vs. 9.59 h/wk). Because there is not a body of literature to refer to when deciding how large a difference in visual activity hours per week is meaningful, it is not possible to quantify clinically any effect of the differences between the two groups. If we were to assume a clinically significant difference, it would only inflate the estimation of the protective effect of sport and outdoor activity hours.
The results may also be affected by observing the children only through grade eight. There are still potential myopes who have not yet converted to myopia by then, thus potentially biasing the results. Another limitation to the use of these activity factors as predictors is that all the data come from assessments in the third grade (i.e., at only one time point). The effects of reading or sports and outdoor activity may be different at other ages. Alternatively, the amount of various activities that a child engages in may be formed by the family dynamics and therefore may be relatively constant across the age range of interest. Future models may incorporate assessments made at various ages. Although the predictors are cross-sectional (e.g., activity level at third grade), the analysis uses longitudinal information about these subjects’ eventual refractive error. This allows us to use the actual myopia status of individual children instead of using inferences based cross-sectional data.
CONCLUSIONS
Greater weekly participation in sports and outdoor activities in the third grade was associated with reduced odds of having myopia by the eighth grade. Reading time was only marginally significant in the univariate predictive models and was not significant in the final, multivariate models. Sports and outdoor hours per week and reading hours per week were not significantly correlated. Parental history of myopia was an important predictor in univariate and multivariate models, with a differential effect of sports and outdoor activity hours per week based on the number of myopic parents. Lower amounts of sports and outdoor activity increased the odds of becoming myopic in those children with two myopic parents more than in those children with either no or one myopic parent. The chance of becoming myopic for children with no myopic parents, compared with those with one or two myopic parents, appears lowest in the children with the highest amount of sports and outdoor activity.
Acknowledgments
Supported by the National Eye Institute and the Office of Minority Research, National Institutes of Health, Grants U10-EY08893 and R24-EY014792; and the Ohio Lions Eye Research Foundation; and the E. F. Wildermuth Foundation.
Footnotes
Presented in part at the Fourth U.S. Symposium on Ocular Epidemiology, Sarasota, Florida, January, 2006.
Disclosure: L.A. Jones, None; L.T. Sinnott, None; D.O. Mutti, None; G.L. Mitchell, None; M.L. Moeschberger, None; K. Zadnik, None
References
- 1.Javitt JC, Chiang YP. The socioeconomic aspects of laser refractive surgery. Arch Ophthalmol. 1994;112:1526–1530. doi: 10.1001/archopht.1994.01090240032022. [DOI] [PubMed] [Google Scholar]
- 2.Sperduto RD, Seigel D, Roberts J, Rowland M. Prevalence of myopia in the United States. Arch Ophthalmol. 1983;101:405–407. doi: 10.1001/archopht.1983.01040010405011. [DOI] [PubMed] [Google Scholar]
- 3.Lee KE, Klein BE, Klein R, Wong TY. Changes in refraction over 10 years in an adult population: the Beaver Dam Eye study. Invest Ophthalmol Vis Sci. 2002;43:2566–2571. [PubMed] [Google Scholar]
- 4.Lin LL, Shih YF, Tsai CB, et al. Epidemiologic study of ocular refraction among schoolchildren in Taiwan in 1995. Optom Vis Sci. 1999;76:275–281. doi: 10.1097/00006324-199905000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Quek TP, Chua CG, Chong CS, et al. Prevalence of refractive errors in teenage high school students in Singapore. Ophthalmic Physiol Opt. 2004;24:47–55. doi: 10.1046/j.1475-1313.2003.00166.x. [DOI] [PubMed] [Google Scholar]
- 6.Lam CS, Goldschmidt E, Edwards MH. Prevalence of myopia in local and international schools in Hong Kong. Optom Vis Sci. 2004;81 doi: 10.1097/01.opx.0000134905.98403.18. 317-223. [DOI] [PubMed] [Google Scholar]
- 7.Fan DS, Lam DS, Lam RF, et al. Prevalence, incidence, and progression of myopia of school children in Hong Kong. Invest Ophthalmol Vis Sci. 2004;45:1071–1075. doi: 10.1167/iovs.03-1151. [DOI] [PubMed] [Google Scholar]
- 8.Gwiazda J, Hyman L, Hussein M, et al. A randomized clinical trial of progressive addition lenses versus single vision lenses on the progression of myopia in children. Invest Ophthalmol Vis Sci. 2003;44:1492–1500. doi: 10.1167/iovs.02-0816. [DOI] [PubMed] [Google Scholar]
- 9.Fulk GW, Cyert LA, Parker DE. A randomized trial of the effect of single-vision vs. bifocal lenses on myopia progression in children with esophoria. Optom Vis Sci. 2000;77:395–401. doi: 10.1097/00006324-200008000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Walline JJ, Jones LA, Mutti DO, Zadnik K. A randomized trial of the effects of rigid contact lenses on myopia progression. Arch Ophthalmol. 2004;122:1760–1766. doi: 10.1001/archopht.122.12.1760. [DOI] [PubMed] [Google Scholar]
- 11.Shih YF, Chen CH, Chou AC, Ho TC, Lin LL, Hung PT. Effects of different concentrations of atropine on controlling myopia in myopic children. J Ocul Pharmacol Ther. 1999;15:85–90. doi: 10.1089/jop.1999.15.85. [DOI] [PubMed] [Google Scholar]
- 12.Shih YF, Hsiao CK, Chen CJ, Chang CW, Hung PT, Lin LL. An intervention trial on efficacy of atropine and multi-focal glasses in controlling myopic progression. Acta Ophthalmol Scand. 2001;79:233–236. doi: 10.1034/j.1600-0420.2001.790304.x. [DOI] [PubMed] [Google Scholar]
- 13.Siatkowski RM, Cotter S, Miller JM, Scher CA, Crockett RS, Novack GD. Safety and efficacy of 2% pirenzepine ophthalmic gel in children with myopia: a 1-year, multicenter, double-masked, placebo-controlled parallel study. Arch Ophthalmol. 2004;122:1667–1674. doi: 10.1001/archopht.122.11.1667. [DOI] [PubMed] [Google Scholar]
- 14.Tan DT, Lam DS, Chua WH, Shu-Ping DF, Crockett RS. One-year multicenter, double-masked, placebo-controlled, parallel safety and efficacy study of 2% pirenzepine ophthalmic gel in children with myopia. Ophthalmology. 2005;112:84–91. doi: 10.1016/j.ophtha.2004.06.038. [DOI] [PubMed] [Google Scholar]
- 15.Saw SM, Chua WH, Hong CY, et al. Nearwork in early-onset myopia. Invest Ophthalmol Vis Sci. 2002;43:332–339. [PubMed] [Google Scholar]
- 16.Angle J, Wissmann DA. The epidemiology of myopia. Am J Epidemiol. 1980;111:220–228. doi: 10.1093/oxfordjournals.aje.a112889. [DOI] [PubMed] [Google Scholar]
- 17.Mutti DO, Mitchell GL, Moeschberger ML, Jones LA, Zadnik K. Parental myopia, near work, school achievement, and children’s refractive error. Invest Ophthalmol Vis Sci. 2002;43:3633–3640. [PubMed] [Google Scholar]
- 18.Goss DA. Nearwork and myopia. Lancet. 2000;356:1456–1457. doi: 10.1016/S0140-6736(00)02864-6. [DOI] [PubMed] [Google Scholar]
- 19.Mutti DO, Mitchell GL, Hayes JR, et al. Accommodative lag before and after the onset of myopia. Invest Ophthalmol Vis Sci. 2006;47:837–846. doi: 10.1167/iovs.05-0888. [DOI] [PubMed] [Google Scholar]
- 20.Gwiazda J, Thorn F, Held R. Accommodation, accommodative convergence, and response AC/A ratios before and at the onset of myopia in children. Optom Vis Sci. 2005;82:273–278. doi: 10.1097/01.opx.0000159363.07082.7d. [DOI] [PubMed] [Google Scholar]
- 21.Gwiazda JE, Hyman L, Norton TT, et al. Accommodation and related risk factors associated with myopia progression and their interaction with treatment in COMET children. Invest Ophthalmol Vis Sci. 2004;45:2143–2151. doi: 10.1167/iovs.03-1306. [DOI] [PubMed] [Google Scholar]
- 22.Zadnik K, Mutti DO, Friedman NE, et al. Ocular predictors of the onset of juvenile myopia. Invest Ophthalmol Vis Sci. 1999;40:1936–1943. [PubMed] [Google Scholar]
- 23.Walline JJ, Zadnik K, Mutti DO. Validity of surveys reporting myopia, astigmatism, and presbyopia. Optom Vis Sci. 1996;73:376–381. doi: 10.1097/00006324-199606000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Pacella R, McLellan J, Grice K, Del Bono EA, Wiggs JL, Gwiazda JE. Role of genetic factors in the etiology of juvenile-onset myopia based on a longitudinal study of refractive error. Optom Vis Sci. 1999;76:381–386. doi: 10.1097/00006324-199906000-00017. [DOI] [PubMed] [Google Scholar]
- 25.Yap M, Wu M, Liu ZM, Lee FL, Wang SH. Role of heredity in the genesis of myopia. Ophthalmic Physiol Opt. 1993;13:316–319. doi: 10.1111/j.1475-1313.1993.tb00479.x. [DOI] [PubMed] [Google Scholar]
- 26.Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143:29–36. doi: 10.1148/radiology.143.1.7063747. [DOI] [PubMed] [Google Scholar]
- 27.Campbell G. Advances in statistical methodology for the evaluation of diagnostic and laboratory tests. Stat Med. 1994;13:499–508. doi: 10.1002/sim.4780130513. [DOI] [PubMed] [Google Scholar]
- 28.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–845. [PubMed] [Google Scholar]
- 29.Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology. 1983;148:839–843. doi: 10.1148/radiology.148.3.6878708. [DOI] [PubMed] [Google Scholar]
- 30.Hsu J. Multiple Comparisons: Theory and Methods. London: Chapman & Hall; 1996. [Google Scholar]
- 31.Singer J, Willett J. It’s about time: using discrete-time survival analysis. J Educ Stat. 1993;18:155–195. [Google Scholar]
- 32.Hammond CJ, Snieder H, Gilbert CE, Spector TD. Genes and environment in refractive error: the twin eye study. Invest Ophthalmol Vis Sci. 2001;42:1232–1236. [PubMed] [Google Scholar]
- 33.Lyhne N, Sjolie AK, Kyvik KO, Green A. The importance of genes and environment for ocular refraction and its determiners: a population based study among 20–45 year old twins. Br J Ophthalmol. 2001;85:1470–1476. doi: 10.1136/bjo.85.12.1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Parssinen O, Lyyra AL. Myopia and myopic progression among schoolchildren: a three-year follow-up study. Invest Ophthalmol Vis Sci. 1993;34:2794–2802. [PubMed] [Google Scholar]
- 35.Shaikh AW, Siegwart JT, Jr, Norton TT. Effect of interrupted lens wear on compensation for a minus lens in tree shrews. Optom Vis Sci. 1999;76:308–315. doi: 10.1097/00006324-199905000-00019. [DOI] [PubMed] [Google Scholar]
- 36.Norton TT, Siegwart JT, Jr, Amedo AO. Effectiveness of hyperopic defocus, minimal defocus, or myopic defocus in competition with a myopiagenic stimulus in tree shrew eyes. Invest Ophthalmol Vis Sci. 2006;47:4687–4699. doi: 10.1167/iovs.05-1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chung K, Mohidin N, O’Leary DJ. Undercorrection of myopia enhances rather than inhibits myopia progression. Vision Res. 2002;42:2555–2559. doi: 10.1016/s0042-6989(02)00258-4. [DOI] [PubMed] [Google Scholar]
- 38.Lovasik JV, Kergoat H, Riva CE, Petrig BL, Geiser M. Choroidal blood flow during exercise-induced changes in the ocular perfusion pressure. Invest Ophthalmol Vis Sci. 2003;44:2126–2132. doi: 10.1167/iovs.02-0825. [DOI] [PubMed] [Google Scholar]
- 39.Reiner A, Shih YF, Fitzgerald ME. The relationship of choroidal blood flow and accommodation to the control of ocular growth. Vision Res. 1995;35:1227–1245. doi: 10.1016/0042-6989(94)00242-e. [DOI] [PubMed] [Google Scholar]
- 40.Schmid KL, Wildsoet CF. Effects on the compensatory responses to positive and negative lenses of intermittent lens wear and ciliary nerve section in chicks. Vision Res. 1996;36:1023–1036. doi: 10.1016/0042-6989(95)00191-3. [DOI] [PubMed] [Google Scholar]
- 41.Rosner M, Belkin M. Intelligence, education, and myopia in males. Arch Ophthalmol. 1987;105:1508–1511. doi: 10.1001/archopht.1987.01060110054030. [DOI] [PubMed] [Google Scholar]
- 42.Teasdale TW, Fuchs J, Goldschmidt E. Degree of myopia in relation to intelligence and educational level. Lancet. 1988;2:1351–1354. doi: 10.1016/s0140-6736(88)90880-x. [DOI] [PubMed] [Google Scholar]
- 43.Beedle SL, Young FA. Values, personality, physical characteristics, and refractive error. Am J Optom Physiol Opt. 1976;53:735–739. [PubMed] [Google Scholar]
- 44.Gawron VJ. Ocular accommodation, personality, and autonomic balance. Am J Optom Physiol Opt. 1983;60:630–639. doi: 10.1097/00006324-198307000-00011. [DOI] [PubMed] [Google Scholar]
- 45.Backmand H, Kaprio J, Kujala U, Sarna S. Personality and mood of former elite male athletes–a descriptive study. Int J Sports Med. 2001;22:215–221. doi: 10.1055/s-2001-16382. [DOI] [PubMed] [Google Scholar]
- 46.Fisher M, Juszczak L, Friedman SB. Sports participation in an urban high school: academic and psychologic correlates. J Adolesc Health. 1996;18:329–334. doi: 10.1016/1054-139X(95)00067-3. [DOI] [PubMed] [Google Scholar]
- 47.Harrison PA, Narayan G. Differences in behavior, psychological factors, and environmental factors associated with participation in school sports and other activities in adolescence. J Sch Health. 2003;73:113–120. doi: 10.1111/j.1746-1561.2003.tb03585.x. [DOI] [PubMed] [Google Scholar]
- 48.Taras H. Physical activity and student performance at school. J Sch Health. 2005;75:214–218. doi: 10.1111/j.1746-1561.2005.00026.x. [DOI] [PubMed] [Google Scholar]
- 49.Field T, Diego M, Sanders CE. Exercise is positively related to adolescents’ relationships and academics. Adolescence. 2001;36:105–110. [PubMed] [Google Scholar]
- 50.Egloff B, Gruhn AJ. Personality and endurance sports. Personal Individ Diff. 1996;21:223–229. [Google Scholar]
- 51.Eysenck HJ, Nias DKB, Cox DN. Sport and personality. Adv Behav Res Ther. 1982;4:1–56. [Google Scholar]
- 52.Kirkcaldy B, Furnham A. Extraversion, neuroticism, psychoticism and recreational choice. Personal Individ Diff. 1991;12:737–745. [Google Scholar]
- 53.Rah MJ, Mitchell GL, Zadnik K. Use of the experience sampling method to measure nearwork. Optom Vis Sci. 2004;81:82–87. doi: 10.1097/00006324-200402000-00005. [DOI] [PubMed] [Google Scholar]
- 54.Rah MJ, Walline JJ, Lynn Mitchell G, Zadnik K. Comparison of the experience sampling method and questionnaires to assess visual activities in pre-teen and adolescent children. Ophthalmic Physiol Opt. 2006;26:483–489. doi: 10.1111/j.1475-1313.2006.00372.x. [DOI] [PubMed] [Google Scholar]
- 55.Bullimore MA, Reuter KS, Jones LA, Mitchell GL, Zoz J, Rah MJ. The Study of Progression of Adult Nearsightedness (SPAN): design and baseline characteristics. Optom Vis Sci. 2006;83:594–604. doi: 10.1097/01.opx.0000230274.42843.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jones LA, Mitchell GL, Mutti DO, Hayes JR, Moeschberger ML, Zadnik K. Comparison of ocular component growth curves among refractive error groups in children. Invest Ophthalmol Vis Sci. 2005;46:2317–2327. doi: 10.1167/iovs.04-0945. [DOI] [PubMed] [Google Scholar]