Abstract
Background/Aims
Irritable bowel syndrome (IBS) is a biopsychosocial disorder. 5-Hydroxytryptamine (5-HT) plays a crucial role in the control of gastrointestinal motility, sensation, and secretion. This study investigated changes in platelet-depleted plasma 5-HT and their correlation with psychopathology in IBS patients and healthy subjects.
Methods
This study involved 21 subjects with IBS and 13 healthy subjects. Fasting and 1-hr postprandial plasma 5-HT concentrations were measured. The SCL-90R symptom checklist was used for the assessment of current psychological symptoms.
Results
Fasting and postprandial plasma 5-HT concentrations were significantly higher in IBS patients (15.11±13.51 ng/mL and 16.31±14.21 ng/mL, respectively) than in healthy subjects (5.55±4.14 ng/mL and 6.25±4.82 ng/mL, respectively; p<0.05). There were no significant changes between fasting and 1-hr postprandial 5-HT concentration in IBS subtypes and healthy subjects. Scores on all SCL-90R subscales except for the interpersonal-sensitivity subscale were significantly higher in IBS patients than in healthy subjects. No correlation was found between SCL-90R items and platelet-depleted plasma 5-HT concentration.
Conclusions
5-HT might play a critical role in IBS, and psychopathological factors are correlated with IBS.
Keywords: Irritable bowel syndrome, 5-hydroxytryptamine, Psychopathology
INTRODUCTION
Irritable bowel syndrome (IBS) is a biopsychosocial disorder affecting 9-17% of patient of all ethnic groups.1 It is associated with abnormal gastrointestinal motor function, visceral sensitivity, and psychosocial or autonomic dysfunction.2 Psychosocial factors, particularly stress, can alter colonic motility, enhance colonic sensation, and influence the timing of patients' presentation to physicians.2-4 Inversely, IBS have a definite impact on health-related quality of life; IBS patients have been found to have a reduced quality of life, as manifested by poorer sleep, problems with employment, relationships, sexual functioning, leisure, travel and diet.5
5-hydroxytryptamine (5-HT), found predominantly within the gastrointestinal tract (80% of body 5-HT), both in enterochromaffin cells (95%) and enteric neurons (5%), is known to play a significant role in the control of gastrointestinal motility, sensation, and secretion.6 Several studies have reported that food intake can stimulate colonic motor activity, change the visceral sensitivity, elevate blood 5-HT levels and lead to symptoms in IBS patients.7-10 5-HT also has central roles in specific brain structures implicated in emotions and stress and their potential relevance to psychological ailments (e.g., anxiety, depression, fear, and stress disorders).11
The aim of this study was to investigate the changes of platelet depleted plasma 5-HT under fasting and fed conditions and its correlation with psychopathology in IBS patients and healthy subjects.
MATERIALS AND METHODS
1. Subjects
This study was carried out on 21 IBS patients diagnosed according to the Rome II criteria12 and 13 healthy subjects. No subject had coexistent disease and all had normal hematology, biochemistry, urinalysis, and sigmoidoscopy, together with a normal colonoscopy or barium enema if aged over 40 years. All healthy controls had normal laboratory investigation (as above) and negative toxicology for substances of abuse. Subjects were excluded if they had: a history of gastrointestinal surgery (other than appendectomy, cholecystectomy, and hiatus hernia repair); gastrointestinal symptoms related to or exacerbated by consumption of milk or milk products; or were taking drugs that might modify either gastrointestinal function or the 5-HT system, such as analgesic medication, tranquillizers, or antidepressants. Subject were excluded if they were pregnant, breast feeding, or hysterectomised, and had to be postpuberty and premenopausal. All medication and cigarette smoking were prohibited for 48 hours prior to the study while alcohol and caffeine containing drinks were stopped 24 hours before the study.
This study was approved by the institutional review board of Chonnam National University Hospital, Gwang-ju, Korea. All subjects were provided with written information on the project, and we obtained the signed informed consent of each subjects.
2. IBS subtypes
We classified the patients with IBS into constipation-predominant (C-IBS), diarrhea-predominant (D-IBS) and alternating diarrhea and constipation (A-IBS) types using the Rome II criteria.12
3. Study design
After an overnight fast, subjects arrived at hospital and an arm vein was cannulated. Blood (9 mL) was taken via vacutainer containing 0.3 mL citrate solution for 5-HT analysis. Further 5 mL blood samples for 5-HT analysis were taken 1 hour later, following ingestion of a standard carbohydrate rich meal (calorie content of 450 kcal) and 200 mL water in the room temprature.
4. Analysis of platelet depleted plasma concentration of 5-HT
Collected blood was transferred to tubes containing 0.5 ml of 3.12% trisodium citrate and centrifuged (room temperature) twice to ensure no platelet contamination of supernatant; initially at 2,500 rpm for 10 minutes and then at 4,000 rpm for a further 10 minutes. Platelet depleted plasma was aspirated and duplicated samples stored at -70℃ for later batch analysis. 5-HT concentrations were measured in duplicate using high performance liquid chromatography (Bio-Rad HPLC kit, Munich, Germany) with fluorometric detection.10,13 All samples were analyzed blind to subject status.
The sensitivity of the high performance liquid chromatography system for the detection of 5-HT was at least 5 nmol/L, with signal to noise ratio of greater than 10 and a coefficient of variation (CV) <20%. The intra-assay CVs for controls for 30.10 nmol/L and 55.66 nmol/L of 5-HT were 4.6% and 4.3%, respectively.
5. Psychological symptom questionnaire
Current psychological symptoms were assessed using the SCL-90R checklist, a self rating test that requires the patient to indicate how much he/she is distressed by each of 90 possible symptoms.14 This test is also scored for a further nine clinical scales: anxiety, depression, hostility, interpersonal sensitivity, obsessive-compulsive behavior, paranoid ideation, phobic behavior, psychosis, and somatization. The raw scores were converted to standard T scores, on a 0-100 scale, using the gender stratified non-psychiatric patient normative group (SCL-90R).
6. Statistical analysis
All statistical analyses were performed by using statistical software (Statistical Program for Social Sciences [SPSS], version 12.0 for Windows; SPSS Inc., Chicago, IL, USA). The student t test was used for continuous variables and the chi-square test with the Yates correction or the Fisher exact test for categorical variables. The paired t test was used for the change of serotonin between fasting and postprandial state. Statistical significance was defined as a p value <0.05 (two-tailed).
RESULTS
1. Characteristics of the study populations
This study was carried out on 21 subjects with IBS (8 men and 13 women), diagnosed according to the Rome II criteria,12 aged 24-78 years (mean 49.5 years), and 13 healthy subjects (7 men and 6 women), aged 29-68 years (mean 49.3 years). Patient with IBS were classified in to diarrhea-predominant (n=10), constipation-predominant (n=11) and alternating type (n=0). There were no statistical differences between the IBS patients and the healthy subjects in age, sex and body mass index (p>0.05, Table 1).
Table 1.
Characteristics of the Study Group
IBS, irritable bowel syndrome; C-IBS, constipation predominant irritable bowel syndrome; D-IBS, diarrahea predominant irritable bowel syndrome.
2. Platelet depleted plasma 5-HT concentrations
1) Difference between IBS subjects and healthy subjects
Under fasting conditions, plasma 5-HT concentration in IBS patients (15.11±13.51 ng/mL) was significantly higher than that of healthy subjects (5.55±4.14 ng/mL, p=0.023). Postprandial 1 hr plasma 5-HT concentration in IBS patients (16.31±14.21 ng/mL) was significantly higher than that of healthy subjects (6.25±4.82 ng/mL, p=0.002, Fig. 1).
Fig. 1.
Platelet-depleted plasma 5-hydroxytryptamine (5-HT) level between IBS patients and healthy subjects. *Serum fasting 5-HT levels were significantly higher in IBS patients and C-IBS patients than in healthy subjects (p<0.05). †Serum postprandial 5-HT levels were significantly higher in IBS patients, C-IBS patients, and D-IBS patients than in healthy subjects (p<0.05). ‡Serum postprandial 5-HT levels were the same as fasting 5-HT levels in D-IBS (p=0.757).
IBS, irritable bowel syndrome; C-IBS, constipation predominant irritable bowel syndrome; D-IBS, diarrhea predominant irritable bowel syndrome.
2) Difference between C-IBS subjects and D-IBS subjects
There were no significant differences in fasting and postprandial 1 hr plasma 5-HT concentrations between C-IBS patients and D-IBS patients (Fig. 1).
3) Difference of IBS subtypes and healthy subjects
Fasting plasma 5-HT concentration in C-IBS patients (14.53±6.61 ng/mL) was significantly higher than that of healthy subjects (5.55±4.14 ng/mL, p=0.006). Postprandial 1hr plasma 5-HT concentration in C-IBS patients (14.91±6.50 ng/mL) was significantly higher than that of healthy subjects (6.25±4.82 ng/mL, p=0.023). Fasting plasma 5-HT concentration in D-IBS patients (15.76±33.17 ng/mL) was higher than that of healthy subjects, but there was no significant difference (p=0.218). Postprandial 1 hr plasma 5-HT concentration in D-IBS patients (17.86±10.12 ng/mL) was significantly higher that of health subjects (p=0.038, Fig. 1).
4) The change between fasting and postprandial 1 hr platelet depleted plasma 5-HT concentrations
Postprandial 1 hr 5-HT concentration was increased compared with fasting 5-HT concentration in D-IBS patients but showed no statistical difference (p=0.757). There were no significant changes between fasting and postprandial 1hr 5-HT concentration in C-IBS patients and healthy subjects (Fig. 1).
3. Comparison of SCL-90 R score between IBS patients and healthy subjects
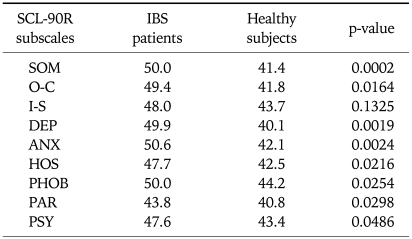
Table 3 gives means for the scores of nine SCL-90R subscales in IBS patients and healthy subjects. IBS patients scored significantly higher than healthy subjects on all SCL-90R subscales, with the exception of the interpersonal-sensitivity subscale (Table 2). No correlation was found between SCL-90R items and platelet depleted plasma 5-HT concentration (Table 3).
Table 3.
Parametric Correlation by Pearson between Platelet-depleted Plasma 5-hydroxytryptamine Levels and SCL-90R Score in IBS Patients
Each figure means correlation coefficient.
IBS, irritable bowel syndrome; SOM, somatization; O-C, obsessive-compulsive; I-S, interpersonal-sensitivity; DEP, depression; ANX, anxiety; HOS, hostility; PHOB, phobic anxiety; PAR, paranoid ideation; PSY, psychoticism.
Table 2.
Comparison of SCL-90R Scores between IBS Patients and Healthy Subjects by t-test
IBS, irritable bowel syndrome; SOM, somatization; O-C, obsessive-compulsive; I-S, interpersonal-sensitivity; DEP, depression; ANX, anxiety; HOS, hostility; PHOB, phobic anxiety; PAR, paranoid ideation; PSY, psychoticism.
DISCUSSION
Many subjects with IBS report exacerbation of their symptoms, particularly abdominal pain and gas, following food ingestion. This appears to be especially associated with meals rich in carbohydrates and fat, as well as being more common in those subjects who are female and/or anxious.15,16 Several studies have indicated that postprandial symptoms may be associated with elevated blood 5-HT levels.9,10 Zuo et al.17 reported that symptomatology following cold water intake may be associated with increased plasma 5-HT concentrations in female subjects with IBS. The majority of 5-HT is synthesized and stored in enterochromaffin cells, which are located throughout the gastrointestinal tract and act as sensory transducer.18,19 The enterochromaffin cells are sensitive to changes in intraluminal pressure and chemical stimuli, and these cells trigger peristaltic and secretory reflexes via primary afferent neurons by secreting 5-HT when the intraluminal pressure increases.18,20 5-HT found in the blood is almost entirely derived from the gastrointestinal tract where it is either rapidly taken up by platelets, which consequently contain the majority of 5-HT in peripheral blood, or is metabolized by the liver and kidney to its metabolite 5-hydroxyindole acetic acid (5-HIAA).21,22 Concentration of 5-HT in platelet depleted plasma will therefore more accurately reflect transient changes in concentration whereas those in platelets might be more indicative of any change over time. Previous studies attempting to address the relationship between plasma 5-HT levels and functional gastrointestinal symptoms have been inconclusive, with one showing that only approximately 14% of subjects with severe gastrointestinal symptoms of a functional but poorly defined nature have elevated levels of plasma 5-HT and another showing only a slightly higher plasma 5-HT concentration in subjects with diarrhea and abdominal pain. Both studies however were carried out under fasting conditions on a heterogeneous group of subjects with functional gastrointestinal disease and did not concurrently assess symptomatology and plasma 5-HT.23 The present study showed that platelet depleted plasma 5-HT concentration in IBS and C-IBS patients was higher than that of healthy subjects under fasting and postprandial conditions. In D-IBS patients, only postprandial 5-HT concentration was higher than that of healthy subjects. Houghton et al.10 reported that symptom exacerbation following meal ingestion in female subjects with D-IBS is associated with increased levels of plasma 5-HT, together with a reduction in 5-HT turnover. But, our study showed that the plasma 5-HT concentration following meal ingestion was not increased significantly in D-IBS patients. In our study, ethnic difference and relatively small sample size from the previous study might lead to different results.
There is growing recognition among physician that, in order to fully understand chronic disease, there should be a convergent assessment not only of biomedical factors, but also of psychosocial ones, such as the physical, social and emotional attitudes and behaviors of patients, as they relate to their prior and current health state, i.e. the health related quality of life (HRQOL).24,25 A previous study using generic HRQOL measures such as the SF-36 has demonstrated that IBS patients have significantly poorer scores than healthy subjects.26,27 It is now clear, for instance, that, on selected SF-36 subscales, IBS patients score significantly lower than patients with gastro-esophageal reflux disease, diabetes mellitus and dialysis-dependent renal disease.27 We used the SCL-90R psychometric checklist for the measurement of psychopathological impairment and distress for individual subjects. SCL-90R is a widely used, validated, generic psychometric checklist composed of nine subscales. Locke et al.28 reported that somatization and interpersonal personality among nine SCL-90R scale were independently associated with functional GI disorders including IBS. In the present study, IBS patients scored significantly higher than healthy subjects on all SCL-90R subscales, with the exception of the interpersonal-sensitivity subscale. Ethnic difference and relatively small sample size from the previous study might lead to different results.
Serotoninergic system to behavior and cognition is imperative for the development of successful treatments for various psychological ailments (e.g., anxiety, depression, fear, and stress disorders) that profoundly impact the quality of human life. Like this, 5-HT plays an important role, not only, in the regulation of GI motility and visceral perception, but also, in the psychological ailments. In fact, antidepressant drugs such as tricyclic antidepressant or selective serotonin reuptake inhibitor were used for the treatment of IBS.11 So, we were interested in the relation of SCL-90R scale and 5-HT levels, but, there was no correlation between SCL-90R and 5-HT levels.
Though small recruited volume of patients, the results show that 5-HT may have a critical role in the pathogenesis of IBS to some degree. Psychopathological factors are found to be related with IBS. However, further study would be necessary regarding the influence of 5-HT dynamics on the psychopathological factor in IBS.
References
- 1.Drossman DA, Li Z, Andruzzi E, et al. U.S. householder survey of functional gastrointestinal disorders: prevalence, sociodemography, and health impact. Dig Dis Sci. 1993;38:1569–1580. doi: 10.1007/BF01303162. [DOI] [PubMed] [Google Scholar]
- 2.Drossman DA, Camilleri M, Mayer EA, Whitehead WE. AGA technical review on irritable bowel syndrome. Gastroenterology. 2002;123:2108–2131. doi: 10.1053/gast.2002.37095. [DOI] [PubMed] [Google Scholar]
- 3.Drossman DA, McKee DC, Sandler RS, et al. Psychosocial factors in the irritable bowel syndrome: a multivariate study of patients and nonpatients with irritable bowel syndrome. Gastroenterology. 1988;95:701–708. doi: 10.1016/s0016-5085(88)80017-9. [DOI] [PubMed] [Google Scholar]
- 4.Whitehead WE, Bosmajian L, Zonderman AB, Costa PT, Jr, Schuster MM. Symptoms of psychologic distress associated with irritable bowel syndrome: comparison of community and medical clinic samples. Gastroenterology. 1988;95:709–714. doi: 10.1016/s0016-5085(88)80018-0. [DOI] [PubMed] [Google Scholar]
- 5.Koloski NA, Talley NJ, Boyce PM. The impact of functional gastrointestinal disorders on quality of life. Am J Gastroenterol. 2000;95:67–71. doi: 10.1111/j.1572-0241.2000.01735.x. [DOI] [PubMed] [Google Scholar]
- 6.Kim DY, Camilleri M. Serotonin: a mediator of the brain-gut connection. Am J Gastroenterol. 2000;95:2698–2709. doi: 10.1111/j.1572-0241.2000.03177.x. [DOI] [PubMed] [Google Scholar]
- 7.Snape WJ, Jr, Matarazzo SA, Cohen S. Effect of eating and gastrointestinal hormones on human colonic myoelectrical and motor activity. Gastroenterology. 1978;75:373–378. [PubMed] [Google Scholar]
- 8.Steadman CJ, Phillips SF, Camilleri M, Haddad AC, Hanson RB. Variation of muscle tone in the human colon. Gastroenterology. 1991;101:373–381. doi: 10.1016/0016-5085(91)90014-c. [DOI] [PubMed] [Google Scholar]
- 9.Bearcroft CP, Perrett D, Farthing MJ. Postprandial plasma 5-hydroxytryptamine in diarrhoea predominant irritable bowel syndrome: a pilot study. Gut. 1998;42:42–46. doi: 10.1136/gut.42.1.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Houghton LA, Atkinson W, Whitaker RP, Whorwell PJ, Rimmer MJ. Increased platelet depleted plasma 5-hydroxytryptamine concentration following meal ingestion in symptomatic female subjects with diarrhoea predominant irritable bowel syndrome. Gut. 2003;52:663–670. doi: 10.1136/gut.52.5.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim JJ. Serotonin, stress, and conditioning. Biol Psychiatry. 2008;63:819–820. doi: 10.1016/j.biopsych.2008.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thompson WG, Longstreth GF, Drossman DA, Heaton KW, Irvine EJ, Müller-Lissner SA. Functional bowel disorders and functional abdominal pain. Gut. 1999;45(Suppl 2):II43–II47. doi: 10.1136/gut.45.2008.ii43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dursun SM, Szemis A, Andrews H, Whitaker P, Reveley MA. Effects of clozapine and typical antipsychotic drugs on plasma 5-HT turnover and impulsivity in patients with schizophrenia: a cross-sectional study. J Psychiatry Neurosci. 2000;25:347–352. [PMC free article] [PubMed] [Google Scholar]
- 14.Derogatis LR, Rickels K, Rock AF. The SCL-90 and the MMPI: a step in the validation of a new self-report scale. Br J Psychiatry. 1976;128:280–289. doi: 10.1192/bjp.128.3.280. [DOI] [PubMed] [Google Scholar]
- 15.Ragnarsson G, Bodemar G. Pain is temporally related to eating but not to defaecation in the irritable bowel syndrome (IBS): patients' description of diarrhea, constipation and symptom variation during a prospective 6-week study. Eur J Gastroenterol Hepatol. 1998;10:415–421. doi: 10.1097/00042737-199805000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Simrén M, Månsson A, Langkilde AM, et al. Food-related gastrointestinal symptoms in the irritable bowel syndrome. Digestion. 2001;63:108–115. doi: 10.1159/000051878. [DOI] [PubMed] [Google Scholar]
- 17.Zuo XL, Li YQ, Yang XZ, et al. Plasma and gastric mucosal 5-hydroxytryptamine concentrations following cold water intake in patients with diarrhea-predominant irritable bowel syndrome. J Gastroenterol Hepatol. 2007;22:2330–2337. doi: 10.1111/j.1440-1746.2006.04772.x. [DOI] [PubMed] [Google Scholar]
- 18.Pan H, Gershon MD. Activation of intrinsic afferent pathways in submucosal ganglia of the guinea pig small intestine. J Neurosci. 2000;20:3295–3309. doi: 10.1523/JNEUROSCI.20-09-03295.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grider JR, Kuemmerle JF, Jin JG. 5-HT released by mucosal stimuli initiates peristalsis by activating 5-HT4/5-HT1p receptors on sensory CGRP neurons. Am J Physiol. 1996;270:G778–G782. doi: 10.1152/ajpgi.1996.270.5.G778. [DOI] [PubMed] [Google Scholar]
- 20.Gershon MD. Review article: roles played by 5-hydroxytryptamine in the physiology of the bowel. Aliment Pharmacol Ther. 1999;13(Suppl 2):15–30. [PubMed] [Google Scholar]
- 21.Da Prada M, Tranzer JP, Pletscher A. Storage of 5-hydroxytryptamine in human blood platelets. Experientia. 1972;28:1328–1329. doi: 10.1007/BF01965326. [DOI] [PubMed] [Google Scholar]
- 22.Tyce GM, Rorie DK, Byer DE, Danielson DR. Free and conjugated amines in human lumbar cerebrospinal fluid. J Neurochem. 1985;44:322–324. doi: 10.1111/j.1471-4159.1985.tb07149.x. [DOI] [PubMed] [Google Scholar]
- 23.Warner RR. Hyperserotoninemia in functional gastrointestinal disease. Ann Intern Med. 1963;59:464–470. doi: 10.7326/0003-4819-59-4-464. [DOI] [PubMed] [Google Scholar]
- 24.Irvine EJ. Quality of life issues in patients with inflammatory bowel disease. Am J Gastroenterol. 1997;92:18S–24S. [PubMed] [Google Scholar]
- 25.Borgaonkar MR, Irvine EJ. Quality of life measurement in gastrointestinal and liver disorders. Gut. 2000;47:444–454. doi: 10.1136/gut.47.3.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Whitehead WE, Burnett CK, Cook EW, 3rd, Taub E. Impact of irritable bowel syndrome on quality of life. Dig Dis Sci. 1996;41:2248–2253. doi: 10.1007/BF02071408. [DOI] [PubMed] [Google Scholar]
- 27.Gralnek IM, Hays RD, Kilbourne A, Naliboff B, Mayer EA. The impact of irritable bowel syndrome on health-related quality of life. Gastroenterology. 2000;119:654–660. doi: 10.1053/gast.2000.16484. [DOI] [PubMed] [Google Scholar]
- 28.Locke GR, 3rd, Weaver AL, Melton LJ, 3rd, Talley NJ. Psychosocial factors are linked to functional gastrointestinal disorders: a population based nested case-control study. Am J Gastroenterol. 2004;99:350–357. doi: 10.1111/j.1572-0241.2004.04043.x. [DOI] [PubMed] [Google Scholar]