Abstract
The role of duodenal reflux and the time required for the development of Barrett's esophagus has remained controversial. We report a case of Barrett's esophagus that developed 6 months after total gastrectomy. A 76-year-old man diagnosed with gastric adenocarcinoma underwent a total gastrectomy and a Rouxen-Y esophagojejunostomy. The gastroesophageal junction in the resected specimen was both grossly and microscopically normal at the time of the operation. A routine follow-up endoscopic examination performed 6 months later revealed a tongue-like projection of redcolored columnar tissue. No reflux symptoms (heartburn or acid regurgitation) had been present during the intervening 6 months. A biopsy specimen from the esophagus showed intestinal-type metaplasia of the columnar epithelium. This case supports the development of Barrett's esophagus solely from duodenal reflux and after a relatively short time in this clinical setting.
Keywords: Barrett's esophagus, Gastrectomy
INTRODUCTION
Barrett's esophagus (BE) is a condition in which columnar epithelium replaces the squamous epithelium that normally lines the distal esophagus.1 BE is an acquired condition resulting from severe esophageal mucosal injury.2 In human development of BE is clearly associated with gastroesophageal reflux. Patients' with BE typically have greater acid exposure compared to patients with erosive and nonerosive gastroesophageal reflux disease (GERD) without BE.3,4 Animal studies also have shown that excision of esophageal mucosa in conjunction with reflux of either acid alone or acid and bile results in re-epithelialization of the esophagus with primarily columnar epithelium, whereas excision of the esophageal mucosa alone results in re-epithelialization primarily with squamous epithelium.5
The roles of duodenal secretions, as an individual or as the potential synergistic, in the pathophysiology of BE remains unclear due to the limited and conflicting data available. In human, reflux of duodenal contents is increased in BE compared with age-matched controls and GERD patients without BE.6,7 However, another study suggested that without acid, duodenogastroesophageal reflux alone does not contribute to the occurrence of BE.8
Furthermore, long duration of reflux symptoms is associated with the higher prevalence of BE at the time of upper endoscopy.9 Thus, "long-standing reflux symptoms" has been accepted in guideline as a indication for screening endoscopy for the detection of BE.10 However, the time that is required for the development of BE has remained controversial. Our report adds one additional case that developed BE 6 months after total gastrectomy.
CASE REPORT
A previously healthy 76 years old Korean man visited our hospital with a month history of abdominal pain, and epigastric soreness. He had no associated vomiting, dysphagia, heartburn, reflux, or other gastrointestinal complaints. His medical history documented benign prostate hyperplasia a year earlier, but used no medication. He had no known family history of gastrointestinal disorders or cancers. He had a 25 pack/year history of tobacco use and 22 grams per day of alcohol consumption.
His abdomen was soft and flat with mild tenderness in the epigastric region. There were no palpable lymph nodes. Upper endoscopy revealed a huge erythematous, irregular shaped, ulceroinfiltrating mass involving lesser curvature side of body and antrum (Fig. 1A). Retroflexed view during endoscopy of the gastric cardia showed that the mass was about 3 cm distal to esophago-gastric junction (Fig. 1B). Distal esophagus appeared endoscopically normal, without evidence of hiatal hernia, tongues or segments of BE (Fig. 1C). The gastric biopsy showed poorly differentiated tubular adenocarcinoma. The patient underwent a total gastrectomy, and a Roux-en-Y esophagojejunostomy. Pathology of the surgical specimen confirmed adenocarcinoma of the gastric body and antrum with pathologic stage of T3N2Mx. A 0.2 cm of the distal esophagus was included in the gastrectomy specimen and the gastro-esophageal junction in the resected specimen was grossly and microscopically normal (Fig. 2). The patient was discharged without any postoperative complications.
Fig. 1.
Endoscopic findings before total gastrectomy. (A) Forward view of the huge erythematous, irregularly shaped, ulceroinfiltrating mass involving the lesser curvature side of the body and antrum. (B) Retroflexed endoscopic view of the gastric cardia shows that the mass is located 3 cm distal to the esophagogastric junction. (C) The distal esophagus appeares endoscopically normal, without evidence of hiatal hernia, tongues, or segments of Barrett's esophagus.
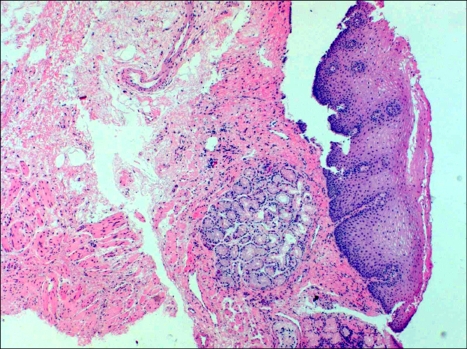
Fig. 2.
Gastroesophageal junction in the resected specimen is both grossly and microscopically normal (H&E stain, ×100).
Six months after gastrectomy, regular follow up endoscopic examination was done. Endoscopic examination revealed tongue-like projection of red-colored columnar tissue extending 3 cm above the anastomosis site (Fig. 3) The. Endoscopic biopsies of the distal esophagus was obtained 2 cm proximal to anastomosis site. Pathology of the endoscopic biopsies of the distal esophagus showed intestinal type metaplasia (Fig. 4). He denied typical reflux symptoms (heartburn or acid regurgitation) during six months.
Fig. 3.
Endoscopic examination after total gastrectomy reveales tongue-like projection of red-colored columnar tissue extending 3 cm above the anastomosis.
Fig. 4.
Endoscopic biopsies of the distal esophagus reveales intestinal-type metaplasia (H&E stain, ×400).
DISCUSSION
The role of bile reflux or enteric reflux in the presence or absence of acid reflux remains controversial. In animal studies, bile reflux alone did not cause columnar re-epithelialization in one study,5 but in other study, esophago-jejunostomy on rats induced glandular metaplasia.11 In human, some authors have suggested a synergistic effect of acid and duodenal reflux in esophageal injury,12 while others suggested that without acid, duodenal reflux alone does not contribute to the occurrence of BE.8 However, as in our case, there have been human cases of post-total gastrectomy development of BE,13-15 which provides evidence that BE can be developed by enteroesophageal reflux only, in the absence of acid.
Additionally, it is generally appreciated that the development of BE needs "long standing" injury. But Westhoff et al., recently reported a case of BE, which developed BE 6 months after total gastrectomy and questioned the concept of "long standing" injury.15 Our patient developed BE 6 months after surgery. Our case supports the findings of Westhoff et al., that other factors may be more important in the development of BE than just the duration of reflux symptoms. It still remains unclear why some patients with gastroesophageal reflux disease develop BE whereas others do not. Our case suggests that either genetic or environmental predisposition is an important factor in the development of BE.
Although total gastrectomy and Roux-en Y procedure is a common procedure in Korea because of high incidence of gastric carcinoma, development of BE in these patients is not reported yet. This may be due to lower prevalence of BE in Korea than Western countries,16 and low awareness of BE by endoscopists during follow up. Therefore, careful follow-up and endoscopic examination is required, since recurrent carcinoma after total gastrectomy has a chance to be adenocarcinoma associated with BE.
In summary, we experienced a rare case of 76 years old Korean male who developed BE six months after total gastrectomy. BE may develop solely from duodenal reflux, it may require relatively short time span for development of BE. We also need careful examination on lower esophagus after total gastrectomy.
References
- 1.Spechler SJ. Clinical practice. Barrett's Esophagus. N Engl J Med. 2002;346:836–842. doi: 10.1056/NEJMcp012118. [DOI] [PubMed] [Google Scholar]
- 2.Falk GW. Barrett's esophagus. Gastroenterology. 2002;122:1569–1591. doi: 10.1053/gast.2002.33427. [DOI] [PubMed] [Google Scholar]
- 3.Neumann CS, Cooper BT. 24 hour ambulatory oesophageal pH monitoring in uncomplicated Barrett's oesophagus. Gut. 1994;35:1352–1355. doi: 10.1136/gut.35.10.1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singh P, Taylor RH, Colin-Jones DG. Esophageal motor dysfunction and acid exposure in reflux esophagitis are more severe if Barrett's metaplasia is present. Am J Gastroenterol. 1994;89:349–356. [PubMed] [Google Scholar]
- 5.Gillen P, Keeling P, Byrne PJ, West AB, Hennessy TP. Experimental columnar metaplasia in the canine oesophagus. Br J Surg. 1988;75:113–115. doi: 10.1002/bjs.1800750208. [DOI] [PubMed] [Google Scholar]
- 6.Champion G, Richter JE, Vaezi MF, Singh S, Alexander R. Duodenogastroesophageal reflux: relationship to pH and importance in Barrett's esophagus. Gastroenterology. 1994;107:747–754. doi: 10.1016/0016-5085(94)90123-6. [DOI] [PubMed] [Google Scholar]
- 7.Vaezi MF, Richter JE. Role of acid and duodenogastroesophageal reflux in gastroesophageal reflux disease. Gastroenterology. 1996;111:1192–1199. doi: 10.1053/gast.1996.v111.pm8898632. [DOI] [PubMed] [Google Scholar]
- 8.Avidan B, Sonnenberg A, Schnell TG, Sontag SJ. Gastric surgery is not a risk for Barrett's esophagus or esophageal adenocarcinoma. Gastroenterology. 2001;121:1281–1285. doi: 10.1053/gast.2001.29587. [DOI] [PubMed] [Google Scholar]
- 9.Lieberman DA, Oehlke M, Helfand M Gastroenterology Outcomes Research Group in Endoscopy. Risk factors for Barrett's esophagus in community-based practice. GORGE consortium. Am J Gastroenterol. 1997;92:1293–1297. [PubMed] [Google Scholar]
- 10.Sampliner RE. Updated guidelines for the diagnosis, surveillance, and therapy of Barrett's esophagus. Am J Gastroenterol. 2002;97:1888–1895. doi: 10.1111/j.1572-0241.2002.05910.x. [DOI] [PubMed] [Google Scholar]
- 11.Pera M, Brito MJ, Poulsom R, et al. Duodenal-content reflux esophagitis induces the development of glandular metaplasia and adenosquamous carcinoma in rats. Carcinogenesis. 2000;21:1587–1591. [PubMed] [Google Scholar]
- 12.Vaezi MF, Richter JE. Contribution of acid and duodenogastro-oesophageal reflux to oesophageal mucosal injury and symptoms in partial gastrectomy patients [see comment] Gut. 1997;41:297–302. doi: 10.1136/gut.41.3.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nishimaki T, Watanabe K, Suzuki T, Hatakeyama K, Watanabe H. Early esophageal adenocarcinoma arising in a short segment of Barrett's mucosa after total gastrectomy. Am J Gastroenterol. 1996;91:1856–1857. [PubMed] [Google Scholar]
- 14.Sandvik AK, Halvorsen TB. Barrett's esophagus after total gastrectomy. J Clin Gastroenterol. 1988;10:587–588. doi: 10.1097/00004836-198810000-00023. [DOI] [PubMed] [Google Scholar]
- 15.Westhoff BC, Weston A, Cherian R, Sharma P. Development of Barrett's esophagus six months after total gastrectomy. Am J Gastroenterol. 2004;99:2271–2277. doi: 10.1111/j.1572-0241.2004.40249.x. [DOI] [PubMed] [Google Scholar]
- 16.Kim JH, Rhee PL, Lee JH, et al. Prevalence and risk factors of Barrett's esophagus in Korea. J Gastroenterol Hepatol. 2007;22:908–912. doi: 10.1111/j.1440-1746.2006.04448.x. [DOI] [PubMed] [Google Scholar]