Abstract
Black esophagus is a rare condition of the esophagus that manifests as endoscopic findings of black-colored esophageal mucosa, which is usually caused by acute esophageal necrosis. We report a case of alcoholic patient who developed black esophagus. The 85-year-old man was admitted to Severance Hospital due to copious hematemesis over 2 days. Upper gastrointestinal endoscopy showed black-colored mucosa in the distal esophagus. Endoscopic biopsies of the esophagus revealed necrotic tissue, without any viable cells. Follow-up upper gastrointestinal endoscopy performed after supportive care with a proton-pump inhibitor, sucralfate, and total parenteral nutrition resulted in the remarkable healing of the esophageal wall with no complications.
Keywords: Black esophagus, Necrosis, Alcohol abuse
INTRODUCTION
Black esophagus is a rare condition characterized by endoscopic findings of black-colored esophageal mucosa, associated with histologic evidence of extensive mucosal necrosis. Several etiologies have been suggested, including ischemia, severe viral infection, hypersensitivity to antibiotics, gastric outlet obstruction with gastro-esophageal reflux, and corrosive injury.1-5 Risk factors include old age, male gender, diabetes mellitus, hypertension, coronary artery disease, alcohol abuse, renal insufficiency, and advanced malignancies.6 However, the exact mechanism leading to black esophagus is still unknown. The most common symptoms of black esophagus are upper gastrointestinal bleeding: coffee-ground vomiting, hematemesis, or melena.
The reported incidence of black esophagus is very low, ranging from 0.0125% to 0.2%.2,7 A total of 88 patients were reported in the literature during the 40 years from 1965 to 2006 in English-language articles.6 In Korea, only one case of black esophagus with concomitant candidiasis after diabetic ketoacidosis has been reported.8 We report here a case of heavy alcoholics with black esophagus improved with supportive care.
CASE REPORT
An 85-year-old man was admitted to the emergency room with a history of hematemesis over 2 days. His medical history included hypertension, diabetes mellitus, alcohol abuse, a gastric ulcer, an old cerebral vascular accident, and benign prostatic hypertrophy. Medications included clopidogrel, ginkgo, necirgolin, nateglinide, alfuzocin, and amitriptyline.
On admission, he was afebrile, with a regular pulse of 100 bpm, a blood pressure of 150/80 mmHg, and a respiratory rate of 20 breaths/min. A digital rectal examination was negative for blood. A test irrigation with normal saline via a nasogastric tube was conducted and a brown liquid with old clots drained.
Laboratory results were as follows: white blood cell count 12,360/µL (neutrophils 88.6%), hemoglobin 18.6 g/dL, hematocrit 53.8%, platelets 209,000/µL, blood urea nitrogen 11.7 mg/dL, creatinine 1.6 mg/dL, alanine aminotransferase 136 IU/L, aspartate aminotransferase 55 IU/L, total bilirubin 2.9 mg/dL, direct bilirubin 1.6 mg/dL, gamma-glutamyltranspeptidase 418 IU/L, alkaline phosphatase 97 IU/L, sodium 130 mmol/L, potassium 2.9 mmol/L, serum glucose 347 mg/dL, prothrombin time 12.7 s, International Normalized Ratio 1.12, and activated partial thromboplastin time 31.0 s.
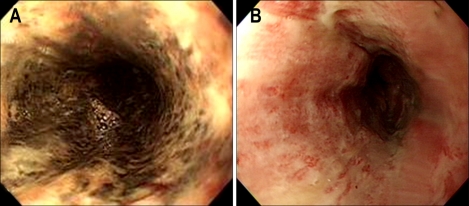
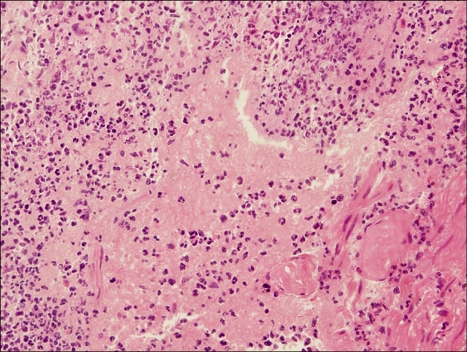
On the following day, upper gastrointestinal endoscopy revealed edematous mucosa with tiny whitish exudates in the proximal-to-mid esophagus, suggestive of diffuse esophageal candidiasis and black-colored mucosa in the lower esophagus (Fig. 1A). Additional findings included severe inflammation and multiple erosions on duodenal bulb. Endoscopic biopsies of the black-colored distal esophagus showed epithelial necrosis, with non-specific inflammatory exudates, and ulcerations without any viable cells (Fig. 2). Periodic acid-Schiff stain revealed no identifiable fungal hyphae. He was treated conservatively with a proton pump inhibitor, sucralfate, and total parenteral nutrition.
Fig. 1.
Endoscopic findings of the esophagus. (A) Black colored mucosa is observed in the lower esophagus. (B) Follow-up endoscopy after 8 days reveals nearly complete resolution of the black colored mucosa, with minimal mucosal edema and tiny whitish exudates remaining in the lower esophagus.
Fig. 2.
Microscopic findings. Biopsied mucosal tissue from the distal esophagus shows a tiny fragment of necrotic tissue, without any viable cells.
On day 8, a follow-up upper gastrointestinal endoscopy was performed. The tiny whitish exudates and edema of the mucosa remained throughout the esophagus. However, the black-colored mucosa of the lower esophagus had resolved (Fig. 1B). Endoscopic biopsies of the esophagus still showed ulceration with necrotic inflammatory exudates and granulation tissue. Immunohistochemical staining for cytomegalovirus was negative. He was discharged without complications.
DISCUSSION
Black esophagus was first reported in 1990 by Goldenberg et al.1 The reported incidence of black esophagus is very low, ranging from 0.0125% to 0.2%.2,7 Malignant melanoma, acanthosis nigricans, pseudomelanosis, melanosis, coal dust deposition, and corrosive ingestion can mimic the endoscopic appearance of black esophagus.9 However, the term 'black esophagus' most often represents acute esophageal necrosis.
Although the mechanism of acute esophageal necrosis is unclear, most authors have suggested ischemic injury as the most likely cause. Ischemia can be caused by hypotension or thrombosis.10,11 A case of acute esophageal necrosis caused by alcohol abuse has been reported.12 The authors suggested that low systemic perfusion, caused by severe alcohol lactic acidosis was the major cause.
In our case, risk factors including old age, male gender, diabetes mellitus, and hypertension with atherosclerotic vascular disease may have predisposed the patient to esophageal ischemia. However, the patient had neither a hypotensive event nor metabolic acidosis. To assess cardiac dysfunction, which can lead to low arterial flow and thrombogenic conditions, echocardiography was performed. However, there was no evidence of cardiac dysfunction.
Anatomically, the esophagus is a well-vascularized organ. The blood supply to the proximal esophagus is provided by the bilateral superior and inferior thyroid arteries and that to the mid esophagus is provided by direct arteries from the aorta. The distal esophagus has been reported to be less vascularized and more vulnerable to ischemic injury. However, all major arteries divide into minute branches, which penetrate into the submucosa to form an extensive interconnecting vascular network in the esophagus. Thus, ischemic injury alone may not be a leading mechanism of black esophagus.
Massive acid reflux can cause black esophagus.5 Massive and persistent esophageal exposure to gastric fluids leads to a decline in blood flow in the mucosa and submucosa of the esophagus. Black esophagus induced by severe vomiting in a healthy young man was reported.13 In this case, vomiting after alcohol abuse led to large amounts of gastric acid bathing the esophageal mucosa, damaging the mucosa through direct caustic injury, and decreasing the amount of blood flow to the mucosa and submucosa. A similar case of acute esophageal necrosis in an immunosuppressed patient with alcoholic hepatitis caused by gastroesophageal reflux has also been reported.14 Gastroesophageal reflux combined with hypoperfusion was thought to a key factor for the esophageal lesion in that case.
In our case, daily alcohol consumption was more than 100 gram. Alcohol ingestion has been reported to reduce lower esophageal sphincter pressure and esophageal peristalsis and increase acid exposure in the esophagus.15 Excessive drinking can cause irritation of the gastric mucosa and the accumulation of large volume of gastric secretions. This can disrupt the defense mechanism of the esophagus. In addition to a history of gastric ulcer, and severe duodenitis, multiple duodenal erosions were noted on upper gastrointestinal endoscopy. Thus, increased acid reflux, gastric stasis, and decreased mucosal protection are likely to be responsible for the development of acute esophageal necrosis associated with alcohol abuse.13,14
Severe viral or fungal infections such as cytomegalovirus, herpes simplex virus, and Candida albicans, can also be involved in the development of acute esophageal necrosis.3,6,9 However, immunohistochemical staining for cytomegalovirus and PAS staining for fungal infections were negative in this case.
The treatment of black esophagus is supportive care in most cases. Most authors recommend adequate hydration, the use of a proton pump inhibitor, sucralfate, and treating the esophageal infection, if present. Additionally, in our case, abstinence from alcohol which may have been an aggravating factor might be important.
The prognosis of black esophagus is typically poor and mortality depends on the underlying illness (older age, higher incidence of malignancy, three or more associated chronic conditions).9 Death secondary to esophageal necrosis occurs in less than 6% of cases.6 However, in our case, the esophageal lesions improved significantly in the gross appearance of the esophageal mucosa, without any complication, such as stricture.
In conclusion, we report a rare case of black esophagus in an elderly patient with several comorbid conditions predisposing to esophageal ischemia and a history of alcohol abuse. The patient was successfully treated conservatively, with hydration, acid suppression, and parenteral nutrition.
ACKNOWLEDGEMENT
The author thanks Sung Won Hong for critical comments on study and support.
The English in this document has been checked by at least two professional editors, both native speakers of English. For a certificate, see: http://www.textcheck.com/cgi-bin/certificate.cgi?id=T2oSZp
References
- 1.Goldenberg SP, Wain SL, Marignani P. Acute necrotizing esophagitis. Gastroenterology. 1990;98:493–496. doi: 10.1016/0016-5085(90)90844-q. [DOI] [PubMed] [Google Scholar]
- 2.Ben Soussan E, Savoye G, Hochain P, et al. Acute esophageal necrosis: 1-year prospective study. Gastrointest Endosc. 2002;56:213–217. doi: 10.1016/s0016-5107(02)70180-6. [DOI] [PubMed] [Google Scholar]
- 3.Cattan P, Cuillerier E, Cellier C, et al. Black esophagus associated with herpes esophagitis. Gastroinest Endosc. 1999;49:105–107. doi: 10.1016/s0016-5107(99)70455-4. [DOI] [PubMed] [Google Scholar]
- 4.Mangan TF, Colly AT, Wytock DH. Antibiotic-associated acute necrotizing esophagitis. Gastroenterology. 1990;99:900. doi: 10.1016/0016-5085(90)90997-f. [DOI] [PubMed] [Google Scholar]
- 5.Reichart M, Busch OR, Bruno MJ, Van Lanschot JJ. Black esophagus: a view in the dark. Dis Esophagus. 2000;13:311–313. doi: 10.1046/j.1442-2050.2000.00126.x. [DOI] [PubMed] [Google Scholar]
- 6.Gurvits GE, Shapsis A, Lau N, Gualtieri N, Robilotti JG. Acute esophageal necrosis: a rare syndrome. J Gastroenterol. 2007;42:29–38. doi: 10.1007/s00535-006-1974-z. [DOI] [PubMed] [Google Scholar]
- 7.Moreto M, Ojembarrena E, Zaballa M, Tanago JG, Ibanez S. Idiopathic acute esophageal necrosis: not necessarily a terminal event. Endoscopy. 1993;25:534. doi: 10.1055/s-2007-1009121. [DOI] [PubMed] [Google Scholar]
- 8.Kim YH, Choi SY. Black esophagus with concomittent candidiasis developed after diabetic ketoacidosis. World J Gastroenterol. 2007;13:5662–5663. doi: 10.3748/wjg.v13.i42.5662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grudell AB, Mueller PS, Viggiano TR. Black esophagus: report of six cases and review of the literature. Dis Esophagus. 2006;19:105–110. doi: 10.1111/j.1442-2050.2006.00549.x. [DOI] [PubMed] [Google Scholar]
- 10.Haviv YS, Reinus C, Zimmerman J. "Black esophagus": a rare complication of shock. Am J Gastroenterol. 1996;91:2432–2434. [PubMed] [Google Scholar]
- 11.Casella G, Perego D, Corti G, et al. Black esophagus: should it be considered an unfavorable prognostic factor? Dis Esophagus. 2001;14:166–168. doi: 10.1046/j.1442-2050.2001.00177.x. [DOI] [PubMed] [Google Scholar]
- 12.Endo T, Sakamoto J, Sato K, et al. Acute esophageal necrosis caused by alcohol abuse. World J Gastroenterol. 2005;11:5568–5570. doi: 10.3748/wjg.v11.i35.5568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Katsinelos P, Pilpilidis I, Dimiropoulos S, et al. Black esophagus induced by severe vomiting in a healthy young man. Surg Endosc. 2003;17:521. doi: 10.1007/s00464-002-4248-8. [DOI] [PubMed] [Google Scholar]
- 14.Saftoui A, Cazacu S, Kruse A, et al. Acute esophageal necrosis associated with alcoholic hepatitis: is it black or is it white? Endoscopy. 2005;37:268–271. doi: 10.1055/s-2005-860995. [DOI] [PubMed] [Google Scholar]
- 15.Watannabe Y, Fujiwara Y, Shiba M, et al. Cigarette smoking and alcohol consumption associated with gastro-oesophageal reflux disease in Japanese men. Scand J Gastroenterol. 2003;8:807–811. doi: 10.1080/00365520310004506. [DOI] [PubMed] [Google Scholar]