Abstract
A 45-year-old female with known situs inversus totalis presented with colicky pain in the left upper abdominal quadrant. The laboratory parameters showed elevated neutrophils and a bilirubin level of 2 mg/dL. CT confirmed situs inversus totalis and dilatation of the intra- and extrahepatic ducts with a 10-mm common bile duct (CBD) stone and a 10-mm gallstone. She underwent papillary dilatation using a radial expansion balloon after sphincterotomy, after which the CBD stone was removed with a basket and balloon. There were no complications, such as bleeding, pancreatitis, or perforation. It might be reasonable to attempt a "partial" biliary endoscopic sphincterotomy followed by a large-balloon dilator in patients with concomitant distal bile duct, papillary stenosis, or altered anatomy (e.g., periampullary diverticulum, Billroth II anatomy). However, when performing an "adequate" biliary endoscopic sphincterotomy this is technically difficult, or in some cases even impossible, and is associated with a higher risk of complications. This paper further expands on the application of these techniques and shows that a papillary balloon dilatation after endoscopic sphincterotomy is a safe, easy, and effective technique for removing bile-duct stones in a patient with situs inversus totalis.
Keywords: Situs inversus totalis, Endoscopic sphincterotomy, Large-balloon dilator, Bile-duct stone
INTRODUCTION
Situs inversus is a rare condition of anatomical alteration resulting in a reversal of visceral organs.1 Endoscopic procedures are difficult in patients with situs inversus because of the left-right reversal of the viscera. Endoscopic sphincterotomy (EST) is standard procedure for the removal of bile duct stones.2
There is growing evidence that suggests that large-balloon dilation (LBD), in conjunction with sphincterotomy can be considered as an alternative therapy in patients with difficult stones such as large stones, distal bile duct stenosis, or altered anatomy (e.g., periampullary diverticulum, Billroth II anatomy).3-10
We report the case of a 45-year-old female with known situs inversus totalis who successfully had stone removed using a minor EST and a large-balloon dilation.
CASE REPORT
A 45-year-old female with known situs inversus was admitted to our emergency department with abdominal pain located in the left upper quadrant. The pain was colicky and associated with nausea, vomiting, fever (38.5℃) and jaundice. A physical examination revealed pronounced tenderness in the left upper abdominal quadrant.
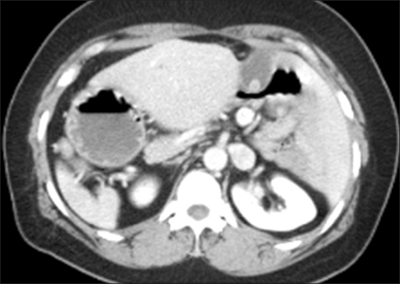
Laboratory tests showed: white blood cell count 20,940/mL, total bilirubin 2.0 mg/d, AST 21 IU/L, ALT 57 IU/L, ALP 400 IU/L, CRP 11.39 mg/dL. All other parameters were in the normal range. An abdominal computed tomography confirmed the situs inversus and showed a dilatation of the intra- and extrahepatic ducts with a CBD stone and a GB stone (Fig. 1).
Fig. 1.
Abdominal CT showing the liver and the gallbladder in the left abdomen. Common bile duct and gallstones are also noted.
After conscious sedation and prophylatic antibiotics, an ERCP was performed with a side-viewing endoscope (Olympus JF-240). The patient was in the usual prone position with the endoscopist at the right side of table. In the stomach we turned the endoscope 180 degrees to the right and reached the second portion of the duodenum. Papilla was maintained in the correct position retrieving the instrument in the short position.
The cholangiography confirmed dilatation of the intraand extrahepatic ducts with a 10 mm sized CBD stone and a 10 mm sized GB stone (Fig. 2).
Fig. 2.
Cholangiography and common bile duct cannulation with an instrument.
The length of the sphincterotomy incision was limited to a third of the major EST measured from the orifice of the papilla (a limited EST). A balloon catheter (CRE balloon; Boston Scientific, Natick, MA, USA) was passed through the sphincterotomy site. After positioning the middle portion of the deflated balloon at the biliary sphincter, the balloon was then gradually filled with the diluted contrast medium, under endoscopic and fluoroscopic guidance (Fig. 3). Pressure was applied until the waist of the balloon gradually disappeared, after which the balloon was maintained inflated for another 60 seconds. The diameter used was 12 mm. The stone was retrieved from the bile duct with conventional methods in one session (Fig. 4). There were no complications, such as bleeding, pancreatitis, or perforation.
Fig. 3.
Large-balloon dilatation under fluoroscopic guidance.
Fig. 4.
Stone extraction with a Dormia basket.
DISCUSSION
An endoscopic sphincterotomy is the procedure of choice for patients with bile duct stones.2 However, in patients with altered anatomy (e.g., periampullary diverticulum, Billroth II anatomy), performing an "adequate" biliary endoscopic sphincterotomy is technically difficult or impossible and is associated with a higher risk of complications such as bleeding and perforation.11
There were many studies on the use of biliary endoscopic sphincterotomy in conjunction with large-balloon (12-20 mm) dilation to treat patients with difficult stones.4,7,8,10,12-14 This technique was first reported by Ersoz et al. in 2003.7 Although there have been some fatal complications, all the current data has shown encouraging results.
The cause of situs inversus is unknown. There is no evidence that situs inversus predisposes to bile duct stones, but it may be a cause of diagnostic confusion. A delay of the diagnosis could be caused when patients with unknown situs inversus complain of left upper abdominal pain.
Endoscopic procedures are difficult in patients with situs inversus due to the left-right reversal. Traditionally, the reversal of the position of the endoscopist in relation to the patient is suggested to overcome the anatomical difficulty.15 In our case, we succeeded to reach the second portion of the duodenum despite maintaining the patient in the prone position with the endoscopist on the right side of the table.
In addition to the difficulty of approching the ampulla, EST is more frequently associated with complications such as bleeding and perforation, when the patient has altered anatomy. Also, if these complications occur, it is difficult to treat them endoscopically or surgically because of the difficult orientation of the mirror-image anatomy, the use of the left hand of the operator, and the position of the operator. Endoscopic balloon dilation (EBD) is technically easier than EST and less post-procedural bleeding occurs. Furthermore, delayed bleeding has been reported following EST but it rarely occurs after EBD in patients with coagulopathy.16,17 The cutting direction of sphincterotome in EST is sometimes technically difficult to control, particularly in patients with altered anatomy including situs inversus. On the contrary, EBD is easy to handle in the above condition and it is a safe procedure in less experienced hands. Moreover, while sphincterotomy is difficult without an elevator of side-viewing endoscope, the use of a forward-viewing or side-viewing endoscope does not affect the feasibility of the technique of EBD. Therefore, EBD is considered an alternative in patients with coagulation disorders and in cases of patients of atypical anatomy.
The most frequent complication of EBD is acute pancreatitis, with an incidence ranging from 4-35%, depending on the series. Therefore, balloon size is limited to 8 or 10 mm and EBD does not enlarge the biliary sphincter enough to remove large bile-duct stones. However, by performing a LBD in a limited EST, the biliary opening is enlarged to a greater extent compared with an EST or EBD alone. In contrast to balloon dilation in patients with an intact sphincter, balloon dilation in patients with an incised papilla enables the dilation to proceed towards the incision rather than in a circumferential fashion, minimizing the chances of acute pancreatitis.
We performed the papillary dilation using a radial expansion balloon after a limited sphincterotomy and then the CBD stone was removed with basket and balloon. There were no complications, such as bleeding, pancreatitis, or perforation.
In conclusion, this report shows that large-balloon dilation after a limited sphincterotomy seems to be a safe, easy, and effective technique for removing bile-duct stones in a patient with situs inversus.
References
- 1.Gastrointestinal: situs inversus viscerum. J Gastroenterol Hepatol. 2002;17:1329. [PubMed] [Google Scholar]
- 2.Binmoeller KF, Schafer TW. Endoscopic management of bile duct stones. J Clin Gastroenterol. 2001;32:106–118. doi: 10.1097/00004836-200102000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Misra SP, Dwivedi M. Large-diameter balloon dilation after endoscopic sphincterotomy for removal of difficult bile duct stones. Endoscopy. 2008;40:209–213. doi: 10.1055/s-2007-967040. [DOI] [PubMed] [Google Scholar]
- 4.Maydeo A, Bhandari S. Balloon sphincteroplasty for removing difficult bile duct stones. Endoscopy. 2007;39:958–961. doi: 10.1055/s-2007-966784. [DOI] [PubMed] [Google Scholar]
- 5.Heo JH, Kang DH, Jung HJ, et al. Endoscopic sphincterotomy plus large-balloon dilation versus endoscopic sphincterotomy for removal of bile-duct stones. Gastrointest Endosc. 2007;66:720–726. doi: 10.1016/j.gie.2007.02.033. [DOI] [PubMed] [Google Scholar]
- 6.Attasaranya S, Sherman S. Balloon dilation of the papilla after sphincterotomy: rescue therapy for difficult bile duct stones. Endoscopy. 2007;39:1023–1025. doi: 10.1055/s-2007-966922. [DOI] [PubMed] [Google Scholar]
- 7.Ersoz G, Tekesin O, Ozutemiz AO, Gunsar F. Biliary sphincterotomy plus dilation with a large balloon for bile duct stones that are difficult to extract. Gastrointest Endosc. 2003;57:156–159. doi: 10.1067/mge.2003.52. [DOI] [PubMed] [Google Scholar]
- 8.Minami A, Hirose S, Nomoto T, Hayakawa S. Small sphincterotomy combined with papillary dilation with large balloon permits retrieval of large stones without mechanical lithotripsy. World J Gastroenterol. 2007;13:2179–2182. doi: 10.3748/wjg.v13.i15.2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bergman JJ, van Berkel AM, Bruno MJ, et al. A randomized trial of endoscopic balloon dilation and endoscopic sphincterotomy for removal of bile duct stones in patients with a prior Billroth II gastrectomy. Gastrointest Endosc. 2001;53:19–26. doi: 10.1067/mge.2001.110454. [DOI] [PubMed] [Google Scholar]
- 10.Kim GH, Kang DH, Song GA, et al. Endoscopic removal of bile-duct stones by using a rotatable papillotome and a large-balloon dilator in patients with a Billroth II gastrectomy (with video) Gastrointest Endosc. 2008;67:1134–1138. doi: 10.1016/j.gie.2007.12.016. [DOI] [PubMed] [Google Scholar]
- 11.Mugica F, Urdapilleta G, Castiella A, et al. Selective sphincteroplasty of the papilla in cases at risk due to atypical anatomy. World J Gastroenterol. 2007;13:3106–3111. doi: 10.3748/wjg.v13.i22.3106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yoo B, Kim J, Jung J, et al. Large balloon sphincteroplasty along with or without sphincterotomy in patients with large extrahepatic bile duct stones: multi center study. Gastrointest Endosc. 2007;65:AB97. [Google Scholar]
- 13.Attasaranya S, Cheon YK, Mchenry L, et al. Large-diameter papillary balloon dilation to aid in endoscopic bile duct stone removal: a multicenter series. Gastrointest Endosc. 2007;65:AB214. doi: 10.1016/j.gie.2007.08.047. [DOI] [PubMed] [Google Scholar]
- 14.Espinel J, Pinedo E, Olcoz JL. Large hydrostatic balloon for choledocolithiasis. Rev Esp Enferm Dig. 2007;99:33–38. doi: 10.4321/s1130-01082007000100007. [DOI] [PubMed] [Google Scholar]
- 15.Pathak KA, Khanna R, Khanna NN. Situs inversus with cholelithiasis. J Postgrad Med. 1995;41:45–46. [PubMed] [Google Scholar]
- 16.Sherman S, Hawes RH, Nisi R, Lehman GA. Endoscopic sphincterotomy-induced hemorrhage: treatment with multipolar electrocoagulation. Gastrointest Endosc. 1992;38:123–126. doi: 10.1016/s0016-5107(92)70375-7. [DOI] [PubMed] [Google Scholar]
- 17.Gholson CF, Favrot D, Vickers B, Dies D, Wilder W. Delayed hemorrhage following endoscopic retrograde sphincterotomy for choledocholithiasis. Dig Dis Sci. 1996;41:831–834. doi: 10.1007/BF02091518. [DOI] [PubMed] [Google Scholar]