Abstract
Background/Aims
Colonoscopy training programs and the minimal experience with colonoscopy required to be considered technically competent are not well established. The aim of this study was to determine the colonoscopy learning curves and factors associated with this difficult procedure at a single center.
Methods
A total of 3,243 colonoscopies were performed by 12 first-year gastroenterology fellows, and various clinical factors were assessed prospectively for 22 months. Acquisition of competence (success rate) was evaluated based on two objective criteria: (i) the adjusted completion rate (>90%) and (ii) cecal intubation time (<20 minutes).
Results
The overall success rate in reaching the cecum in less than 20 minutes was 72.8%. The cecal intubation time was 9.34±4.13 minutes (mean±SD). Trainees' skill at performing cecal intubation in <20 minutes reached the requisite standard of competence after 200 procedures. Cecal intubation time decreased significantly from 11.3 to 9.4 minutes after 100 procedures and improved continuously thereafter. Female patients and advanced patient age (over 60 years) were associated with prolonged cecal intubation time (>20 minutes). Surgery of the uterus and ovaries was significantly correlated with delayed cecal intubation time, but not after sufficient colonoscopy experience.
Conclusions
The minimum number of procedures to reach technical competence was 200. The cecal intubation time was longer in female and older patients.
Keywords: Colonoscopy, Learning curves, Fellows
INTRODUCTION
The incidence of colorectal cancer throughout in South Korea has been increasing over the last 25 years, making colonoscopy a useful tool for the diagnosis, treatment and screening of colorectal cancer. Expertise in colonoscopy can be judged by technical aspects, such as ease and completeness of insertion, precision of observation, and minimal degree of patient discomfort during the procedure. Various factors have been implicated in affecting the success of a colonoscopy. These factors include gender, age, obesity, bowel preparation, and a history of hysterectomy, abdominal surgery, colorectal resection, complicated diverticular disease, and/or peritonitis.1-3 Only a few studies have been reported on colonoscopy training programs, especially the first-year of Gastrointestinal (GI) fellowship training, in Korea.4 Thus, the aim of this study was to evaluate the learning curves of a colonoscopy training program and determine the factors that affect the technical competence of colonoscopy.
MATERIALS AND METHODS
1. Study patients
A prospective study was performed on consecutive patients undergoing elective colonoscopy at Seoul National University Bundang Hospital from March 2007 to December 2008. A total of 12 first-year GI fellows participated in this study. Patients were excluded for the following: (i) emergency colonoscopy, (ii) colon obstruction, (iii) history of colorectal operations, (iv) poor preparation, especially, when hard impacted stool was found in the rectosigmoid area, and (v) when the supervisor had to intervene within 20 minutes. The study protocol was approved by the Ethical Committee at Seoul National University Bundang Hospital. Patients provided written informed consent before participation in the study.
2. Colonoscopy learning
This training program of colonoscopy was processed under the condition that patients did not receive discomfort. Initially, the trainees learned the endoscopy skill through practicing upper endoscopy and sigmoidoscopy. Then, colonoscopy training began with observation of colonoscopies performed by the staff for 20 cases. The GI fellows started performing colonoscopies without the assistance of senior fellows or GI staff after the observation period. However, if they were uncomfortable for this process then the staff waited until they were ready for colonoscopy by themselves. The instructor allowed the trainees 20 minutes to reach the cecum, under the conditions that the procedure was being performed safely and comfortably. However, the supervisor had intervened the procedure in several occasions; (i) if the trainee could not reach splenic flexure within 20 minutes, (ii) if the trainee could not advance the colonoscope for several minutes at the same site, (iii) if the patients asked the procedure performed by the supervisor, or (iv) the trainee felt uncomfortable about the procedure.
Cecal intubation was documented by photographing the identified cecal landmarks such as appendiceal orifice and the ileocecal valve. Patient age, gender, body mass index (BMI), and surgical history were recorded before the procedure by nurses. When the patients were ready for the colonoscopy, the trainee started the insertion, and the cecal intubation time was recorded by the nurse who assisted in the procedure. Positional change and abdominal pressure were found to be important factors for successful cecal intubation, especially during the passage of the rectosigmoid area and hepatic flexure. However, it was not performed routinely. After cecal intubation, the colon was examined on withdrawal by the staff; biopsies and/or treatment were performed as needed.
3. Colonoscopy examination
Bowel cleaning was accomplished by drinking 4 L of polyethyleneglycol-electrolyte solution (Colonlyte; Taejun Co., Seoul, Korea). Patients received intravenous sedatives (midazolam; Bugwang, Seoul, Korea) before the procedure if requested. In addition, pethidine (25 mg) was administered intramuscularly before the procedure. Most patients received antispasmodic drug (Buscopan; Boehringer Ingelheim Co., Seoul, Korea) with intravenously or intramusculary before the procedure except which some contraindicated patients; for examples, uncontrolled hypertension, glaucoma, severe paralytic ileus and severe heart disease, etc. Additional medication was given as needed All colonoscopies were performed with an Olympus CF-240 or CF-260 video colonoscope (Olympus Optical Co., Ltd., Tokyo, Japan).
4. Statistical analysis
All analyses were calculated with the statistical program SPSS version 13.0 (SPSS Inc., Chicago, IL, USA). The learning curves, for the fellows, were calculated in consecutive blocks of 50 procedures. Categorical data were assessed with the chi-square test. All continuous variables were expressed by means and analyzed using the Student's t-test or Fisher's extract method, where appropriate. A one-way variance analysis was used to compare the success rates and the time required for successful cecal intubation among the consecutive blocks of 50 procedures. Multivariate analysis was used to evaluate the independent impact on the prolonged cecal intubation time (20 minutes or more). A p-value <0.05 was considered significant.
RESULTS
1. Demographic data
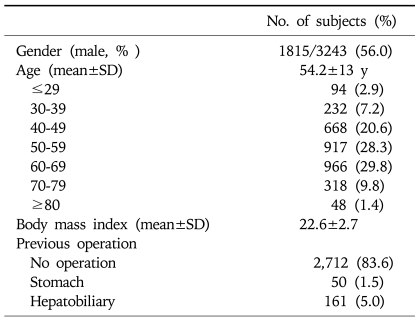
During 22 months from March 2007 to December 2008, 3,243 colonoscopies were enrolled in the study. The mean age of the patients was 54.2±13.0 years, and the mean BMI was 22.6±2.7. The included subjects were 1,815 men (56.0%) and 1,428 women (44.0%). There were 2,712 patients (83.6%) with no history of surgery. That is, 1.5%, 5.0% had stomach and hepatobiliary surgery, respectively. In addition, 5.5%, 2.6% and 4.7% had undergone surgery of the female genital organs, a Caesarian section delivery and appendectomy. One hundred and twenty five patients (12.2%) had a history of a prior polypectomy by colonoscopy. The demographic data are summarized in Table 1.
Table 1.
Baseline Characteristics Relative to Various Factors
SD, standard deviation.
2. Learning curve
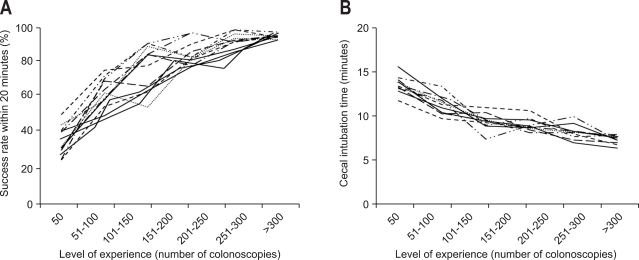
The overall success rate, over the 22 months, in reaching the cecum in less than 20 minutes was 72.8%. The trainees' learning curves were calculated in consecutive blocks of 50 procedures. The trainees' skill at performing cecal intubation in less than 20 minutes improved rapidly and significantly within the first three blocks. That is, the average success rate within 20 minutes was 37% (≤50), 64% (51-100), 77% (101-150), 85% (151-200), 94% (201-250), 95% (251-300), and 94% (>300), in reaching the requisite standard of competence after 200 procedures (Table 2, Fig. 1A).
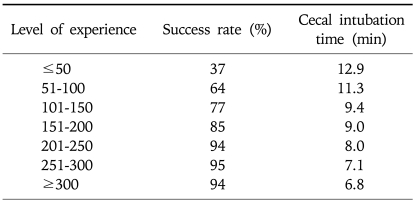
Table 2.
Correlation between Level of Experience, Success Rate (Successful Cecal Intubation within 20 Minutes), and Cecal Intubation Time
Fig. 1.
Learning curve. (A) Correlation between the success rate and level of experience (successful cecal intubation within 20 minutes) for 12 first-year gastroenterology fellows. (B) Inverse correlation between cecal intubation time and level of experience for 12 first-year gastroenterology fellows.
3. Cecal intubation time
The mean cecal intubation time, over the 22 months, was 9.34±4.13 minutes. Time to cecal intubation decreased significantly from 11.3 to 9.4 minutes after 100 procedures and continuously improved thereafter (12.9, 11.3, 9.4, 9.0, 8.0, 7.1, and 6.8 minutes, for every 50 consecutive blocks (Table 2, Fig. 1B). An inverse correlation was noted between the cecal intubation time and success rate. Time to cecal intubation continued to improve.
4. Unsuccessful and prolonged cecal intubation
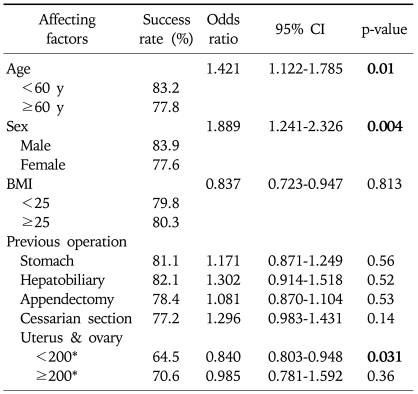
Mutivariate analysis was performed to evaluate factors affecting the cecal intubation. Female and age (over 60 years) were associated with a prolonged cecal intubation time (>20 minutes). However, other factors, BMI and body weight, were not associated with a prolonged cecal intubation time. History of prior surgery, except of the uterus and ovaries, was not associated with the cecal intubation time. A history of uterine and ovarian surgery significantly correlated with a delayed cecal intubation time when the number of cases was below 200; however, the significance disappeared when the trainees accumulated sufficient experience (Table 3). During this program, there was no serious complication such as perforation. This could be related with the caution that the GI staff performed colonoscopy by themselves instead of GI fellow in case of patients with poor conditions to avoid any trouble.
Table 3.
Factors Affecting the Success Rate within 20 Minutes by Multivariate Analysis
Bold figures indicate statistical significance.
*Number of colonoscopies.
DISCUSSION
Colonoscopy and polypectomy have effectively reduced the incidence of colorectal cancer.5,6 However, considerable training and experience is required for optimal performance of a colonoscopy. It is not always possible to reach the cecum even in the hands of an expert.7 Reports from the 1990s indicate that cecal intubation rates above 90% are consistently achieved by experienced colonoscopists; rates above 90% are the goal of colonoscopy training programs.8,9 For screening of asymptomatic persons, cecal intubation rates of 97-99% have been consistently achieved. Thus, >90% is the overall appropriate target for cecal intubation, and a rate >95% should be achievable for screening examinations.8,10
To achieve competency for colonoscopy procedures, at least 100-200 procedures have been reported to be required.4,11,12 A recent study of GI trainees in Korea, showed that the success rate significantly improved and reached the requisite standard competence (>90%) after 150 procedures.4; which is less than the 200 needed in our study. These differences might by explained by the following. First, our first year GI fellows had a short observation time with 20 cases. Second, procedures done by the first year GI fellows did not have senior GI fellows or GI staff available for instruction. If the instructor taught or advised the trainees during the procedure, the learning curve might have reached the level if competence in a shorter time. Previous studies usually were performed in multi centers, where the endoscopic training systems and situations are different with others, suggesting that the data could be heterogenous. However, our data was collected at a single center; our endoscopic training system and the situations reflect the learning curves of first year GI trainees in a general hospital.
Previous studies have shown that colonoscopy is significantly more difficult in women than men.7,13,14; which was also demonstrated in our study. Explanations for this difference include that the colon is longer in women than in men, previous gynecologic surgery and unknown anatomic variations. In addition, cecal intubation was prolonged and more difficult in patients that were older.3,14,15 Similarly, older aged patients, especially over 60 years, had significantly delayed cecal intubation time in the present study. However, contrary to previous reports, a significant difference in the cecal intubation time was not found according to the body weight, BMI, history of abdominal surgery or Caesarian section delivery. Instead, surgery of the uterus and/or ovaries initially showed a significant correlation with delayed cecal intubation; however, this difference disappeared after sufficient experience with ≥200 colonoscopies.
The limitation of this study was not including reason for the colonoscopy, bowel preparation status and findings such as polyps, cancer and inflammation in the analysis. A further study is required to include these parameters in the evaluation of training programs.
In conclusion, our data showed that the minimum number of procedures needed to reach technical competence for colonoscopy is more than 200 cases. Cecal intubation time was prolonged in women, and older aged patients. Prior uterine and/or ovarian surgery initially affected the cecal intubation time; however, after achieving competency this was no longer the case.
ACKNOWLEDGEMENTS
None of the authors had/have conflicts of interest that potentially influence the described research.
References
- 1.Oh SY, Sohn CI, Sung IK, et al. Factors affecting the technical difficulty of colonoscopy. Hepatogastroenterology. 2007;54:1403–1406. [PubMed] [Google Scholar]
- 2.Zuber-Jerger I, Endlicher E, Gelbmann CM. Factors affecting cecal and ileal intubation time in colonoscopy. Med Klin (Munich) 2008;103:477–481. doi: 10.1007/s00063-008-1071-6. [DOI] [PubMed] [Google Scholar]
- 3.Shah HA, Paszat LF, Saskin R, Stukel TA, Rabeneck L. Factors associated with incomplete colonoscopy: a population-based study. Gastroenterology. 2007;132:2297–2303. doi: 10.1053/j.gastro.2007.03.032. [DOI] [PubMed] [Google Scholar]
- 4.Lee SH, Chung IK, Kim SJ, et al. An adequate level of training for technical competence in screening and diagnostic colonoscopy: a prospective multicenter evaluation of the learning curve. Gastrointest Endosc. 2008;67:683–689. doi: 10.1016/j.gie.2007.10.018. [DOI] [PubMed] [Google Scholar]
- 5.Winawer SJ, Zauber AG, Ho MN, et al. Prevention of colorectal cancer by colonoscopic polypectomy: the National Polyp Study Workgroup. N Engl J Med. 1993;329:1977–1981. doi: 10.1056/NEJM199312303292701. [DOI] [PubMed] [Google Scholar]
- 6.Citarda F, Tomaselli G, Capocaccia R, Barcherini S, Crespi M. Efficacy in standard clinical practice of colonoscopic polypectomy in reducing colorectal cancer incidence. Gut. 2001;48:812–815. doi: 10.1136/gut.48.6.812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Waye JD, Bashkoff E. Total colonoscopy: is it always possible? Gastrointest Endosc. 1991;37:152–154. doi: 10.1016/s0016-5107(91)70674-3. [DOI] [PubMed] [Google Scholar]
- 8.Lieberman DA, Faigel DO, Logan JR, et al. Assessment of the quality of colonoscopy reports: results from a multicenter consortium. Gastrointest Endosc. 2009;69:645–653. doi: 10.1016/j.gie.2008.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marshall JB, Barthel JS. The frequency of total colonoscopy and terminal ileal intubation in the 1990s. Gastrointest Endosc. 1993;39:518–520. doi: 10.1016/s0016-5107(93)70162-5. [DOI] [PubMed] [Google Scholar]
- 10.Bair D, Pham J, Seaton MB, Arya N, Pryce M, Seaton TL. The quality of screening colonoscopies in an office-based endoscopy clinic. Can J Gastroenterol. 2009;23:41–47. doi: 10.1155/2009/831029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guidelines for. American Society for Gastrointestinal Endoscopy. Gastrointest Endosc. 1998;48:679–682. doi: 10.1016/s0016-5107(98)70059-8. [DOI] [PubMed] [Google Scholar]
- 12.Cass OW, Freeman ML, Peine CJ, Zera RT, Onstad GR. Objective evaluation of endoscopy skills during training. Ann Intern Med. 1993;118:40–44. doi: 10.7326/0003-4819-118-1-199301010-00008. [DOI] [PubMed] [Google Scholar]
- 13.Hull T, Church JM. Colonoscopy: how difficult, how painful? Surg Endosc. 1994;8:784–787. doi: 10.1007/BF00593441. [DOI] [PubMed] [Google Scholar]
- 14.Church JM. Complete colonoscopy: how often? And if not, why not? Am J Gastroenterol. 1994;89:556–560. [PubMed] [Google Scholar]
- 15.Anderson JC, Messina CR, Cohn W, et al. Factors predictive of difficult colonoscopy. Gastrointest Endosc. 2001;54:558–562. doi: 10.1067/mge.2001.118950. [DOI] [PubMed] [Google Scholar]