Abstract
Inflammatory bowel disease (IBD) describes chronic inflammatory disease of the intestines and has a variable course; Crohn's disease and ulcerative colitis comprise the two main forms of the condition. Although IBD occurs worldwide, its epidemiologic and clinical characteristics vary depending upon the geographic location and the ethnicity of the population. Identifying the characteristic features of IBD in populations living in different geographical locations and with different ethnicities may provide significant clues about its etiology and pathophysiology, which in turn may be helpful in the development of more appropriate treatment strategies for IBD for these different populations. Therefore, it is important for each country and region to evaluate critically the epidemiology, genomics, and clinical characteristics of IBD among its own population. We have performed a critical review of the recent data in Korea, and describe herein the current epidemiologic and genotypic status, as well as the clinical manifestations and therapeutic responses of IBD that are unique to Korean patients.
Keywords: Inflammatory bowel diseases, Crohn's disease, Ulcerative colitis, Korea
INTRODUCTION
Inflammatory bowel disease (IBD) is a chronic relapsing inflammatory disorder of the bowel, consisting mainly of Crohn's disease (CD) and ulcerative colitis (UC). The incidence of IBD has been rising not only in Western countries, but also in Asia, including Korea.1 Intriguingly, the characteristics of Western and Asian IBD patients differ in epidemiology, phenotype and genetic susceptibility.2-7 Evaluating these geographically unique features may provide substantial clues for identifying the pathophysiology and the etiology of IBD. However, such efforts have been challenging in most Asian countries, where there are lack of population-based registries, limited access to health care facilities, limited availability of diagnostic devices, and the occurrence of infectious diseases that mimic IBD, which hindered the accurate assessment of the incidence and the prevalence, the risk factors and the clinical characteristics of IBD.8 Until recently, only Japan has been able to report the reliable data, as it has the accessible and efficient health care system and maintains a national IBD registry under the Ministry of Health, Labor and Welfare.3 In Korea, the Korean Association for the Study of Intestinal Diseases (KASID) has recently taken a leading role in establishing the organizational structural bases for investigating IBD and has performed a series of nationwide studies.1,9,10 Korea has a relatively small nation of territory and the population is ethnically homogeneous. Members of KASID from each province of the nation participate to perform multicenter studies and patients with IBD have been registered by members of KASID.1,9 This review will describe the updated data on Korean IBD patients based on the recent publications.1,8,11-20
EPIDEMIOLOGY
Despite the advances in scientific technologies used to study IBD, its etiology and pathogenesis remain unclear. Traditionally, it has generally been thought that IBD occurs predominantly in the industrialized Western countries. However, as many other parts of the world including Asia, South America and Eastern Europe became industrialized since the middle of the last century, the incidence and the prevalence of IBD in these areas increased dramatically, suggesting that urbanization may be a risk factor for IBD.2,3,8,21-27 On the other hand, in Western Europe and North America, the incidence and the prevalence of IBD have stabilized or only slightly increased over time.28-31
In Korea, the incidence and prevalence of CD and UC are low compared to those of Western countries, but are increasing rapidly. According to a recent update on the descriptive epidemiology of IBD in Korea1 based on the population-based data from an urban district in Seoul, the mean annual incidence rates of CD and UC increased from 0.05 to 0.34 per 100,000 inhabitants in 1986-1990, and from 1.34 to 3.08 per 100,000 inhabitants in 2001-2005, respectively. The adjusted prevalence rates of CD and UC per 100,000 inhabitants were 11.24 (95% CI, 9.29-13.18) and 30.87 (95% CI, 27.47-34.27), respectively. In addition, it was observed that the ratio of the incidence rates of UC to CD was decreasing in Korea, indicating that CD showed a trend of more accelerated incidence rate compared to UC. This finding is similar to that observed in many Western countries.28,32,33 Male predominance in the prevalence rate of CD was observed in the Korean population, a finding similar to those reported in the recent studies from China2 and Japan34 while the incidence of CD in females is predominant or equal to that in males in Western countries.28,32
DIAGNOSIS
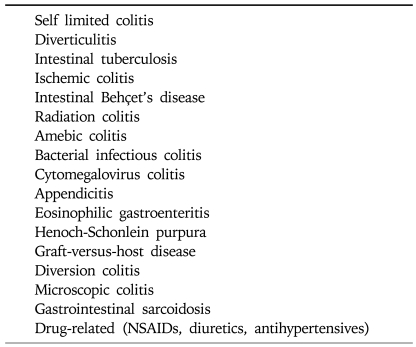
Regarding the diagnosis of IBD, two factors should be considered: first, distinguishing IBD patients from alternative inflammatory disease patients and secondly, correctly differentiating between UC and CD.35 Before establishing a diagnosis of IBD, other various forms of intestinal inflammation with identifiable causes should be excluded using relevant history, careful physical examination, prudent laboratory tests, and thorough review of the radiographic, endoscopic and pathologic data. The differential diagnosis of intestinal inflammation is outlined in Table 1. In some Asian countries including Korea, where intestinal tuberculosis is still prevalent, the distinction between intestinal tuberculosis and CD is extremely difficult because of their clinical similarities. Studies from Korea have shown that the proportion of patients receiving anti-tuberculosis treatment before confirmation of CD was nearly 50% of all CD patients.36 In a study conducted in Korea, four endoscopic characteristics were identified for each disease: anorectal lesions, longitudinal ulcers, aphthous ulcers, and a cobblestone appearance for CD, and involvement of fewer than four segments, a patulous ileocecal valve, transverse ulcers, and scars or pseudopolyps for intestinal tuberculosis. Using these endoscopic parameters, the diagnosis of either intestinal tuberculosis or CD was correctly made in 87.5% of patients.18 In Asia, if a patient has an ulceration in the ileocecal region, intestinal Behçet's disease (BD) should be included as a differential diagnosis.35 In an effort to differentiate intestinal BD and CD, a Korean study reported that round ulcerations, ≤5 in number, focal distributions, and absence of aphthous and cobblestone lesions were dominant features in intestinal BD.12 The authors stated that these characteristics enabled the correct diagnosis of intestinal BD or CD in 92% of patients with ulcers on colonoscopy.
Table 1.
Differential Diagnosis of Intestinal Inflammation
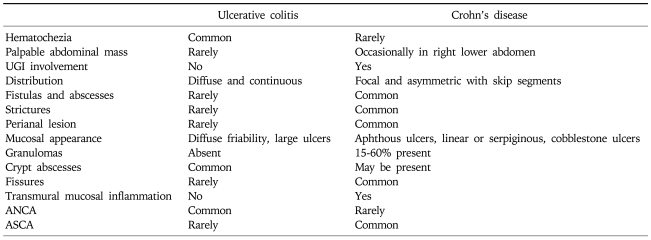
As the two main subforms of IBD, UC and CD have similar clinical manifestations, it is very challenging for the clinicians to correctly diagnose IBD. While there are several diagnostic criteria available for IBD including Mendeloff's criteria,37 Lennard-Jones criteria,38 the international multicentre scoring system of the Organization Mondiale de Gastroenterologie (OMGE),39 and the diagnostic criteria of the Japanese Research Society on IBD,3 there is no single gold standard for the diagnosis of IBD. All diagnostic criteria use an integrating assessment of the clinical presentation, endoscopic, radiographic, and pathologic findings for diagnosis. More recently, serologic assays, utilizing antineutrophil cytoplasmic autoantibody (ANCA) and anti-Saccharomyces cerevisiae antibody (ASCA) have been added as diagnostic tools with an adjunctive role in differentiating UC and CD.40,41 A Korean study demonstrated that the sensitivity (49.4%) and the specificity (79.2%) of ASCA for CD are comparable to those seen in Western countries and that the sensitivity (44.2%) and the specificity (95.8%) of the pANCA for UC are also similar to those previously reported in Western countries.42 However, in a recent Korean study, Lee et al. reported that the prevalence of pANCA in Korean patients with UC was relatively low compared to patients in Western countries (22% vs 59-84%).17 The major distinctive clinical, morphological, structural and pathological features between the two subforms of IBD are listed in Table 2.
Table 2.
Differences in Clinical, Endoscopic, and Histological Features between Ulcerative Colitis and Crohn's Disease
UGI, upper gastrointestinal; ANCA, anti-neutrophil cytoplasmic antibodies; ASCA, anti-saccharomyces cerevisiae antibodies.
As genome-wide association studies have been introduced in an effort to identify the etiologic factors of IBD, many genetic polymorphisms related to an increased risk of IBD have been discovered.43-52 In the near future, it is expected that a more specific genetic map will be identified to improve the diagnosis of IBD. Combined with serologic assays, genetic testing is promising for a number of reasons. First, genetic testing is non-invasive. Second, genetic testing can be used to predict the phenotypic features of disease.53 Serologic tests serve as effective means to predict a complicated course of the disease by showing high associations with disease activity and the sites of involvement in IBD.54,55 A judicious combined utilization of genetic and serologic tests may be more reliable for predicting complicated behavior than the use of either test alone and may be helpful in developing a risk-stratified approach for the selection of medical therapy.56 Moreover, genetic evidence could allow clinicians to identify IBD patients before they become symptomatic and to choose appropriate early preventive measures.
Genotypic features and clinical characteristics of Korean IBD are somewhat different from those of Western countries. In Korea, a recent population based study showed that the most common location of the involvement CD is in both small bowel and colon (66.7%) followed by isolated segments of either small bowel (21.0%) or colon (12.3%).1 This finding is similar to that reported by a Japanese study.57 This contrasts with recent European studies that reported isolated colonic disease as the most common type of CD at diagnosis.29,58 In a genetic polymorphism study with a large number of Northern European and Korean patients with CD and normal controls, CARD15 (NOD2) mutations were not found to be associated with susceptibility to CD in Korean patients, although they were in European populations.59 This finding was confirmed by another study also conducted in Korea.15 On the other hand, recent studies showed that genetic variants in IL23R, tumor necrosis factor superfamily member 15 (TNFSF15), and tumor necrosis factor-α (TNF-α) gene but not autophagy-related 16-like 1 (ATG16L1), which are known to be associated with CD in European populations also contribute to CD susceptibility in Koreans.60-62 In Japan63,64 and Korea65 studies, the HLA-DRB1*1502 allele was shown to be positively associated with UC, whereas the results showed discord about this association in Western populations.66-68
The clinical features of UC at diagnosis are reported to be similar in Koreans and Westerners.20 For instance, there are no differences in the extent and the severity of disease at diagnosis or in the male to female ratio of patients with UC between Korea and Western countries.
EVALUATION OF CLINICAL ACTIVITY
To develop an optimal treatment strategy for IBD, it is essential to fully understand the disease's activity and extension of disease. The Truelove and Witts severity index is one of the most commonly used disease activity indexes for UC, and comprises six items: number of stools per day, presence of blood in stools, temperature, pulse, hemoglobin and erythrocyte sedimentation rate (ESR).69 Another popular activity index is the Mayo Score, which is composed of four variables: frequency of bowel movements, rectal bleeding, findings of sigmoidoscopy and Physician Global Assessment.70 Generally, the anatomic extent of UC is divided into "distal" when the lesions are not found beyond the splenic flexure and "extensive" when the mucosal inflammation is extended proximally to the splenic flexure.71 In a Korean study of 304 UC patients, 44.1% of patients were diagnosed with proctitis, 22.7% with left side colitis and 33.2% with extensive colitis. The clinical severity was mild in 49.0% of patients, moderate in 41.1% and severe in 8.6%.20 As serologic markers for the clinical activity of UC, pANCA and triggering receptors expressed on myeloid cells-1 (TREM-1) have been reported to be useful. The UC activity index was found to be higher in pANCA-positive patients than in pANCA-negative Korean patients.17 The serum TREM-1 level correlated better with disease activity than ESR or CRP, irrespective of disease extent in Korean patients with UC.19
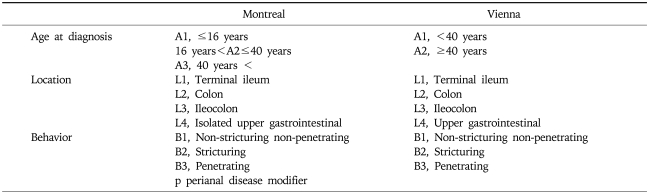
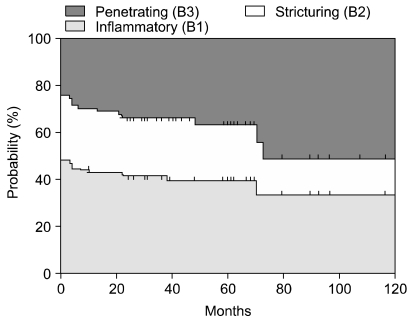
Since CD affects various sites of the intestine and manifests as different endoscopic appearances of involvement, it is suggested that CD is a heterogeneous entity and that different genetic backgrounds may explain the different clinical patterns observed for the disease.72,73 It is, therefore, important to develop a simple classification of CD based on stable and reproducible clinical variables in order to study its genetic or environmental bases. In 1998, the World Gastroenterology Meeting in Vienna proposed a new classification based on three clinical variables including age at diagnosis, location and disease behavior (Table 3).74 According to the Vienna classification, patients are categorized into the A1 group if the diagnosis is made before 40 years of age and A2 if it is made thereafter. Patients are regarded as L1 when the disease is located in the terminal ileum, L2 when it is located in the colon, L3 when it is located in the ileocolon, and L4 when it involves the upper gastrointestinal tract. The B1 group includes patients with non-stricturing non-penetrating disease, the B2 group includes patients with stricturing disease, and the B3 group includes patients with penetrating disease. Among these variables, disease location appears to remain stable, while significant sustained changes are noted in disease behavior over time.75 Recently, the Vienna classification was revised and a new Montreal classification was proposed.76 Regarding age-of-onset, the Montreal revision categorizes early onset of disease as an A1 category for those with an age of diagnosis of 16 years or younger. With respect to disease location, the Montreal classification allows upper gastrointestinal disease to coexist with more distal disease. Lastly, in terms of disease behavior, perianal disease is recognized as a separate subclassification. The data from Severance Hospital in Korea following the Vienna classification showed that patients in groups A1 and A2 made up 88.9% and 11.1%, respectively, of the entire patient population, and that L1, L2, L3, and L4 made up 19.5%, 13.9%, 45.8%, and 20.8%, respectively.77 Notably, the most common location was L3, which is different from the pattern normally seen in Western countries. During the follow-up period, the proportion of B1 and B2 diminished from 48.6% and 27.8% to 37.5% and 25%, respectively, while that of B3 increased from 23.6% up to 37.5% (Fig. 1). The Crohn's disease activity index (CDAI), the most widely applied activity index for CD, consists of eight variables: the number of liquid stools, the extent of abdominal pain, general well-being, the occurrence of extraintestinal symptoms, the need for anti-diarrheal drugs, the presence of abdominal masses, hematocrit and body weight.78 The range of scores is 0 to 600 and in clinical trials, active CD is indicated when the CDAI score is over 150. As the CDAI has been frequently used in clinical trials over two decades and vigorously validated, this index is considered the gold standard for evaluation of disease activity.79 The Harvey Bradshaw index is another convenient and commonly used activity index for CD.80
Table 3.
The Vienna and Montreal Classifications of Crohn's Disease
Fig. 1.
Changes in disease behavior in Korean CD patients according to the Vienna classification.
MANAGEMENT OF IBD
IBD is characterized by its chronicity, with cycles of remission and relapse that occur over the patient's lifetime. The goals of therapy for IBD, therefore, are not only the induction but also the maintenance of remission of symptoms without the use of corticosteroids.
CROHN'S DISEASE
1. Medical management
1) Induction of remission
Clinical trials have documented that sulfasalazine, budesonide, and conventional corticosteroids are effective at inducing remission in mild to moderately active CD.
Although oral aminosalicylates have been widely used in clinical practice to treat active CD, their use is controversial evidence. In the case of mild to moderate CD, clinical trials demonstrate that sulfasalazine administered at 2-6 g/day is more effective than placebo for inducing remission.81,82 This effect is most notable in patients with active colonic or ileocolonic disease.83,84 In contrast, mesalazine has failed to show consistent results in various controlled studies.85-87 Some patients are intolerant of the adverse effects of sulfasalazine, including headache, nausea, skin rash, fever, hepatitis, autoimmune hemolysis, aplastic anemia, leucopenia, folate deficiency, pancreatitis and male infertility. Most of these effects are related to the sulfapyridine moiety of sulfasalazine. Considering that the intestinal bacterial flora probably plays a role in the pathogenesis of CD, antibiotics have been used as therapeutic agents. Although metronidazole and ciprofloxacin are often used for the treatment of CD, controlled trials have failed to show convincing evidence of their efficacy for the induction of remission in active CD.88-91 Budesonide undergoes extensive first-pass hepatic metabolism, which reduces the side effects associated with systemic corticosteroids. Well controlled studies have revealed that budesonide is significantly more effective than placebo and 5-ASA, and is about as effective as conventional corticosteroids for inducing remission in active CD.92-94 Therefore, budesonide has been recommended as a first-line therapy for mild to moderate CD of the ileum and proximal colon in an American Gastroenterological Association position statement and in the European Crohn's and Colitis Organization Consensus.95,96
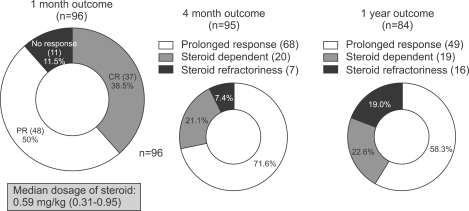
For those patients who do not respond to the first-line therapy described above and for those with moderate to severe CD, oral prednisone 40-60 mg/day should be given. In the case of fulminant and refractory inflammatory CD, remission may be induced with intravenous corticosteroids, such as methylprednisolone at 1-1.5 mg/kg per day. A Korean study showed that serum albumin level could be a significant predictive factor for response to initial steroid therapy in active CD patients.97 Compared to steroid responders, a steroid dependent group was characterized by lower serum albumin levels. According to the data from a Korean study, when a median dosage of oral steroids at 0.59 mg/kg was administered, the overall response rates to the steroid at one month and one year were as high as 88.5% and 58.3%, respectively.98 These rates were comparable to the best response rates from Western studies (Fig. 2). Patients with moderate to severe disease who fail to respond to 5-ASA, budesonide and conventional corticosteroids, and patients intolerant of corticosteroids, may be treated with anti-TNF-α antibody agents including infliximab (intravenous, 5 mg/kg at 0, 2, and 6 weeks) and adalimumab (subcutaneous, 160 mg at 0 and 80 mg at 2 weeks). The results of a nationwide survey conducted in Korea,99 showed that the clinical response rate for infliximab in luminal CD was 51%, and that the clinical remission rate was 36%. Thirteen percent of patients did not respond to infliximab treatment. In patients with fistular disease, the clinical response rate was 45%, clinical remission 31%, and no response 24%. These results are similar to the clinical response rates reported in Western studies. Interestingly, the most common reason for infliximab cessation in Korea was the limitation of the standard national health insurance reimbursement, as it previously covered only one year of infliximab treatment for active CD patients. However, the national health insurance coverage for infliximab has been extended up to 28 injections, regardless of period in a recent amendment.100
Fig. 2.
Overall response rates to steroids in Korean Crohn's disease patients.
2) Maintenance therapy
Despite the widespread use of 5-ASA in clinical practice for the maintenance of medically induced remission in CD patients, this application is not evidence-based. Clinical studies have revealed that sulfasalazine and mesalazine are not actually effective for maintaining medically induced remission in CD patients. In general, corticosteroids are not recommended for maintaining remission due to related systemic adverse effects and lack of efficacy. The results of a Korean study showed that preoperative corticosteroid treatment increased the risk of postoperative infections in patients with CD.101 Treatment with budesonide at 6 mg/day, however, has been shown to prolong the time to relapse and to be effective at maintaining remission for at least six months, but less than one year.102
Immunosuppressive agents such as azathioprine (AZA) and 6-mercaptopurine (6-MP) have been reported to be effective as maintenance therapy and to be advantageous for reducing or discontinuing steroid usage in steroid-dependent CD patients.103-105 However, due to slow onset of action, these drugs are not used as induction therapy in patients with active CD.103 Because azathioprine or mercaptopurine are frequently continued indefinitely as maintenance therapy,106 their long term side effects should be kept in mind. These agents, therefore, are currently reserved for steroid-dependent or refractory patients. Myelotoxicity is one of the significant adverse effects of thiopurine drugs and is reported to be associated with decreased thiopurine methyltransferase (TPMT) and deficiency of inosine triphosphate pyrophosphatase (ITPA).107 Korean patients with IBD who are treated with AZA/6-MP experience myelotoxicity more frequently than similarly treated Europeans. Among 133 IBD patients treated with azathioprine in Korea, leucopenia occurred in 75 cases (56.4%), which is a higher incidence than that reported in Western studies.108 Another Korean study revealed that there is no correlation between TPMT genotype and AZA toxicity.109 Methotrexate is another effective immunosuppressive agent for maintaining remission of CD.
For patients who are unable to maintain remission or who are dependent on steroids in spite of treatment with AZA or 6-MP, infliximab can be used for maintenance of remission, steroid-sparing and mucosal healing (5 mg/kg every eight weeks).110 Alternatively, adalimumab can be given subcutaneously for maintenance therapy at 40 mg every other week. With advances in the understanding of the pathophysiology of CD, a range of new therapeutic agents apart from anti-TNF drugs are under investigation. Among these innovative drugs are the T-cell blocking agents,111 anti-adhesion molecules,112 anti-vascular adhesion protein-1 monoclonal antibody113 and avidity multimers (avimers)114 with high ligand affinity and specificity that allows binding to many targets at the same time.
2. Medical management of fistulizing CD
One of the distinct characteristics of Korean CD patients is the high incidence of perianal fistulas. The incidence rate of perianal fistulas in Korea is 48.5%, which is higher than that reported in other countries (13-38%).13 Because the incidence of CD in Korea has been increasing substantially, the possibility of CD should be considered in Korean patients with perianal fistulas. The first-line therapy for fistulas in patients with CD is antibiotic treatment with metronidazole or ciprofloxacin,96,104,115,116 with AZA or 6-MP being the typical second-line treatment. In cases in which active fistulizing disease fails to respond to treatment with antibiotics and immunosuppressive agents, infliximab or adalimumab can be administered.
3. Surgical management
A significant proportion of CD patients will need surgical management an average of 20 years after diagnosis. Failure of medical therapy remains the most common indication for surgical treatment of CD.117,118 The occurrence of complications despite medical treatment is an additional indication for surgical management.
Worsening obstruction is a frequent complication of CD, especially with small bowel involvement. Whereas acute obstructions are often resolved with medical treatment, chronic obstructions are usually caused by fibrostenotic lesions and require surgical management.119
Not all fistulas require surgery. Although intestinal fistulas occur in one-third of CD patients, only a few patients require surgical management.120 Generally, fistulas associated with abscesses or strictures, that are connected to the genitourinary tract, or that cause intestinal malabsorption are indications for surgical management.
The lifetime risk for intraabdominal abscess in CD patients is approximately 25%.121 Almost all abscesses require drainage either surgically or percutaneously. Although there is controversy as to whether or not intraabdominal CD abscess should be managed surgically, surgical resection is required when an abscess has enteric contents.122 Korean data have shown that nonsurgical treatment including percutaneous catheter drainage can be considered an initial therapy for a CD-related abscess. The overall success rate and cumulative recurrence rate at seven months were 66.7% and 12.5%, respectively.16 A recent Korean study reported that the clinical efficacy of nonsurgical treatment is comparable to that of surgical treatment.123 Other indications for surgical management in CD include free perforation, bleeding and cancer.
In CD, 70-90% of patients will require surgical management during the disease course. Another study reported that the cumulative operation rate was 44%, 61%, and 71% at one, five, and 10 years after diagnosis, respectively.124 Unlike the above Western studies, the rate was much lower in the results of a Korean study with 11.5%, 13.1%, and 18.2% at one, three, and six years after diagnosis, respectively.36 The rate reported in another Korean study was also lower than that reported for Western countries.125 This disparity could be attributed to the different perspectives of different backgrounds toward surgical intervention in CD patients. Another possible reason could be that the Western study was conducted early, when aggressive surgery for CD was prevalent and Korean studies are more recent, when surgical treatment is rarely performed due to the advances in medical treatment.
The rate of complications with surgical management for CD in Korea is 13.6%, which is comparable to that of other countries.126
ULCERATIVE COLITIS
1. Medical management
UC can be treated according to anatomical extent of the disease. In distal UC, in which disease involvement is limited to below the splenic flexure, a topical agent can be effectively applied. Similar to CD, the management of UC is focused on both induction and maintenance of disease remission. In addition, the therapeutic decision depends mainly on clinical severity rather than on histologic severity of inflammation.
1) Induction of remission
In mild to moderate active UC patients, the first line regimen is 5-ASA, including oral and rectal formulations. Effective oral doses for each drug are as follows; sulfasalazine 4-6 g/day, mesalamine 2-4 g/day, balsalazide 6.75 g/day, olsalazine 1.5-3 g/day. The effects of these drugs are usually observed within 2-4 weeks in 40-80% of patients.127,128 Left side colitis can also be managed with topical agents such as rectal mesalazine or rectal corticosteroid. Controlled trials show that topical mesalamine is superior to oral 5-ASA or topical corticosteroid alone in inducing clinical improvement in patients with mild to moderate distal colitis.110,129,130 Furthermore, the combination of oral and topical 5-ASA may produce a better response in the management of mild to moderate distal colitis than administration of either oral or topical formulations alone.131
If the patients fail to respond to 5-ASA agents, they should be managed with oral prednisone 40-60 mg daily for one to two weeks. At one year after starting corticosteroids, a prolonged response is observed in 49% of patients, and 22% of patients become steroid dependent.132
Patients with severe active UC showing aggravated symptoms despite treatment with oral corticosteroids should be hospitalized for intravenous steroid therapy. Further failure to respond to intravenous steroid might require the use of cyclosporine, tacrolimus and a biologic agent such as infliximab. If patients do not respond to maximal medical treatment, superimposed infection with cytomegalovirus or C. difficile should be considered as a potential cause of aggravation.
Although there have been many studies in Western countries indicating the usefulness of cyclosporine in the treatment of severe UC, the efficacy of cyclosporine has been disappointing in Korea, with a reported response rate of only 14%.133 One Korean study was conducted to evaluate the efficacy of cyclosporine and corticosteroid combination therapy in patients with severe UC that was refractory to an initial intravenous corticosteroid treatment. Unlike Western studies, the Korean study concluded that this combination failed to present any additional benefit over corticosteroid therapy alone in terms of short-term response.134 These results suggest that there might be differences in the metabolism of this agent or differences in phenotypes, in terms of responsiveness, based on differences in genetic backgrounds.
Korean UC patients seem to show a better clinical response to medical treatment than their Western counterparts. The overall remission rate in the first attack was 90% in Western population-based studies, whereas the rate in the Korean study with 311 first diagnosed UC patients was 97.4%.20
2) Maintenance management
5-ASA agents are the mainstay of effective treatment for relapse-prevention of UC. Topical 5-ASA reduces the relapse rates in proctitis or left sided colitis, but topical corticosteroids have not shown effectiveness as a maintenance treatment in distal colitis.127,135,136 AZA or 6-MP may be another choice for relapse-prevention in patients who do not respond to 5-ASA or who are dependent on oral steroids. Patients, who have frequent relapses or are steroid-dependent, despite treatment with 5-ASA and immunomodulators, can be treated effectively with infliximab. Recent studies have shown that 45% of infliximab responders remain in the non-relapsed state, compared to 20% of initial responders in the placebo group after 54 weeks of maintenance therapy with infliximab.137 These promising results with infliximab encourage further trials for confirmation of the role of infliximab as an effective management of UC.
2. Surgical management
A surgical approach is required for treatment of UC when there are life-threatening complications such as hemorrhage or perforation, and documented dysplasia or cancer. Other indications for surgery include fulminant colitis with or without toxic megacolon refractory to maximal medical management or intolerance to immunosuppression or medical therapy. Growth failure due to intractable disease course in pediatric UC patients can also be an indication for surgery.138 Since 20-24% of strictures in UC are malignant139 and biopsies of the stricture site are inadequate for excluding malignancy, strictures should be managed with surgery.140
Total proctocolectomy with ileal J-pouch anal anastomosis (IPAA) is the most commonly used surgical method for treatment of UC. Large cohort studies have described this method as relatively safe and durable with a low perioperative mortality rate of 0.2-1.0%. In a recent study of 20 Korean UC patients treated with IPAA, postoperative functional outcomes including sexual and urinary function were found to be tolerable. Despite a relatively high postoperative complication rate (35%), most cases were managed conservatively.14
Pouchitis is the most common long-term complication of IPAA. It develops in 24-48% of IPAA patients and can be controlled with antibiotics including ciprofloxacin or metronidazole. Similar to data from other countries, 37.5% of Korean UC patients undergoing total proctocolectomy with IPAA have pouchitis and most of these cases occur within one year after surgery.141
One of the unique characteristics is that the cumulative probability of colectomy is much lower in Korean UC patients than in Western patients. In Western countries, the cumulative colectomy rate is shown to be 3-10% after one year,142-144 8-20% after five years,144,145 and 24-34% after 10 years.146,147 In contrast, studies from Korea reveal that it is 2.0-3.0% after one year and 3.3% after five to 15 years.17,20 Furthermore, the author showed that there were no deaths associated with UC in that study, suggesting that Korean UC patients tend to have a milder form of the disease.
CONCLUSION
Although IBD is a worldwide disease, its incidence rates and clinical features vary depending on geographic area and population origin. The incidence and the prevalence rates of IBD have been increasing dramatically in Korea. There are some clinical and genotypic characteristics that are unique to Korean IBD patients (Tables 4 and 5). Most of all, the clinical course of IBD in Korean patients seems milder than that in Western countries, as indicated by the lower rates of surgical intervention and better responses to medical management in Korean patients. These differing characteristics may provide significant clues about the etiology and the pathophysiology of IBD. Further comprehensive population-based studies are required to clarify these differences.
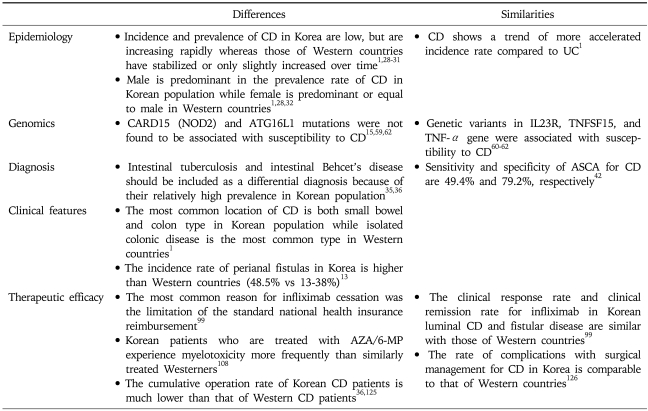
Table 4.
Characteristics of Korean Patients with CD Compared to Those of Western Countries
Table 5.
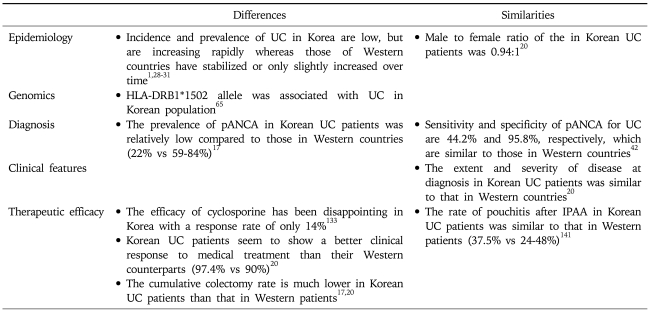
Characteristics of Korean Patients with UC Compared to Those of Western Countries
Although biological therapies have shown a promising role and have altered the management of IBD, they must be used judiciously based on the existing evidence of efficacy and safety. The recent emergence of several promising biologic agents suggests that these novel biologic agents may replace or be used in combination with TNF antagonists in the near future.
References
- 1.Yang SK, Yun S, Kim JH, et al. Epidemiology of inflammatory bowel disease in the Songpa-Kangdong district, Seoul, Korea, 1986-2005: a KASID study. Inflamm Bowel Dis. 2008;14:542–549. doi: 10.1002/ibd.20310. [DOI] [PubMed] [Google Scholar]
- 2.Leong RW, Lau JY, Sung JJ. The epidemiology and phenotype of Crohn's disease in the Chinese population. Inflamm Bowel Dis. 2004;10:646–651. doi: 10.1097/00054725-200409000-00022. [DOI] [PubMed] [Google Scholar]
- 3.Morita N, Toki S, Hirohashi T, et al. Incidence and prevalence of inflammatory bowel disease in Japan: nationwide epidemiological survey during the year 1991. J Gastroenterol. 1995;30(Suppl 8):1–4. [PubMed] [Google Scholar]
- 4.Yang SK, Hong WS, Min YI, et al. Incidence and prevalence of ulcerative colitis in the Songpa-Kangdong District, Seoul, Korea, 1986-1997. J Gastroenterol Hepatol. 2000;15:1037–1042. doi: 10.1046/j.1440-1746.2000.02252.x. [DOI] [PubMed] [Google Scholar]
- 5.Ling KL, Ooi CJ, Luman W, Cheong WK, Choen FS, Ng HS. Clinical characteristics of ulcerative colitis in Singapore, a multiracial city-state. J Clin Gastroenterol. 2002;35:144–148. doi: 10.1097/00004836-200208000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Iida M, Yao T, Okada M. Long-term follow-up study of Crohn's disease in Japan: the Research Committee of Inflammatory Bowel Disease in Japan. J Gastroenterol. 1995;30(Suppl 8):17–19. [PubMed] [Google Scholar]
- 7.Inoue N, Tamura K, Kinouchi Y, et al. Lack of common NOD2 variants in Japanese patients with Crohn's disease. Gastroenterology. 2002;123:86–91. doi: 10.1053/gast.2002.34155. [DOI] [PubMed] [Google Scholar]
- 8.Yang SK, Loftus EV, Jr, Sandborn WJ. Epidemiology of inflammatory bowel disease in Asia. Inflamm Bowel Dis. 2001;7:260–270. doi: 10.1097/00054725-200108000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Kim BJ, Yang SK, Kim JS, et al. Trends of ulcerative colitis-associated colorectal cancer in Korea: a KASID study. J Gastroenterol Hepatol. 2009;24:667–671. doi: 10.1111/j.1440-1746.2008.05730.x. [DOI] [PubMed] [Google Scholar]
- 10.Chang DK, Kim YH, Byeon JS, et al. The current status of ulcerative colitis-associated colorectal cancer in Korea: a KASID study. Korean J Gastroenterol. 2005;46:276–282. [PubMed] [Google Scholar]
- 11.Cheon JH, Kim JH, Kim BY, et al. Allele frequency of thiopurine methyltransferase and inosine triphosphate pyrophosphatase gene polymorphisms in Korean patients with inflammatory bowel diseases. Hepatogastroenterology. 2009;56:421–423. [PubMed] [Google Scholar]
- 12.Lee SK, Kim BK, Kim TI, Kim WH. Differential diagnosis of intestinal Behcet's disease and Crohn's disease by colonoscopic findings. Endoscopy. 2009;41:9–16. doi: 10.1055/s-0028-1103481. [DOI] [PubMed] [Google Scholar]
- 13.Kim JY, Yang SK, Byeon JS. The incidence and natural history of perianal fistulas in Korean patients with Crohn's disease. Intest Res. 2006;4:22–31. [Google Scholar]
- 14.Ko YT, Kim NK, Min BS, et al. Twenty cases of restorative proctocolectomy for ulcerative colitis of Asian patients: analysis of operative safety and functional outcomes in single institution experience. Int J Colorectal Dis. 2008;23:131–132. doi: 10.1007/s00384-007-0278-y. [DOI] [PubMed] [Google Scholar]
- 15.Lee GH, Kim CG, Kim JS, Jung HC, Song IS. Frequency analysis of NOD2 gene mutations in Korean patients with Crohn's disease. Korean J Gastroenterol. 2005;45:162–168. [PubMed] [Google Scholar]
- 16.Lee H, Kim YH, Kim JH, et al. Nonsurgical treatment of abdominal or pelvic abscess in consecutive patients with Crohn's disease. Dig Liver Dis. 2006;38:659–664. doi: 10.1016/j.dld.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 17.Lee JH, Cheon JH, Kim ES, et al. The prevalence and clinical significance of perinuclear anti-neutrophil cytoplasmic antibody in Korean patients with ulcerative colitis. Dig Dis Sci. doi: 10.1007/s10620-009-0847-8. Forthcoming. DOI: 10.1007/s10620-009-0847-8. [DOI] [PubMed] [Google Scholar]
- 18.Lee YJ, Yang SK, Byeon JS, et al. Analysis of colonoscopic findings in the differential diagnosis between intestinal tuberculosis and Crohn's disease. Endoscopy. 2006;38:592–597. doi: 10.1055/s-2006-924996. [DOI] [PubMed] [Google Scholar]
- 19.Park JJ, Cheon JH, Kim BY, et al. Correlation of serum-soluble triggering receptor expressed on myeloid cells-1 with clinical disease activity in inflammatory bowel disease. Dig Dis Sci. 2009;54:1525–1531. doi: 10.1007/s10620-008-0514-5. [DOI] [PubMed] [Google Scholar]
- 20.Park SH, Kim YM, Yang SK, et al. Clinical features and natural history of ulcerative colitis in Korea. Inflamm Bowel Dis. 2007;13:278–283. doi: 10.1002/ibd.20015. [DOI] [PubMed] [Google Scholar]
- 21.Russel MG. Changes in the incidence of inflammatory bowel disease: what does it mean? Eur J Intern Med. 2000;11:191–196. doi: 10.1016/s0953-6205(00)00090-x. [DOI] [PubMed] [Google Scholar]
- 22.Cashman KD, Shanahan F. Is nutrition an aetiological factor for inflammatory bowel disease? Eur J Gastroenterol Hepatol. 2003;15:607–613. doi: 10.1097/00042737-200306000-00005. [DOI] [PubMed] [Google Scholar]
- 23.Jovanovic Z. Epidemiology of Crohn's disease in the Rijeka-Istra region. Lijec Vjesn. 1999;121:8–13. [PubMed] [Google Scholar]
- 24.Appleyard CB, Hernandez G, Rios-Bedoya CF. Basic epidemiology of inflammatory bowel disease in Puerto Rico. Inflamm Bowel Dis. 2004;10:106–111. doi: 10.1097/00054725-200403000-00007. [DOI] [PubMed] [Google Scholar]
- 25.Linares de la Cal JA, Canton C, Hermida C, Perez-Miranda M, Mate-Jimenez J. Estimated incidence of inflammatory bowel disease in Argentina and Panama (1987-1993) Rev Esp Enferm Dig. 1999;91:277–286. [PubMed] [Google Scholar]
- 26.Lakatos L, Mester G, Erdelyi Z, et al. Striking elevation in incidence and prevalence of inflammatory bowel disease in a province of western Hungary between 1977-2001. World J Gastroenterol. 2004;10:404–409. doi: 10.3748/wjg.v10.i3.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sincic BM, Vucelic B, Persic M, et al. Incidence of inflammatory bowel disease in Primorsko-goranska County, Croatia, 2000-2004: a prospective population-based study. Scand J Gastroenterol. 2006;41:437–444. doi: 10.1080/00365520500320094. [DOI] [PubMed] [Google Scholar]
- 28.Molinie F, Gower-Rousseau C, Yzet T, et al. Opposite evolution in incidence of Crohn's disease and ulcerative colitis in Northern France (1988-1999) Gut. 2004;53:843–848. doi: 10.1136/gut.2003.025346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lapidus A. Crohn's disease in Stockholm County during 1990-2001: an epidemiological update. World J Gastroenterol. 2006;12:75–81. doi: 10.3748/wjg.v12.i1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Loftus EV, Jr, Silverstein MD, Sandborn WJ, Tremaine WJ, Harmsen WS, Zinsmeister AR. Crohn's disease in Olmsted County, Minnesota, 1940-1993: incidence, prevalence, and survival. Gastroenterology. 1998;114:1161–1168. doi: 10.1016/s0016-5085(98)70421-4. [DOI] [PubMed] [Google Scholar]
- 31.Loftus EV, Jr, Silverstein MD, Sandborn WJ, Tremaine WJ, Harmsen WS, Zinsmeister AR. Ulcerative colitis in Olmsted County, Minnesota, 1940-1993: incidence, prevalence, and survival. Gut. 2000;46:336–343. doi: 10.1136/gut.46.3.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bernstein CN, Wajda A, Svenson LW, et al. The epidemiology of inflammatory bowel disease in Canada: a population-based study. Am J Gastroenterol. 2006;101:1559–1568. doi: 10.1111/j.1572-0241.2006.00603.x. [DOI] [PubMed] [Google Scholar]
- 33.Gearry RB, Richardson A, Frampton CM, et al. High incidence of Crohn's disease in Canterbury, New Zealand: results of an epidemiologic study. Inflamm Bowel Dis. 2006;12:936–943. doi: 10.1097/01.mib.0000231572.88806.b9. [DOI] [PubMed] [Google Scholar]
- 34.Yao T, Matsui T, Hiwatashi N. Crohn's disease in Japan: diagnostic criteria and epidemiology. Dis Colon Rectum. 2000;43(10 Suppl):S85–S93. doi: 10.1007/BF02237231. [DOI] [PubMed] [Google Scholar]
- 35.Sands BE. From symptom to diagnosis: clinical distinctions among various forms of intestinal inflammation. Gastroenterology. 2004;126:1518–1532. doi: 10.1053/j.gastro.2004.02.072. [DOI] [PubMed] [Google Scholar]
- 36.Park JB, Yang SK, Myung SJ, et al. Clinical characteristics at diagnosis and course of Korean patients with Crohn's disease. Korean J Gastroenterol. 2004;43:8–17. [PubMed] [Google Scholar]
- 37.Calkins BM, Lilienfeld AM, Garland CF, Mendeloff AI. Trends in incidence rates of ulcerative colitis and Crohn's disease. Dig Dis Sci. 1984;29:913–920. doi: 10.1007/BF01312480. [DOI] [PubMed] [Google Scholar]
- 38.Lennard-Jones JE. Classification of inflammatory bowel disease. Scand J Gastroenterol Suppl. 1989;170:2–6. doi: 10.3109/00365528909091339. [DOI] [PubMed] [Google Scholar]
- 39.Myren J, Bouchier IA, Watkinson G, Softley A, Clamp SE, de Dombal FT. The OMGE multinational inflammatory bowel disease survey 1976-1986: a further report on 3175 cases. Scand J Gastroenterol Suppl. 1988;144:11–19. [PubMed] [Google Scholar]
- 40.Saxon A, Shanahan F, Landers C, Ganz T, Targan S. A distinct subset of antineutrophil cytoplasmic antibodies is associated with inflammatory bowel disease. J Allergy Clin Immunol. 1990;86:202–210. doi: 10.1016/s0091-6749(05)80067-3. [DOI] [PubMed] [Google Scholar]
- 41.Vermeire S, Joossens S, Peeters M, et al. Comparative study of ASCA (Anti-Saccharomyces cerevisiae antibody) assays in inflammatory bowel disease. Gastroenterology. 2001;120:827–833. doi: 10.1053/gast.2001.22546. [DOI] [PubMed] [Google Scholar]
- 42.Kim BG, Kim YS, Kim JS, Jung HC, Song IS. Diagnostic role of anti-Saccharomyces cerevisiae mannan antibodies combined with antineutrophil cytoplasmic antibodies in patients with inflammatory bowel disease. Dis Colon Rectum. 2002;45:1062–1069. doi: 10.1007/s10350-004-6361-3. [DOI] [PubMed] [Google Scholar]
- 43.Hugot JP, Chamaillard M, Zouali H, et al. Association of NOD2 leucine-rich repeat variants with susceptibility to Crohn's disease. Nature. 2001;411:599–603. doi: 10.1038/35079107. [DOI] [PubMed] [Google Scholar]
- 44.Ogura Y, Bonen DK, Inohara N, et al. A frameshift mutation in NOD2 associated with susceptibility to Crohn's disease. Nature. 2001;411:603–606. doi: 10.1038/35079114. [DOI] [PubMed] [Google Scholar]
- 45.Hampe J, Cuthbert A, Croucher PJ, et al. Association between insertion mutation in NOD2 gene and Crohn's disease in German and British populations. Lancet. 2001;357:1925–1928. doi: 10.1016/S0140-6736(00)05063-7. [DOI] [PubMed] [Google Scholar]
- 46.Stoll M, Corneliussen B, Costello CM, et al. Genetic variation in DLG5 is associated with inflammatory bowel disease. Nat Genet. 2004;36:476–480. doi: 10.1038/ng1345. [DOI] [PubMed] [Google Scholar]
- 47.Till A, Rosenstiel P, Krippner-Heidenreich A, et al. The Met-196 → Arg variation of human tumor necrosis factor receptor 2 (TNFR2) affects TNF-alpha-induced apoptosis by impaired NF-kappaB signaling and target gene expression. J Biol Chem. 2005;280:5994–6004. doi: 10.1074/jbc.M411541200. [DOI] [PubMed] [Google Scholar]
- 48.Duerr RH, Taylor KD, Brant SR, et al. A genome-wide association study identifies IL23R as an inflammatory bowel disease gene. Science. 2006;314:1461–1463. doi: 10.1126/science.1135245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hampe J, Franke A, Rosenstiel P, et al. A genome-wide association scan of nonsynonymous SNPs identifies a susceptibility variant for Crohn disease in ATG16L1. Nat Genet. 2007;39:207–211. doi: 10.1038/ng1954. [DOI] [PubMed] [Google Scholar]
- 50.Rioux JD, Xavier RJ, Taylor KD, et al. Genome-wide association study identifies new susceptibility loci for Crohn disease and implicates autophagy in disease pathogenesis. Nat Genet. 2007;39:596–604. doi: 10.1038/ng2032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Parkes M, Barrett JC, Prescott NJ, et al. Sequence variants in the autophagy gene IRGM and multiple other replicating loci contribute to Crohn's disease susceptibility. Nat Genet. 2007;39:830–832. doi: 10.1038/ng2061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Raelson JV, Little RD, Ruether A, et al. Genome-wide association study for Crohn's disease in the Quebec Founder Population identifies multiple validated disease loci. Proc Natl Acad Sci U S A. 2007;104:14747–14752. doi: 10.1073/pnas.0706645104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Riis L, Vind I, Vermeire S, et al. The prevalence of genetic and serologic markers in an unselected European population-based cohort of IBD patients. Inflamm Bowel Dis. 2007;13:24–32. doi: 10.1002/ibd.20047. [DOI] [PubMed] [Google Scholar]
- 54.Targan SR, Landers CJ, Yang H, et al. Antibodies to CBir1 flagellin define a unique response that is associated independently with complicated Crohn's disease. Gastroenterology. 2005;128:2020–2028. doi: 10.1053/j.gastro.2005.03.046. [DOI] [PubMed] [Google Scholar]
- 55.Braun J, Targan SR. Multiparameter analysis of immunogenetic mechanisms in clinical diagnosis and management of inflammatory bowel disease. Adv Exp Med Biol. 2006;579:209–218. doi: 10.1007/0-387-33778-4_13. [DOI] [PubMed] [Google Scholar]
- 56.Nikolaus S, Schreiber S. Diagnostics of inflammatory bowel disease. Gastroenterology. 2007;133:1670–1689. doi: 10.1053/j.gastro.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 57.Oriuchi T, Hiwatashi N, Kinouchi Y, et al. Clinical course and longterm prognosis of Japanese patients with Crohn's disease: predictive factors, rates of operation, and mortality. J Gastroenterol. 2003;38:942–953. doi: 10.1007/s00535-003-1177-9. [DOI] [PubMed] [Google Scholar]
- 58.Vind I, Riis L, Jess T, et al. Increasing incidences of inflammatory bowel disease and decreasing surgery rates in Copenhagen City and County, 2003-2005: a population-based study from the Danish Crohn colitis database. Am J Gastroenterol. 2006;101:1274–1282. doi: 10.1111/j.1572-0241.2006.00552.x. [DOI] [PubMed] [Google Scholar]
- 59.Croucher PJ, Mascheretti S, Hampe J, et al. Haplotype structure and association to Crohn's disease of CARD15 mutations in two ethnically divergent populations. Eur J Hum Genet. 2003;11:6–16. doi: 10.1038/sj.ejhg.5200897. [DOI] [PubMed] [Google Scholar]
- 60.Yang SK, Lee SG, Cho YK, Lim J, Lee I, Song K. Association of TNF-alpha/LTA polymorphisms with Crohn's disease in Koreans. Cytokine. 2006;35:13–20. doi: 10.1016/j.cyto.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 61.Yang SK, Lim J, Chang HS, et al. Association of TNFSF15 with Crohn's disease in Koreans. Am J Gastroenterol. 2008;103:1437–1442. doi: 10.1111/j.1572-0241.2007.01752.x. [DOI] [PubMed] [Google Scholar]
- 62.Yang SK, Park M, Lim J, et al. Contribution of IL23R but not ATG16L1 to Crohn's disease susceptibility in Koreans. Inflamm Bowel Dis. 2009;15:1385–1390. doi: 10.1002/ibd.20921. [DOI] [PubMed] [Google Scholar]
- 63.Yoshitake S, Kimura A, Okada M, Yao T, Sasazuki T. HLA class II alleles in Japanese patients with inflammatory bowel disease. Tissue Antigens. 1999;53:350–358. doi: 10.1034/j.1399-0039.1999.530405.x. [DOI] [PubMed] [Google Scholar]
- 64.Masuda H, Nakamura Y, Tanaka T, Hayakawa S. Distinct relationship between HLA-DR genes and intractability of ulcerative colitis. Am J Gastroenterol. 1994;89:1957–1962. [PubMed] [Google Scholar]
- 65.Myung SJ, Yang SK, Jung HY, et al. HLA-DRB1*1502 confers susceptibility to ulcerative colitis, but is negatively associated with its intractability: a Korean study. Int J Colorectal Dis. 2002;17:233–237. doi: 10.1007/s00384-001-0381-4. [DOI] [PubMed] [Google Scholar]
- 66.Satsangi J, Welsh KI, Bunce M, et al. Contribution of genes of the major histocompatibility complex to susceptibility and disease phenotype in inflammatory bowel disease. Lancet. 1996;347:1212–1217. doi: 10.1016/s0140-6736(96)90734-5. [DOI] [PubMed] [Google Scholar]
- 67.De La Concha EG, Fernandez-Arquero M, Santa-Cruz S, et al. Positive and negative associations of distinct HLA-DR2 subtypes with ulcerative colitis (UC) Clin Exp Immunol. 1997;108:392–395. doi: 10.1046/j.1365-2249.1997.3951285.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Cottone M, Bunce M, Taylor CJ, Ting A, Jewell DP. Ulcerative colitis and HLA phenotype. Gut. 1985;26:952–954. doi: 10.1136/gut.26.9.952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Truelove SC, Witts LJ. Cortisone in ulcerative colitis; final report on a therapeutic trial. Br Med J. 1955;2:1041–1048. doi: 10.1136/bmj.2.4947.1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Schroeder KW, Tremaine WJ, Ilstrup DM. Coated oral 5-aminosalicylic acid therapy for mildly to moderately active ulcerative colitis. A randomized study. N Engl J Med. 1987;317:1625–1629. doi: 10.1056/NEJM198712243172603. [DOI] [PubMed] [Google Scholar]
- 71.Shivananda S, Lennard-Jones J, Logan R, et al. Incidence of inflammatory bowel disease across Europe: is there a difference between north and south? Results of the European Collaborative Study on Inflammatory Bowel Disease (EC-IBD) Gut. 1996;39:690–697. doi: 10.1136/gut.39.5.690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Modigliani R, Mary JY, Simon JF, et al. Groupe d'Etude Therapeutique des Affections Inflammatoires Digestives. Clinical, biological, and endoscopic picture of attacks of Crohn's disease. Evolution on prednisolone. Gastroenterology. 1990;98:811–818. doi: 10.1016/0016-5085(90)90002-i. [DOI] [PubMed] [Google Scholar]
- 73.Fiocchi C. Inflammatory bowel disease: etiology and pathogenesis. Gastroenterology. 1998;115:182–205. doi: 10.1016/s0016-5085(98)70381-6. [DOI] [PubMed] [Google Scholar]
- 74.Gasche C, Scholmerich J, Brynskov J, et al. A simple classification of Crohn's disease: report of the Working Party for the World Congresses of Gastroenterology, Vienna 1998. Inflamm Bowel Dis. 2000;6:8–15. doi: 10.1097/00054725-200002000-00002. [DOI] [PubMed] [Google Scholar]
- 75.Louis E, Collard A, Oger AF, Degroote E, Aboul Nasr El Yafi FA, Belaiche J. Behaviour of Crohn's disease according to the Vienna classification: changing pattern over the course of the disease. Gut. 2001;49:777–782. doi: 10.1136/gut.49.6.777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Satsangi J, Silverberg MS, Vermeire S, Colombel JF. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut. 2006;55:749–753. doi: 10.1136/gut.2005.082909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Han JY. Clinical outcome of Crohn's disease. Korean J Gastroenterol. 2002;40(Suppl 5):187A. [Google Scholar]
- 78.Best WR, Becktel JM, Singleton JW. Rederived values of the eight coefficients of the Crohn's Disease Activity Index (CDAI) Gastroenterology. 1979;77:843–846. [PubMed] [Google Scholar]
- 79.Sandborn WJ, Feagan BG, Hanauer SB, et al. A review of activity indices and efficacy endpoints for clinical trials of medical therapy in adults with Crohn's disease. Gastroenterology. 2002;122:512–530. doi: 10.1053/gast.2002.31072. [DOI] [PubMed] [Google Scholar]
- 80.Harvey RF, Bradshaw JM. A simple index of Crohn's-disease activity. Lancet. 1980;1:514. doi: 10.1016/s0140-6736(80)92767-1. [DOI] [PubMed] [Google Scholar]
- 81.Van Hees PA, Van Lier HJ, Van Elteren PH, et al. Effect of sulphasalazine in patients with active Crohn's disease: a controlled double-blind study. Gut. 1981;22:404–409. doi: 10.1136/gut.22.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Anthonisen P, Barany F, Folkenborg O, et al. The clinical effect of salazosulphapyridine (Salazopyrin r) in Crohn's disease. A controlled double-blind study. Scand J Gastroenterol. 1974;9:549–554. [PubMed] [Google Scholar]
- 83.Summers RW, Switz DM, Sessions JT, Jr, et al. National Cooperative Crohn's Disease Study: results of drug treatment. Gastroenterology. 1979;77:847–869. [PubMed] [Google Scholar]
- 84.Malchow H, Ewe K, Brandes JW, et al. European Cooperative Crohn's Disease Study (ECCDS): results of drug treatment. Gastroenterology. 1984;86:249–266. [PubMed] [Google Scholar]
- 85.Tremaine WJ, Schroeder KW, Harrison JM, Zinsmeister AR. A randomized, double-blind, placebo-controlled trial of the oral mesalamine (5-ASA) preparation, Asacol, in the treatment of symptomatic Crohn's colitis and ileocolitis. J Clin Gastroenterol. 1994;19:278–282. doi: 10.1097/00004836-199412000-00003. [DOI] [PubMed] [Google Scholar]
- 86.Singleton JW, Hanauer SB, Gitnick GL, et al. Mesalamine capsules for the treatment of active Crohn's disease: results of a 16-week trial. Pentasa Crohn's Disease Study Group. Gastroenterology. 1993;104:1293–1301. doi: 10.1016/0016-5085(93)90337-c. [DOI] [PubMed] [Google Scholar]
- 87.Hanauer SB, Stromberg U. Oral Pentasa in the treatment of active Crohn's disease: A meta-analysis of double-blind, placebo-controlled trials. Clin Gastroenterol Hepatol. 2004;2:379–388. doi: 10.1016/s1542-3565(04)00122-3. [DOI] [PubMed] [Google Scholar]
- 88.Sutherland L, Singleton J, Sessions J, et al. Double blind, placebo controlled trial of metronidazole in Crohn's disease. Gut. 1991;32:1071–1075. doi: 10.1136/gut.32.9.1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ambrose NS, Allan RN, Keighley MR, et al. Antibiotic therapy for treatment in relapse of intestinal Crohn's disease: a prospective randomized study. Dis Colon Rectum. 1985;28:81–85. doi: 10.1007/BF02552649. [DOI] [PubMed] [Google Scholar]
- 90.Blichfeldt P, Blomhoff JP, Myhre E, Gjone E. Metronidazole in Crohn's disease: a double blind cross-over clinical trial. Scand J Gastroenterol. 1978;13:123–127. doi: 10.3109/00365527809179816. [DOI] [PubMed] [Google Scholar]
- 91.Steinhart AH, Feagan BG, Wong CJ, et al. Combined budesonide and antibiotic therapy for active Crohn's disease: a randomized controlled trial. Gastroenterology. 2002;123:33–40. doi: 10.1053/gast.2002.34225. [DOI] [PubMed] [Google Scholar]
- 92.Greenberg GR, Feagan BG, Martin F, et al. Oral budesonide for active Crohn's disease: Canadian Inflammatory Bowel Disease Study Group. N Engl J Med. 1994;331:836–841. doi: 10.1056/NEJM199409293311303. [DOI] [PubMed] [Google Scholar]
- 93.Tremaine WJ, Hanauer SB, Katz S, et al. Budesonide CIR capsules (once or twice daily divided-dose) in active Crohn's disease: a randomized placebo-controlled study in the United States. Am J Gastroenterol. 2002;97:1748–1754. doi: 10.1111/j.1572-0241.2002.05835.x. [DOI] [PubMed] [Google Scholar]
- 94.Kane SV, Schoenfeld P, Sandborn WJ, Tremaine W, Hofer T, Feagan BG. The effectiveness of budesonide therapy for Crohn's disease. Aliment Pharmacol Ther. 2002;16:1509–1517. doi: 10.1046/j.1365-2036.2002.01289.x. [DOI] [PubMed] [Google Scholar]
- 95.Lichtenstein GR, Abreu MT, Cohen R, Tremaine W. American Gastroenterological Association Institute medical position statement on corticosteroids, immunomodulators, and infliximab in inflammatory bowel disease. Gastroenterology. 2006;130:935–939. doi: 10.1053/j.gastro.2006.01.047. [DOI] [PubMed] [Google Scholar]
- 96.Travis SP, Stange EF, Lemann M, et al. European evidence based consensus on the diagnosis and management of Crohn's disease: current management. Gut. 2006;55(Suppl 1):i16–i35. doi: 10.1136/gut.2005.081950b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hyun JG, Kim JJ, Kim YH, et al. Analysis of clinical, biochemical and pathologic factors according to the response to initial steroid therapy in active Crohn's disease. Korean J Gastrointest Endosc. 2001;22:406–410. [Google Scholar]
- 98.Kim DH. Response rate to oral steroid therapy in patients with Crohn's disease and its clinical predictive factors [master's thesis] Seoul: Yonsei University; 2009. [Google Scholar]
- 99.Lee KM, Kim JS, Ye BD, et al. Infliximab treatment in Crohn's disease: a nation-wide survey in Korea; Paper presented at: The 3rd Japan-Korea IBD symposium; 2008 Sep 20; Seoul, Korea: [Google Scholar]
- 100.Health Insurance Review and Assessment Service [Internet] Seoul: Health Insurance Review and Assessment Service; c2009. Available from: http://www.hira.or.kr/ [Google Scholar]
- 101.Ahn HS, Lee SK, Kim HJ, et al. Risk of postoperative infection in patients with inflammatory bowel disease. Korean J Gastroenterol. 2006;48:306–312. [PubMed] [Google Scholar]
- 102.Sandborn WJ, Lofberg R, Feagan BG, Hanauer SB, Campieri M, Greenberg GR. Budesonide for maintenance of remission in patients with Crohn's disease in medically induced remission: a predetermined pooled analysis of four randomized, double-blind, placebo-controlled trials. Am J Gastroenterol. 2005;100:1780–1787. doi: 10.1111/j.1572-0241.2005.41992.x. [DOI] [PubMed] [Google Scholar]
- 103.Present DH, Korelitz BI, Wisch N, Glass JL, Sachar DB, Pasternack BS. Treatment of Crohn's disease with 6-mercaptopurine: a long-term, randomized, double-blind study. N Engl J Med. 1980;302:981–987. doi: 10.1056/NEJM198005013021801. [DOI] [PubMed] [Google Scholar]
- 104.Hanauer SB, Sandborn W. Management of Crohn's disease in adults. Am J Gastroenterol. 2001;96:635–643. doi: 10.1111/j.1572-0241.2001.3671_c.x. [DOI] [PubMed] [Google Scholar]
- 105.Candy S, Wright J, Gerber M, Adams G, Gerig M, Goodman R. A controlled double blind study of azathioprine in the management of Crohn's disease. Gut. 1995;37:674–678. doi: 10.1136/gut.37.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Lemann M, Mary JY, Colombel JF, et al. A randomized, double-blind, controlled withdrawal trial in Crohn's disease patients in long-term remission on azathioprine. Gastroenterology. 2005;128:1812–1818. doi: 10.1053/j.gastro.2005.03.031. [DOI] [PubMed] [Google Scholar]
- 107.Gearry RB, Barclay ML. Azathioprine and 6-mercaptopurine pharmacogenetics and metabolite monitoring in inflammatory bowel disease. J Gastroenterol Hepatol. 2005;20:1149–1157. doi: 10.1111/j.1440-1746.2005.03832.x. [DOI] [PubMed] [Google Scholar]
- 108.Kim JH, Cheon JH, Kim WH. The frequency and the course of the adverse effects of azathioprine/6-mercaptopurine treatment in patients with inflammatory bowel disease. Korean J Gastroenterol. 2008;51:291–297. [PubMed] [Google Scholar]
- 109.Jun JB, Cho DY, Kang C, Bae SC. Thiopurine S-methyltransferase polymorphisms and the relationship between the mutant alleles and the adverse effects in systemic lupus erythematosus patients taking azathioprine. Clin Exp Rheumatol. 2005;23:873–876. [PubMed] [Google Scholar]
- 110.Baumgart DC, Sandborn WJ. Inflammatory bowel disease: clinical aspects and established and evolving therapies. Lancet. 2007;369:1641–1657. doi: 10.1016/S0140-6736(07)60751-X. [DOI] [PubMed] [Google Scholar]
- 111.Smolen JS, Aletaha D, Koeller M, Weisman MH, Emery P. New therapies for treatment of rheumatoid arthritis. Lancet. 2007;370:1861–1874. doi: 10.1016/S0140-6736(07)60784-3. [DOI] [PubMed] [Google Scholar]
- 112.Olaussen RW, Karlsson MR, Lundin KE, Jahnsen J, Brandtzaeg P, Farstad IN. Reduced chemokine receptor 9 on intraepithelial lymphocytes in celiac disease suggests persistent epithelial activation. Gastroenterology. 2007;132:2371–2382. doi: 10.1053/j.gastro.2007.04.023. [DOI] [PubMed] [Google Scholar]
- 113.Salmi M, Jalkanen S. Developmental regulation of the adhesive and enzymatic activity of vascular adhesion protein-1 (VAP-1) in humans. Blood. 2006;108:1555–1561. doi: 10.1182/blood-2005-11-4599. [DOI] [PubMed] [Google Scholar]
- 114.Silverman J, Liu Q, Bakker A, et al. Multivalent avimer proteins evolved by exon shuffling of a family of human receptor domains. Nat Biotechnol. 2005;23:1556–1561. doi: 10.1038/nbt1166. [DOI] [PubMed] [Google Scholar]
- 115.Carter MJ, Lobo AJ, Travis SP. Guidelines for the management of inflammatory bowel disease in adults. Gut. 2004;53(Suppl 5):V1–V16. doi: 10.1136/gut.2004.043372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Sandborn WJ, Fazio VW, Feagan BG, Hanauer SB. AGA technical review on perianal Crohn's disease. Gastroenterology. 2003;125:1508–1530. doi: 10.1016/j.gastro.2003.08.025. [DOI] [PubMed] [Google Scholar]
- 117.Hurst RD, Molinari M, Chung TP, Rubin M, Michelassi F. Prospective study of the features, indications, and surgical treatment in 513 consecutive patients affected by Crohn's disease. Surgery. 1997;122:661–667. doi: 10.1016/s0039-6060(97)90071-4. [DOI] [PubMed] [Google Scholar]
- 118.Michelassi F, Block GE. Surgical management of Crohn's disease. Adv Surg. 1993;26:307–322. [PubMed] [Google Scholar]
- 119.Prantera C. Indications for surgery in Crohn's disease. Am J Gastroenterol. 1990;85:900–901. [PubMed] [Google Scholar]
- 120.Broe PJ, Bayless TM, Cameron JL. Crohn's disease: are enteroenteral fistulas an indication for surgery? Surgery. 1982;91:249–253. [PubMed] [Google Scholar]
- 121.Ribeiro MB, Greenstein AJ, Yamazaki Y, Aufses AH., Jr Intra-abdominal abscess in regional enteritis. Ann Surg. 1991;213:32–36. doi: 10.1097/00000658-199101000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Gardiner KR, Dasari BV. Operative management of small bowel Crohn's disease. Surg Clin North Am. 2007;87:587–610. doi: 10.1016/j.suc.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 123.Kim DH, Cheon JH, Moon CM, et al. Clinical efficacy of nonsurgical treatment of Crohn's disease-related intraabdominal abscess. Korean J Gastroenterol. 2009;53:29–35. [PubMed] [Google Scholar]
- 124.Bernell O, Lapidus A, Hellers G. Risk factors for surgery and postoperative recurrence in Crohn's disease. Ann Surg. 2000;231:38–45. doi: 10.1097/00000658-200001000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Kim CG, Kim JW, Kim HD, et al. Clinical features of Crohn's disease in Korea. Korean J Gastroenterol. 2002;40:173–180. [Google Scholar]
- 126.Kim HA, Chung SS, Kim KH, Lee RA. The change of the clinical features that Crohn's disease treated by surgery. J Korean Surg Soc. 2005;69:135–138. [Google Scholar]
- 127.Cohen RD, Woseth DM, Thisted RA, Hanauer SB. A meta-analysis and overview of the literature on treatment options for left-sided ulcerative colitis and ulcerative proctitis. Am J Gastroenterol. 2000;95:1263–1276. doi: 10.1111/j.1572-0241.2000.01940.x. [DOI] [PubMed] [Google Scholar]
- 128.Stein RB, Hanauer SB. Medical therapy for inflammatory bowel disease. Gastroenterol Clin North Am. 1999;28:297–321. doi: 10.1016/s0889-8553(05)70058-3. [DOI] [PubMed] [Google Scholar]
- 129.Campieri M, Lanfranchi GA, Bazzocchi G, et al. Treatment of ulcerative colitis with high-dose 5-aminosalicylic acid enemas. Lancet. 1981;2:270–271. doi: 10.1016/s0140-6736(81)90523-7. [DOI] [PubMed] [Google Scholar]
- 130.Marshall JK, Irvine EJ. Rectal corticosteroids versus alternative treatments in ulcerative colitis: a meta-analysis. Gut. 1997;40:775–781. doi: 10.1136/gut.40.6.775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Safdi M, DeMicco M, Sninsky C, et al. A double-blind comparison of oral versus rectal mesalamine versus combination therapy in the treatment of distal ulcerative colitis. Am J Gastroenterol. 1997;92:1867–1871. [PubMed] [Google Scholar]
- 132.Faubion WA, Jr, Loftus EV, Jr, Harmsen WS, Zinsmeister AR, Sandborn WJ. The natural history of corticosteroid therapy for inflammatory bowel disease: a population-based study. Gastroenterology. 2001;121:255–260. doi: 10.1053/gast.2001.26279. [DOI] [PubMed] [Google Scholar]
- 133.Lee DH, Lee JH, Park DY, et al. Experience of cyclosporine A therapy in severe ulcerative colitis refractory to steroid treatment. Korean J Gastroenterol. 1997;30:58–65. [Google Scholar]
- 134.Chung GE, Cheon JH, Lee JY, et al. Efficacy of combination of intravenous cyclosporin A and steroid therapy versus prolonged intravenous steroid therapy alone in patients with severe ulcerative colitis refractory to initial intravenous steroid therapy. Korean J Gastroenterol. 2006;48:263–268. [PubMed] [Google Scholar]
- 135.Hanauer S, Good LI, Goodman MW, et al. Long-term use of mesalamine (Rowasa) suppositories in remission maintenance of ulcerative proctitis. Am J Gastroenterol. 2000;95:1749–1754. doi: 10.1111/j.1572-0241.2000.02185.x. [DOI] [PubMed] [Google Scholar]
- 136.d'Albasio G, Paoluzi P, Campieri M, et al. The Italian IBD Study Group. Maintenance treatment of ulcerative proctitis with mesalazine suppositories: a double-blind placebo-controlled trial. Am J Gastroenterol. 1998;93:799–803. doi: 10.1111/j.1572-0241.1998.228_a.x. [DOI] [PubMed] [Google Scholar]
- 137.Rutgeerts P, Sandborn WJ, Feagan BG, et al. Infliximab for induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2005;353:2462–2476. doi: 10.1056/NEJMoa050516. [DOI] [PubMed] [Google Scholar]
- 138.Berger M, Gribetz D, Korelitz BI. Growth retardation in children with ulcerative colitis: the effect of medical and surgical therapy. Pediatrics. 1975;55:459–467. [PubMed] [Google Scholar]
- 139.Gumaste V, Sachar DB, Greenstein AJ. Benign and malignant colorectal strictures in ulcerative colitis. Gut. 1992;33:938–941. doi: 10.1136/gut.33.7.938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Cohen JL, Strong SA, Hyman NH, et al. Practice parameters for the surgical treatment of ulcerative colitis. Dis Colon Rectum. 2005;48:1997–2009. doi: 10.1007/s10350-005-0180-z. [DOI] [PubMed] [Google Scholar]
- 141.Park IJ, Yu CS, Kim HC, et al. Analysis of pouchitis after restorative proctocolectomy. Korean J Gastroenterol. 2005;46:99–104. [PubMed] [Google Scholar]
- 142.Moum B, Ekbom A, Vatn MH, et al. Clinical course during the 1st year after diagnosis in ulcerative colitis and Crohn's disease: results of a large, prospective population-based study in southeastern Norway, 1990-93. Scand J Gastroenterol. 1997;32:1005–1012. doi: 10.3109/00365529709011217. [DOI] [PubMed] [Google Scholar]
- 143.Leijonmarck CE, Persson PG, Hellers G. Factors affecting colectomy rate in ulcerative colitis: an epidemiologic study. Gut. 1990;31:329–333. doi: 10.1136/gut.31.3.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Langholz E, Munkholm P, Davidsen M, Binder V. Course of ulcerative colitis: analysis of changes in disease activity over years. Gastroenterology. 1994;107:3–11. doi: 10.1016/0016-5085(94)90054-x. [DOI] [PubMed] [Google Scholar]
- 145.Sinclair TS, Brunt PW, Mowat NA. Nonspecific proctocolitis in northeastern Scotland: a community study. Gastroenterology. 1983;85:1–11. [PubMed] [Google Scholar]
- 146.Farmer RG, Easley KA, Rankin GB. Clinical patterns, natural history, and progression of ulcerative colitis: a long-term follow-up of 1116 patients. Dig Dis Sci. 1993;38:1137–1146. doi: 10.1007/BF01295733. [DOI] [PubMed] [Google Scholar]
- 147.Hendriksen C, Kreiner S, Binder V. Long term prognosis in ulcerative colitis: based on results from a regional patient group from the county of Copenhagen. Gut. 1985;26:158–163. doi: 10.1136/gut.26.2.158. [DOI] [PMC free article] [PubMed] [Google Scholar]