Abstract
The caudate lobe often exhibits enlargement and nodularity in cases of cirrhosis, which makes differentiation of hepatocellular carcinoma from other mass-like lesions of the caudate lobe difficult in cirrhotic patients. A 12×6 cm mass-like enlargement of the caudate lobe was incidentally found by computed tomography in a 38-year-old man suffering from alcoholic liver cirrhosis. Magnetic resonance imaging, liver colloidal scan, and sonoguided liver biopsy were used for the differential diagnosis. A literature review revealed two case reports, all of which (like ours) presented with an enlarged caudate lobe supplied with blood via a branch of the portal vein. Therefore, in cases of giant hyperplasia of the caudate lobe, confirmation of the caudate lobe blood supply and the enhancement pattern might be important for the differentiation.
Keywords: Giant hyperplasia, Caudate lobe, Cirrhosis
INTRODUCTION
In cirrhotic patient, the caudate lobe often enlarged by 2 times of normal.1 Hyperplasia (especially caudate lobe), liver cell adenoma and hepatocelluar carcinoma (HCC) are still difficult to diagnosis preoperatively.2 But enlargement of caudate hyperplasia over 6 cm in size is extremely rare. We report a case of giant hyperplastic change of the caudate lobe (more than 12 cm) in a cirrhotic patient with literature review.
CASE REPORT
A 38-year-old man was admitted to our hospital with complaints of mental change and dyspnea for 4 days. Three months before the admission he had been diagnosed as alcoholic liver cirrhosis with massive ascites, but he had received no specific treatment. On his past history, he was severe alcohol abuser (drink 45 g/day for 10 years) and current heavy smoker (10 pack years). His blood pressure was 100/80 mmHg; heart rate 91 beats/min; respiratory rate 32 breaths/min; and body temperature 36.9℃. He showed acutely ill appearance. Physical examination showed confused mentality, icteric sclera, moderate abdominal distension with shifting dullness, hepatomegaly. Laboratory finding were as follows: WBC 6,840/mm3, hemoglobin 10.3 g/dL, platelet 81,000/mm3, total protein 6.3 g/dL, albumin 2.6 g/dL, ALT/AST 186/897 IU/L, LDH/ALP 1,161/498 IU/L, total bilirubin 13.3 mg/dL, creatinine 1.5 mg/dL, prothrombin time 40.8 seconds, serum ammonia 96 µg/dL (normal range: 30-86 µg/dL), alpha-fetoprotein 3.8 ng/dL (normal range: 0-8.1 ng/dL), HBsAg/Ab (-/+), anti-HCV antibody (-). Ascites showed yellowish color and analysis showed WBC 15/µL, albumin 0.8 g/dL (serum ascites albumin gradient: 1.7). Chest radiograph finding showed right pleural effusion. Simple abdomen showed mild paralytic ileus. Gastroenteroscopy showed mild esophageal varix. Abdominal enhanced computed tomography (CT) showed low attenuated 12×6 cm sized mass like lesion, needed to differential diagnosis from other tumorous condition of caudate lobe (Fig. 1). Then, we performed liver colloid scan and magnetic resonance (MR) image to distinguish the mass from the malignancy. On MR image, focal lobulated enlargement of caudate lobe of liver with T1 high, T2 low signal intensity and suppression during fat suppression (Fig. 2). On colloid scan, it showed same degree uptake compared with normal liver parenchyma (Fig. 3). It showed compatible feature of hyperplasia of liver. The ultrasound-guided liver biopsy was done for the confirmative diagnosis. The histological examination of the biopsy revealed mild macrovesicular fatty metamorphosis The cirrhotic nodules consist of regernerative hyperplastic hepatocytes without atypia. The density of hepatocyte of regenerative nodule is higher than that of usual cirrhotic nodule (Fig. 3). Therefore, we diagnosed the patient as having giant hyperplasia of caudate lobe and cirrhosis.
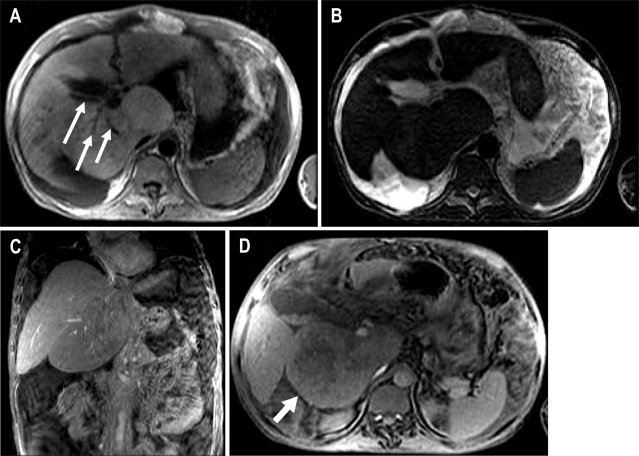
Fig. 1.
(A) Postcontrast CT (arterial phase) shows large, low attenuated mass (12×6 cm sized) in the caudate lobe (arrow). It shows no arterial enhancement. (B) Postcontrast CT (portal phase) shows that the mass like lesion of caudate lobe dose not contained a portal branch. (C) Coronal T2 weighted magnetic resonance image shows isointensity of the caudate lobe. (D) T1 weighted magnetic resonance image shows hyperintensity of the caudate lobe.
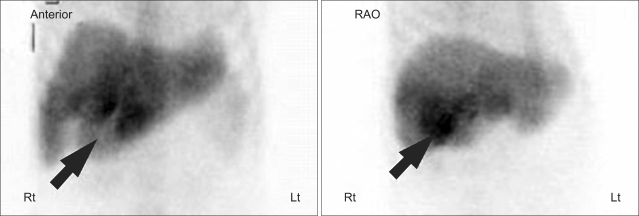
Fig. 2.
Technetium-tin colloid scintigram shows that normal uptake of the enlarged caudate lobe (arrow) and shows same colloid uptake level compared with normal parenchyma.
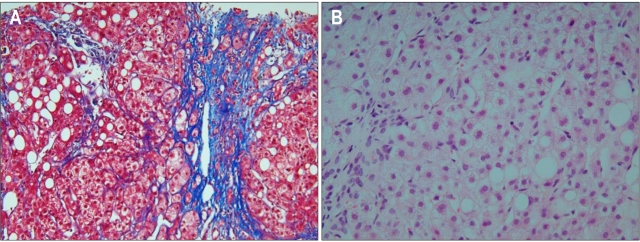
Fig. 3.
(A) Histological examination of ultrasound guided liver biopsy shows micronodular cirrhosis (Masson-trichrome stain, ×100). (B) It shows that mild macrovesicular fatty metamorphosis and many bile pigments with piecemeal necrosis (H&E stain, ×400).
DISCUSSION
The caudate lobe is often enlarged in cases of cirrhosis and the Budd-Chiari Syndrome.1,3-5 The reason that only the caudate lobe shows such huge hyperplasia is unclear. However, differences in different hormones, nutritional elements, and hepatotropic factors in the portal blood flow between the caudate lobe and the other segment of the liver may correlate with the hyperplastic change of the caudate.6 According to Couinaud, the caudate lobe receive a specific pedicle independent of the portal vein and the right gastric vein (or pyloric vein) or parabiliary venous system occasionally drain directly into the posterior edge of the medial segment (segment IV) or the caudate lobe (segment I).7
It is reported that the segment involved with aberrant venous drainage may show various morphologic changes, including focal spared area in fatty liver,8,9 focal fatty infiltration,10 and hyperplastic change11 etc. So, liver biopsy often perform to distinguish from malignant mass. However there are only two case report regarding to giant hyperplasia of caudate lobe. Ohtomo et al. reported two cases about 6-7 cm pseudotumorous lesions of the paracaval portion of the caudate lobe.12 And they pointed out the typical enhancing pattern and presence of a portal vein branch penetrating the center of the enlarged mass lesion. However, it was not certain whether the authors were reporting adenomatous hyperplasia in the caudate lobe, or marked hypertrophy of the caudate lobe which resembled a tumor. According to the radiology and histology given, would be suspected that the former is the case. Gabata et al. also reported giant hyperplastic change of the caudate lobe of the liver are presented in a patient with liver cirrhosis.6 In addition, they insisted that caudate hyperplastic change may be correlated to anomalous caudate portal vein branch. All of cases, including our case, show similar imaging feature that the area with hyperplastic change are hypodense on computed tomography without enhancement and usually contain portal branch. It also showed that hyperintense signal intensity on T1-weighted, hypointense on T2-weighted M.R. images (Fig. 1). It seemed that the typical enhancing pattern, the presence of a portal vein branch ramifying from the left or right main portal vein and penetrating the center of the lesion very helpful to distinguish pseudotumorous enlagement of the caudate lobe.
In conclusion, in case of giant hyperplasia of caudate lobe, confirmation of caudate lobe blood supply and enhancement pattern may be important to differentiation.
References
- 1.Torres WE, Whitmire LF, Gedgaudas-McClees K, Bernardino ME. Computed tomography of hepatic morphologic changes in cirrhosis of the liver. J Comput Assist Tomogr. 1986;10:47–50. doi: 10.1097/00004728-198601000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Kerlin P, Davis GL, McGill DB, Weiland LH, Adson MA, Sheedy PF., 2nd Hepatic adenoma and focal nodular hyperplasia: clinical, pathologic, and radiologic features. Gastroenterology. 1983;84:994–1002. [PubMed] [Google Scholar]
- 3.Mathieu D, Vasile N, Menu Y, Van Beers B, Lorphelin JM, Pringot J. Budd-Chiari syndrome: dynamic CT. Radiology. 1987;165:409–413. doi: 10.1148/radiology.165.2.3659365. [DOI] [PubMed] [Google Scholar]
- 4.Vogelzang RL, Anschuetz SL, Gore RM. Budd-Chiari syndrome: CT observations. Radiology. 1987;163:329–333. doi: 10.1148/radiology.163.2.3562813. [DOI] [PubMed] [Google Scholar]
- 5.Awaya H, Mitchell DG, Kamishima T, Holland G, Ito K, Matsumoto T. Cirrhosis: modified caudate-right lobe ratio. Radiology. 2002;224:769–774. doi: 10.1148/radiol.2243011495. [DOI] [PubMed] [Google Scholar]
- 6.Gabata T, Matsui O, Kadoya M, et al. Giant hyperplasia of the caudate lobe of the cirrhotic liver: correlation with an anomaly of the caudate portal branch. Abdom Imaging. 1999;24:153–156. doi: 10.1007/s002619900465. [DOI] [PubMed] [Google Scholar]
- 7.Couinaud C. The parabiliary venous system. Surg Radiol Anat. 1988;10:311–316. doi: 10.1007/BF02107904. [DOI] [PubMed] [Google Scholar]
- 8.Franceschini LJ, Ortale JR. Ramification of the portal vein at the porta hepatis in humans. Surg Radiol Anat. 1995;17:35–39. doi: 10.1007/BF01629497. [DOI] [PubMed] [Google Scholar]
- 9.Gabata T, Matsui O, Kadoya M, et al. Aberrant gastric venous drainage in a focal spared area of segment IV in fatty liver: demonstration with color Doppler sonography. Radiology. 1997;203:461–463. doi: 10.1148/radiology.203.2.9114105. [DOI] [PubMed] [Google Scholar]
- 10.Matsui O, Kadoya M, Takahashi S, et al. Focal sparing of segment IV in fatty livers shown by sonography and CT: correlation with aberrant gastric venous drainage. AJR Am J Roentgenol. 1995;164:1137–1140. doi: 10.2214/ajr.164.5.7717220. [DOI] [PubMed] [Google Scholar]
- 11.Kawamori Y, Matsui O, Takahashi S, Kadoya M, Takashima T, Miyayama S. Focal hepatic fatty infiltration in the posterior edge of the medial segment associated with aberrant gastric venous drainage: CT, US, and MR findings. J Comput Assist Tomogr. 1996;20:356–359. doi: 10.1097/00004728-199605000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Ohtomo K, Matsuoka Y, Okada M, et al. Pseudotumorous enlargement of the paracaval portion of the caudate lobe: a report of two cases with CT and MR appearance. Abdom Imaging. 1997;22:398–400. doi: 10.1007/s002619900219. [DOI] [PubMed] [Google Scholar]