Abstract
A 72-year-old female with a colonic laterally spreading tumor (LST) was referred to our department. A total colonoscopy revealed a large nongranular LST, 30 mm in diameter, in the ascending colon. Detailed examination with chromoendoscopy confirmed that the lesion was an intramucosal tumor, and endoscopic submucosal dissection (ESD) was performed. After a circumferential incision around the lifted lesion with a submucosal fluid cushion, diffuse adipose tissue was observed in the submucosal layer beneath the lesion. The endoscopic view was blurred when dissecting the submucosal layer due to fat adhering to the lens. Since this made it difficult to continue the procedures, we infused water into the lumen and kept the endoscope tip immersed in the collected water. The resulting improved view made it possible to complete all procedures without withdrawing the endoscope to wipe the lens. The lesion was successfully resected en bloc without complications. The pathological examination indicated the curative resection of a tubulovillous adenoma. We propose that a submerged ESD could also be an effective procedure for colonic neoplasms with submucosal fat by avoiding blurring of the endoscopic view.
Keywords: Colonoscopy, Colonic neoplasms, Submucosa, Resection, Adipose tissue
INTRODUCTION
Endoscopic submucosal dissection (ESD) is a developing therapeutic procedure for neoplasms in early stage of the gastrointestinal tract. The promising clinical outcomes have been reported, but ESD for colorectal neoplasms is performed at a very limited number of institutions even in Japan.1 One of the major reasons is that there are still some technical difficulties in terms of manipulability of the scope, especially at the proximal colon, including injection, mucosal cutting and submucosal dissection. In dissecting of the submucosal layer, we sometimes encounter unexpected submucosal fat; that is the adipose tissue. In case of lesions with submucosal fat, blurring of view caused by adhesive fat on lens make it difficult to continue procedures smoothly. We present a case of colonic laterally spreading tumor (LST) with submucosal fat, managed with submerging ESD successfully without withdrawing of the endoscope.
CASE REPORT
A 72-year-old obese female with fecal occult blood was referred to our department for total colonoscopy, which revealed a nongranular type LST (LST-NG) at the ascending colon, approximately 30 mm in diameter. Chromoendoscopy revealed type III L pit on the surface. Because LST-NG with III L pit had some possibilities of cancerous lesion, endoscopic submucosal dissection was explained as the treatment procedure and informed consent was obtained for the patient and her family.
A single-channel thin endoscope (PCF-Q240AI; Olympus Co, Tokyo, Japan) with a transparent attachment (D-201-12704; Olympus Co) and a high-frequency automated electrosurgical generator (VIO300D; ERBE Elektromedizin GmbH, Tubingen, Germany) were equipped for the ESD.
A mixture of 1% hyaluronate (Suvenyl; Chugai Pharmaceutical Co, Tokyo, Japan) and 10% glycerin, 5% fructose plus 0.9% saline solution (Glyceol; Chugai Pharmaceutical Co., Tokyo, Japan) was used as the submucosal injection solution. The two solutions were premixed in a ratio of 1:7.
A circumferential incision of mucosa all around the lesion was made by a flex knife (KD-630L; Olympus Co) after a sufficient volume of the submucosal injection. The oral incision of the mucosa was performed, followed by the anal incision at the setting of Endocut I mode (effect 1, duration 3 and interval 3). Submucosal dissection was also performed by a flex knife sequentially at the setting of swift coagulation mode (output 40W, effect 4). To control any visible bleeding, hemostatic forceps (HDB2422W; Pentax Corporation, Tokyo, Japan) were used at the setting of soft coagulation mode (output 50W, effect 5). The details of ESD procedure with a flex knife were described by elsewhere.2
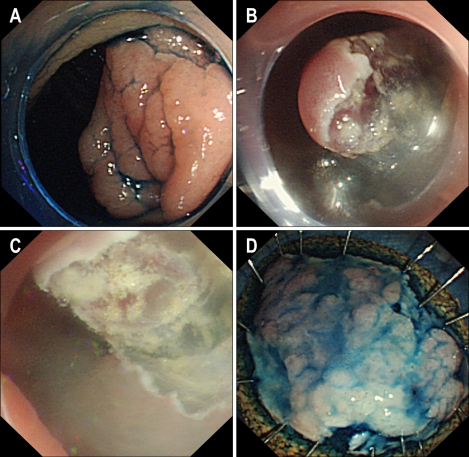
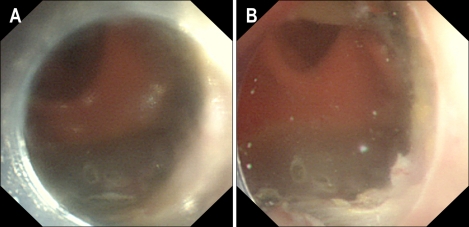
During the submucosal dissection, diffuse submucosal fat was encountered beneath the lesion, and adhesive fat on lens blurred the endoscopic view. Since the lesion was located in the ascending colon, it was quite time-consuming to withdraw the endoscope and wipe the lens repetitively. As a sequence, the lumen of the ascending colon was filled with tap water to keep the endoscope tip immersed in water collects. Suctioning the luminal extra air and changing position were useful for submerging procedure. The improved view through the filling water made it possible to identify the submucosal layer and blood vessels clearly. The bleeding was recognized as a spurting of blood into transparent water, identified with relative ease. The lesion was resected in an en bloc fashion (Fig. 1). After removal of the lesion, submerging observation showed a whole image of the artificial mucosal defect without any bleedings or any perforations (Fig. 2). Any visible vessels within the artificial mucosal defect were treated with hemostatic forceps. Thus, we achieved procedures completely and safely. The total ESD procedure time was approximately 60 minutes. The patient recovered well and discharged on the 6th postoperative day. The resected specimen measured 38×25 mm with the tumor occupying an area of 27 mm in longest diameter. The histological assessment showed a tubulovillous adenoma with moderate atypia. Both the vertical and horizontal margins were free of tumor.
Fig. 1.
Submerged endoscopic submucosal dissection. (A) Colonoscopy revealed a nongranular laterally spreading tumor in the ascending colon that had a flat surface and was approximately 30 mm in diameter. (B) After circumferential incision, the resected piece was separated using a flex knife. Fat adhering to the lens blurred the view during this process. (C) The submerged observation markedly improved the view, with precise identification of the submucosal layer enabling us to achieve the procedures. (D) The lesion was resected en bloc. The pathological examination revealed it to be tubulovillous adenoma with moderate atypia and curative excision.
Fig. 2.
Submerged observation of the artificial mucosal defect. (A) After resecting the lesion, the endoscopic view was blurred by adhering fat. (B) Submerged observation provided a complete image of the artificial mucosal defect without any bleeding or perforation.
DISCUSSION
The adipose tissue in the submucosal layer is one of factors making therapeutic endoscopy more difficult due to blurring of view. On computed tomography studies, the adipose tissue in the submucosal layer is reported to be observed more frequently at the proximal colon than at distal colon.3 Keeping the clear view is essential for therapeutic endoscopy, especially for ESD, but the submucosal fat may disturb the clear endoscopic view. Although the most reliable solution to this problem is wiping the lens after withdrawing the endoscope, at the proximal colon, repetitive cannulation and withdrawing of endoscope is troublesome and painful for patients. In this case, we tried submerging ESD and achieved all the procedures of ESD successfully with improved view through the filled water.
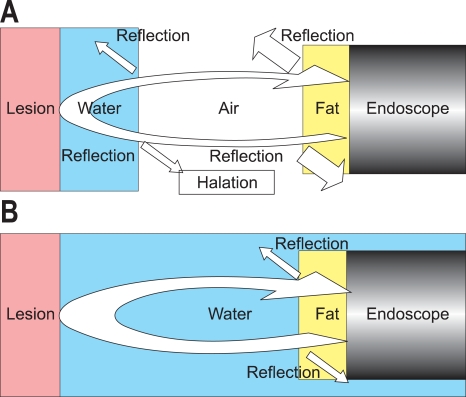
The endoscope illuminates the luminal structures with light guides on the tip, and detects the reflected light on the lesion with its charge coupled device (CCD) on the tip. The adhesive fat on lens not only reduces light intensity due to its turbidity, but also provokes reflection in several boundary lines in the light pathway (Fig. 3A). The reflectance ratio of light is defined with the difference in refractive index of two substances neighboring. The refractive index of air is lower than that of water and that of fat, and the effect of reflection at the boundary line of fat and air is higher than that of fat and water. In the submerging ESD, filling water between the endoscope and the lesion can reduce total reflectance ratio of the light pathway (Fig. 3B). In addition, water on the surface of the lesion can cause the diffuse reflection. This type of reflection can be observed as halations on the video monitor of endoscopy system. In the submerging ESD, filling water also cancels the boundary line with air and reduces diffuse reflection on the surface of the lesion (Fig. 3B). These effects might improve the view and enable us to achieve the procedures more smoothly.
Fig. 3.
Scheme of the reflection boundaries in the light pathway. (A) The adhering fat provokes reflections at the boundary with air. The reflectance ratio is higher than that at the boundary of water and air. (B) Filling water removes the boundary between water and air. Reflections occur only at the boundary with water and fat, for which the reflectance ratio is lower.
A colonoscopic technique with water filling into the lumen is reported in several papers, especially about insertion technique.4 In this insertion technique, complete removal of air is reported to be necessary. They also mention improvement of endoscopic view in the water. However, there are no reports of usefulness of transparent view for therapeutic endoscopy, including ESD.
Of course, filled water can affect transmission of electric current changes generated by high-frequency automated electrosurgical generator. In our case, we equipped the advanced generator with automatically controlled system, which enabled stabilization of cutting and coagulation effects under various conditions.5 Some generators in lower versions may not be expected to have similar effects in submerging ESD.
ESD is still in a developing stage for colonic neoplasms, although promising for large lesions or lesions with submucosal fibrosis. To complete the procedures safely and smoothly, keeping clear view is essential. We propose the submerging ESD can be an effective procedure to avoid blurred view caused by submucosal fat, especially at the proximal colon.
References
- 1.Fujishiro M, Yahagi N, Kakushima N, et al. Outcomes of endoscopic submucosal dissection for colorectal epithelial neoplasms in 200 consecutive cases. Clin Gastroenterol Hepatol. 2007;5:678–683. doi: 10.1016/j.cgh.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 2.Fujishiro M, Yahagi N, Kakushima N, Kodashima S, Ichinose M, Omata M. Successful endoscopic en bloc resection of a large laterally spreading tumor in the rectosigmoid junction by endoscopic submucosal dissection. Gastrointest Endosc. 2006;63:178–183. doi: 10.1016/j.gie.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 3.Harisinghani MG, Wittenberg J, Lee W, Chen S, Gutierrez AL, Mueller PR. Bowel wall fat halo sign in patients without intestinal disease. AJR Am J Roentgenol. 2003;181:781–784. doi: 10.2214/ajr.181.3.1810781. [DOI] [PubMed] [Google Scholar]
- 4.Mizukami T, Yokoyama A, Imaeda H, Kumai K. Collapse-submergence method: simple colonoscopic technique combining water infusion with complete air removal from the rectosigmoid colon. Digest Endosc. 2007;19:43–48. [Google Scholar]
- 5.Kohler A, Maier M, Benz C, Martin WR, Farin G, Riemann JF. A new HF current generator with automatically controlled system (Endocut mode) for endoscopic sphincterotomy--preliminary experience. Endoscopy. 1998;30:351–355. doi: 10.1055/s-2007-1001281. [DOI] [PubMed] [Google Scholar]