Abstract
Background/Aims
Various diagnostic advantages of percutaneous transhepatic cholangioscopy (PTCS) for the determination of the range of tumor and for the characterization of cholangioscopic findings have been reported. The aim of our study is to evaluate the diagnostic and therapeutic role of PTCS in patients with hilar strictures and to investigate its causes.
Methods
We retrospectively studied the medical records and cholangioscopic reports of 177 patients who received PTCS for hilar strictures between January 2000 and December 2005 at Asan Medical Center, Seoul. For each patient, cholagnioscopy, biopsy result, computed tomography (CT) and magnetic resonance cholangiopancreaticography (MRCP), operation, and pathologic reports were collected.
Results
Most patients had malignant hilar strictures or biliary papillomatosis while a few had benign hilar strictures. Presence of tumor vessel on PTCS was a useful diagnostic tool since direct observation of the tumor vessel strongly suggested a malignant tumor in the bile duct. The sensitivity of tumor vessel alone was 56.1%, and sensitivity of PTCS biopsy alone was 76.9%. However, sensitivity of biopsy combined with cholangioscopy of the tumor vessel was 88.4%, which was statistically significant compared with biopsy or tumor vessel alone.
Conclusions
PTCS biopsy combined with cholangioscopic observation was useful in differential diagnosis of hilar strictures. PTCS also had a therapeutic role in some patients with incurable malignant hilar lesion.
Keywords: Cholangiocarcinoma, Cholangiography, Cholangiopancreatography, Magnetic resonance, Neoplasms, Vascular tissue
INTRODUCTION
Numerous inflammatory diseases and malignant or benign bile duct lesions could induce biliary strictures.1 Particularly, biliary structures in the hilar portion or mass lesions require to be differentiated from malignant lesions because 60-70% cholangiocarcinoma has been reported to be developed in the hilar portion.2 Recently, numerous studies reported clinical characteristic, diagnosis and treatment of cholangiocarcinoma. Among them, cholangiocarcinoma in patients, various diagnostic advantages of percutaneous transhepatic cholangioscopy (PTCS) for the determination of the range of tumor as well as for the characterization of cholangioscopic findings have been reported.3-5
Unfortunately, up to the present time, there have been only insufficient reports that describe the role of PTCS in the diagnosis and treatment of hilar strictures. Therefore, we analyzed the diagnostic and therapeutic application of cholangioscopy. In addition, the final pathologic diagnostic finding and the diagnosis by PTCS were compared in patients who underwent surgery.
MATERIALS AND METHODS
1. Study population
Among patients without the past history of biliary duct surgery who underwent PTCS at Asan medical center from January 2000 to December 2005, 177 patients suspected to have hilar lesions were included. Medical records were analyzed retrospectively. Results of imaging studies, such as computed tomography (CT) and magnetic resonance cholangiopancreatography (MRCP), PTCS findings, biopsy results, and findings at surgery and results of pathological examination were obtained.
2. Percutaneous transhepatic biliary drainage
Prior to PTCS, percutaneous transhepatic biliary drainage (PTBD) was performed. First, by abdominal CT, abdominal untrasonography, etc., the dilation result of the intrahepatic bile ducts was assessed, and the feasibility of performing PTBD was determined. As PTBD, using a fluoroscopic imaging technique, a pig-tail catheter (7.5-8.0 Fr, Cook, Bloomington, USA) was inserted to the intrahepatic biliary duct. After performing PTBD, the dilatation of the sinus tract was performed, and a 16-18 Fr catheter was inserted to the fistula that the drainage was performed. Afterward, 7-10 days waiting period was required for the maturation of the sinus tract.
3. PTCS
After the maturation of the sinus tract, PTCS was performed. First, prior to performing PTCS, percutaneous transhepatic cholangiography was performed, and the biliary duct structure and the presence or absence of strictures in the hilar area was assessed, and additionally, the entire biliary ducts were assessed. Subsequently, a cholangioscope (FCN-15X; Pentax, Tokyo, Japan, ECN-1530; Pentax, Japan) was inserted to the sinus tract and PTCS was performed. Lesions in the hilar portion and the biliary duct were assessed macroscopically and biopsy was performed for the lesions suspicious of malignancy. For patients whose strictures in the bile duct were severe and thus difficult to examine, balloon dilatation was performed. After performing balloon dilation, using a cholangioscope, lesions were assessed again, and if needed, biopsy was performed. Presence of the findings that suggest malignancy such as tumor vessels were also evaluated.
4. Treatments and follow up
Surgical procedure was performed on patients who were confirmed to be operable stage hilar cholangiocarcinoma after PTCS. Cases with suspicous cholangiography, CT or MRCP findings were subjected to surgery even if histological results were benign. Preoperative PTCS findings and postoperative histopathological examination results were compared. For those confirmed to have inoperable cholangiocarcinoma by PTCS, CT and MRCP, conservative management was done.
Histological examination was performed also on patients who were not hilar cancer by PTCS but confirmed to be biliary papillomatosis macroscopically. If operable cases in patients with hilar malignancy, surgery was performed, and surgery was performed also on biliary papillomatosis cases if possible. Patients who confirmed to be without hilar strictures and their lesion were found to be benign by PTCS were followed up at outpatient clinics without surgical treatments.
5. Statistical analysis
For statistical analysis, the SPSS program (version 12.0, SPSS Inc, Chicago, Illinois, USA) was used. Individual sensitivity of histological examination and tumor vessel and the sensitivity of the combination of these two were compared by chi-square test. A p-value less than 0.001 was considered to be statiscally significantly different.
RESULTS
Total of 177 patients were included. There were 129 male patients and 48 female patients. Ages of the patients ranged from 23 years old to 81 years old and average age was 59.38 years old. Demographic data of the patients are summarized in Table 1.
Table 1.
Baseline Characteristics of Patients
*Median (range).
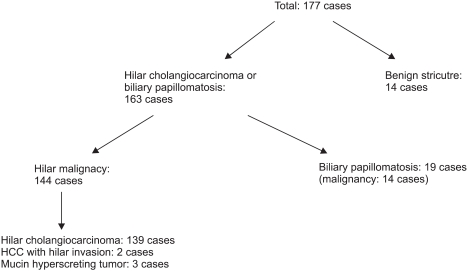
1. Final diagnosis
Among 177 patients, 14 patients (7.9%) were confirmed of benign lesions and the remaining 163 patients (92.1%) were diagnosed of either malignant tumor or the precancerous lesion. Of 19 patients with biliary papillomatosis patients, 14 patients had malignant transformation, which was confirmed by histological examination and the remaining 5 patients did not have malignant lesions. The results of final diagnoses made by PTCS, CT, MRCP and surgery of patients suspected to have hilar lesions were summarized in Fig. 1 and Table 2.
Fig. 1.
Final diagnosis based on computed tomography, magnetic resonance cholangiopancreaticography, percutaneous transhepatic cholangioscopy, and postoperative results.
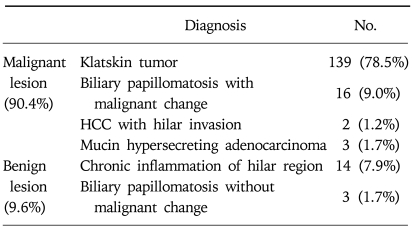
Table 2.
Final Diagnosis: Including CT, MRCP, PTCS, and Postoperative Result
CT, computed tomography; MRCP, magnetic resonance cholangiopancreaticography; PTCS, percutaneous transhepatic cholangioscopy; HCC, hepatocellular carcinoma.
2. Differences between the findings of CT/MRCP and PTCS
Of 177 patients, seven patients had hilar strictures that were considered to be benign by CT or MRCP. Among them, patients found to be malignant after performing PTCS were 5 cases, 1 patient was biliary palillomatosis, and another patient was benign hilar strictures.
There were 165 patients who were strongly suspected of hilar malignancy by CT or MRCP or could not exclude malignancy completely. After PTCS, 12 patients (7.2%) were diagnosed of benign stricture, 139 patients of malignancy, and 14 patients of biliary papillomatosis. Of 12 patients diagnosed of benign strictures, three were lost to follow-up, and the other nine patients are undergoing follow-up at outpatient clinic without any evidence of malignancy. This was summarized in Table 3 and Fig. 2.
Table 3.
The Results of PTCS Biopsy and CT/MRCP
CT, computed tomography; MRCP, magnetic resonance cholangiopancreaticography; PTCS, percutaneous transhepatic cholangioscopy.
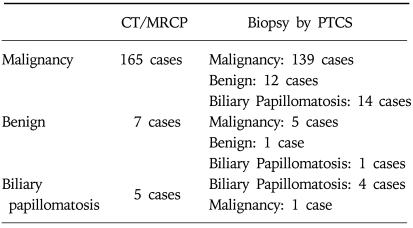
Fig. 2.
Benign hilar lesion noted by percutaneous transhepatic cholangioscopy (PTCS) in a 67-years old man with hilar stricture. (A, B) Hilar stricture is noted in computed tomography (A) and magnetic resonance cholangiopancreaticography (B). PTCS is performed since the CT and MRCP finding could not exclude malignancy. (C) Cholangioscopic finding and biopsy results shows benign hilar stricture.
3. Histological result and subsequent treatments as well as outcomes
Histological examination was done on 162 patients after PTCS. Then, surgery was performed on operable cases with malignancy proven by biopsy or suspected of malignancy by other imaging studies.
Among 15 patients on whom histological examination was not performed, one patient was the case who showed benign findings, and 14 patients were thought to be malignant hilar lesions. Tumor vessels were seen in 8 of 14 patients and histological examination of resected specimen confirmed malingnancy. The remaining 6 patients were strongly suspected of malignancy, but did not undergo surgery since the lesions were unresectable. Of 162 patients performed histological examination by PTCS, 44 patients (27.2%) had histologically benign lesions and the remaining 118 patients (72.8%) malignancy (Table 4).
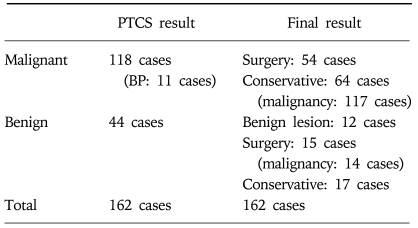
Table 4.
The Result of PTCS Biopsy and Final Diagnosis
BP, biliary papilomatosis; PTCS, percutaneous transhepatic cholangioscopy.
Of 44 patients shown to be benign by biopsy, 15 patients underwent surgery and 29 patients did not undergo surgery. When malignancy was strongly suspcted by CT, MRCP, and cholangiography, the patients underwent surgery even if histological findings were benign. Of 15 patients who underwent surgery, 10 patients underwent radical curative resection and the other 5 patients were found to be inoperable at exploratory laparotomy. Post-surgical histopathological examination revealed malignancy in 14 patients and benign findings in only one patient.
Of 29 patients who did not undergo surgery, 12 patients were thought to have benign biliary duct strictures and did not receive surgery. In the remaining 17 patients, 13 patients were the cases that although they were benign by histological examination, malignancy was suspected by PTCS, CT and MRCP, and 4 patients were biliary papillomatosis patients, and they were the cases received only conservative treatments because their disease stage was inoperable.
In 44 patients (27.2%) whose histological examination results were benign, the cases that were thought to be actually benign clinically were only 29.5% (12/44), and the remaining 70.5% were malignant. However, even in the cases found to be benign by histologial examination, some cases were suspicious to be malignant by PTCS. For example, they were the cases showing tumor vessels, and excluding biliary papillomatosis, among patients suspected to be malignant, tumor vessels were detected in 54.1% (13/24).
Among 118 patients whose result of histological examination applying PTCS was shown to be malignant, surgery was performed on 54 patients. After surgery, the result of 46 patients was confirmed to be malignant, and 3 patients were confirmed to be benign. The remaining 5 patients were those in whom the disease stage was found to be inoperable after surgical procedure and thus terminated the surgery without performing biopsy.
In patients with histologically proven malignancy, 64 patients (54.3%) were inoperable, and they were the cases whose disease was inoperable stage or medically inoperable state. For these patients, only conservative treatments were administered. In addition, among 19 biliary papillomatosis patients, which is precancerous lesions, 11 patients were malignant by histological test using percutaneous transhepatic cholangiography, and in cases performed surgery, 3 cases were found to be malignant additionally.
4. Tumor vessels
Among patients performed PTCS, those with confirmed tumor vessels were reviewed. Among the entire 177 patients, the cases confirmed to show tumor vessels were total 80 cases (45.2%). Analyzing each patient, tumor vessels were seen in 56.1% (78/139) of patients diagnosed as hilar cholangiocarcinom. On the other hand, among patients whose final diagnosis was benign, tumor vessels were suspected in 14.2% (2/14). In addition, as mentioned previously, among individuals shown to be benign by histological examination, except biliary papillomatosis, in the cases suspected to be malignant, 54.1% (13/24) showed tumor vessels, which facilitated the diagnosis. In addition, among patients exhibited tumor vessels, in 8 patients underwent surgery, all were found to be malignant after surgery, which shows that tumor vessels are a very effective predictive factor for diagnosis. The result of the diagnosis of tumor vessels was summarized in Table 5. Furthermore, clinical examples of tumor vessels were described in Fig. 3. Consequently, in the cases whose tumor vessels were positive, the possibility of being malignant was 97.5% (78/80), and in the cases whose tumor vessels were negative, excluding biliary papillomatosis, the possibility of being malignant was 68% (66/97). Therefore, it appears that the possibility of cases with positive tumor vessels to be diagnosed as malignant is very high.
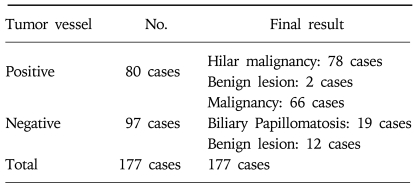
Table 5.
Cholangioscopic Findings of Hilar Tumor: Presence of Tumor Vessel
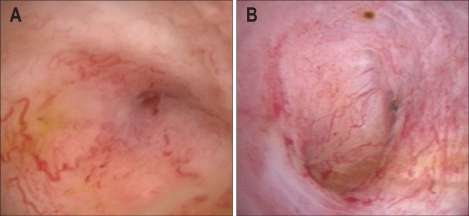
Fig. 3.
Direct cholangioscopic finding of tumor vessel noted during percutaneous transhepatic cholangioscopy (PTCS). (A, B) Adenocarcinoma is proved by PTCS biopsy and post operation pathology.
The diagnostic accuracy determined by the accuracy of the result of tumor vessel, histological examination by PTCS, and combined accuracy of both methods were compared. The positive finding of tumor vessels were shown in 56.1% (78/139) of the entire hilar cholangiocarcinoma, and the diagnosis rate by histological examination was 76.9% (107/139). Nevertheless, diagnosed by the combination of the result of tumor vessels and histological examination by PTCS, it was 88.4% (123/139), and a relatively good diagnosis rate was shown. In comoparison with the diagnosis by either histological examination or tumor vessel alone, it showed a significant different at p<0.001 level.
5. Therapeutic application of PTCS
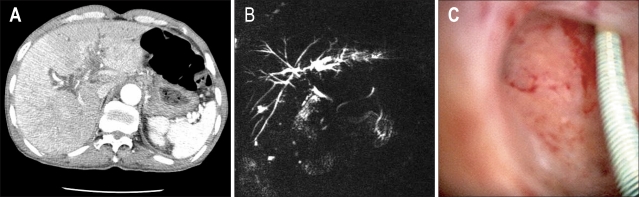
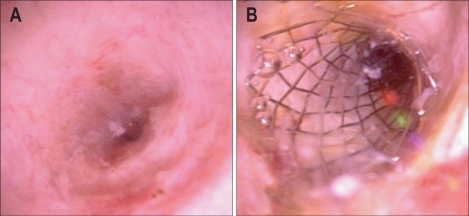
Therapeutic intervention during PTCS was performed in some patients. In 30 patients, ballon dilation of the stricture was performed. In 8 patients, a metal stent was inserted after ballon dilation of the stricture (Fig. 4). In 22 patients, only balloon dilation of the stricture area was performed, therefore, for the area where the access of cholangioscope was difficult due to strictures, histological exmination was performed or dilation of the stricture area was attempted by placing a catheter in the dilated stricture area.
Fig. 4.
Self Extendible metallic stent insertion in 69 years old woman with hilar stricture. (A) CT finding suggesting presence of biliary malignancy and percutaneous transhepatic cholangioscopy (PTCS) demonstrated duct stricture. (B) PTCS biopsy reveals adenocarcinoma. Palliative balloon dilatation and metal stent insertion are performed by using PTCS.
6. Development of complications
Complications occurred in 14 out of 177 patients (7.9%). Hemorrhage was most prevalent and seen in 8 patients, uncontrollable pain during surgery in 5 patients, and leakage of contrast material into the peritoneal cavity due to the insufficient maturation of the sinus tract in 2 patients. All were managed conservatively except for one patient with uncontrollable hemorrhage, who underwent arterial embolization.
DISCUSSION
PTCS is an endoscopic procedure that has been very useful in removal of biliary stones and diagnosis of intrahepatic masses. Moreover, PTCS allows macroscoic examination of the bile duct and histopathologic examination by obtaining biopsy specimens. Therefore, PTCS has been recommended by some investigators prior to surgery for hilar cholangiocarcinoma to assess the extent of the tumor and for early diagnosis.1,6 Through PTCS, assessment of resectability and extent of resection can be made beforehand and survival rate could be improved.6 Unlike malignancies of other sites, determination of feasbile negative resection margin is more important than TMN stage in hilar cholangiocarcinoma. For example, the Bismuth-Corlette IV type cases with the invasion to the second branch of both sides were considered to be unresectable.4,5 In such cases, PTCS allows direct macroscopic examination of the lesions and biopsy for histological examination. Thus, it can be a very useful procedure.
On the other hands, less invasive study such as MRCP may be used to substitute PTCS. Lee et al7 have reported that when findings of PTCS and MRCP were compared in the same patients with hilar cholangiocarcinoma, a high diagnostic concurrence was found. In other words, the Bismuth-Corlette classification obtained by the two methods was compared, and 82.6-100% of substantial concurrence was shown.
CT is a diagnostic modality with very high sensitivity for the diagnosis of intrahepatic cholangiocarcinoma larger than 1 cm. MRCP is an excellent imaging modality that can substitute endoscopic retrograde cholangiopancreatography (ERCP), and it has the advantage that 3-dimensional biliary duct shape could be obtained.8,9 Therefore, CT and MRCP had become essential diagnostic tools not only for the hilar cholangiocarcinoma but also cholangiocarcinoma in general.10 In our study, CT and MRCP had been useful for diagnosis.
Most patients included in our study (167/177, 94.3%) were those in whom CT or MRCP findings suggested hilar malignancy. Thus, PTCS was performed. Most cases whoes were suspected to be malignant by CT or MRCP (155/167, 92.8%) were diagnosed to be malignant. In the entire patients, the cases determined to be benign lesion was small (17/177, 9.6%), and most cases were found to have malignant lesion (160/177, 90.4%). However, some cases of our study suggest that the beneficial effect of PTCS. In some patients, malignant lesions were finally confirmed to be benign lesions by PTCS (12/165, 7.2%), and thus unnecessary surgeries could be avoided. In addition, although a small number, even in patients considered be benign, the actual results were that malignant cases were more abundant. This suggests that for the diagnostic purpose, to add PTCS to radiological tests is useful in some cases. Furthermore, for patients whose results were shown to be malignant, PTCS may be a useful method to determine whether the disease stage is resectable or not.
On the other hand, benign results were obtained from 27.2%, and among them, the cases who were shown to be actual benign were only 29.5%, and the remaining 70.5% patients were thought to be malignant clinically or patients whose malignancy was proven during surgery. Therefore, specificity of histological examination alone could be considered to be low. Nevertheless, even in the cases shown to be benign by histological examination, by determining the findings suspicious to be malignant by cholangioscope, it could be diagnoses as malignant. Tumor vessels have been reported to be a finding that suggests malignancy among PTCS macroscopic findings. According to Kim et al,11 tumor blood vessels could be detected in 61% malignant bile duct strictures, and most cases showing tumor vessels were malignant. In addition, it has been reported that by combining the results of histological examination and tumor vessels, malignant bile duct strictures could be diagnosed in 96%, and thus a better diagnosis rate than either histological examination or tumor vessel results alone could be obtained.11
In our study which focused on hilar lesions, a similar result was obtained, and most patients who showed tumor vessels were the cases with malignant stricture, and in 56.1% (78/139) of the entire hilar cholangiocarcinoma, positive results of tumor vessels were shown. In the entire hilar cholangiocarcinoma patients, the diagnosis rate by histological examination was 76.9% (107/139). However, diagnosed by the combination of the finding of tumor vessels and histological examination, it was 88.4% (123/139), and a relatively good diagnosis rate was shown. The incidence of complications was 7.9% (14 patients), and among them complications requiring emergency treatment were developed only in one patient. Considering this points, in our study, PTCS is thought to be a relatively safe procedure.
In some patients included in our study, the stricture area was widened by performing dilation procedure using a balloon. In some cases among them, a metal stent was used, which may be interpreted as the therapeutic application of PTCS that has been used as a diagnostic purpose in most cases. Generally, in the cases that PTCS was used as therapeutic purposes, it was usefully to the removal of bilialy stones. However, depending on cases, it may be considered to be of help even to conservative treatment for hilar cholangiocarcinoma. Generally, for operable cases, as tretments for cholangiocarcinoma, surgery should be considered,12 nonetheless, many patients are detected at inoperable stages, and thus drainage and other convervative treatments become important treatments.13
In most cholangiocarcinoma patients, drainage procedure is stent insertion using PTBD or ERCP. Stent insertion applying PTCS is thought to have an advantage that stents could be inserted after direct macroscopic examination of the stricture area. Indeed, in our study, it was performed successfully without special complications in 8 patients. However, in most cases, it is known that stenting by the application of PTCS is rare, and even in our study, the number of included patients was small, and thus regarding this, it is thought to require a larger scale investigation.
In conclusion, patients with hilar strictures, prevalence of malignancy was high. PTCS is a useful modality for histopathologic diagnosis and assessment of resectability in patients with hilar strictures, and definite diagnosis can be made in cases with unresectable or inoperable cases. Combination of macroscopic findings such as tumor vessels and histological examination was helpful in diagnosis of malignant hilar strictures. In patients with hilar cholangiocarcinoma, PTCS may be useful as a therapeutic tool, but more investigation is needed.
References
- 1.Seo DW, Lee SK, Yoo KS, et al. Cholangioscopic findings in bile duct tumors. Gastrointest Endosc. 2000;52:630–634. doi: 10.1067/mge.2000.108667. [DOI] [PubMed] [Google Scholar]
- 2.Khan SA, Thomas HC, Davidson BR, Taylor-Robinson SD. Cholangiocarcinoma. Lancet. 2005;366:1303–1314. doi: 10.1016/S0140-6736(05)67530-7. [DOI] [PubMed] [Google Scholar]
- 3.Seo DW, Lee SK, Park JS, et al. Cholangioscopic findings of various bile duct tumors according to histology. Korean J Gastrointest Endosc. 2000;21:780–785. [Google Scholar]
- 4.Yoo BM. Endoscopic Staging of hilar cholangiocarcinoma. Korean J Gastroenterol. 2005;46:16–19. [PubMed] [Google Scholar]
- 5.Lee YJ. Preoperative diagnosis and management for hilar cholangiocarcinoma. Korean J Gastroenterol. 2005;46:28–31. [PubMed] [Google Scholar]
- 6.Nimura Y, Kamiya J, Kondo S, et al. Aggressive preoperative management and extended surgery for hilar cholangiocarcinoma: Nagoya experience. J Hepatobiliary Pancreat Surg. 2000;7:155–162. doi: 10.1007/s005340050170. [DOI] [PubMed] [Google Scholar]
- 7.Lee SS, Kim MH, Lee SK, et al. MR cholangiography versus cholangioscopy for evaluation of longitudinal extension of hilar cholangiocarcinoma. Gastrointest Endosc. 2002;56:25–32. doi: 10.1067/mge.2002.125363. [DOI] [PubMed] [Google Scholar]
- 8.Zhang Y, Uchida M, Abe T, Nishimura H, Hayabuchi N, Nakashima Y. Intrahepatic peripheral cholangiocarcinoma: comparison of dynamic CT and dynamic MRI. J Comput Assist Tomogr. 1999;23:670–677. doi: 10.1097/00004728-199909000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Manfredi R, Barbaro B, Masselli G, Vecchioli A, Marano P. Magnetic resonance imaging of cholangiocarcinoma. Semin Liver Dis. 2004;24:155–164. doi: 10.1055/s-2004-828892. [DOI] [PubMed] [Google Scholar]
- 10.Malhi H, Gores GJ. The modern diagnosis and therapy of cholangiocarcinoma. Aliment Pharmacol Ther. 2006;23:1287–1296. doi: 10.1111/j.1365-2036.2006.02900.x. [DOI] [PubMed] [Google Scholar]
- 11.Kim HJ, Kim MH, Lee SK, Yoo KS, Seo DW, Min YI. Tumor vessel: a valuable cholangioscopic clue of malignant biliary stricture. Gastrointest Endosc. 2000;52:635–638. doi: 10.1067/mge.2000.108969. [DOI] [PubMed] [Google Scholar]
- 12.Tsao JI, Nimura Y, Kamiya J, et al. Management of hilar cholangiocarcinoma: comparison of an American and a Japanese experience. Ann Surg. 2000;232:166–174. doi: 10.1097/00000658-200008000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cheng JL, Bruno MJ, Bergman JJ, Rauws EA, Tytgat GN, Huibregtse K. Endoscopic palliation of patients with biliary obstruction caused by nonresectable hilar cholangiocarcinoma: efficacy of self-expandable metallic wallstent. Gastrointest Endosc. 2002;56:33–39. doi: 10.1067/mge.2002.125364. [DOI] [PubMed] [Google Scholar]