Abstract
Colonoscopy is regarded as a relatively safe procedure and is widely performed. However, complications such as bleeding, perforation, and coagulation syndromes can occur during colonoscopy. Although bowel perforation is as rare as 0.4-1.9% of cases, it is the most serious and awful adverse event which can lead to a death. Colon perforation may occur as either intraperitoneal or extraperitoneal, or in combination. Right subdiaphragmatic free air suggests intraperitoneal perforation while pneumoretroperitoneum, pneumomediastinum, pneumopericardium, and subcutaneous emphysema suggest extraperitoneal perforation. Combined intraperitoneal and extraperitoneal perforation is very rare. Herein, we present a case of combined intraperitoneal and extraperitoneal colon perforation which manifested as pneumoretroperitoneum, pneumomediastinum, pneumopericardium, and subcutaneous emphysema. The lesion was closed with endoscopic clipping.
Keywords: Intestinal perforation, Retropneumoperitoneum, Pneumomediastinum, Pneumopericardium, Subcutaneous emphysema
INTRODUCTION
Colonoscopic exmaination is gradually increasing not only as a diagnostic tool, but also as a therapeutic tool such as colon polypectomy. Colonoscopy is regarded a relatively safe procedure. However, complications such as bleeding and perforation do occur. The complication rates are increasing as the use of colonoscopy is increasing. Colon perforation may be a lethal complication especially in cases of delayed detections. Perforations are categorized into intraperitoneal and extraperitoneal. Generally, intraperitoneal perforation is common. In contrast, extraperitoneal perforation that manifests with pneumoretroperitoneum, pneumomediastinum, pneumopericardium, and subcutaneous emphysema is very rare.
We present a case of combined intraperitoneal and extraperitoneal colon perforation with concomitant pneumoretroperitoneum, pneumomediastinum, pneumopericardium, and subcutaneous emphysema.
CASE REPORT
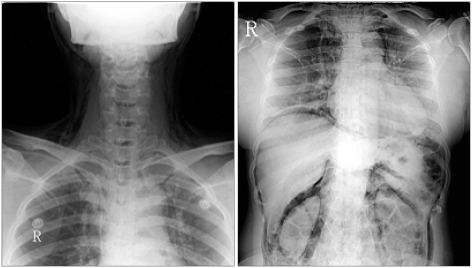
A 46-year-old female was referred via private clinic because of sudden low abdominal pain. On arrival, she complained of abdominal pain, neck swelling, and dyspnea. It seemed that neck swelling, dyspnea, and subcutaneous emphysema developed after colonoscopy in the private clinic. On examination, low abdominal tenderness, rebound tenderness, subcutaneous emphysema, and crepitus were noted in the abdomen, thorax, neck, and face. Initial laboratory tests revealed leukocytosis up to 22,000/mm3 and elevated C-reactive protein level up to 7.37 mg/dL. Right sub-diaphragmatic free air, pneumoretroperitoneum, pneumomediastinum, pneumopericardium, cervical and facial subcutaneous emphysema were observed on the chest and neck X-rays. Perirenal air and psoas shadows were noticed on abdominal X-ray (Fig. 1). On chest CT scan, pneumoperitoneum, pneumomediastirum, pneumopericardium, and subcutaneous emphysema were observed (Fig. 2).
Fig. 1.
Radiographic findings of the neck and chest. Cervical and facial subcutaneous emphysema are noted on the neck X-ray. Right subdiaphragmatic free air, pneumomediastinum, and pneumopericardium are noted on the chest X-ray. Abdomen X-ray shows retroperitoneal air shadow such as perirenal air and psoas shadow.
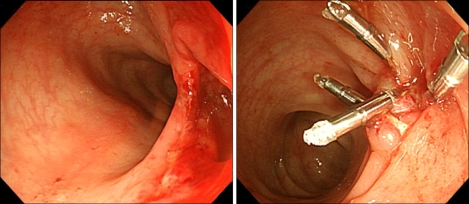
Fig. 2.
Colonoscopic view of the perforation and endoscopic clippings peformed on the lesion. A perforation is noted at lower sigmoid colon. The perforation is completely closed using five clips.
Colon perforation was strongly suspected. A colonoscopy was performed to confirm the site of perforation. A 2 cm perforation was observed at the lower sigmoid colon. In summary, the patient was diagnosed as a sigmoid colon perforation accompanied by pneumoperitoneum, pneumoretroperitoneum, pneumomediastinum, pneumopericardium, and subcutaneous emphysema. Perforation was successfully closed using five endoscopic clips. The patient had nothing through the mouth for 3 days with intravenous antibiotics. Soft diet was tried after 3 days, and there was no sign of peritonitis such as fever or abdominal pain. The patient was discharged after 10 days.
DISCUSSION
The complications of colonoscopy include bleeding, perforation, and post-polypectomy coagulation syndrome. Among these complications, perforation is most common ranging from 0.4% to 1.9%. Previous study reported that perforation was more common with therapeutic colonoscopy when compared to that of the diagnostic colonoscopy (0.44% vs. 0.16%).1 The most common perforation site reported as sigmoid colon (65%).2
The cause of perforation is described by three different mechanisms; (i) pneumatic perforation, (ii) mechanical perforation, and (iii) perforation associated with therapeutic colonoscopy.3 Pneumatic perforation results from rupture of the colon wall due to over distension by insufflated air. Mechanical perforation is caused by the tip or shaft of the endoscope which excessively pressured the intestinal lumen.
Pneumatic perforation and mechanical perforation occur frequently at a site of weakness in the colon wall (e.g., diverticulitis, inflammatory bowel disease, ischemic colitis, or recent surgical anastomosis site). Perforations may also result after colon polypectomy. In addition, electrocauterical injury cause by snares or hot biopsy forceps may occur. The risk of perforation is greatest with large polyps in the proximal colon.
Recent studies reported on underlying mechanisms of colon perforation. Brayko et al4 investigated eleven sigmoid colons insufflated with air via a colonoscope in human cadavers. Serosal tears occurred at a mean pressure of 202±15 mmHg, and mucosal rupture occurred at a mean pressure of 226±14 mmHg. They concluded that most colonic perforations in the sigmoid area occur because of trauma occurred by instrument rather than air insufflation. In our case, sigmoid perforation was thought to be caused by direct mechanical trauma. Although surgical intervention has been the primary treatment for colon perforation, endoscopic clipping has been recently performed as a first line treatment.
When colonoscopy is carried out with a relatively clean bowel after sufficient preparation, leakage of fecal material is not a significant problem which would lead to severe peritonitis or sepsis. Endoscopic clipping and subsequent conservative managements including bowel rest and intravenous antibiotics with hyperalimentation may be preferred to open surgery in cases of iatrogenic perforation.
Colonic perforation may be intraperitoneal, extraperitoneal, or both. Right sub-diaphragmatic free air develops in intraperitoneal perforation while pneumoretroperitoneum, pneumomediastinum, pneumopericardium, and subcutaneous emphysema suggest extraperitoneal perforation. Maunder et al5 described the route of extraperitoneal gas. The soft tissue compartment of the neck, thorax, and abdomen contains four regions the subcutaneous tissue, prevertebral tissue, visceral space, and previsceral space. All of these spaces are connected along the neck, chest, and abdomen. Therefore, air leakage in one space can easily spread to the others.
In this case, the site of perforation was sigmoid colon. Right sub-diaphragmatic free air, pneumoretroperitoneum, pneumomediastinum, pneumopericardium, and subcutaneous emphysema were observed. Therefore, we concluded that the type of perforation was a combined type of intraperitoneal and extraperitoneal perforation. This combined pattern of perforation is extremely rare. Peritonitis was not considered that significant because abdominal fluid collection was scarce on abdominal CT scan. Moreover, vital sign and condition of the patient was stable. That is why we decided to treat her with endoscopic clipping followed by conservative management. The overall outcome was successful.
In summary, we have described a case of combined intraperitoneal and extraperitoneal perforation. Early diagnosis, endoscopic clipping, and conservative management resulted in a satisfactory outcome.
References
- 1.Bakker J, van Kersen F, Bellaar Spruyt J. Pneumopericardium and pneumomediastinum after polypectomy. Endoscopy. 1991;23:46–47. doi: 10.1055/s-2007-1010607. [DOI] [PubMed] [Google Scholar]
- 2.Anderson ML, Pasha TM, Leighton JA. Endoscopic perforation of the colon: lesson from 10-year study. Am J Gastroenterol. 2000;95:3418–3422. doi: 10.1111/j.1572-0241.2000.03356.x. [DOI] [PubMed] [Google Scholar]
- 3.Epstein O. Guidelines on complications of gastrointestinal endoscopy: Complications of colonoscopy. 2006. Nov, www.bsg.org.uk.
- 4.Brayko CM, Kozarek RA, Sanowski RA, Howells T. Diverticular rupture during colonoscopy: fact and fancy? Dig Dis Sci. 1984;29:427–431. doi: 10.1007/BF01296218. [DOI] [PubMed] [Google Scholar]
- 5.Maunder RJ, Pierson DJ, Hudson LD. Subcutaneous and mediastinal emphysema. Pathophysiology, diagnosis and management. Arch Intern Med. 1984;144:1447–1453. [PubMed] [Google Scholar]