Abstract
This study used longitudinal data collected from two trauma-exposed samples, i.e., survivors of community violence (N = 294) and wildfire evacuees (N = 234) to examine a key claim underlying a proposed reformulation of the symptom structure of posttraumatic stress disorder (PTSD). This theory, which we term the PTSD-Dysphoria model, posits that 8 of 17 symptoms of PTSD reflect dysphoria or general psychological distress and might be deemphasized to improve the utility of the PTSD construct (Simms, Watson, & Doebbling, 2002). For each sample, we analyzed PTSD symptoms and measures of general distress administered at two time points. A consistent pattern of findings was observed across assessments for each sample: all 17 PTSD symptoms were highly associated with measures of general distress. Moreover, we found no evidence that dysphoria symptoms were more highly correlated than PTSD-specific symptoms with general distress. Results call into question both the conceptual basis and the clinical utility of differentiating between symptoms that appear to be relatively specific to PTSD and those that seem more broadly characteristic of general psychological distress.
Keywords: posttraumatic stress disorder symptoms, anxiety, depression
Uncertainty exists regarding the most meaningful scheme for classifying symptoms of posttraumatic stress disorder (PTSD), despite having been formally codified nearly three decades ago as a syndrome in the Diagnostic and Statistical Manual of Mental Disorders (DSM; American Psychiatric Association, 1980). PTSD is currently viewed as an anxiety disorder exemplified by three clusters of symptoms that may follow from exposure to a traumatic life event (DSM-IV; American Psychiatric Association, 1994). These three clusters, composed of seventeen symptoms, consist of reexperiencing, (DSM-IV Criterion B; e.g., intrusive thoughts of the trauma), avoidance and emotional numbing, (Criterion C; e.g., avoiding reminders of the trauma), and hyperarousal (Criterion D, e.g., hypervigilance).
One approach to evaluating clusters of symptoms has been to employ factor analysis, on the grounds that each cluster of symptoms should have a unique underlying cause. Using this strategy, the current three-factor DSM-IV classification of PTSD symptoms has received only limited empirical support. The most widely supported organizational frameworks for categorizing PTSD symptoms consist of four symptom clusters. Two separate four-factor classification schemes have received extensive attention. In the first, clusters generally follow the DSM-IV classification with one exception. Specifically, symptoms of avoidance and numbing are differentiated to create two separate symptom clusters, resulting in a model comprised of reexperiencing, numbing, hyperarousal, and avoidance dimensions (DuHamel et al., 2004; King, Leskin, King, & Weathers, 1998; Marshall, 2004; McWilliams, Cox, & Asmundson, 2005; Naifeh, Elhai, Kashdan, & Grubaugh, 2008; Palmieri & Fitzgerald, 2005; Palmieri, Marshall, & Schell, 2007a).
Simms, Watson, and Doebbling (2002) have proposed an alternative four-factor representation of the structure of PTSD symptoms that can be seen as an extension of a theoretical approach originally designed to explain the comorbidity of anxiety and depression (Brown, Chorpita, & Barlow, 1998; L. Clark & Watson, 1991; Mineka, Watson, & Clark, 1998). Simms et al. (2002) analyzed data from approximately 2,000 veterans who had been deployed to the first Gulf War and a similarly large sample of non-deployed soldiers using confirmatory factor analysis. From among six models evaluated, Simms et al. (2002) found that the alternative four-factor model provided the best fit to the data in three different subsamples of veterans.
Within the Simms et al. (2002) model, 8 of the 17 DSM-IV PTSD symptoms (i.e., C3-D3) are reconceptualized as indicators of dysphoria or general psychological distress rather than PTSD-specific symptomatology. These dysphoria symptoms include ‘loss of interest’, ‘emotional detachment’, ‘difficulty concentrating’, ‘irritability’, ‘sleep disturbance’ and additional symptoms common to other disorders. The remaining nine PTSD symptoms (i.e., DSM-IV criteria B1-C2, D4-D5) are subsumed under three PTSD dimensions: an intact reexperiencing cluster with five symptoms, along with avoidance and hyperarousal clusters, each with two symptoms. We will refer to this model as the PTSD-Dysphoria model. Item-dimension alignments for the three previously discussed models of PTSD symptom structure are shown in Table 1.
Table 1.
Item Mappings for Three Alternative Models of the Structure of PTSD Symptoms
| Model |
|||
|---|---|---|---|
| DSM-IV PTSD symptom number and abbreviated content |
1 | 2 | 3 |
| B1. Intrusive thoughts of trauma | R | R | R |
| B2. Recurrent dreams of trauma | R | R | R |
| B3. Flashbacks | R | R | R |
| B4. Emotional reactivity to trauma cues | R | R | R |
| B5. Physiological reactivity to trauma cues |
R | R | R |
| C1. Avoiding thoughts of trauma | A, N | A | A |
| C2. Avoiding reminders of trauma | A, N | A | A |
| C3. Inability to recall aspects of trauma | A, N | N | D |
| C4. Loss of interest | A, N | N | D |
| C5. Detachment | A, N | N | D |
| C6. Restricted affect | A, N | N | D |
| C7. Sense of foreshortened future | A, N | N | D |
| D1. Sleep disturbance | H | H | D |
| D2. Irritability | H | H | D |
| D3. Difficulty concentrating | H | H | D |
| D4. Hypervigilance | H | H | H |
| D5. Exaggerated startle response | H | H | H |
Note. PTSD = Posttraumatic stress disorder. Model 1 = DSM-IV; Model 2 = King et al. (1998); Model 3 = Simms et al. (2002). Symptom clusters to which items contribute: R = Reexperiencing; A = Avoidance; N = Numbing; H = Hyperarousal; D = Dysphoria.
Several research teams have concluded on the basis of confirmatory factor analysis that the PTSD-Dysphoria conceptualization of PTSD symptom structure provides the best fit to their data (e.g., Baschnagel, O’Conner, Colder, & Hawk, 2005; Elkit & Shevlin, 2007; Krause, Kaltman, Goodman, & Dutton, 2007; Palmieri et al., 2007b). For example, in their study of PTSD symptoms in survivors of intimate partner violence, Krause et al. (2007) found that the PTSD-Dysphoria model fit the data better than any other model tested in two separate samples of approximately 400 survivors of intimate partner violence.
Analysis of the internal relations among PTSD symptoms offers very limited information, however, regarding the possible value of any given conceptualization of the structure of PTSD. Because many factor models can adequately explain the association among symptoms, selection of the best structure must be informed by considering the utility of the resulting constructs rather than by model fit alone. For example, a given factor model may be preferred, if it provides a more parsimonious explanation of the relationship between PTSD symptoms and other constructs of interest.
Emerging evidence does provide some support for the construct validity of the PTSD-Dysphoria model. The model predicts that the PTSD dysphoria symptoms should be more strongly associated than other PTSD symptoms with measures of general psychological distress. Simms et al. (2002), Elklit and Shevlin (2007), and Palmieri et al. (2007b) have, in fact, demonstrated that a scale composed of PTSD-Dysphoria symptoms was more associated than scales comprised of the remaining PTSD symptom clusters (i.e., hyperarousal, avoidance, and numbing) with self-report measures of anxiety and depression. For example, in a sample of over 3000 disaster workers exposed to the site of the World Trade Center, Palmieri et al. (2007b) found that a scale comprised of PTSD-Dysphoria symptoms was correlated .80 with a measure of depression. By contrast, correlations between depression and measures of the three remaining PTSD symptom types ranged from .55 to .62. The magnitudes of the correlations found in these studies are summarized in Watson (2009).
The PTSD-Dysphoria model has far-reaching implications for research and clinical practice. For example, the possibility that less diagnostic weight potentially be given to nearly one-half of all PTSD symptoms to reduce the apparent comorbidity of PTSD with other diagnoses such as major depression (Simms et al., 2002) would constitute a major departure from the DSM-IV. Interestingly, others have arrived independently at similar conclusions, noting the presence in the DSM-IV PTSD criteria of symptoms characteristic of other psychiatric disorders, and recommending on conceptual grounds that symptoms not unique to PTSD be removed from the DSM-V criteria (Spitzer, First, & Wakefield, 2007).
Despite the promise of the PTSD-Dysphoria model, further research regarding its validity is required. First, symptom-level analyses are required to determine the extent to which each PTSD symptom is associated with general distress. An exclusive focus on scale-level relations provides an incomplete picture of the degree to which dysphoria symptoms are confounded with general distress. Similarly, it is possible that PTSD symptoms other than those believed to assess dysphoria may also be substantially associated with general distress. The latter relationships may be obscured by analyses that examine only scale-level associations because items within a scale may have different relations than the scale itself to external constructs. Thus, knowing which PTSD subscales are most associated with general distress provides relatively little insight into associations that exist at the level of the individual PTSD symptom.
In addition, the existing literature has operationalized general distress in a manner that may provide an inexact understanding of the relationship between PTSD dysphoria symptoms and general distress. Specifically, previous research has examined the associations of PTSD clusters with scales measuring constructs such as depression, anxiety, and anger (Elklit & Shevlin, 2007; Palmieri et al., 2007b; Simms et al., 2002). Yet, the constituent items on the latter scales are known to measure both general and domain-specific content to varying degrees (L. Clark & Watson, 1991; D. Clark, Steer, & Beck, 1994; Simms, Grös, Watson, & O’Hara, 2008). A more direct test of the construct validity of the PTSD-Dysphoria model would include as indicators of general distress only those symptoms that are relatively unequivocal markers of the construct.
To examine the relations between individual PTSD symptoms and general distress, we analyzed data collected from two separate trauma-exposed samples, each of which was assessed on multiple occasions following trauma exposure. One sample consisted of individuals who had been mandatorily evacuated from their homes to escape one of the most costly and destructive wildfires in California history (Marshall, Schell, Elliott, Rayburn, & Jaycox, 2007). A second sample was composed of young adults who had required hospitalization for physical injuries stemming from community violence (Denson, Marshall, Schell, & Jaycox, 2007; Ramchand, Marshall, Schell, & Jaycox, 2008).
Methods
Participants and Procedures
Data were drawn from participants in two separate research investigations. For the Fire study, individuals who had been subjected to mandatory evacuation from their homes in response to a large wildland-urban interface fire in late October of 2003 were recruited from two adjacent facilities that provided emergency disaster services. All adults in two recruitment sites between the hours of 10 am and 6 pm, over the course of several days, were invited to participate by a member of the research team. A single, randomly selected, adult from each household was invited to complete the survey. For additional information on sampling and sample characteristics, see Marshall et al. (2007).
Of the 402 households approached to participate, 357 persons completed a self-administered questionnaire, yielding a baseline response rate of 89%. At the initial assessment, 54% of participants were male; 64% were non-Hispanic Caucasian, 14.0% were African-American, 15% were Hispanic, and 7% indicated belonging to another group. Participants averaged 40.1 years of age (SD = 13.6). For the current purposes, we used data collected via self-administered questionnaires at the 3- and 15-month follow-up assessments. Sixty-six percent of baseline participants (N = 234) returned a completed 3-month follow-up mail survey; 54% (N = 191) completed and returned the 15-month follow-up survey.
For the Community Violence study, participants were individuals requiring hospitalization for life threatening physical injuries stemming from community violence (e.g., shootings, stabbings). Between October 1998 and June 2000, the research staff attempted to screen all consecutive hospital admissions for blunt or penetrating trauma at a large, urban trauma center. Given the goals of the original study, persons whose injuries were not due to community violence (e.g., motor vehicle collisions) were excluded. Participants were required to be between 18 and 35 years of age, and to be fluent in either English or Spanish. Of the 653 persons screened, 423 were deemed eligible. Of these, a total of 413 (98%) chose to participate. At the initial assessment, 94% of participants were male and 78% were Hispanic. Participants averaged 25.1 years of age (SD = 6.03). Fifty-nine percent of participants sustained injuries stemming from gunshots; the remaining 41% had received injuries from other penetrating or blunt objects.
All Community Violence study participants completed face-to-face structured interviews conducted by trained lay interviewers. The initial interview took place in hospital within days of the injury; the median interval between admission and the baseline interview was 5 days. Subsequent face-to-face in-home interviews were conducted at 3- and 12-months following the initial interview. Of the 413 participants who were interviewed at baseline, 294 participants (71.2%) completed the 3-month follow-up interview and 304 (73.6%) participants completed the 12-month follow-up interview. Seventy-one percent completed the initial interview in English and 29% (N = 120) completed the interview in Spanish. Information about instrument translation can be found in Marshall and Orlando (2002).1 Finally, additional information on sampling and sample characteristics can be found in Denson et al. (2007) or Ramchand et al. (2008).
Participants in both studies were given $25 for each completed assessment. The research protocols for both studies were approved and monitored by the RAND Human Subjects Protection Committee; the Community Violence protocol was also approved and monitored by the Institutional Review Board of the University of Southern California School of Medicine. For the purposes of the current study, we analyzed data from the 3- and 15-month Fire study assessments as well as data from the 3- and 12-month Community Violence study assessments.2
Measures
PTSD symptom severity
For both studies, PTSD symptom severity was assessed using the civilian version of the 17-item PTSD Checklist (PCL; Weathers, Litz, Herman, Huska, & Keane, 1993). PCL items map directly onto DSM-IV symptom criteria. The checklist has been used in diverse samples and has been found to possess solid psychometric properties (Andrykowski, Cordova, Studts, & Miller, 1998; Palmieri et al., 2007b). The PCL requires participants to rate the degree to which they were bothered by each symptom on a scale ranging from 1 (not at all) to 5 (extremely). For the Community Violence and Fire studies, the PCL was modified such that symptoms were assessed with respect to either the attack or the fire (e.g., how much have you been bothered by repeated, disturbing dreams of the fire”). For the Fire study, responses to the questions were provided with respect to the past two weeks; for the Community Violence study, answers were provided with regard to the past 7 days.
General distress
For the Fire study, items measuring general distress were drawn from the eight-item Patient Health Questionnaire (PHQ-8; Kroenke, Spitzer, & Williams, 2001). This instrument, a variant of the PHQ-9, assesses symptoms required to meet a DSM-IV diagnosis of major depression with the exclusion of a single item assessing suicidal ideation. Responses to the PHQ-8 are provided with respect to the frequency with which symptoms were experienced in the past two weeks, using a 4-point scale ranging from 1 (not at all) to 4 (every day). The PHQ-8 is a well-validated and widely used brief screening measure for major depression (Kroenke et al., 2008 Löwe et al., 2008).
For the Community Violence study, items assessing general distress were drawn from abbreviated 6-item versions of the depression and anxiety subscales of the Symptom Checklist-Revised (SCL-90-R; Derogatis, 1992). Participants rated the extent to which they were bothered by each symptom in the past seven days, using a scale ranging from 1 (not at all) to 5 (extremely). The SCL-90-R is among the most widely used self-report symptom inventories; the psychometric properties of the anxiety and depression subscales have been established in various settings (Derogatis, 1992; Derogatis & Savitz, 1999).
Item selection for analyses
For the item-level analyses, we selected specific PHQ-8 and SCL-90-R items that were relatively pure markers of general distress. These items were chosen by reference to the results of two separate factor analytic examinations of the structure of symptoms of depression and anxiety. The explicit objective of each of these investigations was to differentiate symptoms characteristic of general distress from those reflective of domain-specific distress (e.g., depression) (Watson et al., 1995; Simms, Grös, Watson, & O’Hara, 2008). Although using different approaches to analyze inventories containing symptoms of anxiety and depression, both Watson et al. (1995) and Simms et al. (2008) identified separate factors corresponding to the dimensions of general distress and domain-specific distress.
As a first step in determining whether to include a symptom as a marker of general distress, we first sought to establish whether a given symptom in one of our data sets had an essentially equivalent item in Simms et al. (2008) and Watson et al. (1995). In most instances, we found an appropriate match. For a few symptoms (e.g., “suddenly scared for no reason”), we found no match in either Simms et al. (2008) or Watson et al. (1995). In such situations, the item was excluded from further consideration. When we found a comparable item in Simms et al. (2008) and Watson et al. (1995), we then examined the factor loadings for the item reported in the two studies. To be regarded as an indicator of general distress for the purposes of the current study, we required that the general distress factor account for at least 75% of the explained variance for a given item when averaged across the Simms et al. (2008) and Watson et al. (1995) factor solutions.
For the Community Violence data set, six items were relatively pure markers of general distress using this metric: ‘worry too much’ (.89), ‘feeling sad or blue’ (.87), ‘feeling restless’ (.85), ‘feeling fearful’ (.83), ‘feeling tense’ (.79), and ‘feeling hopeless’ (.75). For the Fire study, four items emerged as relatively pure markers of general distress: ‘trouble concentrating’ (.85), ‘moving or speaking so slowly…or being restless or fidgety’ (.85), ‘feeling down, depressed, or hopeless’ (.84), and ‘feeling bad about yourself’ (.78).
Data Analysis
Core analyses
Using the four data sets, we employed structural equation modeling to examine the relationship between individual PTSD symptoms and general distress. In an initial step, we constructed latent factors representing general distress in each data set. For the Community Violence study, general distress was modeled as a single latent factor with the six indicators mentioned above; for the Fire study, general distress was operationalized using the four indicators listed above.
After establishing the adequacy of the latter measurement models, we then examined a model in which general distress and the 17 PCL indicators of PTSD were simultaneously assessed. Instead of imposing an assumed causal structure on PTSD symptoms (e.g., King et al., 1998; Simms et al., 2002), we examined the association between general distress and each individual PCL item. To assess hypotheses about strengths of association rather than the size of covariances, all symptoms were standardized to have a SD = 1 prior to analysis. The variances of the latent general distress factor were also set to 1 to identify the models. Various null hypotheses about these correlations were examined. First, we tested whether the magnitude of the correlations between General Distress and the eight PTSD-Dysphoria symptoms was equal to the magnitude of the correlations between General Distress and the nine remaining non-dysphoria PTSD symptoms (i.e., a 1 df test in which the correlations of General Distress with all symptoms were equal against a relaxed model in which Dysphoria and non-Dysphoria symptoms can have different correlations with General Distress).
In a subsequent step, we conducted a series of analyses comparing the extent to which four groups of symptoms (i.e., Reexperiencing, Avoidance, Dysphoria and Hyperarousal) were associated with General Distress. First, we tested whether all four sets of correlations were equal by examining the increase in chi-square when all correlations were constrained to equality (i.e., a three degree of freedom chi-square test). Irrespective of the outcome of this test, we then conducted three separate follow-up tests to compare the magnitude of each of the individual correlations involving one of the three non-dysphoria symptom clusters and General Distress with the analogous correlations involving PTSD-Dysphoria and General Distress. The latter tests assessed, for example, whether the correlations between General Distress and Reexperiencing symptoms were equal to the correlations between General Distress and PTSD-Dysphoria. We did not adjust these significance tests for multiple testing.
Assessing model fit
Structural equation modeling was conducted, using the Mplus 5.1 software program (Muthén & Muthén, 2006). Robust maximum likelihood parameter estimation (implemented in Mplus as MLR estimation, and asymptotically equivalent to the Yuan-Bentler T2* chi-square; Yuan & Bentler, 2000) was employed. As with many applications of the PCL, item scores were positively skewed.3 Because Satorra-Bentler estimation is not possible with missing data in Mplus 5.1, we used MLR which follows a similar approach to correcting chi-square and standard errors for non-normality. Missing data were dealt with using the full information maximum likelihood to ensure that estimates are unbiased in the presence of data which are either missing at random or completely at random.
For assessing overall model fit, we used the Tucker-Lewis Index (TLI; Tucker & Lewis, 1973), the CFI (Bentler, 1990), the RMSEA (Steiger & Lind, 1980), and the SRMR (Bentler, 1995) fit indices. To determine model acceptability, Hu and Bentler (1999) have suggested use of 0.95 for the CFI or TLI as well as .06 and 0.08 for the RMSEA and SRMR, respectively. However, these recommendations have stimulated cautionary warnings about the extent to which any criteria hold across all possible applications (Marsh, Hau, & Wen, 2004). Nonetheless, most models tested herein fit within these guidelines. The appropriate scaling factor for chi-squared difference tests of nested models was also employed for comparing models (Satorra & Bentler, 1999). To assess the significance of differences between nested models, we used chi-square tests with a p value of 0.05.
Results
Descriptive Analyses
For descriptive purposes and to facilitate comparison to other samples, we created aggregate PCL scores by summing across the 17 items for each assessment in both studies. Fire study participants averaged scores of 32.67 (SD = 16.97), and 30.22 (SD = 15.21) on the PCL at the 3-month and 15-month assessments, respectively. For the Community Violence study, the comparable PCL scores were 34.89 (SD = 14.3) and 33.9 (SD = 14.4) for the 3-month and 12-month assessments. These mean scores suggest that a substantial portion of both samples experienced clinically significant psychological distress at each assessment. To document the foregoing observation, PCL screener responses were categorized to identify persons meeting symptom criteria for PTSD using the procedure recommended by Weathers et al. (1993) and implemented by Palmieri et al. (2007b). Specifically, individual symptoms receiving a score of 3 (moderately) or greater were treated as indicating symptom presence and mapped against the DSM–IV criteria B–D. Following this scoring strategy, 21.9% of Fire study participants met screening criteria for PTSD at 3-months whereas 15.8% met criteria at the 15-month assessment. For the Community Violence sample, 21.4% and 20.1% met screening criteria for PTSD at the 3- and 12-month follow-up assessments, respectively.
Core Analyses
In an initial series of analyses, we examined the adequacy of our measurement models for the General Distress construct in the four separate assessments. As discussed previously, for the Community Violence study, we used 6 indicators of a single general distress factor at each of the assessments. For the Fire study, we used 4 indicators at each of the two follow-up assessments. All items were allowed to load freely on their respective factors and factor variances were fixed to unity to identify the models. As shown in Table 2, these measurement models were found to be reasonable approximations of the data at all four assessments.4 In the next series of tests, we simultaneously modeled the General Distress factor and individual PTSD symptoms with no symptom structure imposed on the latter. Correlations between individual PTSD symptoms and the general distress factor were freely estimated. As shown in Table 3, this basic model fit the data satisfactorily in both samples at each assessment.
Table 2.
Fit Indices for General Distress Measurement Models
| Model | N | χ2 (df) | p-value | CFI | TLI | RMSEA | SRMR |
|---|---|---|---|---|---|---|---|
| Community Violence | |||||||
| 3-Month | 294 | 6.3 (9) | 0.71 | 1.00 | 1.01 | 0.00 | 0.017 |
| 12-Month | 304 | 3.1 (9) | 0.96 | 1.00 | 1.02 | 0.00 | 0.012 |
| Fire | |||||||
| 3-Month | 234 | 7.1 (2) | 0.029 | 0.98 | 0.94 | 0.10 | 0.022 |
| 15-Month | 191 | 14.6 (2) | <0.001 | 0.94 | 0.81 | 0.18 | 0.038 |
Note. CFI = Comparative Fit Index (Bentler, 1990), TLI = Tucker-Lewis Index (Tucker & Lewis, 1973), RMSEA = Root Mean Squared Error of Approximation (Steiger & Lind, 1980), SRMR = Standardized Root-Mean-Squared Residual (Bentler, 1995).
Table 3.
Fit Indices of Models Linking General Distress and Individual PTSD Symptoms
| Model | N | χ2 (df) | p-value | CFI | TLI | RMSEA | SRMR |
|---|---|---|---|---|---|---|---|
| Community Violence | |||||||
| 3-Month | 294 | 146.8 (94) | <0.001 | 0.98 | 0.94 | 0.044 | 0.029 |
| 12-Month | 304 | 142.2 (94) | <0.001 | 0.98 | 0.95 | 0.041 | 0.029 |
| Fire | |||||||
| 3-Month | 235 | 84.6 (53) | 0.004 | 0.99 | 0.95 | 0.050 | 0.018 |
| 15-Month | 191 | 100.4 (53) | <0.001 | 0.98 | 0.92 | 0.068 | 0.021 |
Note. CFI = Comparative Fit Index (Bentler, 1990), TLI = Tucker-Lewis Index (Tucker & Lewis, 1973), RMSEA = Root Mean Squared Error of Approximation (Steiger & Lind, 1980), SRMR = Standardized Root-Mean-Squared Residual (Bentler, 1995). No factor structure was imposed on PTSD symptoms.
The correlations between General Distress and the 17 PCL items from these models are displayed in Table 4. As shown, all correlations were large, using Cohen’s (1992) criterion, and statistically significant. As displayed in Table 5, when we compared the magnitudes of the correlations for the Dysphoria and non-Dysphoria symptoms, we found no significant evidence that the 8 dysphoria symptoms were more strongly correlated than the 9 non-dysphoria symptoms with general distress. After separating the non-Dysphoria symptoms into those assessing the three conceptually distinct dimensions of Reexperiencing, Avoidance, and Hyperarousal, we found that Reexperiencing and Avoidance symptoms each had significantly different correlations with General Distress at one of the two assessments. We found no evidence, however, that correlations between General Distress and PTSD-Dysphoria symptoms were systematically greater than those between General Distress and symptoms from the three remaining PTSD symptom clusters.
Table 4.
Correlations Involving Latent General Distress and Individual PTSD Symptoms
| Community Violence | Fire | Symptom Mean | |||
|---|---|---|---|---|---|
| 3-Month |
12-Month |
3-Month |
15-Month |
||
| PTSD Cluster and Symptom Number | |||||
| Reexperiencing | |||||
| B1 | 0.59 | 0.61 | 0.67 | 0.57 | 0.61 |
| B2 | 0.62 | 0.59 | 0.62 | 0.55 | 0.60 |
| B3 | 0.60 | 0.58 | 0.52 | 0.55 | 0.56 |
| B4 | 0.53 | 0.69 | 0.62 | 0.61 | 0.61 |
| B5 | 0.59 | 0.69 | 0.76 | 0.65 | 0.67 |
| Avoidance | |||||
| C1 | 0.47 | 0.46 | 0.63 | 0.61 | 0.54 |
| C2 | 0.49 | 0.54 | 0.73 | 0.59 | 0.59 |
| Dysphoria | |||||
| C3 | 0.46 | 0.32 | 0.54 | 0.66 | 0.49 |
| C4 | 0.52 | 0.60 | 0.72 | 0.67 | 0.63 |
| C5 | 0.58 | 0.62 | 0.82 | 0.72 | 0.69 |
| C6 | 0.65 | 0.65 | 0.74 | 0.79 | 0.71 |
| C7 | 0.63 | 0.58 | 0.78 | 0.82 | 0.70 |
| D1 | 0.61 | 0.71 | 0.72 | 0.71 | 0.69 |
| D2 | 0.61 | 0.78 | 0.77 | 0.77 | 0.60 |
| D3 | 0.62 | 0.75 | 0.87 | 0.80 | 0.71 |
| Hyperarousal | |||||
| D4 | 0.52 | 0.56 | 0.64 | 0.69 | 0.55 |
| D5 | 0.71 | 0.64 | 0.80 | 0.71 | 0.68 |
| Mean (Reexperiencing) | 0.59 | 0.63 | 0.64 | 0.59 | |
| Mean (Avoidance) | 0.48 | 0.50 | 0.68 | 0.60 | |
| Mean (Dysphoria) | 0.59 | 0.63 | 0.75 | 0.74 | |
| Mean (Hyperarousal) | 0.62 | 0.60 | 0.72 | 0.70 | |
| Mean (Non-Dysphoria) | 0.57 | 0.60 | 0.66 | 0.61 | |
Note. All correlations are significant at p < .001; PTSD = Posttraumatic Stress Disorder; R = Reexperiencing; A = Avoidance; D = Dysphoria; H = Hyperarousal. B1 – D5 correspond to DSM-IV symptom criteria.
Table 5.
Models of the Correlations between Symptoms Found in Specific PTSD Clusters and General Distress
| Models | Community Violence | Fire | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 3 Month | 12 Month | 3 Month | 15 Month | |||||||||
| χ2 | df | p | χ2 | df | p | χ2 | df | p | χ2 | df | p | |
| D = Non-D | 0.38 | 1 | .54 | 1.81 | 1 | .18 | 0.71 | 1 | .40 | 2.16 | 1 | .14 |
| R = A = D = H | 3.52 | 3 | .32 | 7.36 | 3 | .06 | 3.36 | 3 | .34 | 5.05 | 3 | .17 |
| R = D | 0.19 | 1 | .66 | 0.07 | 1 | .79 | 1.51 | 1 | .22 | 4.70 | 1 | .03 |
| A = D | 2.87 | 1 | .09 | 4.39 | 1 | .04 | 0.60 | 1 | .44 | 1.50 | 1 | .22 |
| H = D | 0.70 | 1 | .40 | 3.72 | 1 | .05 | 0.79 | 1 | .37 | 0.70 | 1 | .40 |
Note. D = Dysphoria symptoms; Non-D = Non-Dysphoria symptoms; R = Reexperiencing symptoms; A = Avoidance items; H = Hyperarousal symptoms.
Supplemental Analyses
Our results appear to differ substantially from those of previous researchers who have concluded that symptoms from the Dysphoria cluster are more associated than other PTSD symptoms with General Distress (Elkit & Shevlin, 2007; Palmieri et al., 2007b; Simms et al., 2002). Our analytic strategy also differed in key respects, however. To determine whether the observed discrepancies were attributable to critical methodological differences or merely to sample-specific factors, we attempted to replicate the scale-level results reported previously, using directly comparable methods. In particular, we created aggregate depression and anxiety scales using the full PHQ-8 as well as items drawn from the SCL-90-R anxiety (6 items) and depression scales (6 items). We then examined the correlations between observed scales composed of Depression and Anxiety symptoms and the four PTSD subscales. Finally, to help clarify the extent to which discrepant findings appear attributable to the use of domain-specific (e.g., depression) or general distress items, we also examined the correlations between the four PTSD scales and a scale composed of those general distress items that were found to be relatively pure markers of the construct as described above.
As shown in Table 6, all correlation coefficients involving PTSD-related dysphoria and Depression/Anxiety were larger than the corresponding coefficients involving the remaining PTSD scales and Depression/Anxiety. In the Community Violence study, correlations between PTSD-Dysphoria and Depression averaged .79 whereas the correlations between the remaining PTSD scales and Depression averaged .54, yielding a mean difference of .25. In the Community Violence Study, correlations between PTSD-Dysphoria and Anxiety averaged .77 whereas the correlations between the remaining PTSD scales and Anxiety averaged .64, for a mean difference of .13. In the Fire study, correlations of PTSD-Dysphoria with Depression averaged .85 whereas the remaining correlations averaged .69, resulting in a mean difference of .14. When aggregated across studies, convergent-divergent correlation differences averaged .20 and .14, for depression and anxiety measures, respectively. Thus, when we used directly comparable methods, our findings were broadly consistent with those observed by others (e.g., Palmieri et al., 2007).
Table 6.
Correlations between Observed PTSD Scales and Scales Measuring Depression, Anxiety, and General Distress
| Sample and Assessment | External Criteria | ||
|---|---|---|---|
| Depression | Anxiety | GD | |
| Community Violence (3-Month) | |||
| Reexperiencing | .63 | .71 | .69 |
| Avoidance | .46 | .53 | .52 |
| Dysphoria | .77 | .74 | .81 |
| Hyperarousal | .54 | .64 | .63 |
| Non-Dysphoriaa | .66 | .75 | .73 |
| Community Violence (12-Month) | |||
| Reexperiencing | .63 | .77 | .66 |
| Avoidance | .48 | .54 | .51 |
| Dysphoria | .82 | .79 | .74 |
| Hyperarousal | .52 | .66 | .57 |
| Non-Dysphoriaa | .66 | .80 | .70 |
| Fire (3-Month) | |||
| Reexperiencing | .72 | -- | .70 |
| Avoidance | .71 | -- | .70 |
| Dysphoria | .86 | -- | .85 |
| Hyperarousal | .77 | -- | .73 |
| Non-Dysphoriaa | .80 | -- | .77 |
| Fire (15-Month) | |||
| Reexperiencing | .63 | -- | .63 |
| Avoidance | .61 | -- | .60 |
| Dysphoria | .84 | -- | .83 |
| Hyperarousal | .72 | -- | .71 |
| Non-Dysphoriaa | .70 | -- | .69 |
Note. PTSD = Posttraumatic Stress Disorder. GD = General Distress. The GD scale is composed of symptoms that emerged as relatively pure markers of general distress. Depression and anxiety scales are proxy measures of general distress that contain symptoms that measure, to varying degrees, both general and domain-specific distress. For each measure of general distress and within each assessment, the largest correlation with the four PTSD-Dysphoria scales is shown in boldface. Dashed lines indicate that a scale measuring this construct was not administered.
This scale is composed of the sum of the nine PTSD symptoms that were not included in the Simms et al. (2002) PTSD-Dysphoria factor. Thus, it combines items across three symptom clusters (i.e., reexperiencing, avoidance, hyperarousal). With respect to scale length alone, this 9-item scale is more directly comparable to the 8-item Dysphoria scale.
Finally, as shown in Table 6, the discrepancy between our findings and those reported by others seemed primarily attributable to our use of item-level rather than scale-level analyses. That is, the pattern of relations involving PTSD subscales and measures of General Distress was quite similar irrespective of whether we used disorder-specific scales as proxies for general distress or an index composed solely of symptoms that appeared to be relatively pure markers of general distress.
Discussion
This study examined the construct validity of the PTSD-Dysphoria model of PTSD symptom structure (Simms et al., 2002). To our knowledge, this investigation constituted the first evaluation of relations between individual PTSD items and general psychological distress. In addition, this study measured general distress with symptoms specifically identified in prior empirical research as markers of general distress (Simms et al., 2008; Watson et al., 1995), rather than solely by using disorder-specific scales (e.g., depression scales) as proxies for general distress.
Two important findings emerged. First, all 17 PTSD symptoms were substantially correlated with general distress. To varying degrees, each PTSD item appeared to have variance that was PTSD-specific and variance that was associated with general distress. Moreover, at the level of the individual PTSD symptom, no evidence was found that the associations involving general distress and PTSD symptoms were systematically higher for symptoms categorized by Simms et al. (2002) as reflecting dysphoria. Stated differently, PTSD symptoms purported to be markers of dysphoria (Elklit & Shevlin, 2007; Palmieri et al., 2007b; Simms et al., 2002) were no more strongly correlated than other PTSD symptoms with separate measures of general distress.
Moreover, our findings do not appear to be easily discounted as attributable to sample-specific differences between the current study and prior research. In particular, when analyses were performed at the level of the PTSD symptom scale and without excluding items that were comparatively poor markers of general distress, we were able to reproduce the results reported in other investigations (Elklit & Shevlin, 2008; Palmieri et al., 2007b; Simms et al., 2002). The actual differences in the average magnitude of the scale-level convergent-divergent correlations in the current study were .20 and .14 for depression and anxiety scales, respectively. These differences were comparable—albeit smaller in size (i.e., .31 and .19)—to those reported by Simms et al. (2002), and were similar to those found by Palmieri et al. (2007) for depression and anxiety (i.e., .22 and .09).
These results bear on the conceptualization and measurement of PTSD. With respect to the assessment of PTSD, some have suggested that the dysphoria symptoms of PTSD might profitably be deemphasized (Simms et al., 2002) or removed from the diagnostic criteria entirely (Spitzer et al., 2007) so as to improve the utility of the disorder in future revisions of the DSM. Viewed in light of the current findings, this proposition appears premature. Although the content of some PTSD symptoms may appear conceptually to be non-specific to PTSD, such symptoms are not more strongly associated empirically than other PTSD items with external measures of general distress.
Furthermore, elimination of PTSD symptoms or reduction of their diagnostic importance based solely on associations with general distress seems unlikely to prove fruitful in reshaping the diagnostic criteria for PTSD because all PTSD symptoms are highly associated with general distress. In this context, it is notable that Simms et al. (2008) have recently shown that traumatic intrusions (i.e., PTSD reexperiencing symptoms) have a very large general distress component (p. 41). In fact, the influence of the general factor was actually greater than that of the specific factor for the majority of reexperiencing symptoms examined by Simms et al. (2008). Thus, although reexperiencing symptoms are regarded as relatively specific to PTSD when viewed from the perspective of the PTSD-Dysphoria model (Simms et al., 2002), the findings of Simms et al. (2008) seem to raise the possibility that reexperiencing symptoms might also be non-specific to PTSD.
These results are also relevant to hierarchical models of mood and anxiety disorders that have been invoked to distinguish features that are common to these broad classes of disorders from those that are characteristic of specific conditions (Brown et al., 1998; L. Clark & Watson, 1991; Krueger & Markon, 2006; Mineka et al., 1998). This line of inquiry has culminated in the proposal (Watson, 2005) that these overarching classes of disorders can be differentiated into syndromes that have fear as the core element (e.g., panic disorder, agoraphobia, and simple phobias) and those that share emotional distress as the defining feature (e.g., generalized anxiety disorder, major depression, and PTSD).5
At first glance, the current findings are consistent with the Watson model (2005) inasmuch as they reveal that general distress is central to all PTSD symptoms. On reflection, however, these results indicate that it may not be possible to identify specific symptoms that are both unique to PTSD and that have little or no association with general distress. The observation that all PTSD symptoms are associated with general distress, however, does not imply that uniquely important symptoms of PTSD can not be identified. Longitudinal research indicates, in particular, that hyperarousal may be the defining feature of PTSD (Marshall, Schell, Glynn, & Shetty, 2006; Schell, Marshall, & Jaycox, 2004).6
These findings should not be viewed as suggesting that the PTSD-Dysphoria model (Simms et al., 2002) is a poor representation of the symptom structure of PTSD. This configuration may yet prove superior to alternative structures with respect to both model fit and explanatory power. The results do, however, call into question the conceptual distinction underlying the PTSD-Dysphoria model (Simms et al., 2002), as well as the proposed interpretation of the resulting symptom clusters. Given that symptoms regarded as reflecting dysphoria are no more strongly associated than other PTSD symptoms with external measures of general distress, these data suggest that the dysphoria dimension of the PTSD-Dysphoria model might best be relabeled. As one alternative warranting further study, the dysphoria symptoms could be reinterpreted as reflecting impaired functioning or performance. That is, symptoms such as loss of interest and restricted affect as well as disturbed sleep and concentration might be aptly construed as the absence of normal psychological functioning rather than the presence of dysphoria or general distress.
Although the current results do not support the construct validity of the PTSD-Dysphoria reformulation, it is possible for the model to be modified or elaborated in a post hoc manner to be consistent with the current findings. For example, it is conceivable that dysphoria and non-dysphoria symptoms are similarly correlated with general distress but for different reasons. Dysphoria items may be correlated with general distress because they are indicators of general distress. In contrast, the remaining PTSD symptoms may be associated with general distress because those symptoms cause general distress. This interpretation is broadly consistent with the DSM-IV inasmuch as PTSD symptoms are required to precipitate psychological distress (Criteria F, American Psychiatric Association, 1994). As currently articulated (e.g., Simms et al, 2002), however, the PTSD-Dysphoria model, does not predict the high correlations of all 17 individual PTSD symptoms with general distress. Of course, if the theory is modified to hold irrespective of the pattern of relations found between PTSD symptoms and general distress, then other methods of testing the validity of the theory require explication.
In arriving at these conclusions, it is important to bear in mind certain limitations of the current study. First, despite our use of data from two quite distinct trauma-exposed samples at two time points, future research is needed to determine the degree to which these findings would generalize to survivors of other types of trauma. Moreover, insofar as this study assessed symptoms of anxiety and depression—but not the full range of emotional reactions characteristic of general distress and PTSD (e.g., anger)—additional research is warranted. Future investigations to extend these findings to examine the common and specific aspects of symptoms of multiple disorders might also prove valuable (cf. Grant, Beck, Marques, Palyo, & Clapp, 2008).
In summary, the PTSD-Dysphoria model has been proposed as a useful framework for understanding PTSD insofar as a potentially important distinction is drawn between symptoms that are hypothesized to be common to various disorders and those specific to PTSD (Simms et al., 2002). The current study attempted to assess construct validity more directly than in previous investigations by examining the pattern of associations between individual PTSD symptoms and measures of general distress. Across multiple assessments from two samples, we found no evidence that the eight PTSD-Dysphoria symptoms were uniformly more associated than the remaining nine PTSD symptoms with general distress. In light of these findings, it may be premature to embrace this conceptualization of the structure of PTSD in the forthcoming DSM-V.
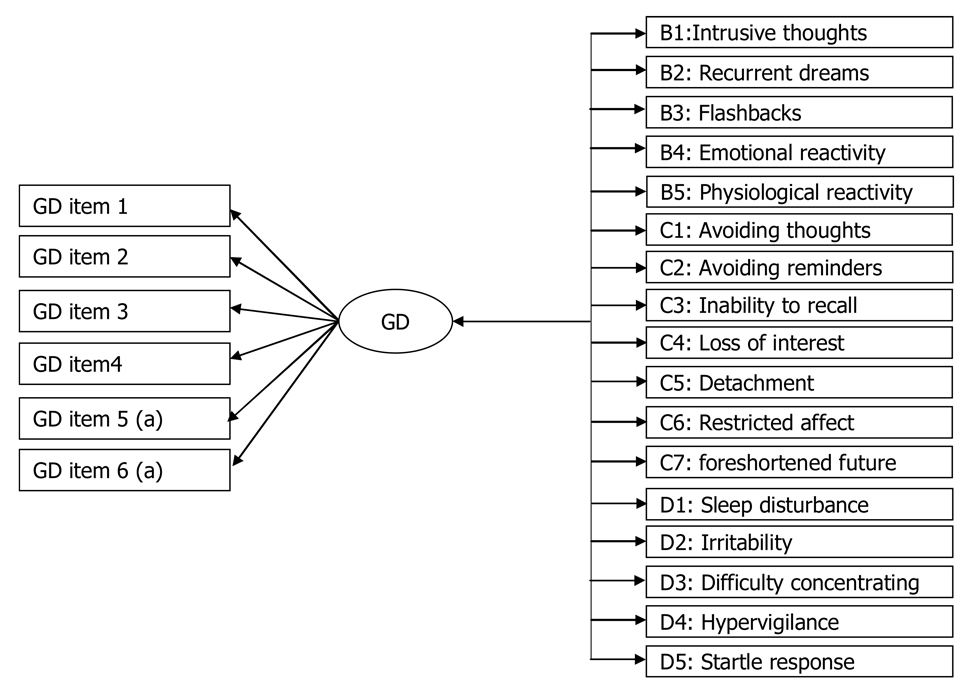
Figure 1.
The Relationship of General Distress to PTSD Items
GD = General Distress; B1-D5 = PTSD symptom numbering in DSM-IV. aGD was measured using 4 and 6 items in the Fire and Community Violence studies, respectively. Bidirectional arrows depict correlations. Unidirectional arrows depict regression paths/loadings.
Acknowledgments
Grant Marshall, Terry Schell, Jeremy Miles (RAND Corporation, Santa Monica, CA). This research was supported by grants R01MH56122 and R01MH071636 from the National Institute of Mental Health and grant R01AA014246 from the National Institute on Alcohol Abuse and Alcoholism. The views expressed are ours and do not necessarily reflect those of the funders or RAND. We thank the RAND Survey Research Group for their assistance with data collection. We gratefully acknowledge the generosity of the trauma survivors who participated in these studies.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/abn.
The Spanish and English versions of the PCL have been established to be psychometrically equivalent (Miles, Marshall, & Schell, 2008). Specifically, no evidence was found of differential item function or an overall scoring bias across the two versions.
Data from the initial assessment of each study were not included. To this point, the PTSD-Dysphoria model has been articulated to apply to PTSD symptoms. Reactions that occur within the hours or days immediately following trauma exposure do not meet criteria for PTSD and may involve different psychological processes.
For the Fire study, all PTSD items were positively skewed, with a mean skew of 1.42, and a range of 0.70 to 2.17. For the Community Violence study, the mean skew was 1.10, ranging from −0.13 to 1.10.
As shown in Table 2, for the 15-month assessment of the Fire study, the TLI and RMSEA were particularly sensitive to misfit involving two items: (i.e., “feeling down, depressed or hopeless” and “feeling bad about yourself”). The addition of a correlated error between these items led to a substantially improved model fit, χ2 = 0.04, p = .85; CFI = 1.00, TLI = 1.03, RMSEA = 0.000, SRMR = 0.001. To retain comparability with the other models, however, we elected not to incorporate this correlated error. For all subsequent models, sensitivity analyses were conducted in which the correlated error term was incorporated. The essential pattern of findings did not vary as a function of whether this parameter was included.
These broad classes have sometimes been referred to as measuring fear and misery (e.g., Cox, Clara, & Enns, 2002; Krueger, 1999).
Interestingly, to the degree that hyperarousal is a core feature of the disorder, PTSD may be more appropriately grouped with fear, rather than distress, disorders (cf. Brown et al., 1998).
References
- Andrykowski MA, Cordova MJ, Studts JL, Miller TW. Posttraumatic stress disorder after treatment for breast cancer: Prevalence of diagnosis and use of the PTSD Checklist – Civilian Version (PCL-C) as a screening instrument. Journal of Consulting and Clinical Psychology. 1998;66:586–590. doi: 10.1037//0022-006x.66.3.586. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Washington, DC: Author; 1980. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- Baschnagel JS, O’Connor RM, Colder CR, Hawk LW., Jr Factor structure of posttraumatic stress among western New York undergraduates following the September 11th terrorist attack on the World Trade Center. Journal of Traumatic Stress. 2005;18:677–684. doi: 10.1002/jts.20076. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, Barlow DH. Structural relationships among dimensions of the DSM–IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology. 1998;107:179–192. doi: 10.1037//0021-843x.107.2.179. [DOI] [PubMed] [Google Scholar]
- Clark DA, Steer RA, Beck AT. Common and specific dimensions of self-reported anxiety and depression: Implications for the cognitive and tripartite models. Journal of Abnormal Psychology. 1994;103:645–654. [PubMed] [Google Scholar]
- Clark LA, Watson D. Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. Journal of Abnormal Psychology. 1991;100:316–336. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd edition. Hillsdale, NJ: Erlbaum; 1992. [Google Scholar]
- Cox BJ, Clara IP, Enns MW. Posttraumatic stress disorder and the structure of common mental disorders. Depression and Anxiety. 2002;15:168–171. doi: 10.1002/da.10052. [DOI] [PubMed] [Google Scholar]
- Denson TF, Marshall GN, Schell TL, Jaycox LH. Predictors of posttraumatic distress one year after exposure to community violence: The importance of acute symptom severity. Journal of Consulting and Clinical Psychology. 2007;75:683–692. doi: 10.1037/0022-006X.75.5.683. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. SCL-90-R: Administration, scoring and procedures manual--II. Baltimore, MD: Clinical Psychometric Research; 1992. [Google Scholar]
- Derogatis LR, Savitz KL. The SCL-90-R, Brief Symptom Inventory, and matching Clinical Rating Scales. In: Maruish ME, editor. The use of psychological testing for treatment planning and outcomes assessment. Mahwah, NJ: Erlbaum; 1999. pp. 679–724. [Google Scholar]
- DuHamel KN, Ostroff J, Ashman T, Winkel G, Mundy EA, Keane TM, et al. Construct validity of the Posttraumatic Stress Disorder Checklist in cancer survivors: Analyses based on two samples. Psychological Assessment. 2004;16:255–266. doi: 10.1037/1040-3590.16.3.255. [DOI] [PubMed] [Google Scholar]
- Elklit A, Shevlin M. The structure of PTSD symptoms: A test of alternative models using confirmatory factor analysis. British Journal of Clinical Psychology. 2007;46:299–313. doi: 10.1348/014466506X171540. [DOI] [PubMed] [Google Scholar]
- Grant DM, Beck JG, Marques L, Palyo SA, Clapp JD. The structure of distress following trauma: Posttraumatic stress disorder, major depressive disorder, and generalized anxiety disorder. Journal of Abnormal Psychology. 2008;117:662–672. doi: 10.1037/a0012591. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- King DW, Leskin GA, King LA, Weathers FW. Confirmatory factor analysis of the Clinician-Administered PTSD Scale: Evidence for the dimensionality of Posttraumatic Stress Disorder. Psychological Assessment. 1998;10:90–96. [Google Scholar]
- Krause ED, Kaltman S, Goodman LA, Dutton M. Longitudinal factor structure of posttraumatic stress symptoms related to intimate partner violence. Psychological Assessment. 2007;19:165–175. doi: 10.1037/1040-3590.19.2.165. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF. The structure of common mental disorders. Archives of General Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Markon KE. Reinterpreting comorbidity: A Model-based approach to understanding and classifying psychopathology. Annual Review of Clinical Psychology. 2006;2:111–133. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsh HW, Hau KT, Wen ZL. In search of golden rules: Comment on hypothesis testing approaches to setting cutoff values for fit indexes and dangers in overgeneralising Hu & Bentler (1999) findings. Structural Equation Modeling. 2004;11:320–341. [Google Scholar]
- Marshall GN, Schell TL, Glynn SM, Shetty V. The role of hyperarousal in the manifestation of posttraumatic psychological distress following injury. Journal of Abnormal Psychology. 2006;115:624–628. doi: 10.1037/0021-843X.115.3.624. [DOI] [PubMed] [Google Scholar]
- Marshall GN, Schell TL, Elliott MN, Rayburn NR, Jaycox LH. Psychiatric disorders among adults seeking emergency disaster assistance after a wildland-urban interface fire. Psychiatric Services. 2007;58:509–514. doi: 10.1176/ps.2007.58.4.509. [DOI] [PubMed] [Google Scholar]
- McWilliams LA, Cox BJ, Asmundson GJG. Symptom structure of posttraumatic stress disorder in a nationally representative sample. Journal of Anxiety Disorders. 2005;19:626–641. doi: 10.1016/j.janxdis.2004.06.003. [DOI] [PubMed] [Google Scholar]
- Miles JN, Marshall GN, Schell TL. Spanish and English versions of the PTSD Checklist-Civilian version (PCL-C): Testing for differential item functioning. Journal of Trauma Stress. 2008;21:369–376. doi: 10.1002/jts.20349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mineka S, Watson D, Clark LA. Comorbidity of anxiety and unipolar mood disorders. Annual Review of Psychology. 1998;49:377–412. doi: 10.1146/annurev.psych.49.1.377. [DOI] [PubMed] [Google Scholar]
- Muthén B, Muthén L. Mplus 4.2. Los Angeles: Muthén and Muthén; 2006. [Google Scholar]
- Naifeh JA, Elhai DJ, Kashdan TB, Grubaugh AL. The PTSD Symptom Scale’s latent structure: An examination of trauma-exposed medical patients. Journal of Anxiety Disorders. 2008;22:1355–1368. doi: 10.1016/j.janxdis.2008.01.016. [DOI] [PubMed] [Google Scholar]
- Palmieri PA, Fitzgerald LF. Confirmatory factor analysis of posttraumatic stress symptoms in sexually harassed women. Journal of Traumatic Stress. 2005;18:657–666. doi: 10.1002/jts.20074. [DOI] [PubMed] [Google Scholar]
- Palmieri PA, Marshall G, Schell TL. Confirmatory factor analysis of posttraumatic stress symptoms in Cambodian refugees. Journal of Traumatic Stress. 2007a;20:207–216. doi: 10.1002/jts.20196. [DOI] [PubMed] [Google Scholar]
- Palmieri PA, Weathers FW, Difede J, King DW. Confirmatory factor analysis of the PTSD Checklist and the Clinician-Administered PTSD Scale in disaster workers exposed to the World Trade Center Ground Zero. Journal of Abnormal Psychology. 2007b;116:329–341. doi: 10.1037/0021-843X.116.2.329. [DOI] [PubMed] [Google Scholar]
- Ramchand R, Marshall GN, Schell TL, Jaycox LH. Posttraumatic distress and physical functioning: A longitudinal study of injured survivors of community violence. Journal of Consulting and Clinical Psychology. 2008;76:668–676. doi: 10.1037/0022-006X.76.4.668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satorra A, Bentler P. A scaled difference chi-square test statistic for moment structure analysis. Los Angeles: UCLA; 1999. [Google Scholar]
- Schell TL, Marshall GN, Jaycox LH. All symptoms are not created equal: The prominent role of hyperarousal in the natural course of posttraumatic psychological distress. Journal of Abnormal Psychology. 2004;113:189–197. doi: 10.1037/0021-843X.113.2.189. [DOI] [PubMed] [Google Scholar]
- Simms LJ, Grös DF, Watson D, O’Hara MW. Parsing the general and specific components of depression and anxiety with bifactor modeling. Depression and Anxiety. 2008;25:34–46. doi: 10.1002/da.20432. [DOI] [PubMed] [Google Scholar]
- Simms LJ, Watson D, Doebbeling BN. Confirmatory factor analyses of posttraumatic stress symptoms in deployed and nondeployed veterans of the Gulf War. Journal of Abnormal Psychology. 2002;111:637–647. doi: 10.1037//0021-843x.111.4.637. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, First MB, Wakefield JC. Saving PTSD from itself in DSM-V. Journal of Anxiety Disorders. 2007;21:233–241. doi: 10.1016/j.janxdis.2006.09.006. [DOI] [PubMed] [Google Scholar]
- Tucker LR, Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38:1–10. [Google Scholar]
- Watson D. Differentiating the mood and anxiety disorders: A quadripartite model. Annual Review of Clinical Psychology. 2009;5:221–247. doi: 10.1146/annurev.clinpsy.032408.153510. [DOI] [PubMed] [Google Scholar]
- Watson D. Rethinking the mood and anxiety disorders: A quantitative hierarchical model for DSM–V. Journal of Abnormal Psychology. 2005;114:522–536. doi: 10.1037/0021-843X.114.4.522. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Weber K, Assenheimer JS, Strauss ME, McCormick RA. Testing a tripartite model: II. Exploring the symptom structure of anxiety and depression in student, adult, and patient samples. Journal of Abnormal Psychology. 1995;104:15–25. doi: 10.1037//0021-843x.104.1.15. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska J, Keane TM. The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. Ninth annual meeting of the International Society for Traumatic Stress Studies; San Antonio. 1993. [Google Scholar]
- Yuan KH, Bentler PM. Three likelihood-based methods for mean and covariance structure analysis with nonnormal missing data. In: Sobel ME, Becker MP, editors. Sociological Methodology 2000. Washington, DC: ASA; 2000. [Google Scholar]