Abstract
Background
Occupational heat stress is a well-known problem, particularly in tropical countries, affecting workers, health and well-being. There are very few recent studies that have reported on the effect of heat stress on mental health, or overall health in workers, although socioeconomic development and rapid urbanization in tropical developing countries like Thailand create working conditions in which heat stress is likely.
Objective
This study is aimed at identifying the relationship between self-reported heat stress and psychological distress, and overall health status in Thai workers.
Results
18% of our large national cohort (>40,000 subjects) often works under heat stress conditions and males are exposed to heat stress more often than females. Furthermore, working under heat stress conditions is associated with both worse overall health and psychological distress (adjusted odds ratios ranging from 1.49 to 1.84).
Conclusions
This association between occupational heat stress and worse health needs more public health attention and further development on occupational health interventions as climate change increases Thailand's temperatures.
Keywords: occupational heat stress, psychological distress, poor overall health, Thailand
Exposure to extreme heat conditions has been found to be hazardous to health and has been linked in many studies to a range of illnesses and premature death (1–4). Workers frequently exposed to heat in their workplace have been found to suffer heat exhaustion, heat stroke, kidney disease, heart or lung disease, accidents, and injuries (5–8). This is especially true for those people whose occupation involves performing physical labor outdoors, who are exposed to higher-than-normal ambient temperatures combined with the body heat generated by the jobs themselves (7, 9).
Factors such as pre-existing disease, clothing, age, gender, ability for heat acclimatization, level of physical activity, and body size, can influence the health impact of heat stress (6, 10, 11). Moreover, socioeconomic factors such as income and urbanization can compound the adverse health outcomes from heat stress (9). For example, poor farmers and laborers are at greatest risk of heat stress due to prolonged heat exposure during hot days, in contrast to urban workers who have middle or high incomes, and are likely to install air conditioning in their dwellings and offices (7). Additionally, infrastructure, buildings, roads, and other major physical structures capture and absorb solar heat radiation in urban areas, causing the temperature to rise faster and to higher levels than in rural areas because of the ‘urban heat island effect’ (12), thus laborers in urban areas may experience the largest temperature-related health risk.
Kjellstrom et al. (7) have identified the potential occupational health problems that climate change and associated increased heat exposure might cause, especially in low- and middle-income countries in tropical areas. For example, heat stroke has been reported among laborers in gold mines in South Africa, and heat stress has been noticed to lower productivity among female workers in a shoe factory in Vietnam (9). They suggest that more research is needed on links between heat stress and adverse health outcomes in working populations, especially in developing countries.
We have conducted such preliminary research in Thailand, a tropical developing country with a large working population commonly exposed to heat with both high air temperature and humidity, particularly during the hot season. Moreover, the mean temperature in Thailand has already increased 0.74°C in the past 40 years, and it is expected that extreme temperature events will become more prevalent in the future (13). However, heat effects on health have received little attention in Thailand and there are very few studies on occupational heat stress and heat-related illness (6, 14) and no published studies report on the effects of heat stress at work on mental health in the Thai context.
Berry et al. (15) illustrated that the increasing heat exposure on workers in tropical countries as an effect of climate change may indirectly cause psychological distress in workers due to reduced work productivity, lost income, and disrupted daily social activity . Therefore, here we present an analysis of self-reported mental and overall health and their association with heat stress among workers in a large national cohort study underway in Thailand. We also note the influence of age, sex, job type and location, income, education, and other work hazards among a group experiencing socioeconomic development, rapid urbanization, demanding jobs, and long working hours in hot conditions.
Methodology
Data
The data derive from the baseline measurements of a large national Thai Cohort Study (TCS) that began in 2005, researching the health-risk transition in the adult Thai population. The study began with a 20-page mailout questionnaire covering social demography, work, health and injuries, social networks and well-being, diet and physical activity, and tobacco, alcohol, and transport. There were 87,134 respondents aged 15–87 years enrolled as distance learning students at Sukhothai Thammathirat Open University (STOU). Further details about the questionnaire data collection and the attributes of respondents are given in Sleigh et al. (16).
Measurements
The information on individual experiences of heat stress was derived from the question: ‘During the last 12 months, how often have you experienced at work high temperatures which make you uncomfortable?’, which 76,113 respondents answered on a four-point scale (‘often,’ ‘sometimes,’ ‘rarely,’ and ‘never’). For analysis, self-reported occupational heat stress was dichotomized into often or not often.
Outcomes assessed were self-reported poor overall health and psychological distress. Poor overall health is based on the first question of the Medical Outcomes short form instrument (SF8) – ‘overall how would you rate your health during the past four weeks (excellent, very good, good, fair, poor, or very poor).’ For analysis, we combined the last two categories as ‘poor overall health’ and the first four categories as ‘not poor overall health.’ Psychological distress is based on the three anxiety-oriented questions of the standard Kessler 6 psychological distress questions: ‘in the past 4 weeks, about how often did you feel … (nervous, restless or fidgety, or everything was an effort)’ with answers on a five-point scale (1=all of the time, 2=most of the time, 3=some of the time, 4=a little of the time, 5=none of the time). For our analysis, if the average response for the three questions was less than or equal to 2, the respondent was classified as psychologically distressed.
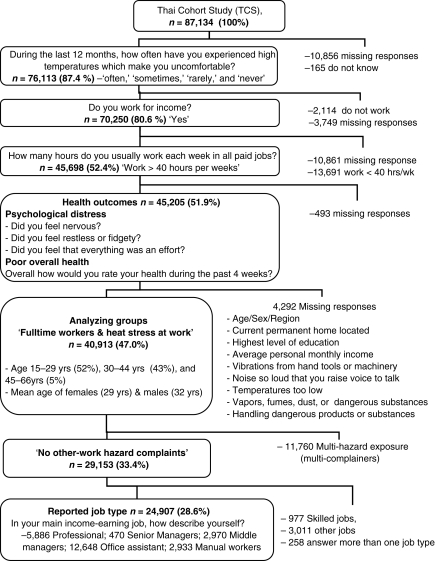
The population hierarchy for participant analysis is shown in Fig. 1. Overall, most of those excluded did not answer the questions regarding work or were not working in paid employment for at least 40 hours per week. All respondents reported age, sex, education, income, location of job, job type, and five other hazards at work (beside high temperature); data on these variables were collected because they could confound or modify our estimates of the association between overall health, psychological distress, and occupational heat stress.
Fig. 1.
Selection process for the analyzed population from the Thai Cohort Study data.
For analysis, age in years was divided into three categories (15–29, 30–44, >45), highest education was divided into three categories (high school, diploma, or university), monthly income (in Thai Baht) was divided into four categories (‘up to 7,000,’ ‘7,001–10,000,’ ‘10,001–20,000,’ and ‘20,001 and more’), and job location was divided into three categories (Bangkok, urban-outside Bangkok, and rural). Some analyses were restricted to the population providing information on job type categorized as office job or physical job (those reporting as ‘skilled workers’ were excluded because we could not categorize them further). Complaints about five other hazards at work (vibrations from tools or machines, loud noise, uncomfortably low temperatures, dangerous fumes (vapors, chemicals, infectious agents), and touching dangerous substances) were each also categorized as often/not often and the ‘often’ results combined into three levels (0 other complaints, 1–2 other complaints, 3–5 other complaints).
Data analysis
Data were digitized using Thai Scandevet software and further processed using SPSS and Stata statistical packages. The initial analysis group included 40,913 fulltime workers for overall heat stress analyses. Final heat stress analyses were restricted to the 24,907 workers whose job type was known (allowing assessment of this variable) and who did not make non-thermal work hazard complaints (preventing any influence on the results of adverse effects of ‘multiple hazard complainers’).
Summary statistics (means and proportions by variable category and sex) were prepared for heat stress, age, education, income, job, and work hazard complaints. All explanatory variables (i.e. sex, age, job location, job type, education, income, other work hazards) were assessed as potential confounders of our estimates of heat stress associations on health outcomes by investigating their association with the exposure of interest (heat stress) or the outcomes (overall health or psychological distress). Both outcomes were assessed graphically for association with heat stress and these analyses were broken down by age group (15–29, 30–44, >45 years) and sex.
The association between heat stress and overall health or psychological distress was assessed by odds ratios (ORs) and 95% confidence intervals. Using multivariable logistic regression, these heat stress ORs were adjusted for the influence of all confounding variables (sex, age, job type, job location, education, income, and complaints of other work hazards). These variables were also evaluated as potential modifiers of heat stress associations by stratified analyses that estimated the ORs separately for each category (i.e. by sex, age group, education group, income group, complaint group, job location, job type and by the joint effect of job type and location). Each stratified OR was adjusted for the confounding influence of other explanatory variables (e.g. sex, age group, etc.).
Finally, using stepwise logistic regression to include only significant confounders and heat stress interaction terms, models were prepared to show the fully adjusted heat stress association on overall health and on psychological distress. The final model for the 40,913 fulltime workers for overall health included heat stress, sex, age, education, other complaints, job location, and two interaction terms (education×heat, and other complaints×heat). The final model for psychological distress included heat stress, sex, age, education, income, other complaints, job location, and an interaction term for other complaints×heat. When job type was offered for the stepwise models and these workers were potentially exposed to heat stress only (restricted data set, n=24,907), the final model for both poor health and psychological distress included heat stress, sex, age, and job location. There were no significant interaction terms in these final models linking heat stress to either health outcome.
Ethical issues
Ethical approval was obtained from STOU Research Committee and the Australian National University Human Research Ethics Committee (ANU HREC). Informed written consent was obtained from all participants.
Results
Characteristics of the cohort
Tables 1 and 2, and Fig. 1 present the main characteristics of all 40,913 Thai cohort members who were fulltime workers. Overall, 56% were female. More than half the cohort was young, aged between 15 and 29 years (52%). Nearly 20% of workplaces were located in Bangkok, 41% were in other urban areas (outside Bangkok), and 39% were in rural areas, 19% of classifiable jobs were physical and 81% were based in an office. Compared with males, females were younger and worked in Bangkok (22 vs 17%). On average, women had moderately higher educational achievements whereas men had substantially higher personal incomes. Overall, 5% of fulltime workers reported often experiencing three to five other hazards beside high temperature at work, more for males (6%) than females (3%). Over 18% (n=7,476) of the analyzed group reported they often experienced uncomfortably high temperatures at work (Table 2). This problem was worse for males (23%) than females (15%); also females more frequently than males reported never experiencing heat stress at work (27 vs 17%).
Table 1.
Socioeconomic and other attributes in a cohort of 40,913 fulltime workers in Thailand
| Male | Female | Total | ||||
|---|---|---|---|---|---|---|
| Attributes | n | % | n | % | n | % |
| Total | 18,148 | 44.7 | 22,765 | 55.6 | 40,913 | 100.0 |
| Job location | ||||||
| Bangkok | 3,117 | 17.2 | 4,961 | 21.8 | 8,078 | 19.7 |
| Urban | 7,682 | 42.3 | 8,955 | 39.3 | 16,637 | 40.7 |
| Rural | 7,349 | 40.5 | 8,849 | 38.9 | 16,198 | 39.6 |
| Job typea | ||||||
| Office | 11,708 | 81.0 | 17,042 | 85.2 | 28,750 | 83.4 |
| Physical | 2,741 | 19.0 | 2,970 | 14.8 | 5,711 | 16.6 |
| Education | ||||||
| University | 5,271 | 29.0 | 6,925 | 30.4 | 12,196 | 29.8 |
| Diploma | 4,900 | 27.0 | 8,208 | 36.1 | 13,108 | 32.0 |
| High school | 7,977 | 44.0 | 7,632 | 33.5 | 15,609 | 38.2 |
| Personal income (Baht/month) | ||||||
| 20,001+ | 2,554 | 14.1 | 1,930 | 8.5 | 4,484 | 11.0 |
| 10,001–20,000 | 6,353 | 35.0 | 5,862 | 25.7 | 12,215 | 29.9 |
| 7,001–10,000 | 5,121 | 28.2 | 6,626 | 29.1 | 11,747 | 28.7 |
| <7,000 | 4,120 | 22.7 | 8,347 | 36.7 | 12,467 | 30.5 |
| Other work hazard complaints | ||||||
| No other complaints | 12,669 | 69.8 | 16,484 | 72.4 | 29,153 | 71.3 |
| Scored 1–2 items with ‘often’ | 4,436 | 24.4 | 5,501 | 24.2 | 9,937 | 24.3 |
| Scored 3–5 items with ‘often’ | 1,043 | 5.8 | 780 | 3.4 | 1,823 | 4.5 |
| Overall health | ||||||
| No poor overall health | 17,484 | 96.3 | 21,503 | 94.5 | 38,987 | 95.3 |
| Poor overall health | 664 | 3.8 | 1,262 | 5.6 | 1,926 | 4.7 |
| Psychological distress | ||||||
| Not psychologically distressed | 16,807 | 92.6 | 20,714 | 90.99 | 37,521 | 91.71 |
| Psychologically distressed | 1,341 | 7.4 | 2,051 | 9.0 | 3,392 | 8.3 |
aJob type is available for analysis with 24,907 respondents (see Section ‘Methods’).
Table 2.
Reported heat stress at work in a cohort of 40,913 fulltime workers in Thailand
| Experience high temperature | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Often | Sometimes | Rarely | Never | Total | |||||||
| Sex | n | % | n | % | n | % | n | % | n | % | |
| Males | 4,081 | 22.5 | 6,187 | 34.1 | 4,743 | 26.1 | 3,137 | 17.3 | 18,148 | 44.4 | |
| Females | 3,395 | 14.9 | 6,479 | 28.5 | 6,789 | 29.8 | 6,102 | 26.8 | 22,765 | 55.6 | |
| Total | 7,476 | 18.2 | 12,666 | 30.9 | 11,532 | 28.3 | 9,239 | 22.6 | 40,913 | 100 | |
Associations of cohort attributes with heat stress, overall health, and psychological distress
Heat stress exposure together with health and psychological distress outcomes are summarized in Table 3. Here we explore the associations of heat stress exposures and health outcomes with potential confounders of the heat stress effects. The prevalence of heat stress (‘often’ experiencing high temperatures at work (n=40,913)) varied considerably among subgroups and was notably high for those with other complaints regarding hazards at work. Nearly 5% of workers reported poor overall health and this figure rose to 9% for those reporting often being troubled by three to five other work hazards. Psychological distress was more common; overall, it affected 8% of workers and was reported by 20% of those with three to five other work hazards.
Table 3.
Heat stress, poor overall health, and psychological distress by potential confounding factors in a cohort of 40,913 fulltime workers
| Heat stress | Poor overall health | Psychological distress | |||||||
|---|---|---|---|---|---|---|---|---|---|
| % | ORa | 95% CI | % | ORa | 95% CI | % | ORa | 95% CI | |
| Total | 18.3 | 4.7 | 8.3 | ||||||
| Sex | |||||||||
| Males | 22.5 | 1 | 3.8 | 1 | 7.4 | 1 | |||
| Females | 14.9 | 0.60** | 0.57–0.63 | 5.6 | 1.55** | 1.40–1.70 | 9.0 | 1.24** | 1.16–1.35 |
| Age group (%) | |||||||||
| 15–29 | 18.2 | 1 | 5.1 | 1 | 9.9 | 1 | |||
| 30–44 | 18.6 | 1.02 | 0.97–1.07 | 4.5 | 0.87* | 0.79–0.95 | 6.7 | 0.65** | 0.60–0.70 |
| >45 | 16.4 | 0.88* | 0.78–0.99 | 3.9 | 0.71* | 0.56–0.90 | 4.3 | 0.41** | 0.33–0.52 |
| Job location | |||||||||
| Bangkok | 14.0 | 1 | 5.8 | 1 | 9.5 | 1 | |||
| Urban | 18.6 | 1.39** | 1.30–1.50 | 4.8 | 0.81* | 0.72–0.92 | 8.3 | 0.86* | 0.78–0.95 |
| Rural | 20.1 | 1.54** | 1.43–1.66 | 4.1 | 0.70** | 0.62–0.79 | 7.7 | 0.80** | 0.72–0.88 |
| Job typeb | |||||||||
| Office | 10.6 | 1 | 3.9 | 1 | 6.6 | 1 | |||
| Physical | 14.3 | 1.40** | 1.26–1.57 | 3.8 | 0.99 | 0.81–1.21 | 6.4 | 0.97 | 0.83–1.14 |
| Education | |||||||||
| University | 15.3 | 1 | 4.9 | 1 | 7.8 | 1 | |||
| Diploma | 17.1 | 1.14** | 1.06–1.22 | 4.7 | 0.99 | 0.88–1.11 | 8.9 | 1.16* | 1.06–1.28 |
| High school | 21.6 | 1.52** | 1.43–1.62 | 4.8 | 0.96 | 0.86–1.09 | 8.2 | 1.05 | 0.97–1.62 |
| Personal income (Baht/month) | |||||||||
| 20,001+ | 12.6 | 1 | 4.4 | 1 | 5.8 | 1 | |||
| 10,001–20,000 | 18.1 | 1.54** | 1.39–1.70 | 4.5 | 0.99 | 0.83–1.17 | 7.1 | 1.26* | 1.09–1.47 |
| 7,001–10,000 | 18.9 | 1.62** | 1.46–1.78 | 5.0 | 1.16 | 0.98–1.37 | 8.8 | 1.56** | 1.36–1.81 |
| < 7,000 | 19.9 | 1.73** | 1.57–1.91 | 5.1 | 1.17 | 0.98–1.38 | 9.9 | 1.77** | 1.55–2.06 |
| Other work hazard complaints | |||||||||
| No other complaints | 11.4 | 1 | 3.9 | 1 | 6.3 | 1 | |||
| Scored 1–2 items with ‘often’ | 30.9 | 3.47** | 3.32–3.67 | 6.7 | 1.75** | 1.59–1.92 | 12.1 | 2.05** | 1.91–2.24 |
| Scored 3–5 items with ‘often’ | 59.4 | 11.34** | 10.26–12.54 | 8.9 | 2.48** | 2.09–2.94 | 19.5 | 3.60** | 3.13–4.06 |
aAssociations with heat stress, poor overall health, and psychological distress each expressed as crude odds ratios (ORs).
bJob type analysis is restricted to 24,907 respondents (see Section ‘Methods’).
* P <0.05;
** P <0.001.
In almost all instances the potential confounders shown in Table 3 (sex, age group, education, income, job type, job location, and other work hazard complaints) were significantly associated with both the exposure of interest (heat stress) and the two outcomes (overall health and psychological distress). Accordingly, our analyses of heat stress effects were adjusted for these confounding variables, or restricted to exclude all those respondents who had multiple work hazard complaints.
Effect of heat stress on overall health and psychological distress
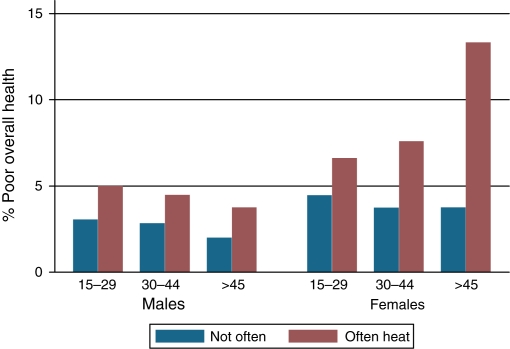
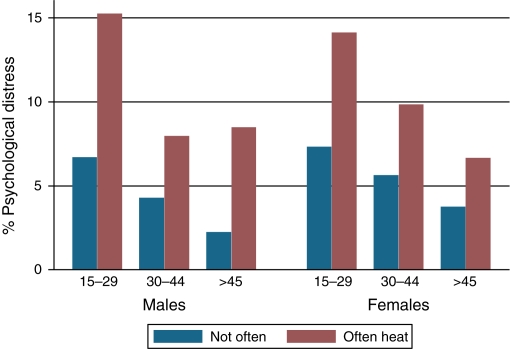
Figs. 2 and 3 reveal the positive association between heat stress and poor health or psychological distress stratified by age group and sex. This analysis was restricted to the 24,907 workers who did not complain of multiple work hazards and whose job type was known. The association between overall health, psychological distress, and occupational heat stress are substantial and revealed no consistent pattern with age. Generally, the adverse effects of heat stress on poor health were worse for females; the opposite association was noted for heat stress and psychological distress, which was especially bad for males aged between 15 and 29 years.
Fig. 2.
Prevalence of reported ‘poor overall health’ by age group, sex, and reported occupational heat stress in 24,907 Thai workers.
Fig. 3.
Prevalence of reported ‘psychological distress’ by age group, sex, and reported occupational heat stress in 24,907 Thai workers.
Modifications of the heat stress effects are summarized in Table 4. For both outcomes, the heat stress effects are increased for workers aged more than 45 years and for the better educated, and for work located in rural areas, but none of these interactions are strong. Perhaps the most notable interaction is the attenuation of heat stress associations among those with multiple work hazard complaints; for example, the association of heat stress and overall health (OR=1.75) compares to an OR of 1.22 for those with three to five complaints.
Table 4.
Stratified odds ratios revealing interaction of demographic and work-related variables with the association between overall health, psychological distress, and occupational heat stress (n=40,913)
| Poor overall health | Psychological distress | ||||
|---|---|---|---|---|---|
| Variables | Heat stress (n)a | ORb | 95% CI | ORb | 95% CI |
| Sex | |||||
| Males | 4,081 | 1.40** | 1.17–1.69 | 1.95** | 1.72–2.22 |
| Females | 3,395 | 1.55** | 1.35–1.79 | 1.78** | 1.59–1.99 |
| Age group | |||||
| 15–29 | 3,906 | 1.38** | 1.18–1.60 | 1.80** | 1.62–2.01 |
| 30–44 | 3,234 | 1.57** | 1.31–1.87 | 1.86** | 1.62–2.14 |
| >45 | 336 | 1.83* | 1.05–3.18 | 2.35* | 1.42–3.88 |
| Education | |||||
| University | 1,867 | 1.94** | 1.58–2.37 | 2.04** | 1.73–2.40 |
| Diploma | 2,240 | 1.26* | 1.02–1.55 | 1.85** | 1.60–2.15 |
| High school | 3,369 | 1.38* | 1.15–1.66 | 1.70** | 1.48–1.94 |
| Income | |||||
| 20,001+ | 563 | 1.76* | 1.20–2.57 | 1.99** | 1.42–2.77 |
| 10,001–20,000 | 2,214 | 1.55** | 1.24–1.92 | 1.74** | 1.47–2.06 |
| 7,001–10,000 | 2,215 | 1.39* | 1.13–1.72 | 1.71** | 1.47–2.00 |
| <7,000 | 2,484 | 1.46** | 1.20–1.77 | 1.99** | 1.73–2.28 |
| Complaint effect | |||||
| No other complaints | 3,324 | 1.75** | 1.49–2.06 | 2.21** | 1.96–2.49 |
| Scored 1–2 items with ‘often’ | 3,070 | 1.33* | 1.12–1.58 | 1.54** | 1.36–1.75 |
| Scored 3–5 items with ‘often’ | 1,082 | 1.22* | 0.87–1.71 | 1.80** | 1.39–2.32 |
| Job location | |||||
| Bangkok | 1,133 | 1.36* | 1.06–1.76 | 1.88** | 1.55–2.29 |
| Urban | 3,089 | 1.49** | 1.25–1.77 | 1.75** | 1.54–2.00 |
| Rural | 3,254 | 1.53** | 1.27–1.84 | 1.90** | 1.66–2.18 |
| Job typec | |||||
| Physical | 420 | 1.91* | 1.21–3.00 | 1.87* | 1.30–2.68 |
| Office | 2,338 | 1.79** | 1.48–2.15 | 2.24** | 1.94–2.58 |
| Job location/typec | |||||
| Bangkok/office | 251 | 2.41** | 1.52–3.80 | 2.62** | 1.84–3.74 |
| Bangkok/physical | 58 | 0.91 | 0.25–3.18 | 1.10 | 0.36–3.38 |
| Urban/office | 945 | 1.84** | 1.37–2.45 | 2.04** | 1.62–2.56 |
| Urban/physical | 150 | 2.32* | 1.13–4.75 | 1.41 | 0.75–2.65 |
| Rural/office | 1,142 | 1.55* | 1.15–2.07 | 2.35** | 1.90–2.90 |
| Rural/physical | 212 | 2.15* | 1.08–4.28 | 2.49** | 1.50–4.11 |
aNumber of respondents who reported heat stress at work (see Section ‘Methods’).
bOdds ratios show within-strata estimates for heat stress associations adjusted for all other explanatory variables.
cJob type analysis restricted to 24,907 respondents (see ‘Methods’).
* P<0.05;
** P<0.001.
Table 5 shows crude and adjusted OR estimates for associations between heat stress and poor health and psychological distress outcomes. The adjusted ORs derive from models that include age, sex, income, education, job location, and other work hazard complaints. Cohort members who experienced heat stress at work had higher odds of poor overall health (crude OR=1.67, P-value <0.001; adjusted OR=1.49, P-value <0.001). They also had higher odds of psychological distress (crude OR=2.22, P<0.001; adjusted OR=1.84, P-value <0.001). For workers who did not complain of other work hazards and for whom job type was reported (n=24,907), the adjusted heat stress models ORs for poor health (1.80) and psychological distress (2.19) differ little from previous estimates.
Table 5.
The association between occupational heat stress, overall health, and psychological distress
| Poor overall health | Psychological distress | ||||
|---|---|---|---|---|---|
| Heat stress | OR | 95% CI | OR | 95% CI | |
| Heat stress (crude estimate) | |||||
| n=40,913 | Not often | 1 | 1 | ||
| Often | 1.67** | 1.50–1.85 | 2.22** | 2.06–2.40 | |
| All variables (adjusted)a | |||||
| n=40,913 | Not often | 1 | 1 | ||
| Often | 1.49** | 1.32–1.66 | 1.84** | 1.69–2.00 | |
| All variables (adjusted)a | |||||
| Restricted n=24,907 | Not often | 1 | 1 | ||
| Often | 1.80** | 1.51–2.14 | 2.19** | 1.92–2.50 | |
| Final models | |||||
| Final model includes interact termsb | |||||
| n=40,913 | Not often | 1 | 1 | ||
| Often | 1.55** | 1.87–3.38 | 2.21** | 1.89–2.37 | |
| Final modelc | |||||
| Restricted n=24,907 | Not often | 1 | 1 | ||
| Often | 1.81** | 1.52–2.15 | 2.17** | 1.90–2.48 | |
* P<0.05;
** P<0.001.
aAdjusted ORs derived from heat stress models that included sex, age, income, education, job location, and complaints (n=40,913) plus job type (n=24,907).
bFinal model for estimating the association between heat stress and poor overall health includes all statistically significant confounders (sex, age, education, complaints, job location), and the two significant interaction terms (education×heat and complaints× heat). Final model for estimating the association between heat stress and psychological distress includes all statistically significant confounders (sex, age, education, income, complaints, job location) and the one significant interaction term (complaints×heat).
cFinal model in restricted group (n=24,907) for association between heat stress and both poor overall health and psychological distress includes all statistically significant confounders (sex, age, and job location).
The final logistic regression models included all significant confounders and all significant interactors (see Section ‘Methods’ and footnote of Table 5). The final ORs linking heat stress to poor overall health were 1.55 (n=40,913) and 1.81 (when restricted to those reporting job type and no other work hazard complaints, n=24,907). For psychological distress, the corresponding final adjusted ORs were similar for the two analytical groups (2.21 for n=40,913 and 2.17 for n=24,907). Accordingly, these final models show considerable and consistent strength of association between heat stress and health outcomes, and the confidence limits and p-values show results unlikely to be due to chance.
Discussion
Statement of principal findings
These findings add to the limited literature on the association between overall health, psychological distress, and occupational heat stress of Thai workers (17). We found heat stress exposure reported by nearly 20% of our large national cohort, more frequently among laborers and male workers, those with low incomes and low education, and declining with age possibly due to an age-related shift away from physical work. Occupational heat stress was reported less frequently in Bangkok, probably reflecting air conditioning in Thai cities, especially in Bangkok (9).
The proportion of male workers who reported poor health and psychological distress declined with age. This was especially noteworthy for psychological distress, possibly reflecting longer work experience and the ability to control emotions among older men. For women, the trend of less psychological distress with advancing age was similar. However, heat-stressed females did show a trend of worsening overall health with increasing age, which may reflect aging as well as more responsibilities and daily stress from the mix of professional work and homemaking once a family has formed. This finding is similar to Lennon (1995), who found that women have substantially higher psychological distress than men (18). However, in our study, men aged between 15 and 29 years reported the highest prevalence of distress (Fig. 3), which may be linked to the high rates of suicide and distress in young men in Thailand (19).
Our principal finding is that heat stress was strongly and significantly associated with both poor overall health and psychological distress, with adjusted ORs ranging from 1.49 to 1.84. These epidemiological associations remained substantial and highly significant statistically when extensively adjusted for confounding (by age, sex, income, education, and job location) and when restricted to those who did not have other (non-thermal) work hazard complaints (i.e. non-complainers). The strength of association between overall health, psychological distress, and occupational heat stress interacts weakly with an array of other sociodemographic variables. However, none of the interactions significantly modified the heat stress associations.
Strengths and weaknesses of the study
Access to a large national cohort of 40,913 Thai workers is the main advantage of this study. It represents working-age Thais reasonably well for geographic location, age, sex, and socioeconomic status (16). Cohort members are better educated than average Thais of the same age and sex, but this difference enabled us to gather complex heat exposure and health outcomes on large numbers by questionnaire. This is the first time such a study has been attempted. The cohort shows a wide range of values for the variables of interest, allowing us to investigate the relationship between heat stress at work and health outcomes.
Furthermore, we can be reassured of our results by the restricted analyses of 24,907 workers with all the multi-complainers excluded and job types known. The results are similar to the overall analysis of 40,913 cohort members that was adjusted for confounding and interaction. However, this study could not directly establish that these overall health problems and psychological distress arose as a result of heat stress. There are some difficulties in interpreting these data on exposure patterns and associated health outcomes given that we cannot be sure that heat stress preceded adverse outcomes. Moreover, the source or nature of the heat stress or the work situations was not categorized in this study. Indeed, we were not able to make a direct measurement of work environments or health outcomes, hence we must classify this study as preliminary in nature. Therefore, there is need for more detailed direct observations in informative work settings to validate our findings and explore the underlying mechanisms.
We were able to find only one other study (an unpublished thesis) of thermal environment and mental health in Thailand, among a small population of 90 workers in a seafood factory (17). This factory study did not document heat stress (but did measure temperature); nor did it find evidence of widespread psychological distress. Although, there are reports on occupational heat exposure and comfort of workers, they do not usually mention psychological distress or mental health problems as a variable (11, 14). Therefore, our study is one of the first to provide evidence on an association between heat stress and psychological distress of workers.
Significance of this study
This is the first large-scale study of occupational heat stress and adverse health outcomes in Thailand. The findings of widespread heat stress and associated ill-health are disturbing. This is particularly important at present because we can expect that the existing problem will worsen if global warming continues and workplaces become even more thermally stressful. Given the constrained resources in middle-income Thailand, and the possibility that psychologically stressful work is becoming more widespread, our results on psychological distress are of particular concern. If workers exposed to excessive heat cannot cool down, they can experience severe psychological distress caused by heat-related exhaustion or develop long-term conditions such as chronic depression or chronic anxiety disorders (11, 20). Furthermore, Ramsey (21) reported that heat stress diminished mental ability and increased injury risks, and others have noted increased suicide risk (15, 22, 23).
Future research
Occupational heat stress requires more public health attention. Further studies are needed to accurately characterize workplace humidity, air movement, radiant temperature, health outcomes, and work performance in various settings in Thailand, especially as the workforce structure changes with economic development (24, 25).
Acknowledgements
We thank the staff at Sukhothai Thammathirat Open University (STOU) who assisted with student contact and the STOU students who are participating in the cohort study. We also thank Dr Bandit Thinkamrop and his team from Khon Kaen University for guiding us successfully through the complex data processing.
Conflict of interest and funding
This study was supported by the International Collaborative Research Grants Scheme with joint grants from the Wellcome Trust UK (GR0587MA) and the Australian NHMRC (268055).
References
- 1.Kovats S, Akhtar R. Climate, climate change and human health in Asian cities. Environ Urban. 2008;20:165–75. [Google Scholar]
- 2.Kovats R, Campbell-Lendrum D, Matthies F. Climate change and human health: estimating avoidable deaths and disease. Risk Anal. 2005;25:1409–18. doi: 10.1111/j.1539-6924.2005.00688.x. [DOI] [PubMed] [Google Scholar]
- 3.McMichael A, McGeehin, Mirabelli M. The potential impacts of climate variability and change on temperature-related morbidity and mortality in the United States. Environ Health Perspect. 2001;9:185–9. doi: 10.1289/ehp.109-1240665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Martens W. Climate change, thermal stress and mortality changes. Soc Sci Med. 1998;46:331–44. doi: 10.1016/s0277-9536(97)00162-7. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Fatalities from occupational heat exposure. Morbidity and Mortality Weekly Report 1984. Available from http://www.cdc.gov/mmwr/preview/mmwrhtml/00000376.htm [cited 24 April 2009]
- 6.Chawsithiwong B. Occupational thermal exposure. Thai J Environ Manage. 2008;4:1–26. [Google Scholar]
- 7.Kjellstrom T, Gabrysch S, Lemke B, Dear K. The “Hothaps” program for assessing climate change impacts on occupational health and productivity: an invitation to carry out field studies. Global Health Action. 2009;2 doi: 10.3402/gha.v2i0.2082. Available from: http://www.globalhealthaction.net/index.php/gha/article/view/2082/2561 [cited 19 April 2010] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rosenstock L, Cullen M. Textbook of clinical occupational and environmental medicine. New York: W.B. Saunders Company; 1994. [Google Scholar]
- 9.Kjellstrom T. Climate change, direct heat exposure, health and well-being in low and middle-income countries. Global Health Action. 2009;2:1–3. doi: 10.3402/gha.v2i0.1958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Occupational Safety and Health Administration. Heat Stress OSHA Standard. Available from http://www.osha.gov/SLTC/heatstress/standards.html [cited 25 June 2009]
- 11.Schneider J. Identification and management of thermal stress and strain; 1999. Paper presented at Queensland Mining Industry Health and Safety Conference Proceedings, Central Queensland University. [Google Scholar]
- 12.USEPA. Heat island effect. Available from http://www.epa.gov/heatislands [cited 20 October 2009]
- 13.Limsakul A, Limjirakan S, Sriburi T. Trends in daily temperature extremes in Thailand; 2009. Paper presented at the Second National Conference on Natural Resources and Environment, Bangkok, Thailand. [Google Scholar]
- 14.Taptagaporn S, Vichit-Vadakan N, Langkulsen U. Climate change impacts on occupational health in South-East Asia – a preliminary analysis based on data from Thailand. Bangkok: Faculty of Public Health, Thammasat University; 2009. [Google Scholar]
- 15.Berry HL, Bowen K, Kjellstrom T. Climate change and mental health: a causal pathways framework. Int J Public Health. 2010;55:123–32. doi: 10.1007/s00038-009-0112-0. [DOI] [PubMed] [Google Scholar]
- 16.Sleigh A, Seubsman S, Bain C Thai cohort team. Cohort profile: the Thai cohort of 87,134 open university students. Int J Epidemiol. 2008;37:266–72. doi: 10.1093/ije/dym161. [DOI] [PubMed] [Google Scholar]
- 17.Vivatpong Y. Bangkok: Department of Psychology, Kasetsart University; 1995. Effects of temperature on worker's health and working behavior in sea-food processing factories. (In Thai with English abstract.) [Google Scholar]
- 18.Lennon MC. Work conditions as explanations for the relation between socioeconomic status, gender, and psychological disorders. Epidemiol Rev. 1995;17:120–7. doi: 10.1093/oxfordjournals.epirev.a036167. [DOI] [PubMed] [Google Scholar]
- 19.Lotrakul M. Suicide in Thailand during the period 1998–2003. Psychiatry Clin Neurosci. 2006;60:90–5. doi: 10.1111/j.1440-1819.2006.01465.x. [DOI] [PubMed] [Google Scholar]
- 20.Hansen A, Bi P, Nitschke M, Ryan P, Pisaniello D, Tucker G. The effect of heat waves on mental health in a temperate Australian city. Environ Health Perspect. 2008;116:1369–75. doi: 10.1289/ehp.11339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ramsey JD. Task performance in heat: a review. Ergonomics. 1995;38:154–65. doi: 10.1080/00140139508925092. [DOI] [PubMed] [Google Scholar]
- 22.Anderson C. Heat and violence. Curr Direct Psychol Sci. 2001;10:33–8. [Google Scholar]
- 23.Page LA, Hajat S, Kovats RS. Relationship between daily suicide counts and temperature in England and Wales. Br J Psychiatry. 2007;191:106–12. doi: 10.1192/bjp.bp.106.031948. [DOI] [PubMed] [Google Scholar]
- 24.Kelly M, Strazdins L, Dellora T, Seubsman S, Sleigh A. Thailand's work and health transition. Int Labour Rev. 2010 doi: 10.1111/j.1564-913X.2010.00092.x. (in press, accepted October 2009) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Statistical Office. Report of the labour force survey. Whole kingdom quarter 4: October–December 2005. Available from http://web.nso.go.th/eng/stat/lfs_e/lfse-tab1.xls [cited 22 June 2009]