Abstract
Chronic heart failure is a clinical syndrome with a high mortality and morbidity. Despite optimal therapy, five-year survival is still only 50%. Central sleep apnoea syndrome is seen in approximately 40% of patients with congestive heart failure. Sleep apnoea syndrome can be divided into two forms in these patients: obstructive sleep apnoea syndrome (OSAS) and central sleep apnoea syndrome (CSAS, Cheyne-Stokes respiration), of which CSAS is the most common. CSAS is a form of sleep apnoea in congestive heart failure which is driven by changes in pCO2. As a consequence of apnoea-hypopnoea an imbalance in myocardial oxygen delivery/consumption ratio will develop, sympathetic and other neurohormonal systems will be activated and right and left ventricular afterload will be increased.
Sleep apnoea is associated with an increased mortality in patients with systolic heart failure. Treatment of sleep apnoea increases left ventricular ejection fraction and transplant-free survival. Because of its high prevalence, poor quality of life, poor outcome, and the beneficial effects of treatment, physicians treating patients with heart failure should be aware of central sleep apnoea. There are different treatment options, but the exact effects and indications of each option have not yet been fully determined. Further studies should be done to further investigate its prevalence, and to establish the most adequate therapy for the individual patient. (Neth Heart J 2010;18:260–3.)
Keywords: Sleep Apnoea, Sleep Apnea Syndromes, Heart Failure, Comorbidity
Chronic heart failure is a clinical syndrome with a high mortality and morbidity. Despite optimal therapy, five-year survival is still only 50%.1 In addition, chronic heart failure is accompanied by a serious reduction of quality of life. Sleep disordered breathing (SDB) affects 2 to 5% of the general population. Its prevalence in chronic heart failure is, however, much higher. When an Apnoea-Hypopnoea Index (AHI) of >15/min was used for the diagnosis of SDB, a consistent prevalence between 49 and 55% was found in various groups of heart failure patients.
Sleep apnoea syndrome can be divided in two forms in these patients: obstructive sleep apnoea syndrome (OSAS) and central sleep apnoea syndrome (CSAS, Cheyne-Stokes respiration), of which CSAS is the most common.2,3 OSAS is caused by a combination of pharyngeal anatomy, pharyngeal function and ventilatory control during sleep. CSAS is a form of sleep apnoea in congestive heart failure which is driven by changes in pCO2. As a consequence of apnoea-hypopnoea an imbalance in myocardial oxygen delivery/consumption ratio will develop, sympathetic and other neurohormonal systems will be activated and right and left ventricular afterload will be increased.3
Sleep apnoea is associated with an increased mortality in patients with systolic heart failure.3 After adjustment for various confounders, heart failure patients without CSAS lived about twice as long as heart failure patients with CSAS (90 vs 45 months). Treatment of sleep apnoea increases left ventricular ejection fraction (LVEF) and transplant-free survival.4,5 After three months of treatment, LVEF and transplant-free survival improved in 57% of patients in whom the AHI was reduced below 15/min. It therefore seems necessary to increase the awareness of sleep apnoea in physicians who treat patients with heart failure, as treatment can improve clinical outcome.
In this article we describe two patients with CSAS and briefly discuss the pathophysiology and treatment options to increase the awareness of this syndrome.
Patient A
The first patient is a male aged 62 years. His medical history shows an anterior and inferior myocardial infarction, atrial flutter, biventricular ICD, ischaemic heart failure and medication-induced hypothyroidism. Besides episodes of atrial flutter, his chronic heart failure was stable, and well treated (irbesartan, carvedilol, amiodarone, furosemide, and acenocoumarol). During an episode of atrial flutter, he reported nocturnal symptoms. He woke up frequently, snored, had witnessed apnoeas, was restless and had many dreams. During the daytime, he frequently fell asleep. Therefore, he was referred to a pulmonologist.
Based on his nocturnal problems a polysomnography(PSG) was performed, showing a predominantly Cheyne-Stokes breathing pattern with an apnoea-hypopnoea index (AHI) of 31/hour. Because of his symptoms in combination with his PSG he started treatment with continuous positive airway pressure (CPAP). After one month he felt better, was less dyspnoeic during the daytime, and slept better. After two months, a new PSG was done showing an apnoea-hypopnoea index of 15/hour. There was no significant change in atrial flutter paroxysms. After four months his exercise capacity had increased, he lost 2.5 kg in weight and had a better quality of life; he did not have to rest during the daytime and he was not limited in his activities.
Patient B
The second patient is a 74-year-old man. His medical history showed an atrial flutter, a dilated and hypokinetic left ventricle (LVEF 20%) and severe mitral valve insufficiency. He also had diabetes, renal impairment, and chronic obstructive pulmonary disease (COPD). His heart failure was well treated with candesartan, nebivolol, digoxin, bumetanide, spironolactone, simvastatin, and acenocoumarol. Despite this, his exercise capacity was very limited. He complained of dyspnoea during minimal exercise, such as walking a very short distance. His wife noticed a changed breathing pattern, more during the night than during the day, in which his breath was alternating between fast and slow. He was seen by the pulmonologist because of his nocturnal symptoms such as waking up frequently, dyspnoea, abnormal breathing pattern, in which he sometimes hyperventilates, and extreme restlessness.
A PSG showed a Cheyne-Stokes breathing pattern during the complete bed-period, with apnoeas up to 45 seconds and desaturations to 82%. This finding in combination with his symptoms was the reason to start treatment with adaptive servo ventilation (ASV), a novel device aimed at stabilising the respiration during sleep. At outpatient follow-up, a few months after starting this therapy, he had fewer complaints, slept better and was less exhausted during the day. He could walk longer distances and started cycling again. A PSG repeated after three months showed less desaturations but still some centrally disturbed sleeping pattern. After one year, a PSG showed a normal breathing pattern, without desaturations, or apnoeas (AHI <5). No changes in medication had occurred.
An echocardiogram showed a huge improvement of left ventricular ejection fraction from 20% at the start of the ASV to 50% after one year. The electrocardiogram showed no changes. The patient was very satisfied with his current condition.
Pathophysiology of CSAS in heart failure
Patients with chronic heart failure often have higher filling pressures leading to pulmonary oedema. As a consequence the pulmonary J receptors will be stretched and the patients will start hyperventilating (figure 1). By this hyperventilation, the PaCO2 drops and the patient will get under his so-called apnoea threshold and stop breathing. The PaCO2 will then rise and by the time the respiratory control centre terminates the apnoea, the patient is already hypercapnic. This hypercapnia stimulates hyperpnoea/ hyperventilation, which in turn induces hypocapnia, which allows the circle of events to start again from the beginning. The duration of the apnoea until the respiratory control centre detects the increase in carbon dioxide tension is prolonged in patients with heart failure because of the increase in circulatory time. If a PSG detects a specific crescendo-decrescendo pattern in both the abdominal and thoracic effort and airflow it is called Cheyne-Stokes respiration (figure 2). The number of hypopnoeas and apnoeas per hour are expressed in the apnoea-hypopnoea index.
Figure 1.
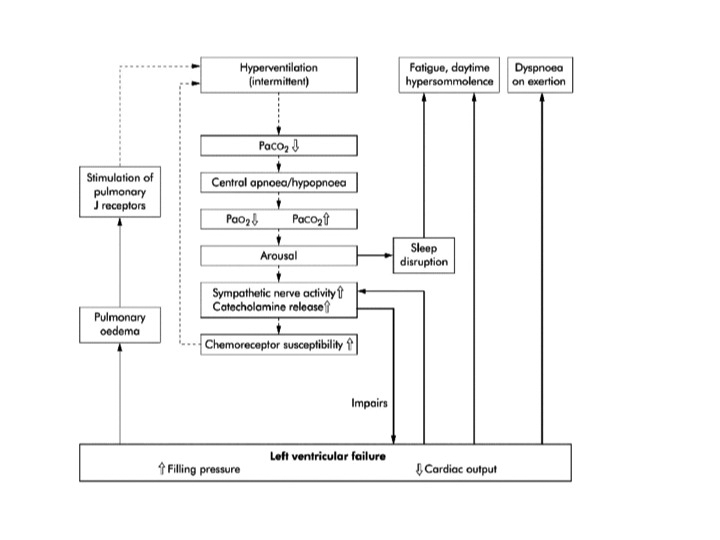
Outline of effect of CSAS in heart failure.
Figure 2.
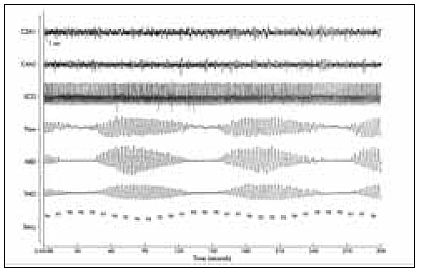
Five minute section of a polysomnographic record of EEG (c3a1, c4a2), electrocardiogram (ECG), oronasal airflow (flow), abdominal ventilatory effort (ABD), thoracic ventilatory effort (THO), and oxygen saturation measured at the finger tip of the left hand (SaO2). Typical breathing pattern with Cheyne-Stokes respiration with hyperpnoeic and apnoeic sequences in sleep stage 2.
Effects of CSAS
The episodes of apnoea and hypopnoea, followed by hyperpnoea, are associated with episodes of hypoxaemia-reoxygenation, arousals and relatively large negative deflections in intrathoracic pressure.2,3 As a consequence, an imbalance in myocardial oxygen delivery/consumption ratio might occur, activating the sympathetic and other neurohormonal systems leading to an increased right and left ventricular afterload.3 Because of the arousals during the night, there are sleep disruptions, which may cause fatigue and somnolence during daytime.
Treatment options
At first the pharmacological treatment of congestive heart failure should be optimised. When this has been established, there are some additional treatment options, as discussed below.
Oxygen
In heart failure an increased chemoresponsiveness to hypercapnia and hypoxaemia exists, in combination with an increased apnoeic threshold. Oxygen delivery reduces the periods of hypoxaemia and tends to decrease the hyperresponsiveness to carbon dioxide. Oxygen therapy during the night seems to stabilise breathing during sleep.6 It was shown by Staniforth that oxygen therapy during the night decreases both AHI and noradrenaline concentration.6
Acetazolamide
Due to the metabolic acidosis induced by acetazolamide, ventilation is increased leading to a further lowering of the PaCO2. However, as the apnoeic threshold is decreased even more, the difference between the prevailing carbon dioxide tension and the apnoeic threshold of carbon dioxide tension increases. As a result the likelihood of developing sleep apnoea decreases.7 It was shown in a recent study that acetazolamide given before sleep decreased the number of central apnoeas from 44 to 22 per hour.7
Continuous positive airway pressure
Continuous positive airway pressure (CPAP) works mainly on the left ventricle by reducing the afterload and so improving cardiac output. By doing so there is less pulmonary oedema and for the patient less reason for hyperventilation. The largest study in this respect is the CANPAP study, which investigated the effect of CPAP on cardiac function and survival in a randomised controlled trial. While they showed a significant decreased AHI and improved LVEF there was no survival benefit.8 However, a post-hoc analysis showed that if the CPAP was titrated effectively (meaning full suppression of the apnoeas) a survival benefit by CPAP could be detected.4
Ventilatory support
Bilevel positive airway pressure (BiPAP) provides a minimum positive expiratory airway pressure to maintain upper airway patency to eliminate possible obstructive apnoeas and hypopnoeas. This is combined with inspiratory pressure support, to maintain a sufficient inspiratory airflow and thus eliminate central apnoeas and hypopnoeas. As with CPAP, BiPAP mainly works on the left ventricle by reducing afterload and so improving cardiac output. In Kohnlein’s study it was shown that CPAP was equally effective in reducing AHI and sleep quality.9
Adaptive servo ventilation (ASV) has recently been introduced. It is a hybrid form of respiratory support that can cycle between pressure support during hypopnoea and ventilator support during apnoea. In a recent study by Philippe it was shown that ASV was equally effective compared with CPAP with respect to reducing AHI.10 However the compliance to ASV was greater leading to a better long-term result in reducing AHI, with even an improved LVEF.
Discussion
Central sleep apnoea syndrome is seen in approximately 40% of patients with congestive heart failure. Treatment is aimed at controlling apnoeas and improving sleep quality, resulting in a significant improvement in daytime sleepiness. Treatment of central sleep apnoea was also associated with a decrease in plasma brain natriuretic peptides and urinary catecholamine excretion, both of which are markers of prognosis in chronic heart failure.10 Stabilised ventilation also improved left ventricular function.10 Therefore, a reduction in the apnoea-hypopnoea index (AHI) is a predictor of improved cardiovascular outcome.5
Because of its high prevalence, poor quality of life, poor outcome, and the beneficial effects of treatment, physicians treating patients with heart failure should be aware of central sleep apnoea. Once the patient starts complaining of restlessness during the night, sleepiness during the daytime, extreme fatigue, and typical breathing patterns, as described in these two cases, a referral to a pulmonologist is indicated. There are different treatment options, but the exact effects and indications for each option have not yet been fully determined. Further studies should be done to further investigate its prevalence, and to establish the most adequate therapy for the individual patient.
References
- 1.Dickstein K, Cohen-Solal A, Filippatos G, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008. Eur Heart J. 2008;29:2388-442. [DOI] [PubMed] [Google Scholar]
- 2.Meguro K, Adachi H, Oshima S, et al. Exercise tolerance, exercise hyperpnea and central chemosensitivity to carbon dioxide in sleep apnea syndrome in heart failure patients. Circ J. 2005;69:695-9. [DOI] [PubMed] [Google Scholar]
- 3.Javaheri S, Shukla R, Zeigler H, Wexler L. Central sleep apnea, right ventricular dysfunction, and low diastolic bloodpressure are predictors of mortality in systolic heart failure. J Am Coll Cardiol. 2007;49:2028-34. [DOI] [PubMed] [Google Scholar]
- 4.Arzt M, Floras JS, Logan AG, Kimoff RJ, et al. Suppression of central sleep apnea by continuous positive airway pressure and transplant-free survival in heart failure: a post hoc analysis of the Canadian Continuous Positive Airway Pressure for Patients With Central Sleep Apnea and Heart Failure trial (CANPAP). Circulation. 2007;115:3173-80. [DOI] [PubMed] [Google Scholar]
- 5.Arzt M, Wensel R, Montalvan S, et al. Effects of dynamic bilevel positive airway pressure support on central sleep apnea in men with heart failure. Chest. 2008;134:61-6. [DOI] [PubMed] [Google Scholar]
- 6.Staniforth AD, Kinnear WJM, Starling R, et al. Effect of oxygen on sleep quality, cognitive function and sympathetic activity in patients with chronic heart failure and Cheyne-Stokes respiration. Eur Heart J. 1998;19:922-8. [DOI] [PubMed] [Google Scholar]
- 7.Javaheri S. Acetazolamide improves central sleep apnea in heart failure; a double-blind, prospective study. Am J Resp Crit Care Med. 2006;173:234-7. [DOI] [PubMed] [Google Scholar]
- 8.Bradley TD, Logan AG, Kimoff RJ, et al. Continuous positive airway pressure for central sleep apnea and heart failure. N Engl J Med. 2005;353:2025-33. [DOI] [PubMed] [Google Scholar]
- 9.Köhnlein T, Welte T. Tan LB, Elliott MW. Assisted ventilation for heart failure patients with Cheyne-Stokes respiration. Eur Respir J. 2002;20:934-41. [DOI] [PubMed] [Google Scholar]
- 10.Pillippe C, Stoïca-Herman M, Drouot X, et al. Compliance with and effectiveness of adaptive servoventilation versus continuous positive airway pressure in the treatment of Cheyne-Stokes respiration in heart failure over a six month period. Heart. 2006;92:337-42. [DOI] [PMC free article] [PubMed] [Google Scholar]


