Abstract
Objective
To assess the hazards at an early phase of the growing epidemic of deaths from tobacco in China.
Design
Smoking habits before 1980 (obtained from family or other informants) of 0.7 million adults who had died of neoplastic, respiratory, or vascular causes were compared with those of a reference group of 0.2 million who had died of other causes.
Setting
24 urban and 74 rural areas of China.
Subjects
One million people who had died during 1986-8 and whose families could be interviewed.
Main outcome measures
Tobacco attributable mortality in middle or old age from neoplastic, respiratory, or vascular disease.
Results
Among male smokers aged 35-69 there was a 51% (SE 2) excess of neoplastic deaths, a 31% (2) excess of respiratory deaths, and a 15% (2) excess of vascular deaths. All three excesses were significant (P<0.0001). Among male smokers aged ⩾70 there was a 39% (3) excess of neoplastic deaths, a 54% (2) excess of respiratory deaths, and a 6% (2) excess of vascular deaths. Fewer women smoked, but those who did had tobacco attributable risks of lung cancer and respiratory disease about the same as men. For both sexes, the lung cancer rates at ages 35-69 were about three times as great in smokers as in non-smokers, but because the rates among non-smokers in different parts of China varied widely the absolute excesses of lung cancer in smokers also varied. Of all deaths attributed to tobacco, 45% were due to chronic obstructive pulmonary disease and 15% to lung cancer; oesophageal cancer, stomach cancer, liver cancer, tuberculosis, stroke, and ischaemic heart disease each caused 5-8%. Tobacco caused about 0.6 million Chinese deaths in 1990 (0.5 million men). This will rise to 0.8 million in 2000 (0.4 million at ages 35-69) or to more if the tobacco attributed fractions increase.
Conclusions
At current age specific death rates in smokers and non-smokers one in four smokers would be killed by tobacco, but as the epidemic grows this proportion will roughly double. If current smoking uptake rates persist in China (where about two thirds of men but few women become smokers) tobacco will kill about 100 million of the 0.3 billion males now aged 0-29, with half these deaths in middle age and half in old age.
Key messages
Of the Chinese deaths now being caused by tobacco, 45% are from chronic lung disease, 15% from lung cancer, and 5-8% from each of oesophageal cancer, stomach cancer, liver cancer, stroke, ischaemic heart disease, and tuberculosis
Tobacco now causes 13% (and will probably eventually cause about 33%) of deaths in men but only 3% (and perhaps eventually about 1%) of deaths in women as the proportion of young women who smoke has become small
Two thirds of men now become smokers before age 25; few give up, and about half of those who persist will be killed by tobacco in middle or old age
If present smoking patterns continue about 100 million of the 0.3 billion Chinese males now aged 0-29 will eventually be killed by tobacco
Tobacco caused 0.6 million deaths in 1990 and will cause at least 0.8 million in 2000 (0.7 million in men) and about 3 million a year by the middle of the century on the basis of current smoking patterns
Introduction
In developed countries male cigarette smoking increased greatly during the first half of the century, but there was a delay of several decades before the resulting increase in male deaths from tobacco was completed.1–8 In the United States, for example, mean daily cigarette consumption per adult rose over 40 years from one in 1910 to four in 1930 and 10 in 1950 (remaining around 10 until 1980), and the proportion of all US deaths in middle age (35-69) attributable to tobacco rose from 12% in the 1950s to 33% in the 1990s. The increase in deaths occurred several decades after the main increase in cigarette use by young adults because the smokers who are at substantial risk in middle age are those who have smoked since early adult life.
Cigarette smoking among Chinese men followed a similar pattern to that among adults in the United States, although the main increase took place 40 years later. Average daily cigarette consumption per man in China was one in 1952, four in 1972, and 10 in 1992; consumption seemed to have stabilised by 1996 at about 11.9–13 (Over 90% of the 1800 billion cigarettes sold, legally or not, in 1996 were smoked by the 0.4 billion men aged 20 or over.14) Since the rise in smoking by Chinese men is so recent it will be several decades before the full effects are seen. So far a similar rise in smoking has not occurred in Chinese women. In fact the female uptake rate of smoking has fallen, and it is not clear whether mortality attributed to tobacco will increase or decrease in the next few decades.
Serious concerns about smoking and health in China developed around 1980, leading to a large prospective study in Shanghai, retrospective studies of a few types of cancer in a few parts of China, and a large nationwide survey of smoking prevalence.12 The known hazards of tobacco in the United Kingdom and United States (where about half of all persistent smokers are killed by it8) led in the mid-1980s to the prediction that tobacco would eventually cause more than two million deaths a year in China,5–7,15–18 and since then Chinese cigarette consumption has increased. Although analogy with findings elsewhere suggests that the hazards in China will eventually be large, it cannot predict accurately how large or when or where in China they will be greatest. Even among non-smokers mortality from diseases that can be caused by tobacco differs widely between the United Kingdom, United States, and China and, within China, between one area and another,19–22 and the effects of tobacco smoking could be greatly modified by such differences. Retrospective studies are needed throughout China to assess the current effects of tobacco on the occurrence of specific diseases, and nationwide prospective studies are needed to monitor the long term evolution of the epidemic. This report describes a large retrospective study.
Subjects and methods
During 1989-91 we interviewed surviving family members (or sometimes, in rural areas, other informants) of the one million people who died during 1986-8 in 98 areas of China to determine whether the dead person had been a smoker before 1980. Most deaths before age 35 were in children, and few were from diseases that are much affected by active smoking. We therefore restricted the analyses to ages 35-69 and, separately, 70 and over. In other countries most of the excess mortality among smokers is from neoplastic, respiratory, or vascular disease, so the smoking habits of adults who had died of these causes were compared with the habits of those who had died of other causes (the reference group).
The strength of proportional mortality analyses is that any bias affecting assessment of the habits of those in the study group should similarly affect assessment of the habits in the reference group. Hence, differences between the proportions of smokers in the reference group and in people who had died of neoplastic, respiratory, or vascular causes can be used to calculate the risk ratios (smoker versus non-smoker) for mortality from those three groups of causes. For example, the excess of lung cancer deaths among smokers can be inferred from the excess of smokers among those who died of lung cancer. These risk ratios, together with the prevalence of smoking in the reference group, can be used to estimate the percentage of all deaths from each particular cause that would have been avoided if the smokers had had no excess mortality from those diseases. As, however, smoking must have caused a few of the deaths in the reference group (for example, some of those from gastric ulcer) our proportional mortality analyses may have slightly underestimated the overall hazards of tobacco.
Study areas
Figure 1 shows the 98 areas studied. The 24 cities (Beijing, Tianjin, Shanghai, and 21 others) were chosen non-randomly to include a wide geographical spread, and the 74 rural counties were chosen by stratified random sampling20 from the 2000 counties whose cancer rates in 1973-5 were recorded in the Chinese cancer atlas.21,22 Many of the cities are large (although for some analyses of female mortality six smaller ones are grouped together), but the counties have smaller populations and were therefore collected into two groups: 34 in coastal provinces (from Liaoning down to Guangdong, including the rural areas near Beijing, Tianjin, and Shanghai) and 40 in inland provinces, which tended to be less economically developed. For the few counties with particularly large populations administrative subareas were included randomly until the total population of the subareas was over 300 000. Although the 24 cities and 74 countries chosen are reasonably representative of urban and rural (including small town) China, the study includes more urban than rural deaths, whereas China is 70% rural. Hence, for “all China” we used a 30:70 mixture of the urban and rural findings.
Figure 1.
Location of study areas: 24 major cities (large circles with names) and 74 rural counties (open unnamed circles). The study areas for Fuzhou city include two small unmarked nearby cities, and those for Beijing exclude one district (out of eight in that city) where the study organisation failed. Provincial boundaries are shown
Underlying causes of death
Deaths were identified primarily from local administrative records, which generally included name, address, sex, age, and certified cause of death. This information was supplemented by review of medical records, which were usually available, or by discussions (a few years after the death) with local health workers, community leaders, and family, or by both. The findings were recorded as parts I and II of a standard death certificate.23 Such records include about 90% of all deaths after age 35, so when calculating adult death rates we made a 10% reduction in the local population estimates (which were available, by age and sex, from local government).
The fieldwork involved over 500 interviewers, who usually worked in teams of two in urban areas and four in rural areas; at least one team member was medically trained. Consistency was checked by repeat interviews of unpredictably selected households by team leaders. Underlying causes were coded by 100 clerks in five teams, each under a trained nosologist from the Ministry of Health with experience of coding standard death certificates using ICD-9 (international classification of diseases, ninth revision). Some batches of data sheets were coded by two teams and the differences discussed to develop consistent coding conventions. At ages 35-69 only 0.4% of causes were ill defined (codes 780-99), but at older ages 4% were ill defined (3% urban, 6% rural). Double data entry was followed by extensive computerised checks and queries to correct gaps, duplications, inconsistencies, and implausibilities.
Smoking habits
Information was sought on the smoking habits of each person who had died. For rural deaths in middle age, four out of five informants were the surviving spouse or another family member. In urban areas informants who were not related to the dead person were often unable to report (or tended to under-report) tobacco use, so the urban analyses use information only from family members. In rural areas, however, both family and other local informants knew about (and reported similar prevalences of) tobacco use by those who had died, and both sources are used. When the interviewee was the surviving spouse (0.3 million cases), their smoking habits at the time of the interview and before 1980 were also recorded. The smoking histories included the amount smoked, age at starting smoking, and age at stopping. This was used to determine whether people had been smokers in 1980, as the terminal illness in 1986-8 is unlikely to have affected smoking behaviour in 1980 (except for diseases preceded by decades of serious symptoms, such as chronic respiratory problems or rheumatic heart disease). Moreover, the large nationwide increase in Chinese cigarette consumption during the 1980s is too recent to have had much effect on deaths in 1986-8 so it is appropriate to relate such deaths to smoking patterns before 1980.
Validity of information on smoking
There are few former smokers in China (except those who stopped because they were ill),12–14,20 and family members were generally confident about whether the dead person had smoked, although they were sometimes uncertain of the age when smoking began. Such uncertainties should, however, affect similarly those who died of different causes. For 453 deaths in Shanghai for which the surviving spouse was the informant both husband and wife had reported their smoking habits in the early 1980s in another study.24 For these 453 households there was no evidence of bias due to differences in the source (proxy or self) of the information on tobacco in the present study.
Validation of reference group
Among people who died from causes other than neoplastic, vascular, or respiratory disease no single cause predominated. The causes of their 87 000 deaths at ages 35-69 were infective or parasitic (9%), diabetes (6%), parkinsonism (0.2%), other nervous or mental disease (8%), renal disease (8%), hepatic disease (chiefly due to chronic hepatitis B infection) (19%), peptic ulcer (4%), other digestive disorders (6%), other medical disorders (6%), road traffic accidents (7%), suicide or homicide (15%), and other non-medical reasons (12%, including 2% ill defined). The main analyses assume that this reference group had had smoking habits similar to those of the general population. Some check on this is provided by married informants who described their own smoking habits as well as those of their dead partner. Smoking rates before 1980 in the 70 000 men and 150 000 women aged 35-69 when their spouse died (standardised to the age and urban/rural proportions of the reference group) were 61.5% and 12.4% compared with 62.1% and 12.5% in the reference group itself. This indicates that the proportional mortality analyses will not exaggerate the hazards of tobacco.
Statistical methods
Risk ratios and standard errors
—Risk ratio calculations were stratified by five year groups of age at death and by study area, with each county or city district a separate stratum. (Small cities have one district, but large ones could have about 10.) For a particular stratified analysis comparing those who smoked in 1980 with those who did not, let z denote the ratio of the Mantel-Haenszel25 “observed minus expected” number of deaths among smokers to its standard error (s) and let R denote the maximum likelihood estimate of the risk ratio, calculated by stratified logistic regression.26 The standard error of R is then estimated as (R−1)/z. Finally (since R is roughly equal to e(z/s), the “one step” risk ratio estimate27), 99% confidence limits for R are estimated by multiplying or dividing it by e(2.575/s), and when R is plotted as a black square the height of that square is proportional to s.27
Age standardisation
—The age standardised death rate at ages 35-69 is defined as the mean of the seven five yearly rates in this age range. From it can be calculated the probability that someone aged just 35 will die before age 70.5,6 (If the standardised rate per 1000 for all causes is D and that for a particular cause is d, then this probability is 1−e(−35D/1000), and the cause specific probability of death at these ages is d/D times this.)
Calculation of a 30:70 mixture of urban and rural results to get results for all China
—Let M denote the age standardised mortality rate, P the proportion of smokers among those who died of the disease of interest, and R the risk ratio (smoker versus non-smoker), and note that the proportion of all deaths attributed to tobacco is (P−P/R). Define w, the urban weight, to be 30×urbanM/(30×urbanM+70×ruralM), and define ChinaP as w×urbanP+(1−w)×ruralP. Finally, define ChinaR from calculation of ChinaP/ChinaR =w×urbanP/urbanR+(1−w)×ruralP/ruralR.
Relative and absolute risks
—The death rates at ages 35-69 for non-smokers and smokers in a particular population are calculated from the mortality for the whole of that population, the smoker:non-smoker risk ratio, and the prevalence of smoking in the reference group, giving M/(1+(R−1)×prevalence) for non-smokers and R times this for smokers.
All cause mortality
—Absolute risks for smokers (and for non-smokers) were obtained by adding the four separate risks from neoplastic, respiratory, vascular, and other causes. The proportional increase in all cause mortality was obtained by multiplying the proportional increase in neoplastic, respiratory, or vascular mortality (that is, relative risk−1) by the fraction of non-smoker deaths that these three accounted for.
Results
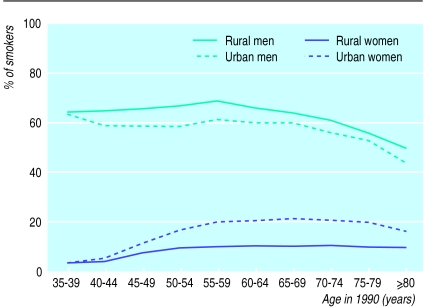
Prevalence of smoking in 1990
Among surviving spouses interviewed in about 1990 the prevalence of smoking in men was high, and higher in rural than urban areas, but in women it was low, and lower in rural than urban areas (fig 2). These prevalences are consistent with those in the 1984 and 1996 nationwide surveys of smoking prevalence.12–14 At ages 35-69 the prevalence of smoking remained fairly constant among men, but among women it was much lower at 35-39 than at 50-69. Over the past few decades young women, particularly in cities, have become much less likely to start smoking. The proportion who started to smoke before age 25 was 10% for all urban women born before 1940, but only 1% for those born in 1950-64. For rural women the prevalences were 4% for those born before 1940 and 2% for those born in 1950-64. These unexpected decreases are statistically reliable. For women born before 1920, 1920-9, 1930-9, 1940-9, 1950-9, and 1960-4 the respective proportions who began smoking before age 25 were 9.8%, 10.1%, 8.8%, 3.3%, 1.3% (91/6866), and 0.6% (6/988) for urban women and 3.9%, 4.3%, 3.9%, 2.9%, 2.2% (93/4291), and 2.5% (17/674) for rural women.
Figure 2.
Smoking prevalence in 1990 among interviewees whose spouse had died in 1986-8
Attributable risk
In general the excesses of neoplastic, respiratory, and vascular deaths among smokers exist because smoking can actually cause those diseases. Hence, the risk ratio (comparing smokers with non-smokers) for such diseases and the proportion of smokers among those dying from these diseases imply the proportion of all such deaths attributed to tobacco.
The main analyses are of deaths at ages 35-69 because medical information about the underlying cause of death for this group is likely to be more reliable than at older ages, and deaths at ages 35-69 produce a greater loss of life expectancy than deaths at older ages. The overall proportion of deaths attributed to tobacco, however, was similar for ages 35-69 and 70 and over.
Lung cancer
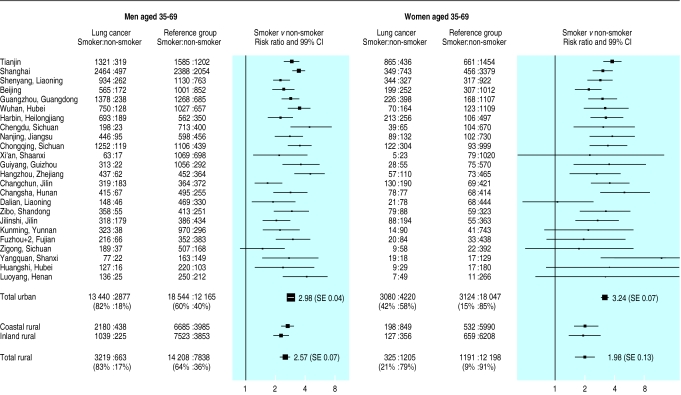
Risk ratios for men
Figure 3 shows the numbers of smokers and non-smokers among men aged 35-69 who died of lung cancer and those in the reference group (men who died from causes other than neoplastic, respiratory, or vascular disease). In the 24 cities 16 317 men died from lung cancer, 82% (13 440) of whom were reported to have smoked before 1980. In the reference group 30 709 men died, 60% (18 544) of whom were reported to have smoked. This suggests that lung cancer is about three times as common among urban smokers as among otherwise similar non-smokers (as crude division of 82/18 by 60/40 gives a risk ratio of 3), and with standardisation for age and city district this becomes 2.98 (SE 0.04, 99% confidence interval 2.9 to 3.1). This calculation does not, however, allow for any biases, the net effect of which would probably have been to decrease the risk ratio. Hence, the true value of the urban smoker:non-smoker lung cancer risk ratio may slightly exceed 3.
Figure 3.
Numbers of deaths of smokers and non-smokers aged 35-69 from lung cancer and all causes other than neoplastic, respiratory, or vascular disease (reference group) together with relative risks and 99% confidence intervals. Results presented for men and women by study region. Height of each square is inversely proportional to length of confidence interval
The findings were similar for rural men (fig 3). Among the 3882 who died of lung cancer, 83% (3219) were reported to have smoked compared with 64% (14 208) of the 22 046 who died in the reference group. After age and county were standardised for, the risk ratio for lung cancer in rural men was 2.57 (0.07, 2.4 to 2.8). Again, however, the true risk ratio probably exceeds this.
The number of lung cancer deaths in men aged 35-69 ranged from only 80 in the large city of Xi’an up to 2961 in Shanghai (fig 3). In general there is a remarkable consistency between the lung cancer risk ratios in different cities: all (and those of the two rural areas) are statistically compatible with the range 2.0 to 4.0.
Risk ratios for women
The age adjusted lung cancer risk ratios for women (right side of fig 3) are similar to those for men. In the 24 cities 7300 women died from lung cancer, 42% (3080) of whom smoked; in the reference group 21 171 women died, 15% (3124) of whom smoked. After the bias caused by the strong correlation of smoking with age among women was allowed for the risk ratio was 3.24 (0.07, 3.1 to 3.5). Thus, for urban women (as for urban men) lung cancer was at least three times as common in smokers as in non-smokers. Among rural women, 21% (325) of the lung cancer deaths and 9% (1191) of the reference group deaths were in smokers. After age was adjusted for the risk ratio was 1.98 (0.13, 1.7 to 2.3). This twofold risk ratio for rural women was seen in both coastal and inland provinces.
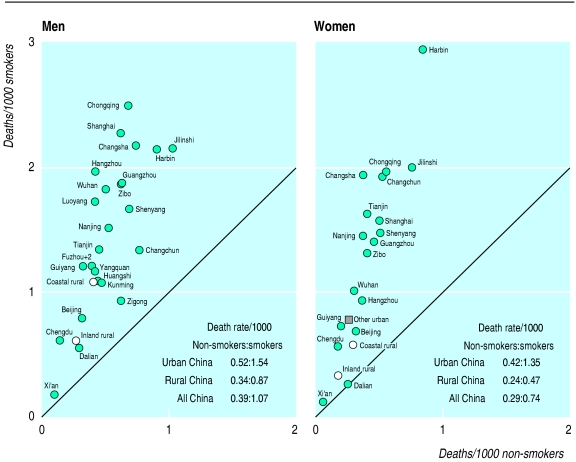
Absolute rates in smokers and non-smokers
The age standardised (35-69) death rate from lung cancer for the whole population of each geographical area is known. This local lung cancer rate, combined with the local prevalence of smoking (in the reference group) and the smoker:non-smoker risk ratio can be used to calculate the local lung cancer rates for smokers and non-smokers. These are plotted against each other in figure 4. Even among non-smokers the lung cancer rates differ enormously between cities. For both sexes, for example, the rate in non-smokers at ages 35-69 in Xi’an was only 0.1 per 1000 (about the same as in American non-smokers5,6), whereas in Harbin it was nearly 1 per 1000. Thus, although the risk ratio was about the same in both cities, the absolute excess of lung cancer produced by smoking was much greater in Harbin than in Xi’an. This was true for both men and women. The very high lung cancer death rate of 3 per 1000 female smokers in Harbin, which is based on large enough numbers to be statistically reliable, is three times the similarly age standardised rate of 1.1 per 1000 female smokers in a large US prospective study during the 1980s,5,6 and greatly exceeds the US national lung cancer death rates at these ages (0.6 per 1000 women, 1.4 per 1000 men) in 1990.
Figure 4.
Death rates at ages 35-69 from lung cancer in smokers versus non-smokers, 1986-8. For women (right) the rates for six of the smaller cities have been averaged (dark square)
Although the rates of lung cancer in non-smokers varied tenfold between cities, the lung cancer mortality in smokers was consistently about three times that in non-smokers, producing the striking pattern in fig 4. Since most of these cities are large the general pattern of absolute risks is reliable. Apart from the consistently high rates in the cold northeast (Harbin, Jilinshi, Changchun, Shenyang), where there is lifelong heavy indoor exposure to domestic coal smoke and cooking fumes, the geographical pattern was irregular, with cities that are not far apart often having disparate disease rates. For example, although the large cities of Chongqing and Chengdu were in the same southwestern province, the rates of lung cancer in them differed fourfold.
Taking all cities together, the lung cancer mortality was 0.5 per 1000 non-smokers (0.52 men, 0.42 women) and 1.5 per 1000 smokers (1.54 men, 1.35 women, representing 12% of all deaths of urban smokers at these ages). For rural China, however, the absolute lung cancer rates were only about half as great, partly, we suspect, because some rural deaths from lung cancer in later middle age were not recognised as such.
Relative risks for specific diseases among men
Table 1 gives risk ratios for men aged 35-69 in urban China, rural China, and, by a weighted combination of these, all China. About 70% of all deaths from cancer in China were from just four diseases: cancer of the lung, oesophagus, stomach, or liver. Each was significantly more common among smokers. For lung cancer the all China risk ratio was 2.72 (SE 0.05) for men aged 35-69, indicating that at non-smoker death rates about half (52.3%) of all deaths from lung cancer in middle aged men would have been avoided. The other risk ratios were 1.61 (SE 0.04) for oesophageal cancer, 1.35 (0.03) for stomach cancer, 1.40 (0.03) for liver cancer, and 1.51 (0.05) for an aggregate of five “minor” cancer sites that studies in other countries have associated with smoking (mouth, pharynx, larynx, pancreas, and bladder, each of which was significantly related to smoking in this study). Finally, the aggregate of all other neoplastic diseases was also somewhat related to smoking (risk ratio 1.24 (0.03)). Hence, taking all neoplastic diseases together, the overall risk ratio was 1.51 (0.02) and the attributable fraction 24.4% (and 18.7% at older ages). Thus, about a quarter of all deaths from cancer in middle aged men would have been avoided at non-smoker death rates.
Table 1.
Numbers of deaths and smoker to non-smoker mortality ratios (standard errors) for urban, rural, and all China at ages 35-69 with summary calculations for ages ⩾70
| Cause of death (ICD-9 code) | Urban
|
Rural
|
All China
|
All China age⩾70
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No of smokers/total | Risk ratio (SE) | No of smokers/total | Risk ratio (SE) | Weighted mean risk ratio (SE) | % of deaths attributed to smoking | Weighted mean risk ratio (SE) | % of deaths attributed to smoking | ||||
| Men | |||||||||||
| (A) Neoplastic (140-208): | 43 205/60 286 | 1.62 (0.02) | 23 998/33 109 | 1.48 (0.03) | 1.51 (0.02) | 24.4 | 1.39 (0.03) | 18.7 | |||
| Lung cancer (162) | 13 440/16 317 | 2.98 (0.05) | 3 219/3 882 | 2.57 (0.08) | 2.72 (0.05) | 52.3 | 2.47 (0.07) | 46.6 | |||
| Oesophageal cancer (150) | 3 964/5 188 | 2.06 (0.05) | 4 951/6 799 | 1.57 (0.05) | 1.61 (0.04) | 27.9 | — | — | |||
| Stomach cancer (151) | 7 145/10 725 | 1.36 (0.03) | 6 637/9 470 | 1.35 (0.04) | 1.35 (0.03) | 18.1 | — | — | |||
| Liver cancer (155) | 9 058/13 478 | 1.39 (0.03) | 5 646/7 979 | 1.41 (0.04) | 1.40 (0.03) | 20.2 | — | — | |||
| Five minor sites* | 3 302/4 656 | 1.58 (0.05) | 1 149/1 560 | 1.48 (0.08) | 1.51 (0.05) | 24.6 | — | — | |||
| Other neoplastic | 6 296/9 922 | 1.16 (0.03) | 2 396/3 419 | 1.28 (0.05) | 1.24 (0.03) | 13.1 | — | — | |||
| (B) Respiratory: | 17 759/24 336 | 1.48 (0.03) | 14 990/20 568 | 1.28 (0.03) | 1.31 (0.02) | 17.2 | 1.54 (0.02) | 24.6 | |||
| Chronic obstructive pulmonary disease, etc† | 13 637/18 383 | 1.57 (0.03) | 10 780/14 439 | 1.41 (0.03) | 1.43 (0.03) | 22.6 | 1.63 (0.03) | 27.4 | |||
| Respiratory tuberculosis (011, 012, 018) | 2 371/3 374 | 1.42 (0.05) | 3 132/4 542 | 1.17 (0.04) | 1.20 (0.04) | 11.3 | — | — | |||
| Other respiratory (rest of 460-519) | 1 751/2 579 | 1.23 (0.05) | 1 078/1 587 | 1.03 (0.06) | 1.07 (0.05) | 4.2 | — | — | |||
| (C) Vascular (390-415, 418-459): | 33 011/51 494 | 1.17 (0.02) | 12 784/18 987 | 1.14 (0.02) | 1.15 (0.02) | 8.5 | 1.06 (0.02) | 3.4 | |||
| Stroke (430-9) | 21 717/33 722 | 1.18 (0.02) | 8 584/12 584 | 1.17 (0.03) | 1.17 (0.02) | 10.0 | — | — | |||
| Ischaemic heart disease (410-4) | 7 480/11 502 | 1.28 (0.03) | 2 271/3 320 | 1.28 (0.05) | 1.28 (0.03) | 14.7 | — | — | |||
| Rheumatic heart disease, etc‡ | 3 814/6 270 | 1.00 (0.03) | 1 929/3 083 | 0.92 (0.04) | 0.94 (0.03) | — | — | — | |||
| (A-C) Subtotal | 93 975/136 116 | 1.39 (0.02) | 51 772/72 664 | 1.31 (0.02) | 1.33 (0.02) | 17.4 | 1.29 (0.02) | 14.8 | |||
| (D) Other causes (reference group) | 18 544/30 709 | 1.00 — | 14 208/22 046 | 1.00 — | 1.00 — | — | — | — | |||
| (A-D) All deaths | 112 519/166 825 | 1.29 (0.02) | 65 980/94 710 | 1.22 (0.02) | 1.23 (0.01) | 13.0 | 1.22 (0.02) | 11.7 | |||
| Women | |||||||||||
| (A) Neoplastic: | 8 162/33 344 | 1.67 (0.03) | 1 959/17 225 | 1.21 (0.05) | 1.37 (0.04) | 4.0 | 1.37 (0.03) | 4.7 | |||
| Lung cancer | 3 080/7 300 | 3.24 (0.06) | 325/1 530 | 1.98 (0.12) | 2.64 (0.08) | 19.4 | 2.50 (0.09) | 20.1 | |||
| Oesophageal cancer | 488/2 126 | 1.65 (0.08) | 363/3 641 | 1.28 (0.09) | 1.34 (0.08) | 2.8 | — | — | |||
| Stomach cancer | 918/4 860 | 1.30 (0.05) | 432/4 149 | 1.13 (0.07) | 1.17 (0.06) | 1.7 | — | — | |||
| Liver cancer | 863/4 045 | 1.49 (0.06) | 297/2 685 | 1.12 (0.08) | 1.22 (0.06) | 2.4 | — | — | |||
| Five minor sites* | 571/2 250 | 1.68 (0.07) | 99/686 | 1.39 (0.15) | 1.53 (0.09) | 6.4 | — | — | |||
| Other neoplastic | 2 242/12 763 | 1.17 (0.03) | 443/4 534 | 0.95 (0.06) | 1.04 (0.04) | 0.5 | — | — | |||
| (B) Respiratory: | 5 464/16 590 | 2.28 (0.04) | 2 359/14 053 | 1.43 (0.05) | 1.61 (0.05) | 7.5 | 1.59 (0.03) | 7.4 | |||
| Chronic obstructive pulmonary disease, etc† | 4 772/13 460 | 2.51 (0.05) | 1 954/10 373 | 1.50 (0.06) | 1.72 (0.05) | 9.3 | 1.70 (0.03) | 8.6 | |||
| Respiratory tuberculosis | 361/1 598 | 1.56 (0.09) | 301/2 652 | 1.25 (0.09) | 1.29 (0.08) | 2.8 | — | — | |||
| Other respiratory | 331/1 532 | 1.37 (0.08) | 104/1 028 | 1.03 (0.12) | 1.14 (0.09) | 1.5 | — | — | |||
| (C) Vascular: | 7 780/37 686 | 1.14 (0.03) | 1 615/14 859 | 0.92 (0.04) | 1.01 (0.03) | 0.2 | 1.02 (0.02) | 0.2 | |||
| Stroke | 4 707/23 266 | 1.11 (0.03) | 1 005/9 175 | 0.88 (0.05) | 0.97 (0.03) | — | — | — | |||
| Ischaemic heart disease | 1 792/7 024 | 1.37 (0.04) | 274/2 054 | 1.22 (0.09) | 1.30 (0.05) | 4.1 | — | — | |||
| Rheumatic heart disease, etc‡ | 1 281/7 396 | 1.04 (0.04) | 336/3 630 | 0.88 (0.07) | 0.94 (0.05) | — | — | — | |||
| (A-C) Subtotal | 21 406/87 620 | 1.50 (0.03) | 5 933/46 137 | 1.19 (0.04) | 1.29 (0.03) | 3.6 | 1.29 (0.02) | 3.8 | |||
| (D) Other causes (reference group) | 3 124/21 171 | 1.00 — | 1 191/13 389 | 1.00 — | 1.00 — | — | — | — | |||
| (A-D) All deaths | 24 530/108 791 | 1.40 (0.03) | 7 124/59 526 | 1.14 (0.04) | 1.23 (0.03) | 2.7 | 1.22 (0.02) | 2.8 | |||
Cancer of mouth, pharynx, larynx, pancreas, or bladder (ICD-9 codes 140-9, 161, 157, or 188).
Chronic obstructive pulmonary disease includes ICD-9 codes 490-2, 496, and 416-7 (pulmonary heart disease).
All vascular except ICD-9 codes 430-9, 410-4, and 416-7.
Chronic obstructive pulmonary disease (risk ratio 1.43 (0.03)) and respiratory tuberculosis (risk ratio 1.20 (0.04)) were also significantly related to smoking. For overall respiratory mortality (mainly from chronic obstructive pulmonary disease and tuberculosis) the risk ratio was 1.48 (0.03) in urban and 1.28 (0.03) in rural China. For all China the proportion of respiratory deaths attributable to smoking was 17.2% at ages 35-69 (and 24.6% at older ages). Respiratory diseases remain a common cause of death in men, particularly in rural China, so although smoking accounts for only about a sixth of such deaths in middle age and a quarter in old age, the absolute hazard is substantial.
Vascular mortality in China mainly involves stroke, which is slightly more common among smokers (risk ratio 1.17 (0.02)), or ischaemic heart disease (risk ratio 1.28 (0.03)). Rheumatic heart disease is also important, particularly in rural areas, and those dying from it were less likely to have smoked. But rheumatic heart disease severe enough to cause death in middle age may be associated with chronic symptoms starting in childhood that might discourage smoking, so the risk ratios among men aged 35-69 (0.77 (0.04) urban, 0.79 (0.05) rural) may reflect such discouragement rather than protection. (Rheumatic heart disease is, however, retained in the analyses of all vascular deaths in table 1, slightly weakening the apparent effects of tobacco.)
Daily number of cigarettes
Table 2 relates the daily cigarette consumption when men last smoked to the risk ratios for death at ages 35-69. It is restricted to male smokers whose most recent habits involved only cigarettes (75% of the urban and 46% of the rural male smokers in table 1) as other tobacco use is less easily quantified. Most were reported to have smoked exactly 10, 20, or 30 a day. In both urban and rural areas the strongest dose-response relations were for lung cancer (risk ratios for about 10, 20, or 30 cigarettes per day: urban 2.08, 3.59, and 6.92; rural 2.23, 3.65, and 7.26; both trends P<0.0001). In places where mortality from lung cancer was substantial even among non-smokers these sevenfold risk ratios would imply large absolute hazards among smokers.
Table 2.
Dose-response relations among men aged 35-69. Values are risk ratios (standard errors) comparing non-smokers with smokers whose most recent habits involved only cigarettes
| Urban: No of cigarettes/day
|
Rural: No of cigarettes/day
|
||||||
|---|---|---|---|---|---|---|---|
| 1-19 | 20 | >20 | 1-19 | 20 | >20 | ||
| Mean No of cigarettes/day | 9.4 | 20.0 | 32.8 | 10.3 | 20.0 | 30.4 | |
| (A) Neoplastic: | 1.44 (0.02) | 1.78 (0.03) | 2.53 (0.06) | 1.44 (0.04) | 1.68 (0.04) | 2.31 (0.10) | |
| Lung cancer | 2.08 (0.05) | 3.59 (0.06) | 6.92 (0.14) | 2.23 (0.10) | 3.65 (0.14) | 7.26 (0.32) | |
| Oesophageal cancer | 1.76 (0.06) | 2.09 (0.07) | 2.82 (0.14) | 1.43 (0.06) | 1.71 (0.08) | 2.13 (0.17) | |
| Stomach cancer | 1.31 (0.04) | 1.38 (0.04) | 1.51 (0.08) | 1.33 (0.05) | 1.56 (0.06) | 1.68 (0.13) | |
| Liver cancer | 1.36 (0.03) | 1.47 (0.04) | 1.55 (0.07) | 1.46 (0.05) | 1.58 (0.06) | 1.84 (0.12) | |
| Five minor sites | 1.43 (0.05) | 1.79 (0.06) | 2.14 (0.12) | 1.42 (0.10) | 1.47 (0.11) | 2.14 (0.25) | |
| Other neoplastic | 1.16 (0.03) | 1.21 (0.04) | 1.51 (0.08) | 1.26 (0.07) | 1.35 (0.08) | 1.62 (0.16) | |
| (B) Respiratory: | 1.28 (0.03) | 1.60 (0.04) | 2.14 (0.07) | 1.11 (0.04) | 1.28 (0.05) | 1.81 (0.11) | |
| Chronic obstructive, etc | 1.33 (0.03) | 1.73 (0.04) | 2.34 (0.09) | 1.22 (0.05) | 1.45 (0.06) | 2.10 (0.13) | |
| Respiratory tuberculosis | 1.24 (0.06) | 1.48 (0.07) | 2.03 (0.14) | 1.01 (0.06) | 1.23 (0.07) | 1.57 (0.15) | |
| Other respiratory | 1.14 (0.06) | 1.29 (0.07) | 1.42 (0.13) | 0.94 (0.09) | 1.00 (0.10) | 1.18 (0.22) | |
| (C) Vascular: | 1.17 (0.02) | 1.18 (0.02) | 1.28 (0.05) | 1.17 (0.04) | 1.24 (0.05) | 1.28 (0.10) | |
| Stroke | 1.15 (0.02) | 1.19 (0.03) | 1.28 (0.05) | 1.19 (0.04) | 1.31 (0.06) | 1.26 (0.11) | |
| Ischaemic heart disease | 1.30 (0.04) | 1.34 (0.04) | 1.53 (0.08) | 1.34 (0.07) | 1.52 (0.09) | 1.85 (0.20) | |
| Rheumatic heart disease, etc | 1.04 (0.04) | 0.94 (0.04) | 0.90 (0.08) | 0.97 (0.06) | 0.84 (0.07) | 0.82 (0.16) | |
| (A-C) Subtotal | 1.28 (0.02) | 1.48 (0.02) | 1.93 (0.05) | 1.26 (0.03) | 1.42 (0.04) | 1.87 (0.08) | |
| All deaths | 1.21 (0.02) | 1.36 (0.02) | 1.70 (0.05) | 1.18 (0.03) | 1.29 (0.03) | 1.60 (0.08) | |
| No of deaths* | 40 389 | 35 169 | 8303 | 15 969 | 12 332 | 2317 | |
Excludes 28 658 urban and 35 362 rural smokers who used some non-cigarette tobacco.
Several of the other neoplastic and respiratory diseases also show strong (and significant) dose relations. This illustrates the causal nature of the associations of smoking with not only lung cancer but also cancer of the oesophagus, cancer of five “minor” sites, chronic obstructive pulmonary disease, and respiratory tuberculosis—indeed, men in urban China smoking more than 20 cigarettes a day had double the death rate from tuberculosis of non-smokers. For stomach cancer, liver cancer, stroke, and ischaemic heart disease the dose relations were weaker (though still significant). For the aggregate of all other vascular diseases, however, they were non-significantly reversed, perhaps because rheumatic heart disease discourages heavy smoking. But taking all neoplastic, respiratory, and vascular diseases together in men aged 35-69 (subtotal A-C in table 2), the urban risk ratios of 1.28, 1.48, and 1.93 (with negligibly small standard errors) for about 10, 20, and 30 cigarettes per day show a strong trend, as do the corresponding rural risk ratios of 1.26, 1.42, and 1.87.
Age smoking began
Table 3 relates the age when men reportedly began smoking to mortality at ages 35-69. It includes all male smokers, irrespective of the type or amount of tobacco, except for the 0.6% for whom the age smoking began was not reported. The lung cancer risk ratios were greatest for those reportedly starting before age 20, intermediate for those starting at ages 20-24, and least for those starting later. The trends were highly significant both in urban areas (respective risk ratios 4.11, 2.94, and 2.45; trend P<0.0001) and in rural areas (risk ratios 3.07, 2.62, 2.26; trend P<0.0001). The trends must, however, have been weakened by misreporting of the age smoking began because this information relates to habits several decades earlier, perhaps before the informant knew the dead person. Moreover, the great fluctuations in Chinese social circumstances during the decades before 1980, with large changes in cigarette sales, mean that few middle aged cigarette smokers who died in 1986-8 will have had consistent tobacco consumption since early adult life. In urban China, however, table 3 shows that for those reportedly starting before age 20 (mean starting age 17) the excess of lung cancer associated with smoking was almost twice as great as for those starting later (age 20-24 or ⩾25: mean starting age 24). The tendency for those who start early to smoke more accounts for only a small part of this difference.
Table 3.
Age at starting smoking: effect on death rates in men aged 35-69. Values are risk ratios (standard errors) comparing non-smokers with smokers
| Urban: age began smoking
|
Rural: age began smoking
|
||||||
|---|---|---|---|---|---|---|---|
| <20 | 20-24 | ⩾25 | <20 | 20-24 | ⩾25 | ||
| Mean No of cigarettes/day | 16.4 | 14.8 | 13.1 | 11.2 | 11.8 | 10.7 | |
| Mean g leaf tobacco/day | 4.8 | 3.3 | 2.5 | 10.0 | 7.3 | 6.2 | |
| Mean age began | 17.0 | 20.8 | 29.3 | 17.3 | 20.9 | 29.3 | |
| (A) Neoplastic: | 1.90 (0.03) | 1.60 (0.02) | 1.53 (0.03) | 1.58 (0.04) | 1.52 (0.03) | 1.42 (0.03) | |
| Lung cancer | 4.11 (0.07) | 2.94 (0.05) | 2.45 (0.05) | 3.07 (0.11) | 2.62 (0.09) | 2.26 (0.09) | |
| Oesophageal cancer | 2.52 (0.09) | 2.05 (0.06) | 1.85 (0.07) | 1.75 (0.07) | 1.63 (0.06) | 1.44 (0.06) | |
| Stomach cancer | 1.48 (0.05) | 1.33 (0.04) | 1.32 (0.04) | 1.41 (0.06) | 1.39 (0.04) | 1.34 (0.05) | |
| Liver cancer | 1.44 (0.04) | 1.37 (0.03) | 1.38 (0.04) | 1.39 (0.06) | 1.44 (0.04) | 1.39 (0.05) | |
| Five minor sites | 1.79 (0.07) | 1.58 (0.05) | 1.50 (0.06) | 1.77 (0.12) | 1.46 (0.09) | 1.31 (0.10) | |
| Other neoplastic | 1.18 (0.04) | 1.15 (0.03) | 1.19 (0.04) | 1.32 (0.07) | 1.30 (0.06) | 1.26 (0.06) | |
| (B) Respiratory: | 1.91 (0.04) | 1.50 (0.03) | 1.29 (0.03) | 1.44 (0.04) | 1.28 (0.03) | 1.20 (0.04) | |
| Chronic obstructive, etc | 2.02 (0.05) | 1.60 (0.04) | 1.34 (0.04) | 1.62 (0.05) | 1.39 (0.04) | 1.31 (0.04) | |
| Respiratory tuberculosis | 1.86 (0.08) | 1.42 (0.06) | 1.22 (0.06) | 1.25 (0.06) | 1.18 (0.05) | 1.12 (0.06) | |
| Other respiratory | 1.40 (0.08) | 1.20 (0.06) | 1.19 (0.07) | 1.06 (0.09) | 1.08 (0.07) | 0.94 (0.08) | |
| (C) Vascular: | 1.19 (0.03) | 1.16 (0.02) | 1.18 (0.02) | 1.15 (0.04) | 1.14 (0.03) | 1.13 (0.03) | |
| Stroke | 1.20 (0.03) | 1.17 (0.02) | 1.18 (0.03) | 1.19 (0.04) | 1.17 (0.04) | 1.17 (0.04) | |
| Ischaemic heart disease | 1.32 (0.04) | 1.26 (0.03) | 1.30 (0.04) | 1.28 (0.07) | 1.31 (0.06) | 1.23 (0.07) | |
| Rheumatic heart disease, etc | 0.96 (0.05) | 1.00 (0.04) | 1.03 (0.04) | 0.92 (0.06) | 0.94 (0.05) | 0.90 (0.06) | |
| (A-C) Subtotal | 1.58 (0.03) | 1.38 (0.02) | 1.33 (0.02) | 1.40 (0.03) | 1.32 (0.02) | 1.26 (0.03) | |
| All deaths | 1.43 (0.03) | 1.28 (0.02) | 1.26 (0.02) | 1.27 (0.03) | 1.22 (0.02) | 1.19 (0.03) | |
| No of deaths* | 26 553 | 50 894 | 34 376 | 15 332 | 30 422 | 19 801 | |
Excludes 0.6% (696 urban, 425 rural) of smokers for whom age at starting smoking was not known.
Except perhaps for liver cancer, the excesses of the other neoplastic and respiratory diseases among smokers tended to be greatest for those who started before age 20: for all respiratory disease the respective risk ratios were 1.91, 1.50, and 1.29 in urban and 1.44, 1.28, and 1.20 in rural China; both of these trends were highly significant (P<0.0001). But for vascular disease there was no apparent relation with the age smoking began. Taking all neoplastic, respiratory, and vascular deaths together, however, men reported to have started smoking before age 20 still had significantly greater risks than those reported to have started later.
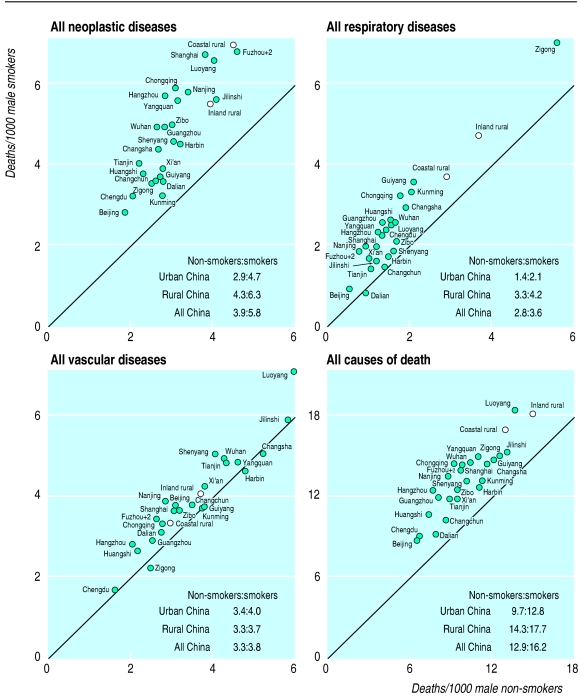
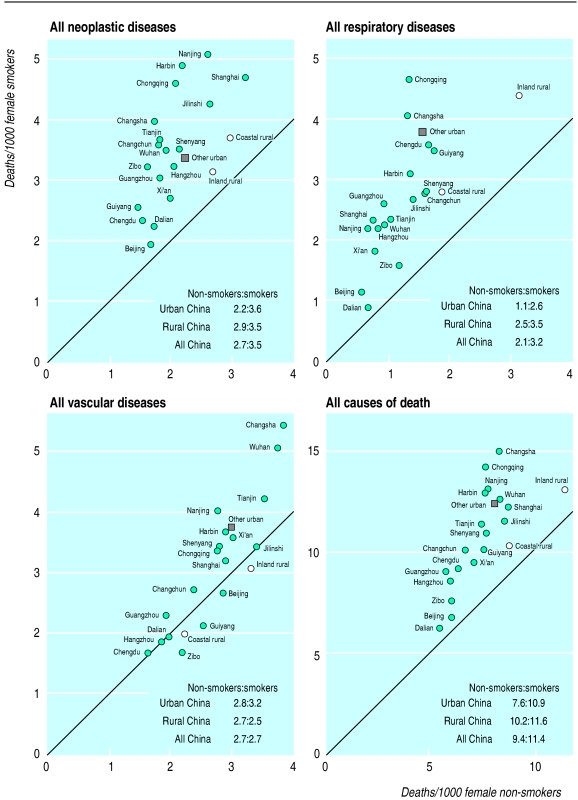
Absolute risks among men
Figure 5 shows the absolute risks in each area for neoplastic, respiratory, and vascular mortality and for all causes of death. For cancer as a whole the death rates among non-smokers varied twofold, but in most areas the overall cancer death rates among smokers were about 50% greater than those of non-smokers. Deaths from lung cancer account for about half of this excess cancer mortality among smokers.
Figure 5.
Death rates of male smokers and non-smokers aged 35-69 in 1986-8 from four main categories of cause
Throughout China, respiratory disease is a major cause of adult death, even among non-smokers. The rural rates tend to be higher than the urban rates, and the rural respiratory mortality of 3.3 per 1000 non-smokers and 4.2 per 1000 smokers (fig 5) implies a greater absolute tobacco hazard than the corresponding urban rates of 1.4 and 2.1. Values vary greatly among counties and cities, however, with particularly high respiratory death rates in the inland southwest.20,22 The small southwestern city of Zigong had extraordinarily high respiratory mortality among both non-smokers and smokers: at 1986-8 rates, one man in six would die before age 70 from chronic obstructive pulmonary disease (which includes respiratory heart disease) or some other respiratory condition. (As Zigong is relatively small, the overall urban rates would not have been much changed by its exclusion.) Respiratory death rates were comparably high in some of the rural counties within a few hundred kilometres of Zigong. Although vascular mortality in non-smokers varied widely between areas, the small absolute excess among smokers did not.
For non-smokers and smokers respectively the overall male mortality at ages 35-69 was 9.7 and 12.8 in urban China, 14.3 and 17.7 in rural China, and 12.9 and 16.2 in all China. At a constant death rate of 16.2 per 1000 smokers, 43.3% of those aged 35 would die before 70. If the fraction of these deaths attributed to smoking is 3.3/16.2 then at 1986-8 death rates 9% of male smokers would be killed by tobacco in middle age and at the death rates of the late 1990s the risk must already be at least 10%. But the death rates of smokers and of non-smokers are likely to diverge substantially in future so that for young men who now become persistent smokers the risk of being killed by tobacco in middle age will be much greater.
Results among women
Only 15% of the smokers who died at 35-69 were women. The results for women in some cities are therefore based on small numbers, and we combined the results for the six cities with fewer than 50 female smokers in the reference group as “other urban.” The risk ratios were similar for women and men (tables 1 and 4), but because fewer women smoked only 2.7% of the deaths of women aged 35-69 were attributed to smoking compared with 13.0% of those of men. The only substantial difference was that no significant association of stroke with smoking was seen in rural women, although the association with ischaemic heart disease remained. Likewise, the general pattern of absolute risks was similar among women (fig 6) and men (fig 5), except that in rural China there was no significant association of smoking with female vascular mortality. In urban areas the absolute hazards of tobacco were about as great for women as for men, but in rural areas they were only about half as big, chiefly because in rural areas women smoked less and started later (table 4).
Table 4.
Risk ratios of death from all causes for smokers compared with non-smokers among women aged 35-69 according to number of cigarettes smoked per day and age at starting smoking
| Urban
|
Rural
|
||||
|---|---|---|---|---|---|
| No of women | Risk ratio (SE) | No of women | Risk ratio (SE) | ||
| No of cigarettes/day | |||||
| 1-19 | 12 196 | 1.34 (0.03) | 2129 | 1.15 (0.07) | |
| 20 | 5 186 | 1.49 (0.05) | 535 | 1.19 (0.12) | |
| >20 | 851 | 1.69 (0.15) | 88 | 1.38 (0.35) | |
| Age at starting smoking | |||||
| <20 | 5 152 | 1.49 (0.06) | 1281 | 1.38 (0.10) | |
| 20-24 | 8 119 | 1.50 (0.04) | 2216 | 1.24 (0.07) | |
| ⩾25 | 11 040 | 1.32 (0.03) | 3548 | 1.04 (0.05) | |
Figure 6.
Death rates of female smokers and non-smokers aged 35-69 in 1986-8 from four main categories of cause
Deaths attributed to tobacco
We applied the percentages of various diseases attributed to smoking in table 1 to independent estimates28 of the numbers of deaths from these diseases at ages 30-69 and ⩾70 (table 5). This suggests that in 1990 there were about 0.6 million deaths from tobacco in China. (The difference between the age range 35-69 and 30-69 is unimportant, as the relevant diseases cause few deaths at ages 30-34.) The calculation can be done in several ways, but all give similar results. For example, it could have been calculated for the three broad catergories of neoplastic, respiratory, and vascular disease or, even more crudely, for the 13% of deaths in men and 3% in women in table 5. Alternatively, the cause specific death rates from the study could have been used (indicating fewer deaths from heart disase but more from cancer of the stomach or oesophagus). In each case, however, 0.6 million of the deaths in 1990 would be attributed to tobacco (0.5 million in men and 0.1 million in women and 0.3 million at ages 35-69 and 0.3 million at older ages). These deaths attributed to tobacco were due to respiratory disease in 0.3 million cases, neoplastic disease in 0.2 million, and vascular disease in 0.1 million. The estimate of 0.1 million vascular deaths due to tobacco is less reliable than that of deaths from neoplastic and respiratory diseases, but in other populations cigarettes have been shown to cause some vascular hazard. The main uncertainties lie not in the number of deaths at ages 35-69 but in the number of deaths at older ages, particularly from respiratory disease. Our estimate of 0.6 million deaths from tobacco in 1990 is based more directly on local epidemiological evidence than the previous WHO estimate of 0.8 million for 1990.18
Table 5.
Deaths attributed to tobacco/total deaths (thousands) for all China, 1990
| Cause of death* | Men
|
Women
|
|||||
|---|---|---|---|---|---|---|---|
| <30† | 30-69 | ⩾70 | <30† | 30-69 | ⩾70 | ||
| Neoplastic: | 0/45 | 146/629 | 47/250 | 0/32 | 11/334 | 10/174 | |
| Lung | 0/2 | 51/98 | 24/51 | 0/1 | 7/37 | 6/28 | |
| Oesophagus | 0/1 | 23/84 | 8/44 | 0/1 | 1/38 | 1/23 | |
| Stomach | 0/1 | 26/142 | 6/66 | 0/2 | 1/65 | 1/43 | |
| Liver | 0/7 | 35/174 | 5/34 | 0/3 | 1/55 | 1/24 | |
| Five minor sites | 0/2 | 11/44 | 4/21 | 0/1 | 1/19 | 1/11 | |
| Chronic obstructive pulmonary disease, etc | 0/8 | 66/290 | 140/512 | 0/11 | 19/201 | 48/552 | |
| Respiratory tuberculosis | 0/11 | 13/111 | 13/53 | 0/12 | 2/63 | 2/30 | |
| Stroke | 0/11 | 30/302 | 15/359 | 0/8 | 0/221 | 0/372 | |
| Ischaemic heart disease | 0/5 | 24/164 | 6/217 | 0/3 | 5/123 | 5/251 | |
| Other causes† | 0/822 | 0/745 | 0/448 | 0/817 | 0/568 | 0/473 | |
| Total | 0/870 | 279/2154 (13%) | 221/1805 (12%) | 0/859 | 37/1390 (3%) | 65/1807 (4%) | |
The percentages attributed to smoking in table 1 have been combined with the global burden of disease28 estimates of the total numbers of deaths (taking larynx cancer as 5% of lung cancer and pulmonary heart disease as 10% of chronic obstructive pulmonary disease).
As in table 1.
No deaths from other causes and none before age 30 are attributed to tobacco.
The annual number of adult deaths in China is projected to rise from 7 million in 1990 (table 5) to 9 million in 2000, mainly because of population growth.28 Hence even without any further growth in the percentage of deaths attributed to tobacco the absolute number of such deaths will rise to 0.8 million in 2000. The expected increase in the percentage attributable to tobacco will, however, further increase this figure so that during the first decade of the next century Chinese mortality from tobacco will probably be about 1 million a year.
Discussion
The main findings are broadly compatible with the limited evidence available from Chinese prospective studies.29–33 A nationally representative prospective study of 224 500 men attributes about 12% of deaths at ages 40-79 to tobacco.33 Our results are also compatible with the findings of case-control studies in various parts of China on lung cancer,34–37 oesophageal cancer,38–42 stomach cancer,38 liver cancer,43–45 stroke,46 and myocardial infarction.47–49 Moreover, the main conclusions from the proportional mortality analyses can be confirmed by analyses that use the surviving spouses as the control group: this would multiply the all China risk ratios in table 1 in men and women by 1.04 and 1.08, with risks for all deaths becoming 1.28 and 1.33 and the proportions of deaths attributed to smoking becoming 15% and 4% (instead of 13% and 3%).
Causality
Most of the deaths associated with tobacco were due to neoplastic or respiratory disease. Mortality from these diseases was positively related to both the daily dose and, with the possible exception of liver cancer, the duration of smoking (the risks in middle age being greatest for those who smoked most and started youngest, tables 2–4). In 1985, the World Health Organisation’s International Agency for Research on Cancer concluded that smoking was an important cause of cancers of the lung, oesophagus, mouth, pharynx, larynx, pancreas, and bladder,50 and a more recent review adds cancers of the stomach and liver.51 Smoking can cause chronic obstructive lung disease.2,8,52 When tuberculosis was an important cause of death in Britain mortality from it was strongly related to smoking.8 For these and other reasons2,4,8 tobacco should be regarded as having actually been a cause of most or all of the excess mortality from neoplastic and respiratory disease among smokers.
For stroke and for ischaemic heart disease the risk ratios comparing smokers with non-smokers are not large, even in early middle age, and are not strongly related either to the daily number of cigarettes or to the age when smoking began. It is nevertheless likely that the association between smoking and vascular death in China is partly or wholly causal since studies in other countries have found a strong relation between prolonged cigarette use and vascular disease in middle age.2,4,8,49
Two causes of one death
The wide geographical variation across China in death rates among non-smokers and the size of the absolute excess among smokers shows that other important causes exist for the main diseases that can be caused by smoking. The 10-fold variation from one city to another in death rates from lung cancer in non-smokers (fig 4) may be due to a combination of both childhood and adult exposure4 to indoor fumes from domestic fuel34–37 (rather than to external air pollution or passive smoking); dietary factors may also be relevant.3 Because the risk ratio comparing smokers and non-smokers is relatively constant the absolute excess risk associated with smoking tends to be highest where the cancer rates in non-smokers are highest. In theory the correlation between lung cancer rates in smokers and non-smokers might be a statistical artefact produced by misclassification of many smokers as non-smokers, but the scale of such errors would have to have been implausibly large, especially among women, to have produced it.
Variation in the absolute tobacco hazard among smokers means that one particular death may have had two causes, avoidance of either of which would have avoided the death. For example, when a smoker living in the city of Harbin dies of lung cancer it is likely that the death would not have happened if that person had smoked but lived in the city of Xi’an or had lived in Harbin but not smoked. This is particularly relevant for smokers who die of tuberculosis, in whom infection with the tubercle bacillus is obviously one cause but death might not have occurred if the person had not also smoked.
Causality and increased probability
In China, as elsewhere, the ability of smoking to cause a particular disease just implies an increased probability of premature death from it. Thus many smokers do not get lung cancer (so smoking is not a “sufficient cause” of it), some non-smokers do get lung cancer (so smoking is not a “necessary cause” of it), but many smokers who get lung cancer would not have done so if they had not smoked (so smoking is an important cause of this disease).3 Also, since everybody eventually dies, the overall probability of death for smokers and for non-smokers is 100%. Smokers, however, are more likely to die before they reach old age—and on average those killed by smoking at ages 35-69 lose about 20-25 years of life.5–8
Main diseases attributed to tobacco in China
The main way that smoking kills people in China is by making diseases that are already fairly common somewhat more so. About 60% of the deaths attributed to tobacco were due to lung cancer or chronic obstructive pulmonary disease. Almost all the remainder were due to just six other diseases, each responsible for 5-8% of these deaths (oesophageal cancer, stomach cancer, liver cancer, tuberculosis, stroke, and ischaemic heart disease). The risk ratios for these eight diseases are generally much lower in China than in the United Kingdom or United States, but the background rates among non-smokers are (with the exception of ischaemic heart disease) much greater in China so the absolute risk produced by tobacco is still substantial among both men and women who smoke.
Tobacco hazard at current death rates
The all cause risk ratios for urban men who started smoking around the age of 20 averaged 1.35, and table 1 suggests that at present the risk ratios do not change between middle and old age. If, hypothetically, the risk ratio remained constant at 1.35 at all ages this would mean that one in four smokers (0.35/1.35) who started smoking at age 20 would eventually be killed by tobacco. The corresponding proportions are one in five for rural men, one in three for urban women, and one in four for rural women. Moreover, the risk ratios for men must have increased slightly since 1987. So at current (1990s) death rates for non-smokers and for smokers who started around age 20, about one smoker in four would be killed by tobacco. This is confirmed by the national prospective study.33
Tobacco hazard at future death rates
In countries such as the United Kingdom and United States recent studies show that about half of all persistent cigarette smokers are eventually killed by tobacco (a quarter at ages 35-69, a quarter at older ages).5–8 Studies at an earlier stage of the epidemic in these countries had, however, suggested that only about one smoker in four would be killed by it.7 Likewise, our study of Chinese death rates in 1987 must substantially underestimate the future tobacco hazards in middle and old age because few of those studied had been smoking substantial numbers of cigarettes since early adult life. The full effects of the large increase in Chinese cigarette consumption that took place between the 1950s and the 1970s, and the even larger increase from 500 billion cigarettes in 1980 to 1800 billion in 1996, will not be seen for many years. As the increase was mainly to due to an increase in each smoker’s cigarette consumption rather than an increase in the proportion of smokers it will substantially increase the risk per smoker even if cigarettes often replaced other types of tobacco.1–8 These large changes in cigarette consumption over the past few decades will at least double the current hazard of one smoker in four being killed by tobacco. So about half the young adults in China who are now becoming persistent cigarette smokers will eventually be killed by the habit.
Future deaths from smoking in China
For public health purposes what can still be substantially influenced is not the number of deaths from smoking in this decade or the next but the numbers of deaths over the next several decades if current smoking patterns persist. Detailed predictions for particular diseases are not reliable, especially since the background rates among non-smokers may change unpredictably in ways that also change the absolute effects of tobacco. (As well as nationwide changes in diet,3,20 exercise, and indoor air pollution in future decades, changes in chronic infective processes could affect the background rates of chronic obstructive pulmonary disease or of other conditions.) Although the detail of the long term future is uncertain, the overall pattern is not, and will, on current smoking uptake rates, be different for women and men.
Women
Our results show that the risks for those who smoke are much the same for women and men. The prevalence of smoking remains high among older women in cities such as Beijing, Harbin, Shenyang, and, particularly, Tianjin (where one third of those aged 35-69 in the reference group smoked). Although a substantial minority of women born before 1940 became smokers by age 25, only about 2% of those born since 1950 have done so. In two large nationwide surveys the prevalence of smoking among women aged 15-24 was 0.5% both in 1984 and in 1996.12–14 If the current pattern of low uptake rates persists then eventually deaths from smoking in women will fall, perhaps to about 1% of all female deaths. However, the danger remains that, as has happened in many Western countries,5 the number of young women becoming persistent smokers will increase—indeed, surveys have reported 10% of young women smoking in selected small areas in China.53
Men
At present about two thirds of young men in China become daily smokers before age 25, generally starting around age 20 and then persisting.12–14 If this pattern continues, and if about half of all such smokers are killed by the habit, then tobacco will eventually cause about one third of all deaths in Chinese men, and the nationwide proportion of deaths due to smoking will rise from 13% in 1987 to about 33%. (In the United States, the proportion of deaths at ages 35-69 attributed to smoking increased from 12% in the 1950s to 33% in the 1990s.5,6) Hence, about 100 million of the 0.3 billion Chinese males now aged 0-29 will be killed by tobacco (half dying in middle age, half in old age), which would imply about 3 million male deaths a year from tobacco when the young adults of today reach old age.
Overall projections
The projections of one million deaths a year from tobacco during the first decade of the next century and three million a year in the middle of the century are consistent with previous estimates of about two million Chinese deaths from tobacco in 2025.15–17 If current smoking patterns persist in China then such projections cannot be substantially wrong.
Acknowledgments
We thank former minister Chen Min Zhang for his encouragement, the thousands of doctors, nurses, and other field workers who conducted the surveys, and the million interviewees.
Editorial by Lopez and Paper p 1423
Footnotes
Funding: Medical Research Council and Imperial Cancer Research Fund in Britain; US National Institutes of Health grant No 5R01 CA 33638 to TCC, RP, JC and JL; and Chinese Academy of Medical Science and Ministry of Public Health in China.
Competing interest: None declared
References
- 1.Doll R, Peto R. Mortality in relation to smoking: 20 years’ observations on male British doctors. BMJ. 1976;ii:1525–1536. doi: 10.1136/bmj.2.6051.1525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Surgeon General. Reducing the health consequences of smoking: 25 years of progress. Report of the surgeon general, 1989. Rockville, MD: US Department of Health and Human Services; 1989. [Google Scholar]
- 3.Doll R, Peto R. The causes of cancer. J Natl Cancer Inst. 1981;66:1191–1308. [PubMed] [Google Scholar]
- 4.Zaridze D, Peto R, editors. Tobacco: a major international health hazard. Lyons: International Agency for Research on Cancer; 1986. (IARC scientific publication No 74.) [Google Scholar]
- 5.Peto R, Lopez AD, Boreham J, Thun M, Heath C. Mortality from tobacco in developed countries: indirect estimation from national vital statistics. Lancet. 1992;339:1268–1278. doi: 10.1016/0140-6736(92)91600-d. [DOI] [PubMed] [Google Scholar]
- 6.Peto R, Lopez AD, Boreham J, Heath C, Thun M. Mortality from tobacco in developed countries, 1950-2000. Oxford: Oxford University Press; 1994. [DOI] [PubMed] [Google Scholar]
- 7.Peto R. Smoking and death: the past 40 years and the next 40. BMJ. 1994;309:937–939. doi: 10.1136/bmj.309.6959.937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Doll R, Peto R, Wheatley K, Gray R, Sutherland I. Mortality in relation to smoking: 40 years’ observations on male British doctors. BMJ. 1994;309:901–911. doi: 10.1136/bmj.309.6959.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weng XZ. The anti-smoking campaign in China. In: Dunstan B, Jamrozik K, editors. Tobacco and health 1990—the global war: proceedings of the seventh world conference on tobacco and health. Perth: Health Department of Western Australia; 1990. pp. 131–132. [Google Scholar]
- 10.Mackay J. Transnational tobacco companies versus state monopolies in Asia. In: Slama K, editor. Tobacco and health: proceedings of the ninth world conference on tobacco and health. New York: Plenum Press; 1995. pp. 61–66. [Google Scholar]
- 11.Zolty B. Country profiles: China. In: Lopez AD, Collishaw N, editors. Tobacco or health—a global status report. Geneva: World Health Organisation; 1997. pp. 441–445. [Google Scholar]
- 12.Weng XZ, editor. Report on the 1984 Chinese national smoking prevalence survey. Beijing: People’s Medical Publishing House; 1988. [Google Scholar]
- 13.Yang GH, Fan LX, Huan ZJ, Li FT, Chen AP, Zhang YF, et al. Abstracts of the 10th world conference on tobacco and health. Beijing: Chinese Medical Association; 1997. The 1996 national survey of smoking prevalence in China; p. 3. [Google Scholar]
- 14.Yang GH, editor. Report on the 1996 nationwide survey of smoking prevalence. Beijing: China Science and Technology Press; 1997. [Google Scholar]
- 15.Peto R. Tobacco: UK and China. Lancet. 1986;ii:1038. doi: 10.1016/s0140-6736(86)92645-0. [DOI] [PubMed] [Google Scholar]
- 16.Peto R. Tobacco-related deaths in China. Lancet. 1987;ii:211. doi: 10.1016/s0140-6736(87)90783-5. [DOI] [PubMed] [Google Scholar]
- 17.Yu JJ, Mattson ME, Boyd GM, Mueller MD, Shopland DR, Pechacek TF, et al. A comparison of smoking patterns in the People’s Republic of China with the United States: an impending health catastrophe in the Middle Kingdom. JAMA. 1990;264:1575–1579. [PubMed] [Google Scholar]
- 18.Ad Hoc Committee on Health Research Relating to Future Intervention Options. Investing in health research and development. Geneva: World Health Organisation; 1996. (Document TDR/Gen/96.1.) [Google Scholar]
- 19.World Health Organisation. World health statistics annual 1995. Geneva: WHO; 1996. [Google Scholar]
- 20.Chen JS, Campbell TC, Li JY, Peto R. Diet, lifestyle and mortality in China. Oxford: Oxford University Press, Cornell University Press, and People’s Medical Publishing House; 1990. [Google Scholar]
- 21.Editorial Committee for the Atlas of Cancer Mortality. Atlas of cancer mortality in the People’s Republic of China. Shanghai: China Map Press; 1979. [Google Scholar]
- 22.Zhou YS, editor. Atlas of mortality from main death causes in China. Beijing: China Cartographic Publishing House; 1990. [Google Scholar]
- 23.World Health Organisation. International classification of diseases, ninth revision (ICD-9). Geneva: WHO; 1977. [Google Scholar]
- 24.Deng J, Gao YT. The prevalence of smoking habit among 110 000 adult residents in urban Shanghai [in Chinese] Chin J Prev Med. 1985;5:271–274. [PubMed] [Google Scholar]
- 25.Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22:719–748. [PubMed] [Google Scholar]
- 26.Armitage P, Berry G. Statistical methods in medical research. 2nd ed. Oxford: Blackwell Scientific; 1987. [Google Scholar]
- 27.Early Breast Cancer Trialists’ Collaborative Group. Treatment of early breast cancer. Vol 1. Worldwide evidence 1985-1990. Oxford: Oxford Medical Publications, 1990.
- 28.Murray CJL, Lopez AD, eds. The global burden of disease and injury series. Vol 1. A comprehensive assessment of mortality and disability from diseases, injuries and risk factors in 1990, and projected to 2020. Boston: Harvard School of Public Health, 1996.
- 29.Chen ZM, Xu Z, Collins R, Li WX, Peto R. The early health effects of the emerging tobacco epidemic in China: 16-year prospective study. JAMA. 1997;278:1500–1504. doi: 10.1001/jama.278.18.1500. [DOI] [PubMed] [Google Scholar]
- 30.Yuan JM, Ross RK, Wang XL, Gao YT, Henderson BE, Yu MC. Morbidity and mortality in relation to cigarette smoking: a prospective male cohort study in Shanghai, China. JAMA. 1996;275:1646–1650. [PubMed] [Google Scholar]
- 31.Lam TH, He Y, Li LS, Li LS, He SF, Liang BQ. Mortality attributable to smoking in China. JAMA. 1997;278:1505–1508. [PubMed] [Google Scholar]
- 32.Gao YT, Dent J, Yuan ZX, Qin DL, Xiang YB, Zhou TK, et al. Follow-up of 210 000 adults in Shanghai, China. In: Wang DM, editor. Abstracts of the 1995 congress of the International Epidemiological Association regional meeting in Shanghai. Shanghai: Chinese Medical Association; 1995. pp. 18–19. [Google Scholar]
- 33.Niu SR, Yang GH, Chen ZM, Wang JL, Wang GH, He XZ, et al. Emerging tobacco hazards in China. 2. Early mortality results from a prospective study. BMJ. 1998;317:1423–1424. doi: 10.1136/bmj.317.7170.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gao YT, Blot WJ, Zheng W, Fraumeni J, Hsu CW. Lung cancer and smoking in Shanghai. Int J Epidemiol. 1988;17:277–280. doi: 10.1093/ije/17.2.277. [DOI] [PubMed] [Google Scholar]
- 35.Xu ZY, Blot WJ, Xiao HP, Wu A, Feng YP, Stone BJ, et al. Smoking, air pollution, and the high rates of lung cancer in Shenyang, China. J Natl Cancer Inst. 1989;81:1800–1806. doi: 10.1093/jnci/81.23.1800. [DOI] [PubMed] [Google Scholar]
- 36.Liu ZY. Smoking and lung cancer in China: combined analysis of eight case-control studies. Int J Epidemiol. 1992;21:197–201. doi: 10.1093/ije/21.2.197. [DOI] [PubMed] [Google Scholar]
- 37.Gao YT, Blot WL, Zheng W, Ershow A, Hsu CW, Levin LL, et al. Lung cancer among Chinese women. Int J Epidemiol. 1988;17:277–280. doi: 10.1093/ije/17.2.277. [DOI] [PubMed] [Google Scholar]
- 38.Li JY, Ershow A, Chen ZJ, Wacholder S, Li GY, Guo W, et al. A case-control study of cancer of the oesophagus and gastric cardia in Linxian. Int J Cancer. 1989;43:755–761. doi: 10.1002/ijc.2910430502. [DOI] [PubMed] [Google Scholar]
- 39.Wang YP, Han XY, Su W, Wang YL, Zhu TW, Sasaba T, et al. Oesophageal cancer in Shanxi province, People’s Republic of China: a case-control study in high and moderate risk areas. Cancer Causes Control. 1992;3:107–113. doi: 10.1007/BF00051650. [DOI] [PubMed] [Google Scholar]
- 40.Gao YT, McLaughlin JK, Blot WJ, Ji BT, Benichou J, Dai Q, et al. Risk factors for oesophagus cancer in Shanghai, China. 1. Role of cigarette smoking and alcohol drinking. Int J Cancer. 1994;58:192–196. doi: 10.1002/ijc.2910580208. [DOI] [PubMed] [Google Scholar]
- 41.Li JF, Nyren O, Wolk A, Bergstrom N, Yuen J, Adami HO, et al. Risk factors for oesophageal cancer in Northeast China. Int J Cancer. 1994;57:38–45. doi: 10.1002/ijc.2910570108. [DOI] [PubMed] [Google Scholar]
- 42.Cheng KK, Day NE, Duffy SW, Lam TH, Fork M, Wong J. Pickled vegetables in the aetiology of oesophageal cancer in Hong Kong Chinese. Lancet. 1992;339:1314–1318. doi: 10.1016/0140-6736(92)91960-g. [DOI] [PubMed] [Google Scholar]
- 43.Yu MC, Henderson BE. A case-control study of hepatocellular carcinoma and the hepatitis B virus, cigarette smoking and alcohol consumption. Cancer Res. 1987;47:654–655. [PubMed] [Google Scholar]
- 44.Lu SN, Lin TM, Chen CJ, Chen JS, Liaw YF, Chang WY, et al. A case-control study of primary hepatocellular carcinoma in Taiwan. Cancer. 1988;62:2051–2055. doi: 10.1002/1097-0142(19881101)62:9<2051::aid-cncr2820620930>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 45.Lam KC, Yu MC, Leung JWC, Henderson BE. Hepatitis B virus and cigarette smoking: risk factors for hepatocellular carcinoma in Hong Kong. Cancer Res. 1982;42:5246–5248. [PubMed] [Google Scholar]
- 46.Li SC, Schoenberg BS, Wang CC, Cheng XM, Bolis CL, Wang KJ. Cerebrovascular disease in the People’s Republic of China: epidemiologic and clinical features. Neurology. 1985;35:1708–1713. doi: 10.1212/wnl.35.12.1708. [DOI] [PubMed] [Google Scholar]
- 47.Yao LC, Du FC, Xu YC, Hong LJ, Zhou JY, Ye BF, et al. Cigarette smoking and coronary heart disease: a case-control study [in Chinese] Chin J Epidemiol. 1984;5:98–99. [Google Scholar]
- 48.He Y, Lam TH. A review on studies of smoking and coronary heart disease in China. Chin Med J (in press). [PubMed]
- 49.Parish S, Collins R, Peto R, Youngman L, Barton J, Jayne K, et al. for the International Studies of Infarct Survival (ISIS) Collaborators. Cigarette smoking, tar yields, and non-fatal myocardial infarction: 14 000 cases and 32 000 controls in the United Kingdom BMJ 1995311471–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.International Agency for Research on Cancer. IARC monographs on the evaluation of the carcinogenic risk of chemicals to humans. Vol 38. Tobacco smoking. Lyons: IARC, 1986.
- 51.Doll R. Cancers weakly related to smoking. Br Med Bull. 1996;52:35–49. doi: 10.1093/oxfordjournals.bmb.a011531. [DOI] [PubMed] [Google Scholar]
- 52.Fletcher CM, Peto R. The natural history of chronic airflow obstruction. BMJ. 1977;i:1645–1648. doi: 10.1136/bmj.1.6077.1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Charlton A, Mackay J, Moyer C, Niu SR, Lam TH. Smoking and youth in China, 1992: review and recommendations. Geneva: International Union Against Cancer; 1993. [Google Scholar]