Abstract
Background
Rotator cuff tears are common shoulder problems whose propagation is difficult to predict because of the structural and mechanical inhomogeneity of the supraspinatus tendon. We have previously shown that the supraspinatus and the infraspinatus tendons mechanically interact when the supraspinatus tendon is intact or exhibits a full-thickness tear so that an increase in supraspinatus tendon strain is paralleled by an increase in infraspinatus tendon strain. Such interaction is critical and suggests that an increase in infraspinatus tendon strain that accompanies an increase in supraspinatus tendon strain may shield the supraspinatus tendon from further injury but increase the risk of injury to the infraspinatus tendon. In this study, the mechanical interactions between the supraspinatus and infraspinatus tendons were evaluated for the commonly occurring supraspinatus tendon partial-thickness tears through a range of rotation angles.
Methods
For each joint rotation and supraspinatus tendon tear size evaluated, the supraspinatus tendon was loaded, and images corresponding to 5N, 30N, 60N and 90N of supraspinatus tendon load were isolated for the speckle painted supraspinatus and infraspinatus tendons. A region of interest outlining the insertion site was isolated and displacements between the 5N loaded image and each of the others were measured, from which normalized average principal strains were quantified in both tendons.
Results
The observed effect on infraspinatus tendon strain paralleled that observed on strain in the supraspinatus tendon. Introducing a supraspinatus tendon partial-thickness tear and increasing load caused an increase in normalized average maximum and a decrease in normalized average minimum principal strain in the infraspinatus tendon. Increasing rotation angle from internal to external rotation caused a general decrease in normalized average maximum and increase in normalized average minimum principal strain in both tendons.
Conclusion
The supraspinatus and infraspinatus tendons mechanically interact for the intact and partially torn supraspinatus tendons for neutral and rotated glenohumeral joint.
Level of Evidence
This is a basic science research study
Keywords: rotator cuff tears, supraspinatus strain, shoulder mechanics, shoulder, infraspinatus strain, mechanical interactions
Introduction
Rotator cuff tears are common and debilitating shoulder injuries that cause significant pain and disability. Partial-thickness tears have the highest incidence of occurrence of all rotator cuff tears, and have been reported to impact 13–37% of the general population.4,8–10 Despite their high incidence of occurrence, objective data to guide clinical decision-making for the treatment of partial-thickness rotator cuff tears has been limited.4,14,16 Currently, the size of the partial-thickness tear greatly influences clinical decision making regardless of the location of the tear.6,17 Additionally the decision to surgically repair a rotator cuff tear does not ensure satisfactory clinical outcome, with some patients reporting only minimal improvement following repair.11,13,19
Due to the anatomic inhomogeneity of the rotator cuff, establishing more reliable criteria for clinical intervention than the size of the tear is necessary. Several studies evaluated the effect of a supraspinatus tendon tear on the remaining intact portion of the tendon to understand the effect of a supraspinatus tendon tear on the loading environment.2,18 Tissue strain was used to evaluate the load bearing capacity of the remaining intact portion of the tendon to provide data to assess the risk of tear propagation. However, despite the importance of this data, assessing the likelihood of partial-thickness tear propagation is complicated by the loading environment and the complex tissue architecture of the rotator cuff. For instance, the interaction between the humeral head and the torn supraspinatus tendon has been shown to decrease the effect of a supraspinatus tendon tear on strain in the supraspinatus tendon at certain joint positions.2 Additionally, interactions between the complex network of tendons and other soft connective tissues that allow the glenohumeral joint its wide range of motion further complicates the ability to predict the likelihood of tear propagation. Therefore, other rotator cuff structures, such as the infraspinatus tendon, may impact the likelihood of supraspinatus partial-tear propagation and be reciprocally impacted by the existence of a supraspinatus tendon tear.
Previously, we have shown that with the arm at the side (physiologically neutral position, defined by 0° humeral abduction, rotation and flexion), strain in the infraspinatus tendon increases with the introduction of a supraspinatus tendon full-thickness tear.1 The observed increase in strain in the infraspinatus tendon paralleled increase in strain in the supraspinatus tendon. The inhomogeneity of the supraspinatus tendon limits the extrapolation of these results to the more commonly occurring partial-thickness tear. It is likely that a partial-thickness tear in the supraspinatus tendon will cause a different loading environment than a full-thickness tear and impact the interaction between the two tendons. Additionally, the joint rotation angle affects the contact area between the infraspinatus tendon and the humeral head, potentially impacting the strain environment in the infraspinatus tendon and the interaction between the two tendons. Therefore, the objective of this study is to investigate whether there is a mechanical interaction between the intact infraspinatus and supraspinatus tendons through a range of rotation angles that would cause increased strains in the infraspinatus tendon when the supraspinatus tendon is subjected to partial-thickness tears. We hypothesize that: H1: Increasing the partial-thickness tear size in the supraspinatus tendon will cause an increase in average maximum and a decrease in average minimum principal strain in the infraspinatus tendon; H2: Increasing the load level applied to the supraspinatus tendon will cause an increase in average maximum and decrease in average minimum principal strain in the infraspinatus tendon; H3: The effect of supraspinatus tendon tear thickness on infraspinatus tendon strain will differ with increasing supraspinatus tendon load. H4: Altering the rotation angle from internal to external rotation, will cause an increase in average maximum and a decrease in average minimum principal strain in the infraspinatus and supraspinatus tendons.
Materials and Methods
Following IRB exempt approval, ten healthy, fresh-frozen cadaveric shoulders (7 males, 3 females, age 48.7±15.1 yrs) were randomly chosen for inclusion and dissected free of soft tissue, retaining the proximal humerus, supraspinatus and infraspinatus tendons. Specimens with visible rotator cuff tears or fraying were excluded from the study. The proximal end of the infraspinatus tendon was sutured using a Krakow stitch to allow application of a load. Prior to mechanical testing, specimens were maintained in a physiologic bath of phosphate buffered saline (PBS).
The supraspinatus and infraspinatus tendon bursal surfaces were air-brushed with black paint to create a fine texture for texture correlation strain analysis using Vic2D (V4.4.1, Correlated Solutions Inc., Columbia, SC). This software utilizes a texture correlation algorithm3 as described previously.1
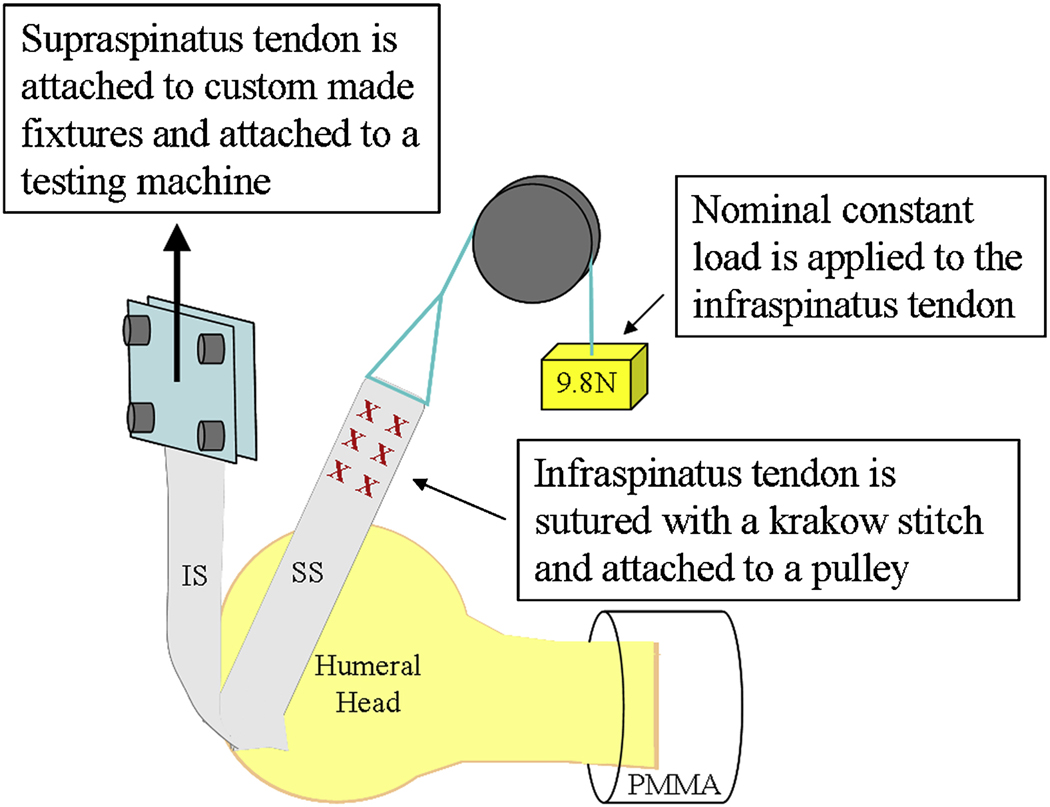
A modification of the experimental setup described in our previous study was used. Briefly, the humerus was mounted in Poly(methyl methacrylate) (PMMA) in custom grips and the supraspinatus tendon was attached to a testing machine (5543, Instron, Norwood, MA) to allow for controlled loading (figure 1). During supraspinatus tendon loading, the infraspinatus tendon was attached to a pulley system with a nominal, constant load of 9.8 N. In this study, the fixture was modified to allow for a controlled and reproducible rotation of the humeral head. The joint was initially positioned such that the direction of loading of both tendons was along their physiologically neutral position, defined by a 0° humeral abduction, rotation and flexion. The effect of internal and external rotation was also evaluated by internally and externally rotating the humeral head by 30° degrees at 0° humeral abduction and flexion.
Figure 1.
Schematic representation of experimental setup.
The supraspinatus tendon loading protocol previously described was used.1 Briefly, the supraspinatus tendon was preconditioned, followed by a constant ramp to 90N at a rate of 0.1% of the tendon length per second. A maximum load of 90N was chosen (~15% of ultimate load), and represents a large but reasonable load.12 The loading protocol was applied to the intact supraspinatus tendon at neutral position and at internal and external rotation. An anterior edge partial-thickness tear through 66% of the width of the tendon was surgically created in the supraspinatus tendon bursal side and the loading protocol was repeated again at all 3 rotation angles. The tear was then extended through 66% of the tendon thickness and the loading protocol was repeated once again at all 3 rotation angles. Finally the tear was extended through 100% of the tendon thickness and the loading protocol was repeated once again at all 3 angles. The order in which the joint positions were evaluated was randomly altered at each tear size. Both tendons were generously moistened with PBS after each completion of the loading protocol.
Images were taken of the supraspinatus and the infraspinatus insertion sites at 1 second intervals during the loading ramp phase of the testing protocol. For each tear level (intact, 33% partial-thickness, 66% partial-thickness and full thickness), images at 5N, 30N, 60N and 90N of supraspinatus tendon loads were chosen for evaluation for the infraspinatus. As described, a region of interest was outlined to mark the insertion site of the infraspinatus tendon and the consistently intact posterior third of the supraspinatus tendon’s insertion site, for images that correspond to a nominally loaded supraspinatus tendon (figure 2)1. A digital grid of nodes was then fitted in the region of interest. Displacements of the nodes between the 5N load and each of the 30, 60N and 90N loads were measured and the two-dimensional Lagrangian finite strain tensor (εxx, εyy, and εxy) from which the principal strain components were calculated. Average maximum and minimum principal strains were determined for the infraspinatus tendon insertion site. Principal strain components capture a simple and complete depiction of the loading environment by absorbing the shear strain component into the orthogonal tensile (maximum principal strain) and compressive (minimum principal strain) components through a coordinate rotation. This allows the complex strain environment to be fully characterized by the tensile and compressive deformation indicated by average maximum and minimum principal strain, respectively.
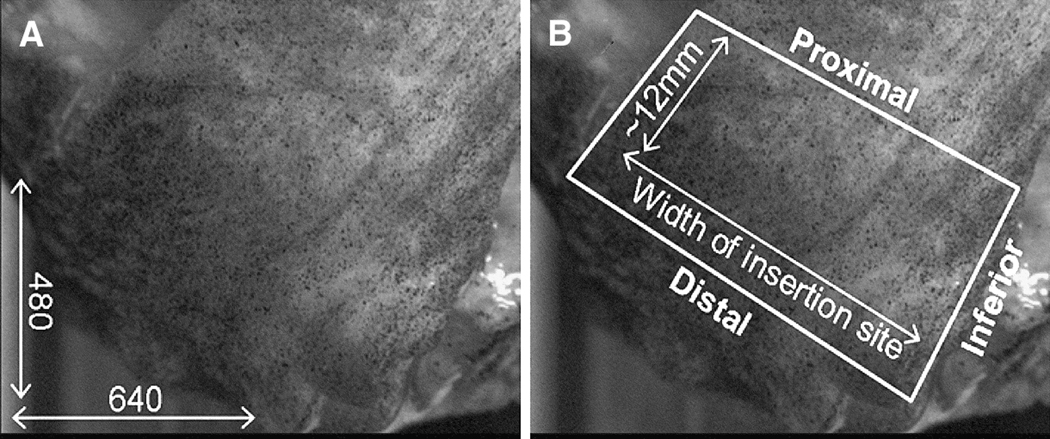
Figure 2.
The region of interest for strain analysis in the infraspinatus tendon is shown in white. (A) Image resolution was approximately 0.05mm/pixel. (B) The distal, superior and inferior borders are defined by the natural edges of the tendon, and the proximal border is approximately 12mm proximal to the distal edge.
The insertion site of the infraspinatus tendon is not planar but rather slightly curved due to the curvature of the humeral head. Therefore, our “strain” measurements refer to “apparent strain”.
To evaluate the effect of partial-thickness tears (H1), at each load and rotation, data from each subject was normalized by dividing by the average principal strain of the intact tendon case, and separate repeated measures one-way ANOVA’s were conducted with post hoc Bonferroni to compare each tear condition to the intact (control) case only. To evaluate the effect of load at each tear and joint position (H2), average principal strains at each load was normalized by average principal strain at 30N load and separate repeated measures ANOVA’s were conducted with post hoc Bonferroni to compare all normalized loaded conditions. To evaluate the effect of joint rotation (H4), for each tear and load, average principal strains for both internal and external rotation were normalized by the average principal strain values at neutral rotation, and separate repeated measures ANOVA’s were conducted with post hoc Bonferroni to compare all joint positions. Significance (*) was set at p ≤ 0.05 and a trend (#) at p ≤ 0.1.
Results
In general, the observed effect on infraspinatus tendon strain paralleled that observed for strain in the supraspinatus tendon. In comparison to the intact tendon case, introducing a partial-thickness tear in the supraspinatus tendon resulted in a higher normalized average maximum and minimum principal strain in the supraspinatus and infraspinatus tendons. As expected, increasing the load applied to the supraspinatus tendon resulted in an increase in normalized average maximum and minimum principal strain in both tendons. In contrast to our hypothesis, increasing the rotation angle from internal to external rotation resulted in no significant effect on normalized average maximum principal strain in the supraspinatus or infraspinatus tendons, and a decrease in normalized average minimum principal strain in the supraspinatus tendon only. The effect of rotation depended on the load and tear size evaluated in the supraspinatus but not the infraspinatus tendon. Raw average maximum and minimum principal strain values are shown for the supraspinatus (Table I) and infraspinatus tendons (Table II) in the electronic supplement.
Table I.
Raw average maximum and minimum principal strain values in the supraspinatus tendon
| Joint Position |
Load | Intact | 33% Tear | 66% Tear | 100% Tear | |
|---|---|---|---|---|---|---|
| Average Maximum Principal Strain |
0° rotation | 30N | 3.58 ± 1.41 | 4.47 ± 1.56 | 4.88 ± 2.33 | 5.12 ± 2.89 |
| 60N | 5.30 ± 1.70 | 5.97 ± 1.80 | 6.38 ± 2.47 | 7.29 ± 3.71 | ||
| 90N | 6.36 ± 1.82 | 7.01 ± 1.87 | 7.48 ± 2.61 | 8.71 ± 4.18 | ||
| 30° internal | 30N | 5.22 ± 4.09 | 5.14 ± 4.24 | 5.28 ± 4.78 | 5.94 ± 5.75 | |
| 60N | 7.77 ± 5.19 | 7.23 ± 5.27 | 7.50 ± 5.69 | 8.10 ± 6.70 | ||
| 90N | 9.43 ± 5.64 | 8.59 ± 5.74 | 8.88 ± 6.10 | 9.47 ± 7.11 | ||
| 30° external | 30N | 4.75 ± 2.56 | 5.58 ± 3.21 | 5.54 ± 3.27 | 5.65 ± 5.33 | |
| 60N | 6.51 ± 3.75 | 7.64 ± 4.34 | 7.55 ± 4.62 | 8.29 ± 6.29 | ||
| 90N | 7.79 ± 4.43 | 9.02 ± 4.89 | 8.81 ± 5.49 | 10.63 ± 7.21 | ||
| Average Minimum Principal Strain |
0° rotation | 30N | −2.49 ± 2.36 | −3.59 ± 3.38 | −3.61 ± 2.61 | −4.64 ± 2.73 |
| 60N | −4.26 ± 3.41 | −5.92 ± 4.61 | −5.94 ± 3.68 | −7.49 ± 4.12 | ||
| 90N | −5.59 ± 3.98 | −7.48 ± 5.10 | −7.68 ± 4.11 | −9.38 ± 4.80 | ||
| 30° internal | 30N | −4.20 ± 3.03 | −4.29 ± 2.50 | −4.03 ± 2.48 | −4.18 ± 1.92 | |
| 60N | −7.92 ± 3.24 | −7.63 ± 3.18 | −7.25 ± 2.93 | −7.66 ± 2.52 | ||
| 90N | −11.21 ± 3.15 | −10.27 ± 3.22 | −9.71 ± 3.01 | −10.14 ± 3.07 | ||
| 30° external | 30N | −2.85 ± 2.21 | −3.08 ± 1.46 | −2.68 ± 1.95 | −3.92 ± 2.73 | |
| 60N | −4.11 ± 3.10 | −4.61 ± 2.17 | −4.08 ± 3.01 | −6.47 ± 3.95 | ||
| 90N | −4.84 ± 3.73 | −5.52 ± 2.86 | −4.87 ± 3.79 | −8.34 ± 4.64 | ||
Table II.
Raw average maximum and minimum principal strain values in the supraspinatus tendon
| Joint Position |
Load | Intact | 33% Tear | 66% Tear | 100% Tear | |
|---|---|---|---|---|---|---|
| Average Maximum Principal Strain |
0° rotation | 30N | 2.19 ± 1.84 | 3.50 ± 4.09 | 3.31 ± 4.10 | 3.98 ± 4.65 |
| 60N | 3.11 ± 3.22 | 5.03 ± 6.01 | 4.75 ± 6.07 | 5.55 ± 6.92 | ||
| 90N | 3.84 ± 4.00 | 6.00 ± 7.23 | 5.61 ± 7.28 | 6.56 ± 8.09 | ||
| 30° internal | 30N | 2.06 ± 1.08 | 1.79 ± 0.87 | 2.25 ± 1.69 | 2.29 ± 2.11 | |
| 60N | 3.47 ± 2.25 | 3.00 ± 2.13 | 3.56 ± 2.89 | 3.51 ± 3.66 | ||
| 90N | 4.72 ± 3.72 | 4.26 ± 4.34 | 4.60 ± 4.25 | 4.45 ± 5.16 | ||
| 30° external | 30N | 1.38 ± 0.94 | 1.64 ± 1.06 | 1.64 ± 1.19 | 1.43 ± 1.11 | |
| 60N | 1.62 ± 1.11 | 1.97 ± 1.30 | 1.89 ± 1.47 | 1.78 ± 1.31 | ||
| 90N | 1.73 ± 1.15 | 2.09 ± 1.41 | 1.95 ± 1.60 | 1.97 ± 1.43 | ||
| Average Minimum Principal Strain |
0° rotation | 30N | −2.63 ± 1.80 | −3.50 ± 2.76 | −3.14 ± 2.39 | −3.08 ± 2.59 |
| 60N | −3.80 ± 2.54 | −4.85 ± 3.73 | −4.39 ± 3.23 | −4.29 ± 3.36 | ||
| 90N | −4.53 ± 3.01 | −5.59 ± 4.20 | −5.07 ± 3.71 | −4.94 ± 3.70 | ||
| 30° internal | 30N | −2.01 ± 2.76 | −2.09 ± 3.04 | −2.01 ± 2.40 | −1.84 ± 2.43 | |
| 60N | −2.94 ± 4.04 | −2.71 ± 3.58 | −3.03 ± 3.37 | −2.58 ± 3.35 | ||
| 90N | −3.75 ± 5.00 | −3.20 ± 4.24 | −3.76 ± 4.30 | −3.09 ± 4.10 | ||
| 30° external | 30N | −1.53 ± 1.32 | −1.66 ± 1.87 | −1.70 ± 1.72 | −1.82 ± 1.35 | |
| 60N | −1.99 ± 1.67 | −2.15 ± 2.30 | −2.22 ± 2.19 | −2.80 ± 2.30 | ||
| 90N | −2.22 ± 1.80 | −2.38 ± 2.48 | −2.45 ± 2.34 | −3.58 ± 3.32 | ||
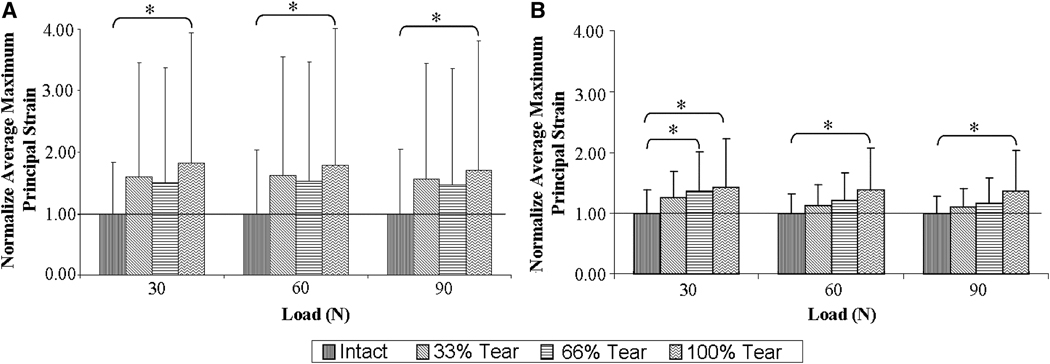
Effect of Partial-Thickness Tears
In support of our hypothesis, at neutral rotation, introduction of a partial-thickness tear resulted in significantly higher normalized average maximum principal strain in both tendons. In the supraspinatus tendon, normalized average maximum principal strain was significantly higher at 90N for 66% partial-thickness and 100% full-thickness tears than intact and at 30N for 100% full-thickness than intact (Figure 3). Similarly, in the infraspinatus tendon, for all supraspinatus tendon loads, normalized average maximum principal strain was higher for the 100% supraspinatus tendon full-thickness tear case than intact (Figure 3). In the supraspinatus tendon, normalized average minimum principal strain was significantly higher for the 100% full-thickness than intact for all loads. There was no significant difference in infraspinatus normalized average minimum principal strain between the evaluated tears and the intact tendon case.
Figure 3.
Effect of partial-thickness tear on normalized average maximum principal strain in the (A) infraspinatus and (B) supraspinatus tendon at neutral position. A statistical symbol (*) above a bar denotes significant difference from 1 (intact). At this joint position, introduction of a supraspinatus tendon tear caused an increase in normalized average maximum principal strain in the infraspinatus (A) and supraspinatus (B) tendons.
For both the supraspinatus and infraspinatus tendons, at 30° internal rotation, no significant differences were found for either principal strain component between the intact and torn supraspinatus tendon cases. At 30° external rotation, introducing any of the tears evaluated resulted in no significant increase in normalized average maximum principal strain in the supraspinatus or infraspinatus tendons. Normalized average minimum principal strain in the infraspinatus tendon was not significantly altered with the introduction of a partial-thickness tear in the supraspinatus tendon. Normalized average minimum principal strain in the supraspinatus tendon was higher for the full-thickness than the intact tendon case at 60N and 90N loads only.
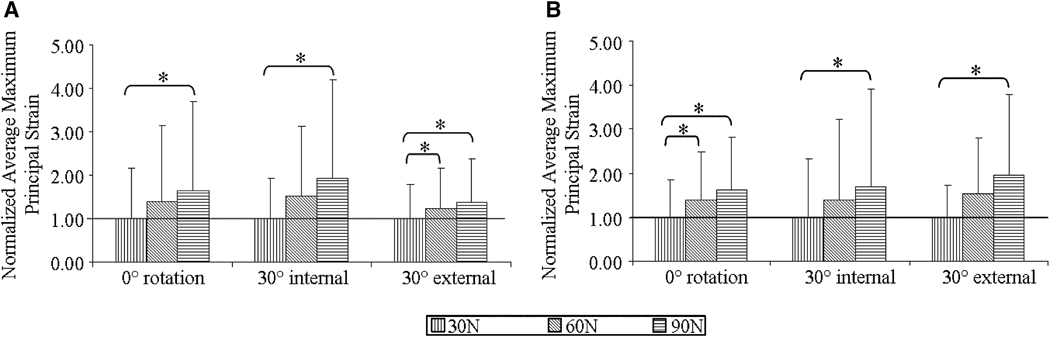
Effect of load
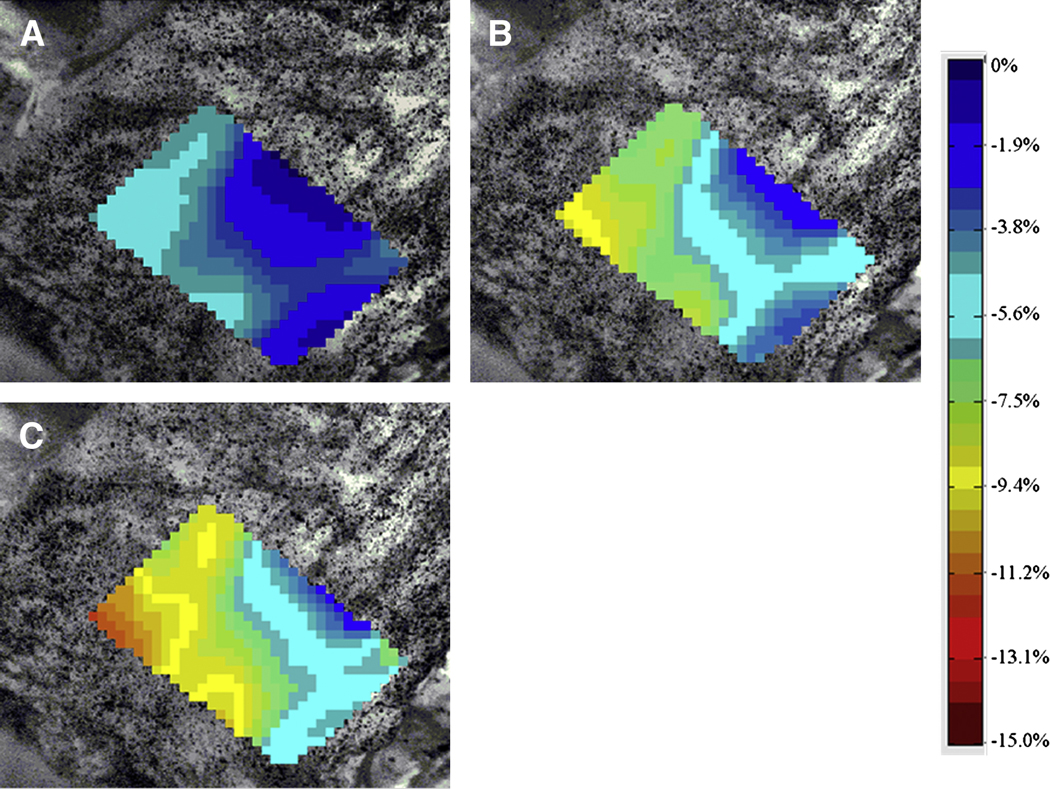
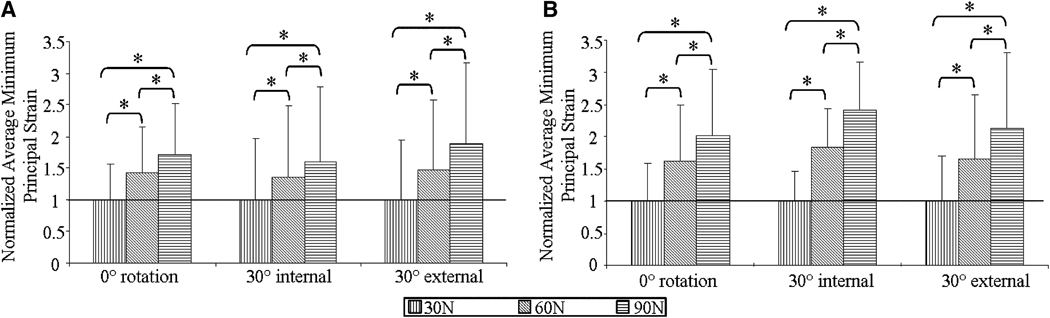
In the infraspinatus tendon, normalized average maximum principal strain was lower for 30N than 90N (significant for all joint position and tear conditions, with the exception of 66% tear at 30° external rotation) and 60N (significant for 33% and 100% tears at 30° external rotation) of supraspinatus tendon loads. Similarly, normalized average minimum principal strain in the infraspinatus tendon was significantly lower at 30N than at 60N (at neutral rotation for all tears and at 30° external rotation for intact, 33%, 66% tear cases) and 90N (for all tears at all joint positions) of supraspinatus tendon loads. Figure 4 shows normalized average maximum principal strain at 100% tear. Typical strain maps depicting the distribution of minimum principal strain per load in the infraspinatus tendon for the intact supraspinatus tendon case are shown in Figure 5.
Figure 4.
In the infraspinatus tendon, at 100% tear, normalized average maximum (A) and minimum (B) principal strain was significantly greater at 90N than 60N, and for some shown cases, at 60N than control
Figure 5.
Strain maps of minimum principal strain in the infraspinatus tendon at (A) 30N, (B) 60N, and (C) 90N for the intact supraspinatus tendon case. There was an increase in compressive strain (larger negative number) with increase in supraspinatus tendon load.
In the supraspinatus tendon, normalized average maximum and minimum principal strains were significantly higher for 90N than 60N and both were significantly higher than 30N for all tear cases at neutral rotation and 30° internal rotation. The same results were observed at 30° external rotation, with the exception that normalized average minimum principal strain was significantly lower for only 30N than 90N for the intact, 33% and 66% tear cases and similarly for normalized average maximum principal for the 66% tear case. Figure 6 shows normalized average maximum (A) and minimum (B) principal strain in the supraspinatus tendon at 100% tear.
Figure 6.
In the supraspinatus tendon, at 100% tear, normalized average maximum (A) and minimum (B) principal strain was significantly greater at 90N than 60N and control, and at 60N than control
Effect of rotation
For all partial-thickness tears and loads evaluated, normalized average maximum principal strain in the supraspinatus and infraspinatus tendons was not significantly altered with change in joint rotation.
In the supraspinatus tendon, the effect of joint rotation on normalized average minimum principal strain in the supraspinatus tendon was significant at 90N for the intact, 33% and 66% tear cases. More specifically, at this load level, normalized average minimum principal strain was significantly higher at 30° internal rotation than at 30° external rotation for the intact, 33% and 66% tear cases, and than neutral rotation for the intact supraspinatus tendon case. Normalized average minimum principal strain was not significantly affected by joint rotation in the infraspinatus tendon.
Discussion
Our results support our hypothesis that as supraspinatus tendon partial-thickness tear size increases, there is an increase in normalized average maximum and minimum principal strain in the infraspinatus tendon. As expected, this effect of supraspinatus partial-thickness tear size on infraspinatus tendon strain corresponded to an increase in normalized average maximum and minimum principal strain in the supraspinatus tendon. Similarly, our results supported our hypothesis that loading in the supraspinatus tendon caused an increase in normalized average maximum and minimum principal strain in the infraspinatus tendon. In contrast to our hypothesis, for all tears and loads, normalized average maximum principal and minimum principal strain in the infraspinatus tendon was not impacted by changing the joint rotation angle from internal to external rotation. Similarly, in the supraspinatus tendon, rotation angle had no effect on normalized average maximum principal strain. The effect of rotation angle on normalized minimum principal strain in the supraspinatus tendon was dependent on the load being evaluated, where at 90N, internal rotation resulted in higher normalized average minimum principal strain than at external rotation for the intact, 33% and 66% tear, and than at neutral rotation for the intact supraspinatus tendon case only. Joint rotation had no effect on supraspinatus tendon strain for the full-thickness tear case.
The increase in normalized average maximum principal strain observed in the infraspinatus tendon with the introduction of partial-thickness tears indicates that the supraspinatus and infraspinatus tendons mechanically interact under these tear conditions. While expected, results support evaluating the loading capacity of the infraspinatus tendon in the presence of a supraspinatus tendon partial-thickness tear. The significant increase in normalized average maximum principal strain observed with the introduction of partial-thickness supraspinatus tendon tears may indicate an increase in risk of injury to the infraspinatus tendon.
Results did not support our hypotheses regarding the effect of joint rotation. We hypothesized that changing the rotation angle from internal to external rotation would cause an increase in strain in both the supraspinatus and infraspinatus tendons. This was expected since contact between the humeral head with a tendon is expected to have a strain-shielding effect on tendon strain as was found in a previous study 2. On this basis, it was expected that the contact between the infraspinatus tendon and the humeral head would be greatest at 30° internal rotation and least at 30° external rotation resulting in lower and higher strains at these angles respectively. Interestingly, the effect of rotation was only significant in the supraspinatus tendon at the highest load evaluated for the partial-thickness, but not the full-thickness tear condition. It is likely that rotation increases the non-homogeneous distribution of strain in the supraspinatus tendon, causing a decrease in some regions and an increase in others in comparison to the intact tendon case that becomes extreme and significant only at the highest load evaluated. In addition, at the full-thickness tear case, the size of the small region (33%) of the supraspinatus tendon remaining intact is less susceptible to the large strain variability that accompanies rotation, thus becoming unaffected by rotation. For instance, it is likely that larger tear sizes that compromise the anterior portion of the supraspinatus tendon, eliminate the effect of rotation on the posterior region of the supraspinatus tendon by disabling the anterior portion to further load (possibly at external rotation) or alleviating load (possibly at internal rotation) from the posterior region. It was also expected that changes in supraspinatus tendon strain would parallel those observed in the infraspinatus tendon due to the mechanical interaction between the two tendons. It is possible that high strains experienced by the supraspinatus tendon in internal rotation at 90N would have caused even greater strains in the infraspinatus tendon if there was no strain shielding effect by the humerus. In the infraspinatus tendon, results imply that the anatomical position of the two tendons (unique to each rotation angle) causes a specific direction of supraspinatus tendon loading on infraspinatus tendon strain that is responsible for the observed effect of rotation. It is also likely that despite the high strains experienced by the supraspinatus tendon at 30° internal rotation, the effect of partial-thickness tear size in the infraspinatus tendon may have been masked as a result of humeral head strain-shielding.
In this study, the effect of anterior edge, bursal-side partial-thickness supraspinatus tendon tears was evaluated. Caution should be taken in extrapolating results from this study to other types of partial-thickness tears. We expect that the ability of the supraspinatus tendon to interact with the infraspinatus tendon depends on the type and location of the tear. Minagawa et al described the anatomy of the rotator cuff and noted that the supraspinatus and the infraspinatus tendons interdigitate in the posterior half of the supraspinatus tendon.15 In addition, Clark et al found that the confluent region between the supraspinatus and infraspinatus tendons occurs in the anatomic third layer through the thickness of the supraspinatus tendon.5 This implies that in this study, the confluent region between the two tendons was completely intact through the full width of the tendon for the intact and 33% partial-thickness tear. For the larger 66% partial-thickness and 100% full-thickness tears, the confluent region was still completely preserved in the posterior 33% width of the tendon, thereby preserving the interaction between the two tendons. We expect that tears that compromise the entire confluent region, such as posterior side supraspinatus tears or tears that affect the third layer through the thickness of the tendon, may cause a disruption in the interaction between the supraspinatus and infraspinatus tendons causing minimal changes in infraspinatus tendon strain with significant increases in supraspinatus tendon loading or tear size. Therefore, the location of a supraspinatus tendon tear is expected to impact the interaction between it and the infraspinatus tendon.
Conclusion
This study demonstrates that the interaction between the infraspinatus tendon and the strained supraspinatus tendon causes increases in infraspinatus tendon strain in the presence of anterior edge, bursal-side partial-thickness supraspinatus tendon tears. We have also shown that increasing supraspinatus tendon loading for the evaluated tear and joint position caused a mechanical interaction between the two tendons as indicated by the increase in infraspinatus tendon strain paralleling the increase in supraspinatus tendon strain. A possible effect of this interaction may be that the mechanical interaction between these two tendons protects the injured supraspinatus tendon from further injury. Alternatively, the mechanical interaction between the supraspinatus and infraspinatus tendons may contribute to the observed fatty infiltration in the infraspinatus tendon that accompanies intact infraspinatus tendons and torn supraspinatus tendons.7 Finally, we have shown that rotation angle has no impact on normalized average minimum principal strain in both tendons, but impacts normalized average maximum principal strain in the supraspinatus tendon at the highest load. Since the mechanical interaction between the two tendons may shield the torn supraspinatus tendon from further injury, but in turn may also cause chronic detrimental changes in the supraspinatus tendon, it is possible that in managing rotator cuff tears in the clinical setting it may be advantageous to control the amount of interaction between the two tendons by controlling joint rotation or loading.
Supplementary Material
Acknowledgments
Funding: This study was supported by a grant from the NIH/NIAMS (AR050176) and the NIH/NIAMS supported Penn Center for Musculoskeletal Disorders (AR050950)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclaimers: None
IRB exemption was obtained for this study. IRB exemption was authorized by 45 CFR 46.101, category 4. Expiration date: 9/19/10
Contributor Information
Nelly Andarawis-Puri, McKay Orthopaedic Research Laboratory, University of Pennsylvania.
Andrew F. Kuntz, McKay Orthopaedic Research Laboratory, University of Pennsylvania.
Soung-Yon Kim, Orthopaedic Surgery, Division of Shoulder and Elbow Surgery, Kangwon National University Hospital, South Korea.
Louis J. Soslowsky, McKay Orthopaedic Research Laboratory, University of Pennsylvania, 424 Stemmler Hall, Philadelphia, PA, Phone: 215-898-8653; Facsimile: 215-573-2133
References
- 1.Andarawis-Puri NA, Ricchetti ET, Soslowsky LJ. Interaction Between the Supraspinatus and Infraspinatus tendons: Effect of Anterior Supraspinatus Tendon Full-Thickness Tear on Infraspinatus Tendon Strain. Am J Sports Med. 2009 doi: 10.1177/0363546509334222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bey MJ, Ramsey ML, Soslowsky LJ. Intratendinous strain fields of the supraspinatus tendon: effect of a surgically created articular-surface rotator cuff tear. J Shoulder Elbow Surg. 2002;11:562–569. doi: 10.1067/mse.2002.126767. [DOI] [PubMed] [Google Scholar]
- 3.Bey MJ, Song HK, Wehrli FW, Soslowsky LJ. A noncontact, nondestructive method for quantifying intratissue deformations and strains. J Biomech Eng. 2002;124:253–258. doi: 10.1115/1.1449917. [DOI] [PubMed] [Google Scholar]
- 4.Breazeale NM, Craig EV. Partial-thickness rotator cuff tears. Pathogenesis and treatment. Orthop Clin North Am. 1997;28:145–155. doi: 10.1016/s0030-5898(05)70275-3. [DOI] [PubMed] [Google Scholar]
- 5.Clark JM, Harryman DT., 2nd Tendons, ligaments, and capsule of the rotator cuff. Gross and microscopic anatomy. J Bone Joint Surg Am. 1992;74:713–725. [PubMed] [Google Scholar]
- 6.Flatow EL, Altchek DW, Gartsman GM, Iannotti JP, Miniaci A, Pollock RG, et al. The rotator cuff. Commentary. Orthop Clin North Am. 1997;28:277–294. doi: 10.1016/s0030-5898(05)70286-8. [DOI] [PubMed] [Google Scholar]
- 7.Fuchs B, Gilbart MK, Hodler J, Gerber C. Clinical and structural results of open repair of an isolated one-tendon tear of the rotator cuff. J Bone Joint Surg Am. 2006;88:309–316. doi: 10.2106/JBJS.E.00117. [DOI] [PubMed] [Google Scholar]
- 8.Fukuda H. Partial-thickness rotator cuff tears: a modern view on Codman's classic. J Shoulder Elbow Surg. 2000;9:163–168. [PubMed] [Google Scholar]
- 9.Fukuda H, Hamada K, Nakajima T, Tomonaga A. Pathology and pathogenesis of the intratendinous tearing of the rotator cuff viewed from en bloc histologic sections. Clin Orthop Relat Res. 1994:60–67. [PubMed] [Google Scholar]
- 10.Fukuda H, Hamada K, Yamanaka K. Pathology and pathogenesis of bursal-side rotator cuff tears viewed from en bloc histologic sections. Clin Orthop Relat Res. 1990:75–80. [PubMed] [Google Scholar]
- 11.Goutallier D, Postel JM, Gleyze P, Leguilloux P, Van Driessche S. Influence of cuff muscle fatty degeneration on anatomic and functional outcomes after simple suture of full-thickness tears. J Shoulder Elbow Surg. 2003;12:550–554. doi: 10.1016/s1058-2746(03)00211-8. [DOI] [PubMed] [Google Scholar]
- 12.Halder A, Zobitz ME, Schultz F, An KN. Mechanical properties of the posterior rotator cuff. Clin Biomech (Bristol, Avon) 2000;15:456–462. doi: 10.1016/s0268-0033(99)00095-9. [DOI] [PubMed] [Google Scholar]
- 13.Lichtenberg S, Liem D, Magosch P, Habermeyer P. Influence of tendon healing after arthroscopic rotator cuff repair on clinical outcome using single-row Mason-Allen suture technique: a prospective, MRI controlled study. Knee Surg Sports Traumatol Arthrosc. 2006;14:1200–1206. doi: 10.1007/s00167-006-0132-8. [DOI] [PubMed] [Google Scholar]
- 14.Matava MJ, Purcell DB, Rudzki JR. Partial-thickness rotator cuff tears. Am J Sports Med. 2005;33:1405–1417. doi: 10.1177/0363546505280213. [DOI] [PubMed] [Google Scholar]
- 15.Minagawa H, Itoi E, Konno N, Kido T, Sano A, Urayama M, et al. Humeral attachment of the supraspinatus and infraspinatus tendons: an anatomic study. Arthroscopy. 1998;14:302–306. doi: 10.1016/s0749-8063(98)70147-1. [DOI] [PubMed] [Google Scholar]
- 16.Nicholson GP. Arthroscopic acromioplasty: a comparison between workers' compensation and non-workers' compensation populations. J Bone Joint Surg Am. 2003;85-A:682–689. [PubMed] [Google Scholar]
- 17.Peterson CA, 2nd, Altchek DW. Arthroscopic treatment of rotator cuff disorders. Clin Sports Med. 1996;15:715–736. [PubMed] [Google Scholar]
- 18.Reilly P, Amis AA, Wallace AL, Emery RJ. Supraspinatus tears: propagation and strain alteration. J Shoulder Elbow Surg. 2003;12:134–138. doi: 10.1067/mse.2003.7. [DOI] [PubMed] [Google Scholar]
- 19.Zumstein MA, Jost B, Hempel J, Hodler J, Gerber C. The clinical and structural long-term results of open repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2008;90:2423–2431. doi: 10.2106/JBJS.G.00677. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.