Abstract
Chronic pain is a pervasive health care issue affecting over 50 million Americans and costing more than $100 billion dollars annually in lost productivity and health care costs. As a financially and emotionally taxing condition, the families and friends of people with chronic pain, as well as society at large, are affected. Current theory supports the role of biological, psychological, and environmental factors in the etiology, exacerbation, and maintenance of chronic pain. Recently, the specific role of pain-related fear in pain experience has received increasing attention. This article summarizes current understanding of the role of pain-related fear in the onset of acute pain incidents, the transition of acute pain to chronic, and the pain severity and disability of patients with ongoing chronic pain conditions. Treatments demonstrated to reduce pain-related fear are presented, evidence demonstrating their efficacy at reducing disability and pain severity are summarized, and recent criticisms of the fear-avoidance model and future directions are considered.
Keywords: Fear, Pain, Fear-avoidance, Catastrophizing
Introduction
Overwhelming evidence suggests a complex combination of psychological, cognitive, environmental, and neurophysiological factors in the etiology and maintenance of chronic pain [1]. The inclusion of psychosocial factors in the conceptual framework of pain theory helps to explain the limited association between organic pathology and pain severity. Over the past decade, the specific role of fear in the onset, development, and maintenance of pain has received increasing attention [2]. Investigators have suggested that fear of pain and activity, driven by the anticipation of pain and increased injury—rather than the noxious sensory stimuli associated with pain itself—produces strong negative reinforcement for the persistence of avoidance behavior, resulting in putative functional disability in people with persistent pain [3, 4]. Although avoidance behavior may be reinforcing in the short-term through the reduction of distress associated with noxious stimulation [5], if allowed to persist, it may become a maladaptive response leading to increased fear, limitation of activity, and other physical and psychological consequences that contribute to disability and persistence of pain.
Negative appraisals of pain, including catastrophic interpretations such as the belief that the presence of or onset of pain connotes pathology and therefore harm, are thought to contribute to the development of pain-related fear. The role of catastrophizing and the resulting pain-related fear have been articulated in “fear-avoidance” models of chronic pain [2, 3, 6, 7]. Since initially formulated, a substantial accumulation of evidence confirms that fear-avoidance beliefs are associated with disability and impaired physical performance in chronic pain [8, 9]. In addition, fear-avoidance beliefs have been shown to relate to the future onset of (back) pain in the general population [10], and may be predictive of pain persistence, disability, and long-term sick leave in patients with acute pain-related injuries [11].
The purpose of this article is to provide an understanding of the role of fear and negative appraisals in the experience of pain. Following an introduction of the core constructs of the fear-avoidance model and a discussion of the common methods for assessing these constructs, we provide an illustrative summary of evidence for the 1) implication of fear and fear-avoidance as related to constructs in the onset of new acute pain incidents; 2) transition of pain from acute to chronic; and 3) severity and exacerbation of pain in a chronic pain condition. Frequently used measures to assess pain-related fear are presented. Treatments targeting fear-related beliefs are presented, and evidence supporting these approaches is reviewed. Finally, discussion involving recent criticisms and suggestions for future research are provided in order to advance our understanding of the role of fear in pain. Specifically, the following questions are addressed:
What role does fear play in the onset of an acute pain incident, the transition of an acute painful episode to a chronic condition, and the aggravation of an already chronic pain condition?
How are beliefs about pain-related fear assessed?
How do treatments address fear of pain, and how effective are they?
What are the limitations of the fear-avoidance model of chronic pain?
Fear-Avoidance Model
Early fear-avoidance models [3, 6, 12] conceptualized the role of pain and avoidance behavior as distinct from the sensory component of pain. Mainly, they proposed that avoidance of pain was not directly related to current pain severity, but rather was the result of specific expectancies, beliefs, and interpretations surrounding the perception of pain. These models stressed the reciprocal interaction between affective states and cognitive-interpretive processes—the idea that thinking affects mood and mood influences appraisals, thereby affecting the experience of pain.
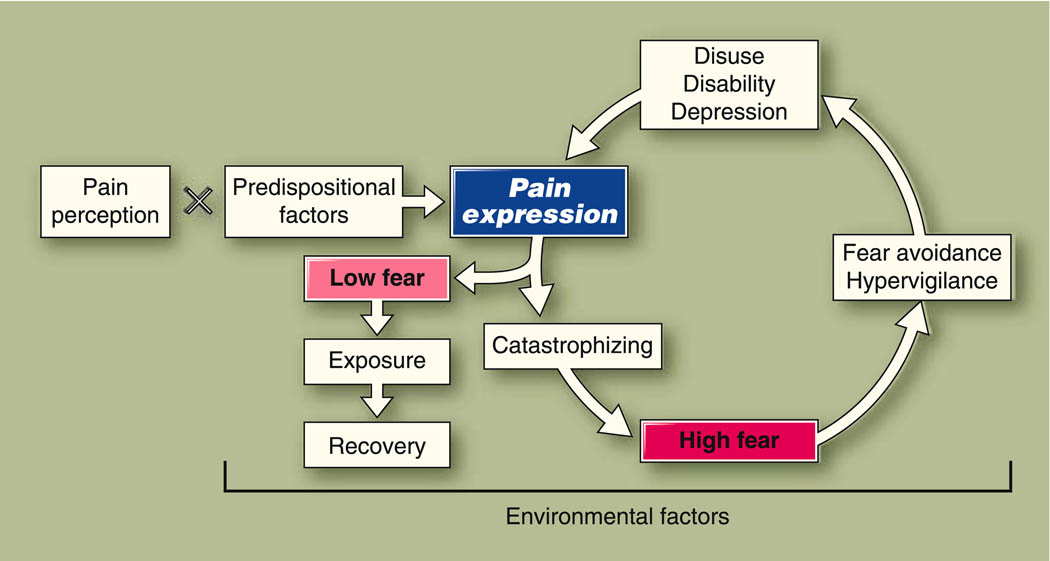
Contemporary fear-avoidance models [2, 4, 13] have expanded on these earlier conceptualizations through expansion of the cognitive and affective constructs thought to be involved in pain perception and experience. Each model varies slightly with regard to the constructs that are emphasized; however, all share the following general tenets (Fig. 1):
When pain is perceived following injury, an individual’s idiosyncratic beliefs will determine the extent to which pain is interpreted as threatening or harmful.
An extremely negative (ie, “catastrophic”) interpretation of pain induces physiological (arousal), cognitive, and behavioral (avoidance) fear responses.
The cognitive shift that takes place during fear enhances threat perception (eg, by narrowing attention), further feeding the catastrophic appraisal of pain, avoidance of activity, and disability [2].
Fig. 1.
Fear-avoidance model of pain. Pain perceptions (eg, a physical injury, migraine headache) interact with predispositional factors (eg, anxiety sensitivity, genetic risk factors) to result in individual pain expression. Pain expression is also influenced by environmental factors (eg, disability compensation system, social support). People may have low pain-related fear, such that they do not stop all activities and adopt the belief that activity will always result in pain or further injury. In this case, people will continue activities, have confirming experiences that pain does not always equal harm, and maintain their quality of life. Alternately, people may catastrophize about the causes surrounding their pain, and have high pain-related fear. This begins the negative feedback cycle of pain: fear-avoidance and cessation of activity, leading to disuse, disability, and depression
Prior to reviewing evidence supporting the role of fear in chronic pain, a summary of key constructs implicating the contemporary fear-avoidance models will be provided.
Catastrophizing
Pain catastrophizing can be defined as an exaggerated negative orientation toward actual or anticipated pain experiences. Substantial debate has surrounded the specific nature of catastrophizing as a psychological construct; however, current conceptualizations most often describe it in terms of appraisal or as a set of maladaptive beliefs [14]. Current fear-avoidance models propose that catastrophizing beliefs precipitate pain-related fear, leading to avoidance, followed by disuse, disability, and depression.
Pain-Related Fear
Fear is defined as an emotional reaction to a specific, identifiable, and immediate threat, such as a dangerous animal or traumatic event [15]. Pain-related fear evolves as a result of catastrophic beliefs and negative interpretations that pain is equivalent to harm. Pain-related fear may include fear of movement, activity, or work.
Instruments Used to Measure Pain-Related Fear and Catastrophizing
Pain-related fear and negative appraisals such as catastrophizing are most commonly measured through self-reports provided by patients regarding their current beliefs and emotional state. However, these methods have received criticism due to the assumption that individuals are cognizant of psychological constructs such as pain-related fear and catastrophizing [16]. Despite these limitations, the availability and ease of using such instruments proliferates their use. The four most commonly used measures in fear-avoidance research are summarized in Table 1.
Table 1.
Instruments used to asses fear-avoidance
|
Fear-Avoidance Beliefs Questionnaire (FABQ; [12]): Consists of 16 items, which may be divided into 2 subscales: 1) beliefs about harm from physical activity; and 2) beliefs about harm from work specific activities. Internal consistency excellent in both chronic (α=0.82) and acute (α= 0.74) pain populations. Has acceptable test re-test reliability at 0.74 [12]. |
|
Fear of Pain Questionnaire (FPQ; [51]): Designed to be utilized in both clinical and nonclinical populations within a variety of contexts. The questionnaire consists of 30 items, resulting in a total score and 3 subscales: 1) fear of severe pain; 2) fear of minor pain; and 3) dental/medical pain. Has good internal consistency (α=0.86–0.95) in both clinical and nonclinical populations, and has been demonstrated to have good test re- test reliability within a 3-week time-frame (0.69–0.76 for various subscales). |
|
Tampa Scale of Kinesphobia (TSK): Developed by Kori and colleagues to assess excessive fear of physical activity from perceived threat of pain [52]. The original measure consists of 17 items. Has been demonstrated to have good internal consistency (α=0.68–0.80) [4, 53] and test re-test reliability (stability) up to 50 days (intra-class correlation coefficient of 0.72; [54]). |
|
Pain Catastrophizing Scale (PCS; [55]): Designed to measure individuals’ tendencies to increase their focus on pain-related thoughts and thereby exaggerate the value of painful stimuli. Moderately correlated with other pain-related affective constructs such as depression and anxiety (ranging from 0.32–0.46). This suggests that catastrophizing, although related to affective constructs, is a unique construct. In a study evaluating the test re- test reliability over a 50 day period, the PCS had an intra-class correlation coefficient of 0.73 [54]. |
Evidence for the Role of Fear in Pain Experience
Previous pain encounters, and environmental and social contexts such as growing up with a parent out of work due to a chronic pain condition, may affect fear-avoidance beliefs in an uninjured population through observation and learning. These increased pain-related fear beliefs may heighten individuals’ attention to ambiguous physical sensations in themselves, thereby increasing the risk of a new acute pain episode [17]. Although limited, there is evidence consistent with this hypothesis. Linton et al. [18] demonstrated an increased risk for future low back pain among individuals that catastrophized about pain in a pain-free population. This finding has been replicated in prospective cohort studies for both musculoskeletal and back pain conditions [10, 19]. An additional method for assessing the degree to which catastrophizing and fear-avoidance beliefs may contribute to acute pain has been to assess the degree that these beliefs predict postoperative pain following elective surgeries. Presurgical pain catastrophizing has been shown to be a significant predictor of both postoperative pain and longer recovery time [20].
Research suggests that pain-related fear serves as a risk factor for the development and persistence of chronic pain and long-term sick leave following an acute pain episode [11]. In a recent example, Nieto et al. [21] evaluated the role of fear of movement and pain catastrophizing in predicting pain-related disability and depression in patients with subacute whiplash injuries sustained following motor vehicle collisions. Even after controlling for pain characteristics, both catastrophizing and fear of movement were significant predictors of both disability and depression.
Escape and avoidance of activities perceived to be associated with pain often prevent people with chronic pain from the realization that these activities may not actually lead to increased pain. Because they are not directly exposed to the activity, they obtain no feedback disconfirming their maladaptive beliefs, thereby promoting disuse and disability. In addition, people with chronic pain with high fear-avoidance may selectively attend to possible sources of threat (eg, potential pain signals) and become hypervigilant to any pain associated with movement and activity [22], assiduously avoiding these activities. Over time, more and more activities may be avoided as people begin to generalize their beliefs. The result of inactivity may promote physical deconditioning. As a consequence, patients place significant limitation and avoidance among more exercises that they anticipate will initiate or aggravate pain. Thus begins the creation and perpetuation of a dysfunctional cycle. The role of this pain-related fear in the maintenance of ongoing chronic pain conditions is evident from cross-sectional studies evaluating disability and measures of fear-avoidance.
A systematic review of the literature on psychological risk factors in back and neck pain indicated evidence for a significant association between fear-avoidance beliefs and increased pain and disability [23]. A recent prospective study evaluating the prevalence of sickness absence as a result of low back pain identified fear-avoidance beliefs as a significant predictor of number of sick days, even after controlling for work environmental factors [24•]. The evidence for catastrophizing in chronic pain adjustment is particularly strong with regard to specific negative appraisals [25].
Evidence for Individual Difference Variables as Risk Factors for Pain-Related Fear
Trait (ie, stable) characteristics and individual difference variables demonstrating the greatest potential as vulnerability factors include anxiety sensitivity, illness and injury sensitivity, and more recently, genetic variations. Anxiety sensitivity (AS) is defined as the fear of anxiety-related sensations, and is conceived as a partly heritable enduring personality characteristic [26]. A recent functional magnetic imaging study demonstrated that AS, in contrast to pain-related fear beliefs, was associated with activation of the medial prefrontal region, which is associated with self-focused attention. Pain-related fear beliefs were associated with activation of the ventral lateral frontal region, which is involved in response regulation, and anterior and posterior cingulate regions, which are associated with monitoring and evaluation of affective responses [27]. Results from this study suggest that AS is a unique construct within the fear-avoidance model. Individuals with high AS interpret unpleasant physical sensations (eg, rapid heart beating, feeling faint) as signals of danger more often than individuals with low AS.
AS correlates with measures of fear-avoidance and has been shown to be associated with distress, analgesic use, and physical and social functioning in patients across a wide range of different pain-related conditions [2]. Moreover, path analyses and mediation models suggest that AS magnified fear-avoidance beliefs and the negative interpretation of bodily sensations, which in turn leads to enhanced pain experience and pain avoidance [28].
Researchers have begun to consider illness and injury sensitivity as another vulnerability factor for fear-avoidance [29]. Illness and injury sensitivity are conceptually more strongly related to the content of fear-avoidance beliefs of chronic pain patients than that of AS. This can be illustrated by the items of inventories used to measure AS and illness or injury sensitivity, mainly the Anxiety Sensitivity Index (ASI) and Illness Sensitivity Index (ISI) [30]. The ASI contains items with very specific applications to panic symptoms (eg, fear of heart beating fast), whereas the ISI contains items reflecting worried thought patterns regarding one’s future physical condition (eg, the anticipation of an injury). Recent studies in healthy volunteers demonstrated that illness or injury sensitivity may be a more specific vulnerability factor for maladaptive pain responses than AS [29]. In a cross-sectional study, illness and injury sensitivity, AS, fear of negative evaluation, and trait anxiety were tested for their independent contributions to pain catastrophizing and fear-avoidance beliefs. Illness or injury sensitivity appeared to be the single best predictor of pain catastrophizing, pain-related fear, and pain avoidance; however, more research is needed to substantiate its role in chronic pain adjustment.
There is accumulating evidence for genetic associations implicated in fear-recognition, harm-avoidance, and pain-related anxiety. In a recent study evaluating genetic variations associated with fear of dental pain, participants with the melanocortin-1 receptor (MC1R) gene variant, responsible for the expression of red hair color, were more than twice as likely to avoid dental care as were participants with no MC1R gene [31]. In addition, Blaya et al. [32] provide preliminary evidence for the association between variants in the X chromosome gene EF-hand domain containing 2 (EFHC2) and the processing of fear-recognition and harm-avoidance. As techniques for extracting, analyzing, and interpreting genetic variations advance and become more widely available, the complex interaction between genetic make-up and the environment in the experience of pain will become better delineated.
Evidence for the Effect of Health Care Provider Beliefs on Pain-Related Fear
Health practitioners sometimes hold personal beliefs that may indirectly encourage fear-avoidance in their patients [33]. Fear-avoidance beliefs of health care providers were found to be related to treatment behavior and recommendations for patients’ engagement of physical activities [34]. The beliefs of patients and health care providers may interact with each other in a mutually reinforcing way, because a patient’s beliefs may guide the choice of which or which type of health care provider is visited [35], and therefore what treatment they receive [36].
Treatments Targeting Fear-Related Constructs
Because catastrophizing and fear-avoidance beliefs appear to play such a prominent role in maladaptive responses to pain and disability, it is of vital importance that these negative and maladaptive beliefs are addressed. Educational interventions in a primary care setting addressing fear-avoidance beliefs and the encouragement of patients to stay active have been found to reduce disability in back pain patients [37]. In addition, a population-based media campaign was shown to be effective in changing beliefs about back pain and reducing disability and worker’s compensation costs related to back pain [38]. The improvement in population beliefs about back pain were sustained until 3 years after cessation of the campaign [39].
Education alone may not, however, be sufficient for reducing fear-avoidance beliefs in patients with high levels of catastrophizing and fear-avoidance beliefs [40]. These patients may require a more tailored and intensive treatment approach, such as graded exposure to disconfirm their fear-avoidance beliefs [9]. In graded exposure therapy, a hierarchy of fearful activities is established, and patients are encouraged to engage in a moderately feared activity until disconfirmation of harm beliefs for this particular activity has occurred. Patients then proceed to the next item in the hierarchy until they are able to perform activities identified as most feared. During the performance of these activities, behavioral experiments are used to challenge the catastrophic interpretations of the consequences of the activity. Graded exposure appears to be a very effective treatment for altering fear-avoidance beliefs and catastrophizing, and for reducing pain and disability in chronic pain patients characterized by high levels of fear-avoidance [9, 41]. Several studies have demonstrated the potential for cognitive-behavior therapy (CBT) to cause a reduction in fear-avoidance beliefs, and that treatment success may be mediated by changes in fear-avoidance beliefs [42].
Although graded exposure is the most specific treatment for reducing fear-avoidance beliefs, most rehabilitation programs for chronic pain patients contain at least some components that are likely to be effective at reducing fear-avoidance beliefs (eg, education, physical exercise, challenging negative cognitions) [43]. However, often these programs do not directly emphasize fear and avoidance of activities. This is particularly important in rehabilitation for chronic pain patients due to physical exercise being a central component to most programs. Patients fear of pain and harm will likely serve as impediments to adherence to exercise regimens, leading to premature termination of treatment. Because fear-avoidance plays an important role, particularly among individuals with musculoskeletal disorders, it would seem reasonable to assess patients’ beliefs using one or more of the instruments described above. For those patients who appear to have high fears of activity, it may be appropriate to address these activities specifically— both by providing information and by exposing them to feared and avoided activities—allowing them to obtain corrective feedback disconfirming their beliefs. Graded activity that gradually allows patients to confront feared activities without the anticipated dire consequences should be a powerful way to modify maladaptive and inaccurate beliefs. Increasing activity in manageable increments will increase patients’ self-confidence in their abilities, in addition to their willingness to progress and undertake more strenuous activities.
In sum, given evidence of the significant role fear-avoidance beliefs play in pain experience, the following treatment steps are recommended when a patient presents with a chronic pain condition:
Step 1: Assess fear beliefs in general or use one of the standardized instruments (see Table 1).
Step 2: Address fears through reassurance that “pain does not equal harm”. For low fear patients, education provided by a primary care physician may be adequate; for high fear patients, referral for CBT may be indicated.
Step 3: Help patients set realistic expectations (individualized to the patient).
Step 4: Gradually increase activities (individualized based on their lifestyle) starting at a level that is appropriate and acceptable to the patient. Consider the use of graphs so that patients can monitor their activities and progress toward goals. For low-fear patients, self-monitored gradual increase in activity may be adequate; for high-fear patients, therapist (physical therapist, psychologist) guided and monitored graded exposure of feared and avoided activity may be indicated.
Step 5: Encourage patient self-monitoring so as to stay on target; provide a form of reinforcement to encourage continuation and observe progress; encourage self-monitoring as a way to increase perceptions of self-efficacy and decrease catastrophizing beliefs.
Limitations of the Fear-Avoidance Model and Future Directions
One criticism of the fear-avoidance model involves the conceptualization and measurement of the constructs implicated in the model. Despite evidence that fear and anxiety are unique constructs with fear being a proximate emotion and anxiety anticipatory, these terms are often used interchangeably in the literature, complicating the interpretation of findings [16]. Whether some of the measures used to assess fear-avoidance beliefs actually measure what they purport to measure has also been brought into question [44]. Moreover, several measures appear abstract and not sufficiently related to activities that patients with different types of pain are likely to avoid. For example, a patient whose pain is located in the lower back might not avoid activities that involve upper arm movements. Conversely, a patient with carpel tunnel syndrome might avoid use of the hands and upper arms but not activities that involve lower limbs, such as walking. Thus, it may be appropriate to develop measures that are more specific, enhancing the predictive value as compared to more generally based measurement tools [45].
One of the strengths of the fear-avoidance model of pain is the clear testability and directionality of the model. Negative appraisals of pain and catastrophizing are conceptualized as precipitating pain-related fear, and pain-related fear mediates the relationship between injury and disability. However, a vast majority of the evidence evaluating the role of pain-related fear and catastrophizing in chronic pain has come from cross-sectional studies that do not allow for directional conclusions. Recently, however, a well-designed prospective sequential analysis of the fear-avoidance model of pain was published [46••]. Participants with musculoskeletal injuries participating in a 10-week disability management intervention completed catastrophizing and fear-avoidance measures pre-, mid-, and post-treatment. The authors hypothesized that early changes in catastrophizing (mid scores-pre scores) would predict late changes in fear of movement (post scores-mid scores). Although overall changes in catastrophizing and fear of movement were predictive of return to work, early changes in catastrophizing were not associated with late changes in fear of movement. Methodological issues may account for lack of relationship between early changes in catastrophizing and late changes in pain-related fear; however, these results challenge the notion that catastrophizing clearly precipitates pain-related fear. It is more likely that the model is a more complex dynamic, such that there is an interactive process between pain-related fear, catastrophizing, and negative appraisals.
As described by the founders of the contemporary fear-avoidance models in a letter to the editor written in response to the article by Wideman et al. [46••], Vlaeyen, Crombez, and Linton [47] state that the “fear avoidance model was never meant to be a final model to be unconditionally embraced or falsified. Rather, the fear avoidance model is a theory-based heuristic in search for a better understanding of the dynamics of pain disability‥‥ We are pleased to see that the model is evolving, and growing steadily out of its infancy.”
The greatest amount of research evaluating the fear-avoidance model has focused on patients with chronic back pain and patients who are known to have undergone a physical trauma (eg, motor vehicle collision). In these instances, there is often a specific event that appears instrumental in the pain onset—injury. Patients with these types of pain are likely to have specific activities they attempt to avoid as they are related to their injury, and if performed, might be expected to cause further tissue damage. There are many pain syndromes for which there is often no identifiable physical trauma (eg, fibromyalgia, migraine, painful diabetic neuropathy). Some preliminary studies support the role of the fear-avoidance model for conditions that do not involve trauma [48]. In these examples, fear of injury following specific activities may be less obvious. It may be fear of pain rather than injury that precipitates the avoidance of activity. There is some evidence that patients’ interpretation of the cause of their pain, particularly its association with a physical trauma, plays an important role in the perceptions of their physical limitations [49]. Research is needed to investigate potential differences between fear of pain and fear of injury, as these may be addressed differently within treatment.
Much as the gate-control theory [50] provided a physiological framework for understanding how peripheral excitation and central inhibition culminate in the physiological expression of either increased or decreased pain, the fear-avoidance model has provided a much needed framework for understanding how complex psychological processes, including negative appraisals and fear, culminate in the representation and expression of pain in individuals. Each model has stimulated research that has improved our understanding of the underlying mechanisms, thereby improving our methods for treating chronic pain.
Conclusions
Given the extensive body of literature summarized above, it is apparent that fear-induced avoidance of activities and escape from activities play an important role in persistence and aggravation of pain, making anticipatory anxiety an important contribution to disability. How patients interpret their plight, anticipation of the future, and appraisals of the impact of their behavior on pain need to be considered, along with neurophysiological factors when developing an optimal treatment plan. Careful assessment and matching of treatment to patients’ attitudes and beliefs should contribute to improved outcome. Thus far, there appears to be no question that awareness and treatment of fear and negative appraisals regarding pain are important factors to consider when treating patients with both acute and chronic pain.
Acknowledgments
The authors would like to thank Christina Kemp for her insightful editorial comments on an earlier draft of this article, and to Deven Wilson for assistance in creation of Fig. 1.
Footnotes
Disclosure Dr. Dennis C. Turk, in the past 12 months, has served as a consultant to Eli Lily, Forrest Pharmaceuticals, Johnson & Johnson, Philips Respironics, Shire, and SK LifeScience; he has also received grants from Endo Pharmaceuticals and Johnson & Johnson. No other potential conflicts of interest relevant to this article were reported.
Contributor Information
Dennis C. Turk, Email: turkdc@u.washington.edu, Department of Anesthesiology & Pain Medicine, University of Washington, Box 356540, Seattle, WA 98195, USA.
Hilary D. Wilson, Email: hdwilson@u.washington.edu, Department of Anesthesiology & Pain Medicine, University of Washington, Box 356540, Seattle, WA 98195, USA.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.Gatchel RJ, Peng YB, Peters ML, et al. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull. 2007;133:581–624. doi: 10.1037/0033-2909.133.4.581. [DOI] [PubMed] [Google Scholar]
- 2.Asmundson G, Norton P, Vlaeyen J. Fear-avoidance models of chronic pain: an overview. In: Asmundson G, Vlaeyen J, Crombez G, editors. Understanding and Treating Fear of Pain. Oxford: Oxford University Press; 2004. pp. 3–24. [Google Scholar]
- 3.Lethem J, Slade PD, Troup JD, Bentley G. Outline of a fear-avoidance model of exaggerated pain perception—I. Behav Res Ther. 1983;21:401–408. doi: 10.1016/0005-7967(83)90009-8. [DOI] [PubMed] [Google Scholar]
- 4.Vlaeyen JW, Kole-Snijders AM, Boeren RG, van Eek H. Fear of movement/(re)injury in chronic low back pain and its relation to behavioral performance. Pain. 1995;62:363–372. doi: 10.1016/0304-3959(94)00279-N. [DOI] [PubMed] [Google Scholar]
- 5.McCracken LM, Gross RT, Sorg PJ, Edmands TA. Prediction of pain in patients with chronic low back pain: effects of inaccurate prediction and pain-related anxiety. Behav Res Ther. 1993;31:647–652. doi: 10.1016/0005-7967(93)90117-d. [DOI] [PubMed] [Google Scholar]
- 6.Philips HC. Avoidance behaviour and its role in sustaining chronic pain. Behav Res Ther. 1987;25:273–279. doi: 10.1016/0005-7967(87)90005-2. [DOI] [PubMed] [Google Scholar]
- 7.Vlaeyen JW, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85:317–332. doi: 10.1016/S0304-3959(99)00242-0. [DOI] [PubMed] [Google Scholar]
- 8.Linton SJ. A review of psychological risk factors in back and neck pain. Spine. 2000;25:1148–1156. doi: 10.1097/00007632-200005010-00017. [DOI] [PubMed] [Google Scholar]
- 9.Vlaeyen JW, De Jong JR, Onghena P, et al. Can pain-related fear be reduced? The application of cognitive-behavioural exposure in vivo. Pain Res Manag. 2002;7:144–153. doi: 10.1155/2002/493463. [DOI] [PubMed] [Google Scholar]
- 10.Picavet HS, Vlaeyen JW, Schouten JS. Pain catastrophizing and kinesiophobia: predictors of chronic low back pain. Am J Epidemiol. 2002;156:1028–1034. doi: 10.1093/aje/kwf136. [DOI] [PubMed] [Google Scholar]
- 11.Boersma K, Linton SJ. Screening to identify patients at risk: profiles of psychological risk factors for early intervention. Clin J Pain. 2005;21:38–43. doi: 10.1097/00002508-200501000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Waddell G, Newton M, Henderson I, et al. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52:157–168. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- 13.McCracken LM, Zayfert C, Gross RT. The Pain Anxiety Symptoms Scale: development and validation of a scale to measure fear of pain. Pain. 1992;50:67–73. doi: 10.1016/0304-3959(92)90113-P. [DOI] [PubMed] [Google Scholar]
- 14.Severeijns R, Vlaeyen JW, van den Hout MA. Do we need a communal coping model of pain catastrophizing? An alternative explanation. Pain. 2004;111:226–229. doi: 10.1016/j.pain.2004.07.024. [DOI] [PubMed] [Google Scholar]
- 15.Rachman S. Anxiety. Hove: Psychological Press; 1998. [Google Scholar]
- 16.McNeil DW, Vowles KE. Assessment of fear and anxiety associated with pain: conceptualization, methods, and measures. In: Asmundson G, Vlaeyen J, Crombez G, editors. Understanding and Treating Fear of Pain. Oxford: Oxford University Press; 2004. pp. 189–211. [Google Scholar]
- 17.Arntz A, Claassens L. The meaning of pain influences its experienced intensity. Pain. 2004;109:20–25. doi: 10.1016/j.pain.2003.12.030. [DOI] [PubMed] [Google Scholar]
- 18.Linton S, Buer N, Vlaeyen J, Hellsing AL. Are fear-avoidance beliefs related to the inception of an episode of back pain? A prospective study. Psychol Health. 1999;14:1051–1059. doi: 10.1080/08870440008407366. [DOI] [PubMed] [Google Scholar]
- 19.Severeijns R, Vlaeyen JW, van den Hout MA, Picavet HS. Pain catastrophizing and consequences of musculoskeletal pain: a prospective study in the Dutch community. J Pain. 2005;6:125–132. doi: 10.1016/j.jpain.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 20.Kendell K, Saxby B, Farrow M, Naisby C. Psychological factors associated with short-term recovery from total knee replacement. Br J Health Psychol. 2001;6:41–52. doi: 10.1348/135910701169043. [DOI] [PubMed] [Google Scholar]
- 21.Nieto R, Miró J, Huguet A. The fear-avoidance model in whiplash injuries. Eur J Pain. 2009;13:518–523. doi: 10.1016/j.ejpain.2008.06.005. [DOI] [PubMed] [Google Scholar]
- 22.Leeuw M, Peters ML, Wiers RW, Vlaeyen JW. Measuring fear of movement/(re)injury in chronic low back pain using implicit measures. Cogn Behav Ther. 2007;36:52–64. doi: 10.1080/16506070601070400. [DOI] [PubMed] [Google Scholar]
- 23.Linton SJ, Andersson T. Can chronic disability be prevented? A randomized trial of a cognitive-behavior intervention and two forms of information for patients with spinal pain. Spine. 2000;25:2825–2831. doi: 10.1097/00007632-200011010-00017. [DOI] [PubMed] [Google Scholar]
- 24. Jensen JN, Karpatschof B, Labriola M, Albertsen K. Do fear-avoidance beliefs play a role on the association between low back pain and sickness absence? A prospective cohort study among female health care workers. J Occup Environ Med. 2010;52:85–90. doi: 10.1097/JOM.0b013e3181c95b9e. This well-designed prospective study provides evidence for the role of fear-avoidance beliefs on low back pain severity and sickness absence
- 25.Keefe FJ, Rumble ME, Scipio CD, et al. Psychological aspects of persistent pain: current state of the science. J Pain. 2004;5:195–211. doi: 10.1016/j.jpain.2004.02.576. [DOI] [PubMed] [Google Scholar]
- 26.Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behav Res Ther. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- 27.Ochsner KN, Ludlow DH, Knierim K, et al. Neural correlates of individual differences in pain-related fear and anxiety. Pain. 2006;120:69–77. doi: 10.1016/j.pain.2005.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Keogh E, Hamid R, Hamid S, Ellery D. Investigating the effect of anxiety sensitivity, gender and negative interpretative bias on the perception of chest pain. Pain. 2004;111:209–217. doi: 10.1016/j.pain.2004.06.017. [DOI] [PubMed] [Google Scholar]
- 29.Vancleef LM, Peters ML, Gilissen SM, De Jong PJ. Understanding the role of injury/illness sensitivity and anxiety sensitivity in (automatic) pain processing: an examination using the extrinsic affective simon task. J Pain. 2007;8:563–572. doi: 10.1016/j.jpain.2007.02.431. [DOI] [PubMed] [Google Scholar]
- 30.Taylor S. The structure of fundamental fears. J Behav Ther Exp Psychiatry. 1993;24:289–299. doi: 10.1016/0005-7916(93)90053-y. [DOI] [PubMed] [Google Scholar]
- 31.Binkley CJ, Beacham A, Neace W, et al. Genetic variations associated with red hair color and fear of dental pain, anxiety regarding dental care and avoidance of dental care. J Am Dent Assoc. 2009;140:896–905. doi: 10.14219/jada.archive.2009.0283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Blaya C, Moorjani P, Salum GA, et al. Preliminary evidence of association between EFHC2, a gene implicated in fear recognition, and harm avoidance. Neurosci Lett. 2009;452:84–86. doi: 10.1016/j.neulet.2009.01.036. [DOI] [PubMed] [Google Scholar]
- 33.Houben RM, Ostelo RW, Vlaeyen JW, et al. Health care providers’ orientations towards common low back pain predict perceived harmfulness of physical activities and recommendations regarding return to normal activity. Eur J Pain. 2005;9:173–183. doi: 10.1016/j.ejpain.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 34.Linton SJ, Vlaeyen J, Ostelo R. The back pain beliefs of health care providers: are we fear-avoidant? J Occup Rehabil. 2002;12:223–232. doi: 10.1023/a:1020218422974. [DOI] [PubMed] [Google Scholar]
- 35.Werner EL, Ihlebaek C, Skouen JS, Laerum E. Beliefs about low back pain in the Norwegian general population: are they related to pain experiences and health professionals? Spine. 2005;30:1770–1776. doi: 10.1097/01.brs.0000171909.81632.fe. [DOI] [PubMed] [Google Scholar]
- 36.Turk DC, Okifuji A. What factors affect physicians’ decisions to prescribe opioids for chronic noncancer pain patients? Clin J Pain. 1997;13:330–336. doi: 10.1097/00002508-199712000-00011. [DOI] [PubMed] [Google Scholar]
- 37.Godges JJ, Anger MA, Zimmerman G, Delitto A. Effects of education on return-to-work status for people with fear-avoidance beliefs and acute low back pain. Phys Ther. 2008;88:231–239. doi: 10.2522/ptj.20050121. [DOI] [PubMed] [Google Scholar]
- 38.Buchbinder R, Jolley D, Wyatt M. 2001 Volvo Award Winner in Clinical Studies: effects of a media campaign on back pain beliefs and its potential influence on management of low back pain in general practice. Spine. 2001;26:2535–2542. doi: 10.1097/00007632-200112010-00005. [DOI] [PubMed] [Google Scholar]
- 39.Buchbinder R, Jolley D. Effects of a media campaign on back beliefs is sustained 3 years after its cessation. Spine. 2005;30:1323–1330. doi: 10.1097/01.brs.0000164121.77862.4b. [DOI] [PubMed] [Google Scholar]
- 40.de Jong JR, Vlaeyen JW, Onghena P, et al. Fear of movement/(re) injury in chronic low back pain: education or exposure in vivo as mediator to fear reduction? Clin J Pain. 2005;21:9–17. doi: 10.1097/00002508-200501000-00002. discussion 69–72. [DOI] [PubMed] [Google Scholar]
- 41.de Jong JR, Vlaeyen JW, Onghena P, et al. Reduction of pain-related fear in complex regional pain syndrome type I: the application of graded exposure in vivo. Pain. 2005;116:264–275. doi: 10.1016/j.pain.2005.04.019. [DOI] [PubMed] [Google Scholar]
- 42.Vowles KE, Gross RT. Work-related beliefs about injury and physical capability for work in individuals with chronic pain. Pain. 2003;101:291–298. doi: 10.1016/S0304-3959(02)00337-8. [DOI] [PubMed] [Google Scholar]
- 43.Williams A de C, McCracken LM. Cognitive-behavioral therapy for chronic pain: an overview with specific reference to fear and avoidance. In: Asmundson G, Vlaeyen J, Crombez G, editors. Understanding and Treating Fear of Pain. Oxford: Oxford University Press; 2004. pp. 293–312. [Google Scholar]
- 44.Burwinkle T, Robinson JP, Turk DC. Fear of movement: factor structure of the Tampa scale of kinesiophobia in patients with fibromyalgia syndrome. J Pain. 2005;6:384–391. doi: 10.1016/j.jpain.2005.01.355. [DOI] [PubMed] [Google Scholar]
- 45.Turk DC, Robinson JP, Sherman JJ, et al. Assessing fear in patients with cervical pain: development and validation of the Pictorial Fear of Activity Scale-Cervical (PFActS-C) Pain. 2008;139:55–62. doi: 10.1016/j.pain.2008.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Wideman TH, Adams H, Sullivan MJ. A prospective sequential analysis of the fear-avoidance model of pain. Pain. 2009;145:45–51. doi: 10.1016/j.pain.2009.04.022. This prospective sequential analysis of a pain disability treatment intervention provides evidence for the role of catastrophizing and fear avoidance beliefs in treatment outcome, and highlights some of the latest controversies within the fear-avoidance literature
- 47.Vlaeyen JW, Crombez G, Linton SJ. The fear-avoidance model of pain: we are not there yet. Comment on Wideman et al. “A prospective sequential analysis of the fear-avoidance model of pain” [Pain 2009] and Nicholas “First things first: reduction in catastrophizing before fear of movement” [Pain 2009] Pain. 2009;146:222. doi: 10.1016/j.pain.2009.08.022. author reply 222–223. [DOI] [PubMed] [Google Scholar]
- 48.Martins IP, Gouveia RG, Parreira E. Kinesiophobia in migraine. J Pain. 2006;7:445–451. doi: 10.1016/j.jpain.2006.01.449. [DOI] [PubMed] [Google Scholar]
- 49.Turk DC, Okifuji A. Perception of traumatic onset, compensation status, and physical findings: impact on pain severity, emotional distress, and disability in chronic pain patients. J Behav Med. 1996;19:435–453. doi: 10.1007/BF01857677. [DOI] [PubMed] [Google Scholar]
- 50.Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965;50:971–979. doi: 10.1126/science.150.3699.971. [DOI] [PubMed] [Google Scholar]
- 51.McNeil DW, Rainwater AJ., 3rd Development of the Fear of Pain Questionnaire—III. J Behav Med. 1998;21:389–410. doi: 10.1023/a:1018782831217. [DOI] [PubMed] [Google Scholar]
- 52.Kori SH, Miller RP, Todd DD. Kinisophobia: a new view of chronic pain behavior. Pain Manag. 1990;3:35–43. [Google Scholar]
- 53.Crombez G, Vlaeyen JW, Heuts PH, Lysens R. Pain-related fear is more disabling than pain itself: evidence on the role of pain-related fear in chronic back pain disability. Pain. 1999;80:329–339. doi: 10.1016/s0304-3959(98)00229-2. [DOI] [PubMed] [Google Scholar]
- 54.Lame IE, Peters M, Kessels AG, et al. Test-retest stability of the Pain Catastrophizing Scale and the Tampa Scale for Kinesiophobia in chronic pain patients. J Health Psychol. 2008;13:820–826. doi: 10.1177/1359105308093866. [DOI] [PubMed] [Google Scholar]
- 55.Sullivan MJL, Bishop SR, Pivik J. The Pain Catastrophizing Scale: development and validation. Psychol Assess. 1995;7:524–532. [Google Scholar]