Abstract
STUDY DESIGN
Case report.
BACKGROUND
No head-to-head comparisons of different orthoses for patients with stage II posterior tibial tendon dysfunction (PTTD) have been performed to date. Additionally, the cost of orthoses varies considerably, thus choosing an effective orthosis that is affordable to the patient is largely a trial-and-error process.
CASE DESCRIPTION
A 77-year-old woman was seen with complaints of abnormal foot posture (“my foot is out”), minimal medial foot and ankle pain, and a 3-year history of conservatively managed stage II PTTD. The patient was not able to complete 1 single-limb heel rise on the involved side, while she could complete 3 on the uninvolved side. Ankle strength testing revealed a mild to moderate loss of plantar flexor strength (20%–31% deficit on the involved side), combined with a 22% deficit in isometric ankle inversion and forefoot adduction strength. To assist this patient in managing her flatfoot posture and PTTD, 3 orthoses were considered: an off-the-shelf ankle-foot orthosis (AFO), a custom solid AFO, and a custom articulated AFO. The patient’s chief complaint was partly cosmetic (“my foot is out”). As decreasing flatfoot kinematics may unload the tibialis posterior muscle, thus prevent the progression of foot deformity, the primary goal of orthotic intervention was to improve flatfoot kinematics. Given the difficulties in clinical approaches to evaluating flatfoot kinematics, a quantitative gait analysis, using a multisegment foot model, was used.
OUTCOMES
In the frontal plane, all 3 orthoses were associated with small changes toward hindfoot inversion. In the sagittal plane, between 2.7° and 6.1°, greater forefoot plantar flexion (raising the medial longitudinal arch) occurred. There were no differences among the orthoses on hindfoot inversion and forefoot plantar flexion. In the transverse plane, the off-the-shelf design was associated with forefoot abduction, the custom solid orthosis was associated with no change, and the custom articulated orthosis was associated with forefoot adduction.
DISCUSSION
Based on gait analysis, the higher-cost custom articulated orthosis was chosen as optimal for the patient. This custom articulated orthosis was associated with the greatest change in flatfoot deformity, assessed using gait analysis. The patient felt it produced the greatest correction in foot deformity. Reducing flatfoot deformity while allowing ankle movement may limit progression of stage II PTTD.
Keywords: biomechanics, PTTD, tendinopathy
Posterior tibial tendon dysfunction (PTTD) is typically described as a progressive disorder ranging from stage I to stage IV, with hallmarks of advancing flatfoot deformity and deteriorating function. Ultimately, stage IV is identified by the presence progression of this dysfunction is not clear, though strengthening programs and the use of orthoses may slow its progression.24,26 Patients’ perception of their pain and functional limitation can be mild, which is in stark contrast to the advanced flat-foot deformity and weakness patients commonly exhibit. The clinical paradox of mild functional limitation with advanced flatfoot deformity poses a problem when trying to select an appropriate orthosis. Advanced flatfoot deformity and weakness support the clinical use of custom orthoses, which, though expensive, give maximal support to the foot and theoretically prevent further deformity. Yet minimal functional limitations and complaints of pain suggest that custom orthoses, which limit foot and ankle movement, may be unnecessary. Furthermore, custom orthoses may lead to altered gait patterns and contribute to weakness and, therefore, dependency.
Numerous clinical guidelines recommend the use of orthoses for the conservative management of PTTD.7,11,15,19,29,34 These guidelines are not based on controlled trials comparing orthoses but, rather, on observational studies and theory. Thus choosing an appropriate orthosis is difficult. Although there are only limited data, current evidence suggests that the use of more restrictive orthoses that cross the ankle joint will be the most successful in the clinical management of stage II PTTD. A 2-year follow-up using the validated Foot Function Index (FFI) questionnaire reported that 90% of patients wearing the custom Arizona ankle-foot orthosis (AFO) had decreased pain and increased function.3 Similar results have been reported for individuals using other AFO designs.6 A recent 7-year follow-up study indicated overall long-term success (defined as the patient being orthosis free and avoiding surgery) in 69.7% of cases treated with a custom-AFO design.26 Off-the-shelf orthoses that extend above the ankle, such as the AirLift PTTD orthosis (DJ Orthopedics, Vista, CA), are also available commercially and widely used, despite limited data on effectiveness.27 Overall, data support the use of more restrictive custom orthoses that extend proximal to the ankle joint3,6; but off-the-shelf designs offer a considerable cost savings and are clinically popular.
Recently, numerous researchers31,32,36,40 have identified specific flat-foot kinematics in subjects with stage II PTTD that are linked to damage of the tibialis posterior tendon or the spring ligament.9,32 In vivo kinematic models, as well as static measurements of foot posture (eg, radiographs), suggest that excessive hindfoot eversion and forefoot abduction are typical in individuals with stage II PTTD.31,40 To unload the tibialis posterior tendon, correction of a patient’s flatfoot kinematics toward hindfoot inversion and forefoot adduction is proposed as a goal for orthoses.32 The spring ligament is commonly damaged in individuals with PTTD.9,14 The spring ligament prevents hindfoot eversion and plantar flexion of the talus.20 Therefore, orthoses that induce inversion of the hindfoot and raise the medial longitudinal arch (MLA) are recommended to unload the spring ligament.20 Correction of forefoot abduction is thought to occur by controlling the hindfoot and MLA.2,4,12 This focus on decreasing stress to the tibialis posterior and spring ligament by targeting correction of specific foot kinematics may contrast with approaches that focus on forefoot varus. With this approach, orthotic designs include forefoot varus corrections to indirectly correct other foot kinematics, such as hindfoot inversion, but may not directly target correction of MLA height or forefoot abduction. Perhaps due to the necessity to offload the tibialis posterior muscle in patients with PTTD, current custom orthotic designs have focused on directly compensating for the function of the muscle and associated spring ligament, and not on forefoot mechanics.
Weakness in subjects with stage II PTTD may impact functional mobility and influence orthosis selection. Imaging studies have identified atrophy of the tibialis posterior muscle in individuals with stage II PTTD,37,41 while another study, testing overall isokinetic ankle strength, found significant weakness in all planes of ankle motion.1 Ankle plantar flexion weakness may account for functional impairments and gait disturbances reported by patients with PTTD.3,24 Orthoses that restrict ankle motion (solid AFO), while very popular, may induce plantar flexor weakness and increase dependence on the orthosis for support. Nevertheless, in cases of severe deformity, the use of orthoses that restrict ankle plantar flexion may be justified to correct flatfoot deformity and unload the tibialis posterior muscle. Consistent with theory that unloading the foot is necessary, orthoses that are custom made and allow ankle movement (hinged AFOs) are considered insufficient. Similarly, off-the-shelf orthoses that rely on a general fit to limit hindfoot movement and support the MLA are controversial. The less optimal performance of these orthoses compared to solid AFOs would be a smaller correction in foot kinematics. The foot kinematics these orthoses are currently designed to control are hindfoot eversion and MLA lowering.
The purpose of this case report was to select the most appropriate of 3 common AFO designs for a patient with stage II PTTD, based on correction of flatfoot kinematics using quantitative gait analysis. Correction of flatfoot kinematics is the theoretical goal of treatment using orthoses for stage II PTTD, and this goal is made more apparent when patients present with only minimal pain and limitation but advanced flatfoot deformity. It was assumed that hindfoot inversion, forefoot adduction, and forefoot plantar flexion (raising the MLA) would provide a positive benefit to the patient by potentially unloading support structures, such as the tibialis posterior tendon and spring ligament, and improving joint alignment to limit the onset of arthritic changes in the lateral talocrural joint.
CASE DESCRIPTION
History
A 77-year-old woman with minimal complaints of right medial foot and ankle pain and a 3-yearhistory of conservatively managed stage II PTTD was evaluated for optimal orthosis selection. Her medical history included a “bad back” that had bothered her for approximately 15 years and had been attributed to arthritis. The patient had diagnostic imaging and managed her back pain with medication and rest. The patient also complained of hip pain that was also attributed to arthritis and primarily limited her ability to comfortably reach her feet to lace her shoes. She was on blood pressure and thyroid medication to manage high blood pressure and hypothyroidism. She considered herself “generally healthy” otherwise. A general screen of the proximal joints of the lower extremity revealed a limited and weak right hip secondary to pain but no other impairments (TABLE 1).
TABLE 1.
Clinical Profile
| Involved Side | Uninvolved Side | I/U Ratio | |
|---|---|---|---|
| Lower extremity screening | |||
| Range of motion (deg) | |||
| External rotation | 0–25 | ||
| Abduction | 0–35 | ||
| Strength | |||
| Within normal limits, except hip external rotation | 3+/5 | ||
| and abduction | 3/5 | ||
| Pain* | 6/10 | ||
| Measures of foot/ankle strength | |||
| Isometric plantar flexor strength (N) | |||
| Maximum dorsiflexion | 83.0 | 103.8 | 0.80 |
| 5° dorsiflexion | 60.5 | 76.1 | 0.80 |
| 20° plantar flexion | 23.6 | 34.0 | 0.69 |
| Isometric ankle inversion/forefoot adduction (N) | 50.2 | 64.4 | 0.78 |
| Single heel rise ability | 0 | 3 | |
Abbreviation: I/U, involved to uninvolved strength ratio.
Response to pain at its worst in the past 24 hours, on 0-to-10 scale, with 0 being “no pain” and 10 “the worst pain imaginable.”
She was diagnosed with stage II PTTD by a fellowship-trained foot and ankle orthopedic surgeon 1 year after the pain began (2 years previous to this case report). Consistent with published recommendations,17 the diagnosis of stage II PTTD was made based on the history, clinical exam, and radiographic evaluation, while the use of further imaging studies (magnetic resonance imaging) was not deemed necessary. Following her diagnosis, she pursued various treatments, including the use of an off-the-shelf AFO (AirLift PTTD; DJ Orthopedics), as well as exercise focused on ankle strengthening. The course of conservative care with exercise, combined with using an orthosis, was motivated by published protocols and the theory that the tendon should be unloaded initially, followed by reloading to remodel and heal the tendon.1,6,24,25 The validated FFI questionnaire was used to provide baseline information on the patient’s pain and function and to document change with care. The patient’s FFI average was 41%, with subscale scores of 10% for activity limitation, 60.6% for disability, and 52.8% for pain. The patient rated her medial foot and ankle pain as 7/10, with 0 being “no pain” and 10 being “the worst pain imaginable,” when describing the pain at its worst in the past 24 hours.
Physical therapy management consisted of 12 weeks of exercise and stretching, including 8 clinic visits and a home exercise program. Strengthening included resisted ankle inversion and forefoot adduction using a Thera-Band placed around the forefoot. Similar exercises have been shown to selectively activate the tibialis posterior muscle and are recommended for strengthening.23 Additionally, both double- and single-limb heel rises were completed, focusing on inverting the heel during the activity. Exercises to stretch the calf muscle and perform ankle inversion/eversion range of motion were also included. Following treatment, the patient’s FFI average was 17.8% and her subscale scores were 0% for activity limitation, 33.5% for disability, and 20% for pain. Pain was rated at 3/10 at its worst. Despite the continued presence of weakness, the patient had discontinued physical therapy care after the initial 12-week program, feeling that she had reached a plateau with her functional mobility, pain, and strength. After improvement with use of the AFO and physical therapy, it was recommended that she “step-down” to the use of in-shoe foot orthoses. The in-shoe orthoses were an off-the-shelf design, with a full-length foot plate, chosen for its medial arch support. A medial heel wedge of cork (approximately 5 mm) was added to the involved side to further support and correct hindfoot valgus position and medial arch height. The patient had used the in-shoe orthoses and the AFO interchangeably over the past 2 years.
The main indications for surgery are significant flatfoot deformity, persistent symptoms, and functional limitations.30 The patient’s flatfoot deformity was significant (FIGURE 1A) enough to make her a candidate for surgery; however, her symptoms and functional limitations were only minimal for her lifestyle. Further, she continued to adequately manage her pain with the use of in-shoe orthoses, intermittent exercise, and AFO wear.
FIGURE 1.

(A) Foot posture for this patient with advanced stage II posterior tibial tendon dysfunction (PTTD) of the right foot. (B) Weight-bearing radiographs of the right foot in this patient demonstrating advanced flatfoot deformity. Average angles reported in the literature44 include talar-first metatarsal angle (7.1°; 95% confidence interval: 3.0° to 11.2°); average (SD) calcaneal pitch angle, 20.8° (4.1°); navicular coverage angle, 19.3° (23.8°).
The patient presented at this point (approximately 2 years after conservative treatment with physical therapy and bracing, and about 3 years since the pain first started) with complaints of limited recreational mobility (walking for fitness and to go shopping) due to her foot and ankle pain, although the AFO or in-shoe orthoses had been helpful. Her current pain at its worst in the past 24 hours was 3/10, with 0 as “no pain” and 10 “the worst pain imaginable.” She also consistently complained that, cosmetically, her foot was still “out,” meaning that her involved foot was noticeably laterally deviated when she walked.
Tests and Measures
Signs consistent with stage II PTTD included excessive hindfoot eversion when standing and a positive too-many-toes sign, indicating forefoot abduction (FIGURE 1A). A thorough assessment of foot alignment and structure included a clinical exam, radiographic exam, and use of validated MLA measurements. The foot and ankle exam revealed a hindfoot eversion deformity of 18° on the right and 8° on the left, during standing. Hindfoot inversion to neutral was possible on the right, while on the left an inversion angle of 7° was passively achieved. Weight-bearing radiographs were available and used to characterize the structure of the flatfoot (FIGURE 1B).38,44 Interpretation of the radiographic findings suggested loss of MLA height and advanced forefoot abduction deformity. The Arch Height Index (AHI), a reliable and valid measure of MLA height,43 was 0.277, when recorded in a seated position. This indicated a lower MLA compared to the uninvolved side (0.303) and published normative data (mean ± SD, 0.340 ± 0.030).5 The patient was also noted to have a forefoot varus deformity (a position of forefoot inversion relative to the hindfoot), when assessed in a non–weight-bearing position. But this was not measured, as it was deemed less severe than the other flat-foot deviations (hindfoot eversion, forefoot abduction, and a low MLA), and is less commonly described in the clinical or radiological examination of individuals with PTTD.21,38,44
In terms of strength and function, the patient was able to complete only 5 bilateral heel rises, with a decrease in heel elevation on the involved (right) side. The use of the double heel rise has been described as helpful in assessing inversion range, or correction of valgus hindfoot positioning compared to standing.25 During the bilateral heel rise, the patient was able to achieve an inverted position bilaterally; however, hindfoot inversion of the uninvolved side was greater than that of the involved side. The single heel rise is an assessment of strength, and the patient was not able to complete a single heel rise on the involved side. On the uninvolved side, she completed 3 heel rises, with minimal upper extremity support for balance and a heel height similar to that of a bilateral heel rise. During the single heel rise, the hindfoot did not move from its everted standing position on the involved side, an indication of tibialis posterior weakness and/or plantar flexion weakness. She complained of pain on the medial ankle and under the MLA during single- and double-heel-rise tests, ranging between 2/10 and 4/10.
The ability to complete a heel rise is also dependent on strength in the ankle plantar flexor muscle group. A strength profile was completed, including isometric ankle plantar flexor testing, as well as ankle inversion and forefoot adduction testing meant to isolate the role of the tibialis posterior muscle.18,23 Isometric plantar flexor testing was done on the Biodex System 4 at 3 ankle positions (maximum dorsiflexion, 5° of dorsiflexion, and 20° of plantar flexion). Ankle inversion and forefoot adduction testing was done using a custom strength-testing device, previously described and validated,18 that includes a sliding plate connected in series with a force transducer. Subjects were asked to invert the ankle and adduct the forefoot isometrically, while peak force was recorded (TABLE 1).
The strength profile revealed mild to moderate weakness of the plantar flexors (20%–31% deficit compared to the uninvolved side) and a 22% deficit in ankle inversion and forefoot adduction (deep posterior compartment weakness). The patient reported between 2/10 and 4/10 pain during strength testing, but did not feel that pain limited her ability to provide maximum effort during testing. In our experience, the amount of plantar flexor weakness was not sufficient to explain the loss of single-heel-rise ability. The clinical hypothesis was that the failure to heel rise was related to abnormal mechanics due to the flatfoot deformity. Consequently, the therapeutic goals were to (1) use an orthosis to stabilize the foot as much as possible, and (2) prevent further weakness of the ankle plantar flexors and subtalar inverters, if possible. However, the cost of a custom AFO can be more than $1000, which is considerably greater than the current orthoses she was using (both her off-the-shelf in-shoe orthosis and her off-the-shelf AFO were $60.00). Yet it was also clear clinically that her foot alignment was not adequately controlled with her current off-the-shelf foot orthosis and AFO. The presence of forefoot abduction deformity was clinically obvious and was one of the patient’s chief complaints. Gait analysis was used to help determine whether custom orthoses offered better correction of flatfoot deformity than the off-the-shelf orthosis she was using. It was assumed that greater correction of foot alignment would positively affect mobility, maintain current ankle strength, limit progression to arthritic changes seen with stage IV PTTD, and prevent reoccurrence of painful episodes.
Device Design and Fabrication
For this patient, 3 AFOs were considered, based on positive outcomes with other patients3,6,27 and the components necessary to correct the observed flatfoot deformity. The first orthosis was an off-the-shelf AFO (AirLift PTTD; DJ Orthopedics, Vista, CA), the second a custom-molded AFO with a nonarticulating ankle (Arizona AFO, Inc, Mesa, AZ), and the third a custom-molded AFO with an articulating ankle (Arizona AFO, Inc). These orthoses may be broadly described as utilizing 2 mechanisms to manage the symptoms and flatfoot deformity observed in individuals with PTTD. First, each of these orthoses provides compression to the ankle, which aids in controlling swelling and provides proprioceptive support.10,27 Second, each orthosis attempts to correct foot alignment by applying forces in locations needed to return the foot to a neutral position or prevent further deformity from occurring. Limits for hind-foot eversion are provided by 3 points of contact—lower lateral leg, medial malleolus, and lateral heel—to maintain a neutral hindfoot-to-leg position. To support or correct the height of the MLA, the mechanism used is different for the custom and off-the-shelf orthoses. For the custom orthoses (articulated or solid), support for the MLA comes from a foot plate that extends to the metatarsal heads and is fitted to the MLA, while the foot is held in a neutral hindfoot alignment and supported arch. For the off-the-shelf orthosis, an airbladder component is positioned under the MLA and inflated to raise the MLA. Control of forefoot abduction is accomplished by relying on coupled motion in the midfoot, occurring with correction of hindfoot eversion. Additionally, 3 points of contact, including the lateral heel, medial arch, and lateral forefoot (by the orthosis and shoe), may aid in correcting forefoot abduction.
Three weeks before a scheduled testing session, casting for the custom orthoses was completed by a certified pedorthist. The foot was marked for boney landmarks and wrapped with fiberglass. The foot was positioned in contact with a casting plate on the floor, with the hind-foot positioned in subtalar neutral, as palpated by the pedorthist. The resulting negative mold was sent to the Arizona Company for the manufacture of 2 orthoses for testing.
The custom orthoses were modified to include a “window” needed to visualize the calcaneus for gait analysis (FIGURES 2 AND 3). The custom orthoses are constructed using a 3-mm polypropylene (plastic) ankle shell sewn inside a leather cover. The plastic shell covers the medial and lateral ankle (clam-shell) and continues around the foot, to extend along the plantar aspect of the foot and end proximal to the metatarsal heads. The posterior portion of the heel contains no plastic support. In the solid-ankle design this posterior heel is covered with leather, while in the articulated-ankle design the foot and shank parts of the orthosis are separated by a joint that leaves the posterior heel open. In the solid-ankle design the leather portion on the posterior heel was removed without altering the plastic support. In the articulated design the window was already available but was enlarged by trimming distal to the joint into the foot part of the orthosis to allow kinematic marker placement. The window locations were chosen to avoid the plastic support structure of the orthoses and, qualitatively, did not appear to alter the integrity of the orthoses but, rather, removed the leather cover that was deemed aesthetic. Windows were also made in the testing shoe in the area of the heel marker and marker on the dorsal surface of the first metatarsal. Similar efforts to maintain the stability of the shoe were taken by adding a heel strap and replacing the shoe lacing. A previous study indicated that heel counter stability was altered less than 10% following similar shoe alterations.42 The modifications made to the shoe and orthoses were completed with input from the authors and pedorthist, with efforts to maintain the integrity of the orthoses while completing the protocol. The custom orthoses were considered fit to wear long term by the patient following the testing protocol, if suggested.
FIGURE 2.

The 3 orthoses evaluated for use in this case report with modifications needed for motion analysis testing.
FIGURE 3.
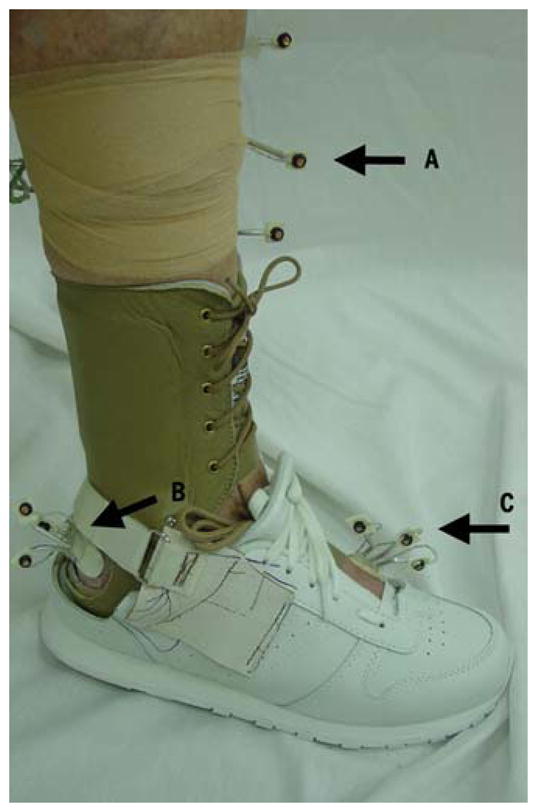
Custom solid orthosis with shoe, modified for testing in the laboratory. Holes were cut in the orthosis and shoe to allow visualization of the infrared markers for kinematic testing. (A) Tibia markers; (B) window cut in the orthosis and shoe to allow visualization of the calcaneal markers; (C) window cut in the shoe to allow visualization of the metatarsal markers.
The patient was seen 2 weeks prior to testing for fitting of the orthoses. Each of the custom orthoses was fit by the pedorthist, which included contouring the molding over the medial navicular process and medial malleolus to alleviate pressure during standing. These were deemed common alterations by the attending pedorthist for the final fitting of these custom orthoses. The off-the-shelf orthosis was fit according to manufacturer recommendations and was checked to ensure that the same shoe could be used during the kinematic testing. The subject was given a wearing schedule to gradually accommodate to the orthoses over the following 2 weeks and to keep a log of the time spent wearing each orthosis. The subject was instructed to wear each orthosis for a few hours each day, wearing the same orthosis for 3 days before starting the next one. This routine was repeated for 2 weeks until the motion testing occurred.
Motion Analysis Testing
At the time of testing, the patient had worn each orthosis an average of 15 hours over the 2 weeks prior and reported that she felt the custom orthoses seemed to provide greater support (“they prevent my foot from going out”), compared to the off-the-shelf design. But the off-the-shelf design was easier to wear and was more comfortable. The session consisted of a series of walking trials to test each orthosis. Initially, the off-the-shelf AFO was used along with the modified shoe. The off-the-shelf AFO contains an airbladder along the medial side that was filled to a pressure level of 4 PSI (27.6 kPa) in a non–weight-bearing position. The 4 PSI level was chosen as a midlevel inflation comfortable to patients and previously found to achieve correction of foot kinematics.33 Infrared-emitting diodes (IREDs) were then taped to the skin through the visualization holes in the shoe. The subject was asked to walk down a 5-m walkway at a speed of 1.3 m/s. Speed was maintained within 5%, using an infrared timing system. Following 5 successful trials, in which the involved foot landed completely on the force plate and the markers were in view, the shoe was removed by unlacing the front and unhooking the custom heel counter that was attached to the back of the shoe. This was done without removing the IREDs. The off-the-shelf AFO was removed by cutting the neoprene sleeve, again without disrupting the placement of the kinematic markers. Next, the custom molded, solid-ankle AFO was donned, along with the shoe, and the walking trials were repeated. Finally, this same procedure was repeated with the custom-articulated AFO.
Kinematic data were collected using a 3-segment foot model that included the tibia, calcaneus (hindfoot), and first metatarsal (forefoot), similar to a previously described model.40 Briefly, sets of 3 IREDs were mounted on rigid thermoplastic platforms, and then attached using double-sided adhesive tape. Anatomic landmarks were digitized to establish local anatomically based coordinate systems for each segment. Motion of the distal most foot segment was then calculated relative to the adjacent proximal segment, based on the Euler rotation sequence of flexion/extension, inversion/eversion, and abduction/adduction, as suggested by Cole et al.8 The model used for this case report consisted of the first metatarsal, which was used to determine angle of flexion/extension, as well as abduction/adduction, between the forefoot and hindfoot segments. Two banks of infrared cameras (Optotrak 3020; Northern Digital Inc, Waterloo, Ontario, Canada), in conjunction with Motion Monitor software, Version 7.24 (Innovative Sports Training, Inc, Chicago, IL) was used to track IRED sets on each segment at a sampling rate of 60 Hz. The field of view of the Optotrak is 2.25 m2 at a distance of 2 m. The manufacturer reports accuracy of tracking an individual IRED at ±0.1 mm, with additional studies also reporting excellent precision and repeatability using the Optotrak system.28,39 Using a 10-N threshold of vertical forces, collected at 1000 Hz from an embedded force plate (model 9286; Kistler Instrumente AG, Winterthur, Switzerland), initial contact and toe-off points of the gait cycle were identified. Kinematic data were smoothed using a fourth-order, zero-phase-lag Butterworth filter, with a cut-off frequency of 6 Hz. Trials were averaged and variables of interest were interpolated to 101 points (0%–100% stance) for comparison between the orthoses. The midpoint of each of the foot-ankle rockers (10%, 50%, and 90% of stance) was chosen as representative of the various mechanical demands placed on the foot across the gait cycle and was used as a point to compare among orthosis conditions.35
To aid in the decision of which orthosis provided the greatest change in foot kinematics, an intraclass correlation coefficient (ICC3,1) was calculated and used to determine the standard error in the measurements (SEM). Two times the SEM (2SEM) was used to assess those changes that were above error and should be interpreted as meaningful differences between orthosis conditions. The 2SEM values were 1.2° for hindfoot eversion/inversion, 1.2° for forefoot plantar flexion/dorsiflexion, and 0.5° for forefoot abduction/adduction.
OUTCOMES
The effect of the various orthoses was determined by comparison with wearing the shoe only (ie, no support except the shoe). In the frontal plane, small changes toward hindfoot inversion occurred with all 3 orthoses, most notably during first and second rocker. The off-the-shelf orthosis and the custom articulated orthosis were the most successful in producing hindfoot inversion compared to the shoe-only condition. Unexpectedly, the custom solid orthosis did not produce hindfoot inversion above the error range of the 2SEM when compared to the shoe-only condition across the stance phase. During third rocker, changes were below the 2SEM error range for all 3 orthoses tested.
In the sagittal plane, between 2.7° and 6.1° of greater forefoot plantar flexion (raising of the MLA) was observed with all 3 orthoses tested, compared to the shoe-only condition. The effect was greatest at 50% of stance, when the foot was flat on the ground. At third rocker the greatest forefoot plantar flexion was seen with the custom solid orthosis.
In the transverse plane, the off-the-shelf orthosis resulted in increased forefoot abduction, the custom solid orthosis produced no change, and the custom articulated orthosis produced forefoot adduction. The custom articulated orthosis, when compared to the off-the-shelf orthosis, resulted in between 3.5° and 5.4° greater forefoot adduction.
Following the recommendation to wear the custom articulated orthosis, the patient was contacted by telephone for a 3-month follow-up. She continued to wear the custom articulated orthosis an average of 4 to 5 hours a day when she was most active on her feet. The patient continued to report that her foot felt the most supported in the custom orthosis but, when it was removed, her foot was still out.
DISCUSSION
Based on the clinical presentation and kinematic testing of the 3 orthoses, a decision was made on the most effective orthosis for this patient. The patient was encouraged to wear the custom articulated orthosis because (1) this orthosis provided the greatest correction of flatfoot kinematics, compared to only wearing a shoe, and (2) this orthosis contained an articulated ankle, allowing ankle plantar flexion/dorsiflexion movement, which may be beneficial to minimize weakness induced by wearing a solid orthosis. Given her complaints related to her foot being out, continued weakness despite rehabilitation, and severe foot deformity, a more costly and supportive orthosis was clinically justified. Although changes toward improvement in flatfoot kinematics were observed with the custom articulated-ankle orthosis, complete correction of foot deformity was not achieved, suggesting that further improvement in orthosis designs are needed.
Overall, for hindfoot inversion, the 3 points of pressure used by each of the tested orthoses to correct alignment produced small changes. The 2 orthoses with a freely moving ankle joint were associated with the greatest changes towards hindfoot inversion. This may be the influence of muscle function to provide additional hindfoot control with the freely moving ankle joint. Movement at the ankle may allow greater use of the plantar flexors, including the triceps surea, as well as the deep posterior compartment muscles (tibialis posterior, flexor digitorum longus, and flexor hallucis longus). These muscles also cross medial to the subtalar joint and contribute to inversion.22 At the end of stance, each of the 3 orthoses offered no greater control in hindfoot inversion than the shoe, with all changes smaller than 1°. The large forces transmitted through the foot at the end of stance may limit the effectiveness of orthoses at this point in stance. It has been argued that small changes of 2° may be clinically meaningful if these changes are able to unload support structures during repetitive tasks such as walking.16 Changes of greater than 2° were observed when testing the 2 orthoses with a movable ankle. Nevertheless, given the excessive (greater than 15°) hindfoot eversion observed in this subject and the small changes that were associated with wearing the orthoses, greater corrections in hindfoot control are needed.
Forefoot plantar flexion occurred with each of the orthoses across all 3 phases of stance, suggesting an unloading of the ligaments such as the spring ligament. Forefoot plantar flexion in this kinematic model is reflective of raising the MLA, with changes between 4.8° and 6.1° occurring during the midstance phase of gait (50% stance). During the midstance phase, the 2 articulated orthoses were associated with slightly greater changes (6.0° and 6.1°) in forefoot plantar flexion compared to the solid orthosis (4.8°). This is in agreement with in vitro data, in which a custom-molded articulated orthosis was associated with greater changes in MLA height, compared to a solid orthosis.19 It remains unclear what design components make the articulated orthosis more successful in correcting arch height at midstance; however, our hypothesis, again, relates to improved dynamic support of the foot when ankle motion is allowed, due to recruitment of ankle musculature. There was also a strong effect towards maintaining the height of the MLA observed with the custom-molded solid orthosis at the end of stance. The end of stance was not evaluated in previous in vitro studies and suggests support for the spring ligament when large forces are transferred through the forefoot. The lack of a moving ankle may alter gait patterns and contribute to further weakness in this subject; but this may be a necessary consequence of unloading the forefoot at the end of stance.
The airbladder component of the off-the-shelf orthosis was unable to correct advanced forefoot abduction deformity, while the design of the custom articulated orthosis provided greater correction. Forefoot abduction may contribute to excessive loading of the tibialis posterior tendon13 and was poorly controlled in some subjects tested with an off-the-shelf orthosis in a previous study.13,33 This case suggests that the off-the-shelf orthosis worsened forefoot abduction compared to the shoe condition, which may be due to placement of the inflated air bladder in subjects with advanced forefoot abduction deformity. When the forefoot is abducted, the airbladder may push the forefoot into further abduction when inflated. Across all phases of stance, the custom-articulated orthosis produced forefoot adduction, while the solid orthosis had a minimal effect and the off-the-shelf orthosis produced greater forefoot abduction. The footbed of the custom articulated orthosis is closely fitted to the plantar surface of the foot, with trim lines that extend around the posterior aspect of the calcaneus and distal to the metatarsal heads. This close fit may produce forefoot adduction over the fit of the other orthoses.
This case report sought to determine the best orthosis for this patient from a group of 3 AFO styles, based on improvement in flatfoot kinematics. The recommendation to use the custom-articulated orthosis was based on correction of flat-foot kinematics, and the patient agreed with this recommendation based on comfort. The primary foot kinematics deemed important to control, for this patient, included hindfoot eversion, forefoot abduction, and a low MLA. The 3 orthoses compared in this study all were designed to target these foot kinematics and have demonstrated positive outcomes.3,6,26 The procedures to test each orthoses in this case report are not possible in clinical practice but, rather, were used to demonstrate the effects of the specific orthoses on foot kinematics in a patient with advanced stage II PTTD, who presented with a flatfoot and ankle weakness. Further research may expand the procedures used in this case to examine the effects of articulated-ankle components and muscle function in individuals with PTTD. In the presence of only small changes seen in this subject, despite marked flatfoot deformity, other orthoses designs may be considered. For example, in-shoe foot orthoses with medial posting have been suggested to manage hindfoot eversion and forefoot varus, such as observed in this subject. Although current orthoses have targeted foot kinematics to unload the tibialis posterior tendon and spring ligament, future studies may consider alternate device designs for patients similar to the one presented in this study. Additionally, experimentally controlled studies are needed to provide more information on the long-term clinical outcomes expected from different orthoses.
This patient presented with advanced flatfoot deformity but mild complaints of pain and only limited functional loss. An articulated-ankle component was one feature noted in the custom orthosis that provided the greatest improvement in foot kinematics. The presence of only a mild to moderate strength loss in this patient may suggest risk for further strength loss, should the solid-ankle orthosis be adopted. The consistent finding in this patient of improved kinematics with the articulated versus solid ankle design underscored the importance of allowing ankle movement for foot function. Further, the hinged orthosis design was the only orthosis that influenced this patient’s chief cosmetic complaint of her foot being out.
CONCLUSIONS
The most appropriate of the 3 orthoses considered for the correction of flatfoot deformity in this patient was the custom articulated orthosis. Although at a considerably higher cost than the off-the-shelf orthosis, the custom articulated orthosis produced similar improvement in hindfoot inversion and forefoot plantar flexion but also resulted in more forefoot adduction. This was in contrast to the off-the-shelf orthosis, which was associated with greater forefoot abduction, and to the solid-ankle orthosis, which minimally improved forefoot abduction. It should be noted that relatively small changes in abnormal foot movement were observed with all the orthoses, despite, in some cases, expensive custom designs.
TABLE 2.
Descriptive Data for Each Kinematic Variable at the Midpoint of Each Rocker*
| Shoe Only | Off-the-Shelf Orthosis | Custom Solid-Ankle Orthosis | Custom Articulated-Ankle Orthosis | |
|---|---|---|---|---|
| First rocker | ||||
| Hindfoot eversion/inversion | −19.3 ± 0.0 | −17.4 ± 0.4 | −18.9 ± 0.4 | −17.0 ± 0.4 |
| Forefoot plantar flexion/dorsiflexion | −16.9 ± 2.5 | −20.5 ± 2.9 | −20.2 ± 0.9 | −19.6 ± 0.5 |
| Forefoot abduction/adduction | −5.0 ± 0.0 | −7.7 ± 1.2 | −4.2 ± 0.2 | −2.6 ± 0.8 |
| Second rocker | ||||
| Hindfoot eversion/inversion | −19.2 ± 0.2 | −16.5 ± 0.3 | −18.7 ± 0.6 | −16.8 ± 0.5 |
| Forefoot plantar flexion/dorsiflexion | −10.7 ± 0.6 | −16.8 ± 1.0 | −15.5 ± 0.8 | −16.7 ± 1.0 |
| Forefoot abduction/adduction | −4.9 ± 0.7 | −5.7 ± 1.3 | −3.9 ± 0.8 | −2.1 ± 1.4 |
| Third rocker | ||||
| Hindfoot eversion/inversion | −15.3 ± 0.0 | −14.3 ± 0.3 | −15.0 ± 0.6 | −15.9 ± 0.3 |
| Forefoot plantar flexion/dorsiflexion | −20.4 ± 0.2 | −23.4 ± 0.5 | −26.2 ± 0.5 | −23.4 ± 1.1 |
| Forefoot abduction/adduction | −8.5 ± 0.3 | −10.1 ± 1.1 | −7.6 ± 1.1 | −4.7 ± 1.4 |
Data are mean ± SD degrees. Positive values indicate hindfoot inversion, forefoot dorsiflexion, and forefoot adduction. First rocker, 0%–20% of stance; second rocker, 20%–80% of stance; third rocker, 80%–100% of stance. The 2SEM values were 1.2° for hindfoot eversion/inversion, 1.2° for forefoot plantar flexion/dorsiflexion, and 0.5° for forefoot abduction/adduction.
Acknowledgments
We thank the DJ Orthopedics Inc and the Arizona Company for providing the braces used in this study.
References
- 1.Alvarez RG, Marini A, Schmitt C, Saltzman CL. Stage I and II posterior tibial tendon dysfunction treated by a structured nonoperative management protocol: an orthosis and exercise program. Foot Ankle Int. 2006;27:2–8. doi: 10.1177/107110070602700102. [DOI] [PubMed] [Google Scholar]
- 2.Amaral De Noronha M, Borges NG., Jr Lateral ankle sprain: isokinetic test reliability and comparison between invertors and evertors. Clin Biomech (Bristol, Avon) 2004;19:868–871. doi: 10.1016/j.clinbiomech.2004.05.011. http://dx.doi.org/10.1016/j.clinbiomech.2004.05.011. [DOI] [PubMed]
- 3.Augustin JF, Lin SS, Berberian WS, Johnson JE. Nonoperative treatment of adult acquired flat foot with the Arizona brace. Foot Ankle Clin. 2003;8:491–502. doi: 10.1016/s1083-7515(03)00036-6. [DOI] [PubMed] [Google Scholar]
- 4.Blackwood CB, Yuen TJ, Sangeorzan BJ, Ledoux WR. The midtarsal joint locking mechanism. Foot Ankle Int. 2005;26:1074–1080. doi: 10.1177/107110070502601213. [DOI] [PubMed] [Google Scholar]
- 5.Butler RJ, Hillstrom H, Song J, Richards CJ, Davis IS. Arch height index measurement system: establishment of reliability and normative values. J Am Podiatr Med Assoc. 2008;98:102–106. doi: 10.7547/0980102. [DOI] [PubMed] [Google Scholar]
- 6.Chao W, Wapner KL, Lee TH, Adams J, Hecht PJ. Nonoperative management of posterior tibial tendon dysfunction. Foot Ankle Int. 1996;17:736–741. doi: 10.1177/107110079601701204. [DOI] [PubMed] [Google Scholar]
- 7.Churchill RS, Sferra JJ. Posterior tibial tendon insufficiency. Its diagnosis, management, and treatment. Am J Orthop. 1998;27:339–347. [PubMed] [Google Scholar]
- 8.Cole GK, Nigg BM, Ronsky JL, Yeadon MR. Application of the joint coordinate system to three-dimensional joint attitude and movement representation: a standardization proposal. J Biomech Eng. 1993;115:344–349. doi: 10.1115/1.2895496. [DOI] [PubMed] [Google Scholar]
- 9.Deland JT, de Asla RJ, Sung IH, Ernberg LA, Potter HG. Posterior tibial tendon insufficiency: which ligaments are involved? Foot Ankle Int. 2005;26:427–435. doi: 10.1177/107110070502600601. [DOI] [PubMed] [Google Scholar]
- 10.Eils E, Rosenbaum D. The main function of ankle braces is to control the joint position before landing. Foot Ankle Int. 2003;24:263–268. doi: 10.1177/107110070302400312. [DOI] [PubMed] [Google Scholar]
- 11.Elftman NW. Nonsurgical treatment of adult acquired flat foot deformity. Foot Ankle Clin. 2003;8:473–489. doi: 10.1016/s1083-7515(03)00119-0. [DOI] [PubMed] [Google Scholar]
- 12.Ferber R, Davis IM, Williams DS., 3rd Effect of foot orthotics on rearfoot and tibia joint coupling patterns and variability. J Biomech. 2005;38:477–483. doi: 10.1016/j.jbiomech.2004.04.019. http://dx.doi.org/10.1016/j.jbiomech.2004.04.019. [DOI] [PubMed]
- 13.Flemister AS, Neville CG, Houck J. The relationship between ankle, hindfoot, and forefoot position and posterior tibial muscle excursion. Foot Ankle Int. 2007;28:448–455. doi: 10.3113/FAI.2007.0448. http://dx.doi.org/10.3113/FAI.2007.0448. [DOI] [PubMed]
- 14.Gazdag AR, Cracchiolo A., 3rd Rupture of the posterior tibial tendon. Evaluation of injury of the spring ligament and clinical assessment of tendon transfer and ligament repair. J Bone Joint Surg Am. 1997;79:675–681. doi: 10.2106/00004623-199705000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Geideman WM, Johnson JE. Posterior tibial tendon dysfunction. J Orthop Sports Phys Ther. 2000;30:68–77. doi: 10.2519/jospt.2000.30.2.68. [DOI] [PubMed] [Google Scholar]
- 16.Genova JM, Gross MT. Effect of foot orthotics on calcaneal eversion during standing and treadmill walking for subjects with abnormal pronation. J Orthop Sports Phys Ther. 2000;30:664–675. doi: 10.2519/jospt.2000.30.11.664. [DOI] [PubMed] [Google Scholar]
- 17.Holmes GB, Jr, Mann RA. Possible epidemiological factors associated with rupture of the posterior tibial tendon. Foot Ankle. 1992;13:70–79. doi: 10.1177/107110079201300204. [DOI] [PubMed] [Google Scholar]
- 18.Houck JR, Nomides C, Neville CG, Samuel Flemister A. The effect of stage II posterior tibial tendon dysfunction on deep compartment muscle strength: a new strength test. Foot Ankle Int. 2008;29:895–902. doi: 10.3113/FAI.2008.0895. http://dx.doi.org/10.3113/FAI.2008.0895. [DOI] [PMC free article] [PubMed]
- 19.Imhauser CW, Abidi NA, Frankel DZ, Gavin K, Siegler S. Biomechanical evaluation of the efficacy of external stabilizers in the conservative treatment of acquired flatfoot deformity. Foot Ankle Int. 2002;23:727–737. doi: 10.1177/107110070202300809. [DOI] [PubMed] [Google Scholar]
- 20.Jennings MM, Christensen JC. The effects of sectioning the spring ligament on rearfoot stability and posterior tibial tendon efficiency. J Foot Ankle Surg. 2008;47:219–224. doi: 10.1053/j.jfas.2008.02.002. http://dx.doi.org/10.1053/j.jfas.2008.02.002. [DOI] [PubMed]
- 21.Johnson KA, Strom DE. Tibialis posterior tendon dysfunction. Clin Orthop Relat Res. 1989:196–206. [PubMed] [Google Scholar]
- 22.Klein P, Mattys S, Rooze M. Moment arm length variations of selected muscles acting on talocrural and subtalar joints during movement: an in vitro study. J Biomech. 1996;29:21–30. doi: 10.1016/0021-9290(95)00025-9. [DOI] [PubMed] [Google Scholar]
- 23.Kulig K, Burnfield JM, Requejo SM, Sperry M, Terk M. Selective activation of tibialis posterior: evaluation by magnetic resonance imaging. Med Sci Sports Exerc. 2004;36:862–867. doi: 10.1249/01.mss.0000126385.12402.2e. [DOI] [PubMed] [Google Scholar]
- 24.Kulig K, Reischl SF, Pomrantz AB, et al. Nonsurgical management of posterior tibial tendon dysfunction with orthoses and resistive exercise: a randomized controlled trial. Phys Ther. 2009;89:26–37. doi: 10.2522/ptj.20070242. http://dx.doi.org/10.2522/ptj.20070242. [DOI] [PubMed]
- 25.Lee MS, Vanore JV, Thomas JL, et al. Diagnosis and treatment of adult flatfoot. J Foot Ankle Surg. 2005;44:78–113. doi: 10.1053/j.jfas.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 26.Lin JL, Balbas J, Richardson EG. Results of non-surgical treatment of stage II posterior tibial tendon dysfunction: a 7- to 10-year followup. Foot Ankle Int. 2008;29:781–786. doi: 10.3113/FAI.2008.0781. http://dx.doi.org/10.3113/FAI.2008.0781. [DOI] [PubMed]
- 27.Logue JD. Advances in orthotics and bracing. Foot Ankle Clin. 2007;12:215–232. v. doi: 10.1016/j.fcl.2007.03.012. http://dx.doi.org/10.1016/j.fcl.2007.03.012. [DOI] [PubMed]
- 28.Maletsky LP, Sun J, Morton NA. Accuracy of an optical active-marker system to track the relative motion of rigid bodies. J Biomech. 2007;40:682–685. doi: 10.1016/j.jbiomech.2006.01.017. http://dx.doi.org/10.1016/j.jbiomech.2006.01.017. [DOI] [PubMed]
- 29.Marzano R. Functional bracing of the adult acquired flatfoot. Clin Podiatr Med Surg. 2007;24:645–656. vii. doi: 10.1016/j.cpm.2007.06.002. http://dx.doi.org/10.1016/j.cpm.2007.06.002. [DOI] [PubMed]
- 30.Myerson MS, Badekas A, Schon LC. Treatment of stage II posterior tibial tendon deficiency with flexor digitorum longus tendon transfer and calcaneal osteotomy. Foot Ankle Int. 2004;25:445–450. doi: 10.1177/107110070402500701. [DOI] [PubMed] [Google Scholar]
- 31.Ness ME, Long J, Marks R, Harris G. Foot and ankle kinematics in patients with posterior tibial tendon dysfunction. Gait Posture. 2008;27:331–339. doi: 10.1016/j.gaitpost.2007.04.014. http://dx.doi.org/10.1016/j.gaitpost.2007.04.014. [DOI] [PubMed]
- 32.Neville C, Flemister A, Tome J, Houck J. Comparison of changes in posterior tibialis muscle length between subjects with posterior tibial tendon dysfunction and healthy controls during walking. J Orthop Sports Phys Ther. 2007;37:661–669. doi: 10.2519/jospt.2007.2539. http://dx.doi.org/10.2519/jospt.2007.2539. [DOI] [PubMed]
- 33.Neville C, Flemister AS, Houck JR. Effects of the AirLift PTTD brace on foot kinematics in subjects with stage II posterior tibial tendon dysfunction. J Orthop Sports Phys Ther. 2009;39:201–209. doi: 10.2519/jospt.2009.2908. http://dx.doi.org/10.2519/jospt.2009.2908. [DOI] [PubMed]
- 34.Noll KH. The use of orthotic devices in adult acquired flatfoot deformity. Foot Ankle Clin. 2001;6:25–36. doi: 10.1016/s1083-7515(03)00077-9. [DOI] [PubMed] [Google Scholar]
- 35.Perry J. Gait Analysis: Normal and Pathological Function. Thorofare, NJ: SLACK Inc; 1992. [Google Scholar]
- 36.Ringleb SI, Kavros SJ, Kotajarvi BR, Hansen DK, Kitaoka HB, Kaufman KR. Changes in gait associated with acute stage II posterior tibial tendon dysfunction. Gait Posture. 2007;25:555–564. doi: 10.1016/j.gaitpost.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 37.Rosenfeld PF, Dick J, Saxby TS. The response of the flexor digitorum longus and posterior tibial muscles to tendon transfer and calcaneal osteotomy for stage II posterior tibial tendon dysfunction. Foot Ankle Int. 2005;26:671–674. doi: 10.1177/107110070502600902. [DOI] [PubMed] [Google Scholar]
- 38.Saltzman CL, Brandser EA, Berbaum KS, et al. Reliability of standard foot radiographic measurements. Foot Ankle Int. 1994;15:661–665. doi: 10.1177/107110079401501206. [DOI] [PubMed] [Google Scholar]
- 39.States RA, Pappas E. Precision and repeatability of the Optotrak 3020 motion measurement system. J Med Eng Technol. 2006;30:11–16. doi: 10.1080/03091900512331304556. http://dx.doi.org/10.1080/03091900512331304556. [DOI] [PubMed]
- 40.Tome J, Nawoczenski DA, Flemister A, Houck J. Comparison of foot kinematics between subjects with posterior tibialis tendon dysfunction and healthy controls. J Orthop Sports Phys Ther. 2006;36:635–644. doi: 10.2519/jospt.2006.2293. http://dx.doi.org/10.2519/jospt.2006.2293. [DOI] [PubMed]
- 41.Wacker J, Calder JD, Engstrom CM, Saxby TS. MR morphometry of posterior tibialis muscle in adult acquired flat foot. Foot Ankle Int. 2003;24:354–357. doi: 10.1177/107110070302400409. [DOI] [PubMed] [Google Scholar]
- 42.Williams DS, 3rd, McClay Davis I, Baitch SP. Effect of inverted orthoses on lower-extremity mechanics in runners. Med Sci Sports Exerc. 2003;35:2060–2068. doi: 10.1249/01.MSS.0000098988.17182.8A. http://dx.doi.org/10.1249/01.MSS.0000098988.17182.8A. [DOI] [PubMed]
- 43.Williams DS, McClay IS. Measurements used to characterize the foot and the medial longitudinal arch: reliability and validity. Phys Ther. 2000;80:864–871. [PubMed] [Google Scholar]
- 44.Younger AS, Sawatzky B, Dryden P. Radiographic assessment of adult flatfoot. Foot Ankle Int. 2005;26:820–825. doi: 10.1177/107110070502601006. [DOI] [PubMed] [Google Scholar]


