Abstract
Purpose
To evaluate the repeatability of Fourier-domain optical coherence tomography (FD-OCT) pachymetric mapping and compare OCT central corneal thickness (CCT) measurements with those of ultrasound pachymetry and Orbscan II.
Setting
Doheny Eye Institute, University of Southern California, Los Angeles, CA
Methods
An FD-OCT system (RTVue-CAM, Optovue Inc., Fremont, CA) was used to map the corneal thickness of fifty normal participants. The scans were centered on either the corneal vertex or pupil. The repeatability of central and pericentral map sectors were assessed by pooled standard deviation (SD). The CCT measured by OCT was compared with those measured by ultrasound and Orbscan II by paired t-test, Pearson correlation, and Bland-Altman analysis.
Results
Pupil centration (SD: 1.3 μm central, 1.8-3.8 μm pericentral) provided better repeatability than vertex centration (1.7 μm central, 2.4-5.7 μm pericentral) in all sectors (P<0.035). The CCT measured by OCT, ultrasound, and Orbscan II (acoustic factor 0.92) was 536.9±27.0, 556.6±30.5, and 537.2±32.6 μm, respectively. The CCT measured by OCT was significantly thinner than ultrasound pachymetric readings (P=0.007, mean difference −19.7 μm, 95% limits of agreement -40.4 to 0.9 μm) but not those of Orbscan II (P=0.2637, mean difference -0.3 μm, 95% limits of agreement -24.0 to 23.5 μm). The OCT CCT correlated well with those of ultrasound and Orbscan II (Pearson r = 0.940 and 0.934, respectively).
Conclusion
Pachymetric mapping with FD-OCT was highly repeatable. The repeatability was better with pupil-centered scans than with corneal vertex-centered scans. Ultrasound pachymetry, FD-OCT and Orbscan II should not be used interchangeably for the assessment of corneal thickness.
Introduction
The measurement of corneal thickness (pachymetry) has various important applications in monitoring corneal diseases such as corneal edema and keratoconus, measuring intraocular pressure, and managing ocular hypertension. It is also essential in considering eligibility for refractive surgical procedures such as LASIK and phototherapeutic keratectomy and in determining the amount of the correction that can safely be performed.
Traditional methods for measuring corneal thickness use spot pachymetry techniques, such as ultrasound pachymetry,1 specular and confocal microscopy,2 and optical low-coherence reflectometry.3 Ultrasound pachymetry is still the standard because of its reliability, ease of use, and relatively low cost.
Pachymetric mapping systems, such as the slit scanning tomography,4 Scheimpflug photography,4 or very-high frequency ultrasound imaging,5 provide several advantages over spot measurements. Mapping reveals corneal thickness over a wide area and allows easy visualization of abnormal patterns such as keratoconus and pellucid marginal degeneration. It also permits preoperative planning for surgeries that do not just involve the center of the cornea, such as astigmatic keratotomy, phototherapeutic keratectomy, and lamellar keratoplasty. Many surgeons use the slit scanning corneal topography/pachymetry (Orbscan II; Bausch & Lomb, Inc., Rochester, NY) to obtain pachymetry maps for refractive procedures. However, because of its limited resolution, the Orbscan slit scanning technology tends to underestimate corneal thickness in the presence of corneal opacities.6, 7
Optical coherence tomography (OCT) is a non-contact imaging technique based on principles of low-coherence interferometry.3 Its high axial resolution allows better delineation of the anterior and posterior surfaces of the cornea. Time-domain (TD) anterior segment OCT systems capable of generating pachymetric maps have been reported.8,9 Fourier domain OCT (FD-OCT), a newer generation of OCT, has acquisition speeds 10-100 times faster than TD-OCT systems.10-12 Its very high scan speed may minimize the effect of eye movement during data acquisition and improve the repeatability of the pachymetry maps.
We used a FD-OCT system with a scan speed of 26,000 axial scans/sec to image the cornea and generate pachymetry maps. In this study, we evaluate pachymetry map repeatability for both the central and peripheral corneal areas. We also compare the central corneal thickness (CCT) measured by three instruments: OCT, ultrasound pachymetry, and Orbscan II.
Methods
Subjects
Fifty normal volunteers were recruited for this study at the Doheny Eye Institute, Los Angles, CA. To participate in this study, subjects must have: no corneal pathology, no history of previous corneal surgery, and a best-corrected vision better than 20/25; they must not have worn contact lenses within the past three months; and they must be between 18 and 60 years of age.
This study followed the tenants of the Declaration of Helsinki, was in accord with the Health Insurance Portability and Accountability Act of 1996, and was approved by the Institutional Review Board of the University of Southern California. Written informed consent was obtained from all subjects. All measurements were taken at the same time of the day, between 10 am and 4 pm. The ultrasound measurement required contact with the eye and was performed last. Corneal thickness measurements were performed sequentially, using OCT, scanning-slit topography (Orbscan II), and ultrasonic pachymetry.
OCT Imaging
An FD-OCT system (RTVue, software version 4.0, Optovue Inc., Fremont, CA) with a corneal adaptor module (CAM) was used in this study. The system works at 830 nm wavelength and has a scan speed of 26,000 axial scans per second. The depth resolution of the FD-OCT system is 5 μm (full-width-half-maximum) in tissue. The CAM produced telecentric scanning for anterior segment imaging using either a wide-angle (long lens) or high-magnification (short lens) adaptor lens. We used the wide-angle lens, which provided a scan width of 6mm and a transverse resolution of 15 μm (focused spot size).
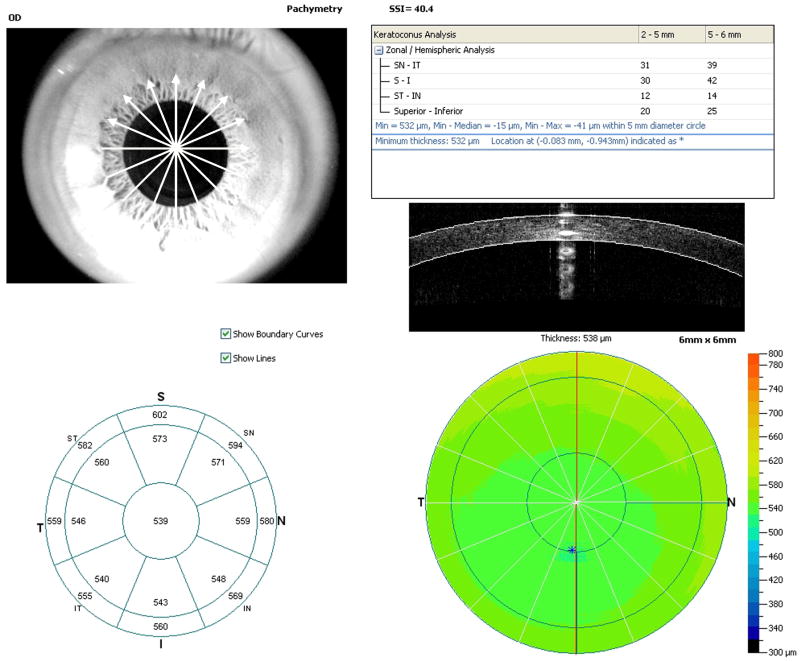
The “Pachymetry” scan pattern was used to map the cornea. The pattern consisted of 8 high-definition meridional scans (1024 axial scans per meridian) acquired in only 0.32 seconds (Figure 1, upper left). The corneal thickness profile was measured by an automated algorithm detecting the anterior and posterior corneal boundaries on the cross-sectional images. A 6-mm-diameter pachymetry map was then formed by interpolating the thickness profiles on the eight meridians. The maps (Figure 1, bottom) were divided into zones by octants and annular rings (2, 5, and 6 mm). The average pachymetry of each zone was displayed in the sector map (Figure 1, bottom left). The average pachymetry of the central 2 mm area was recorded as the CCT for OCT measurements. The sector average pachymetry of superior (S), superotemporal (ST), temporal (T), inferotemporal (IT), inferior (I), inferonasal (IN), nasal (N), and superonasal (SN) octants from 2 to 5 mm diameter were recorded as pericentral corneal thicknesses.
Figure 1.
Fourier-domain optical coherence tomography (OCT) pachymetry map printout.
Each eye was scanned three times within a single visit. All scans were performed with the subject in the sitting position. The subject's head was stabilized with a chin/forehead rest. The subject's gaze was fixed with an internal fixation target. The OCT and video camera images were displayed in real-time to aid alignment. Subjects were repositioned after each OCT scan.
To center the corneal mapping scans, the operator used one of the two landmarks: the corneal vertex and the pupil. To center the scan on the vertex, the operator adjust the position of the OCT probe until a bright vertical flare line was seen on the real-time OCT image and then moving the vertex flare to the center of the image. Alternatively, the operator could center the scan on the pupil using the real-time video image of the eye and the circular overlay. We used the corneal vertex to align the center of the scan pattern before May 2008 and switched to pupil centering afterwards.
Ultrasound Pachymetry and Orbscan II
For scanning-slit topography/tomography (Orbscan II, Bausch & Lomb, Rochester, NY), the patient was positioned with a chin rest and asked to look at a fixation target while the scan is performed. The Orbscan II projects vertical slit illumination onto the cornea at an angle of 45° and captured the slit sectional images on a video camera. Twenty slits are projected from the left and twenty from the right in a sequential fashion. Topography maps and pachymetry maps were generated by a computer software program. The acoustic equivalent correction factor of 0.92 was used according to manufacturer's recommendations. Central 2-mm corneal thickness was obtained from the Orbscan II pachymetry map for comparison.
After Orbscan II measurement, the cornea was anesthetized with topical 0.5% proparacaine hydrochloride and three consecutive central corneal measurements were made with an ultrasonic pachymeter (Corneo-Gage Plus, Sonogage, Cleveland, OH).
All measurements were carried out by a single examiner experienced in the use of all three devices.
Statistical Analysis
In scans acquired with pupil centration, we observed that the vertex flare was within 0.5 mm of the center of the scan in the great majority of normal subjects, indicating these two landmarks were very close. The OCT scans centering at the corneal vertex and the pupil were combined for CCT comparison with ultrasound pachymetry and Orbscan II. But OCT scans with different scan centers were separated for pericentral corneal thickness analysis and repeatability calculation.
Results were presented as mean ± standard deviations (SD). The CCT measured by OCT was compared with those measured by ultrasound pachymetry and Orbscan II by paired t-test, Pearson correlation, and Bland-Altman analysis.13 The generalized estimating equation (GEE)14 was used to account for the inter-eye correlation in the variance of t-test. The significance level was set at 0.05 for all the tests.
Repeatability of the OCT pachymetry map sector averages was assessed by the pooled standard deviation obtained from the multiple measurements on each eye. In general, let xij denote the jth measurement for the ith individual eye (i = 1,…, n, j = 1,…,ni), then the repeatability in terms of pooled standard deviation can be calculated as
where is the average measurement for the ith individual eye. We used two-sided F-test to compare the repeatabilities of the OCT pachymetry maps centered on corneal vertex and on pupil.
All statistical analysis was performed with SAS software version 9.1.3 (SAS Institute Inc., Cary, NC).
Results
Fifty normal subjects (22 male and 28 female, 32.9 ± 8.7 years of age [range 20 to 59 years]) were included in this study. The OCT pachymetry scan pattern was centered on the corneal vertex in 32 subjects (64 eyes) and on the pupil in 18 subjects (36 eyes). The average OCT CCT was 536.6 ± 28.5 μm for vertex centration and 537.2 ± 32.6 μm for pupil centration. The mean difference between OCT CCTs measured with two different scan centers was < 1 μm, hence two groups of OCT CCT measurements were combined for comparison with ultrasound pachymetry and Orbscan II. The CCT averaged 536.9 ± 27.0 μm by OCT, 556.6 ± 30.5 μm by ultrasound, and 537.2 ± 32.6 μm by Orbscan II for all subjects (Table 1).
Table 1.
Central corneal thickness measured by three instruments
| Number of eyes | OCT | Ultrasound | Orbscan II |
|---|---|---|---|
| 100 | 536.9 ± 27.0 | 556.6 ± 30.5 | 537.2 ± 32.6 |
OCT = optical coherence tomography, ultrasound = ultrasound pachymetry
All values of mean and standard deviation are in micrometers (μm).
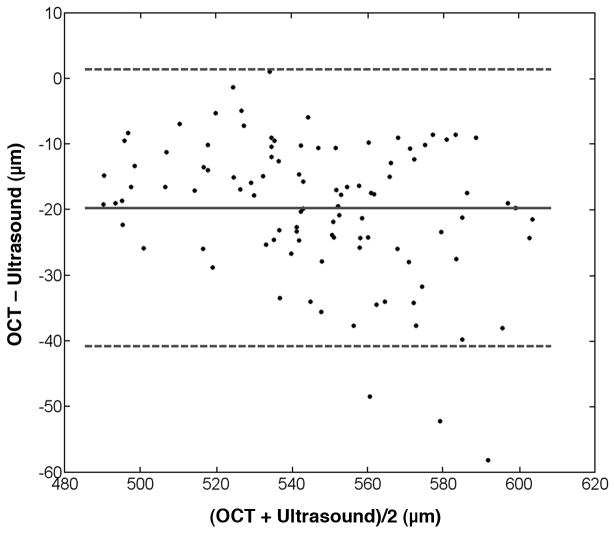
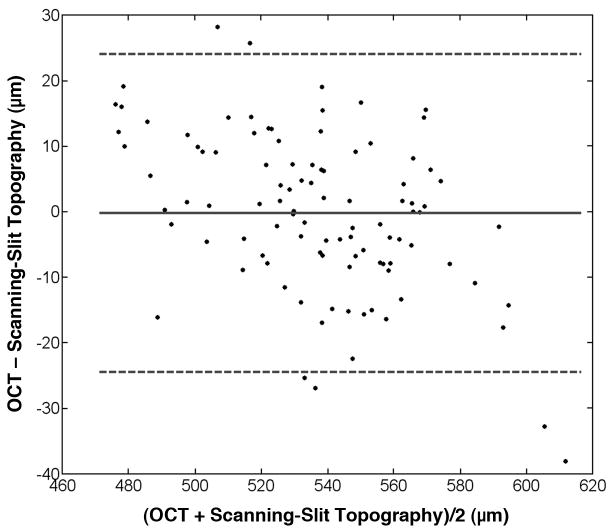
The GEE paired t-test showed that CCT measured by OCT was significantly thinner than ultrasound pachymetric readings (P = 0.007). These results were confirmed by Bland-Altman analysis (Figure 2). The mean difference was −19.7 μm with 95% limits of agreement from −40.4 to 0.9 μm. There was no statistically significant difference between OCT and Orbscan II central pachymetric measurements (GEE paired t-test p = 0.2637, mean difference −0.3 μm with 95% limits of agreement from −24.0 to 23.5 μm, Figure 3). The CCT measured by OCT correlated well with those measured by ultrasound pachymetry and Orbscan II (Pearson r = 0.940, 0.934, respectively).
Figure 2.
The Bland-Altman plot comparing OCT and ultrasound pachymetry central corneal thickness measurements. The mean difference was −19.7 μm (solid line) with 95% limits of agreement from -40.4 to 0.9 μm (dashed lines).
Figure 3.
The Bland-Altman plot comparing OCT and Orbscan II central corneal thickness measurements. The mean difference was -0.3 μm (solid line) with 95% limits of agreement from -24.0 to 23.5 μm (dashed lines).
The average OCT peripheral corneal thicknesses were grouped by different scan centers and listed by sectors in Table 2.
Table 2.
Corneal thickness in pericentral sectors measured by optical coherence tomography
| scan center | Number of eyes | T | ST | S | SN | N | IN | I | IT |
|---|---|---|---|---|---|---|---|---|---|
| Corneal vertex | 64 | 539.8 ± 27.9 | 551.8 ± 28.6 | 563.8 ± 29.8 | 565.5 ± 29.9 | 560.5 ± 29.9 | 552.9 ± 30.2 | 544.8 ± 30.1 | 538.3 ± 28.6 |
| Pupil | 36 | 544.3 ± 26.7 | 558.3 ± 27.1 | 570.0 ± 27.5 | 569.3 ± 26.9 | 560.4 ± 26.6 | 551.3 ± 25.9 | 544.8 ± 26.1 | 540.4 ± 26.3 |
T = temporal; ST = superotemporal; S = superior, SN = superonasal, N = nasal, IN = inferonasal, I = inferior, IT = inferotemporal
All values of mean and standard deviation are in micrometers (μm).
For OCT scans centered on the corneal vertex, the pachymetry map repeatability was 1.7 μm for CCT and 2.4–5.7 μm for pericentral measurements. For OCT scans centered on the pupil, the repeatability was 1.3 μm for CCT and 1.8–3.8 μm for the pericentral pachymetry. The pupil centration gave better pachymetry map repeatability than vertex centration in all sectors (P<0.035, Table 3).
Table 3.
Repeatability of the optical coherence tomography mapping by sector
| scan center | Central | T | ST | S | SN | N | IN | I | IT |
|---|---|---|---|---|---|---|---|---|---|
| Corneal vertex | 1.7 | 2.5 | 4.3 | 5.7 | 5.2 | 4.2 | 3.8 | 3.3 | 2.4 |
| Pupil | 1.3 | 1.9 | 2.8 | 3.7 | 3.8 | 3.1 | 2.8 | 2.2 | 1.8 |
| *P-value | 0.035 | 0.013 | <0.0001 | <0.0001 | 0.005 | 0.006 | 0.009 | <0.0001 | 0.003 |
P-value of the two-sided F-test
All values of repeatability measurements are in micrometers (μm).
Discussion
Optical coherence tomography relies on low coherence interferometry to generate cross-sectional images of the bio-tissue. The original OCT technology is now classified as time-domain OCT (TD-OCT), in which the reference mirror is moved mechanically through a range of delays to measure the reflectivity of the tissue. The scan speed in TD-OCT is limited by the mechanical cycle time of the reference mirror and the inefficiency of sequential signal detection. The scan speed of TD-OCT anterior segment imaging systems ranges from 200 axial scans per second (Heidelberg SL-OCT, Heidelberg Engineering, Vista, CA) to 2,000 axial scans per second (Visante, Carl Zeiss Meditec, Inc., Dublin, CA). Fourier-domain OCT has been developed to speed up image acquisition. In FD-OCT, the reference mirror is stationary and the axial scan is generated by Fourier transformation of spectral interferogram. The FD-OCT system used in this study was capable of a scan speed of 26,000 axial scans per second, more than ten times faster than the TD-OCT systems. This FD-OCT system also has an axial resolution of 5 μm, which is slightly more than 3 times better than the TD-OCT systems.
Faster scan speed can reduce data acquisition time, minimize eye movement during the scan, and improve the repeatability of the pachymetric measurements. In this study, intrasession repeatability was measured. Our results showed 1.3 – 1.7 μm repeatability for CCT measurements and 2.8 – 3.9 μm repeatability for pericentral corneal thickness measurements (averaged by octants in the 2-5 mm diameter ring). This performance was better than those reported for TD-OCT in the literature. Li et al 15 reported CCT intrasession repeatability of 4.9 μm and 5.8 μm with Visante OCT and SL-OCT, respectively. They also showed intersession reproducibility of 6.3 μm with Visante and 7.6 μm with SL-OCT. The axial-scan density was lower in their study (approximately 256 axial scans over a 16mm scan length). Similarly, Mohamed et al 16 evaluated repeatability of Visante OCT pachymetry measurements in terms of coefficient of variation (CV). They showed intrasession CVs of 0.3% (central) and 0.4% (25mm) and intersession CVs of 0.5% (central) and 0.6% (2-5 mm). The pooled SD measurements in our study were equivalent to intrasession CVs of 0.21-0.24% (central) and 0.31-0.37% (25mm). Thus our results support the hypothesis that the higher speed and resolution of FD-OCT over TD-OCT improved the repeatability of pachymetric mapping.
Prakash et al17 used an FD-OCT system similar to ours in their study and reported corneal thickness intersession reproducibility of 2.1 μm (central) and 3.6 μm (2-5 mm pericentral). Their OCT pachymetric maps were centered on the corneal vertex and their reproducibility numbers were similar to the repeatability we obtained with corneal vertex centration.
The two possible landmarks for centering the corneal map are the vertex and the pupil. In normal subjects, the corneal vertex and the center of the pupil are usually very close to each other. Therefore the normative data obtained with either centration methods could be combined. In a previous article, we defined pachymetry-based parameters for keratoconus screening: minimum, minimum-median, I-S, IT-SN corneal thicknesses, and the vertical location of the thinnest cornea.18 If there is one abnormal parameter, the cornea is suspicious for keratoconus. If there are two abnormal parameters, the eye is likely to have keratoconus or other ectactic conditions. The normal/keratoconic cutoff values were calculated by the parameters measured from normal subjects. The first-percentile IT-SN cutoff value calculated from the FD-OCT data in this study would be −51.5 μm for the scans centered on the corneal vertex and −51.2 μm for the scans centered on the pupil. Similarly, the I-S cutoff value would be −47.4 μm for vertex centration and −51.8 μm for pupil centration. The difference between cutoff values with two types of scan centration was less than 5 μm. This result suggested that we might combine the normal pachymetry scans obtained with both types of scan centration to build the normative database for keratoconus screening.
To map the cornea for surgical applications and for keratoconus screening, however, we recommend using the pupil as the primary centration reference. The vertex position can be altered by surgeries such as LASIK, photorefractive keratectomy, or phototherapeutic keratectomy; by diseases such as keratoconus; or by corneal scarring. Thus, if one wants to compare the difference in pachymetry maps before and after corneal surgery, using the pupil as the centration landmark allows the two maps to be registered correctly. In corneal scar cases, it is difficult to locate the corneal vertex due to the distorted corneal surface. In keratoconus, the ectasia is usually located inferotemporal and therefore the corneal vertex is also shifted inferotemporally. Thus using the pupil as the center might better reveal the asymmetric thinning in keratoconus.18 Since our results showed that pupil centration gave better repeatability than vertex centration, there is no reason to use vertex centration. We have changed our preferred centration landmark from the vertex to the pupil and also urge other investigators and clinicians to adapt pupil centration as the standard for OCT corneal mapping.
In this study, mean CCT values measured with ultrasound pachymetry were significantly larger than those measured with the FD-OCT system (19.7 μm) or Orbscan II (19.4 μm). This result agreed well with previous studies that used TD-OCT systems. Several investigators have reported that ultrasound pachymetry measured CCT was systematically thicker than that measured by TD-OCT: Ponce et al, 19 Visante OCT, 7.5 μm; Li et al, 9 Visante OCT, 14.4 μm; Zhao et al, 20 Visante OCT, 16.5 μm; Kim et al, 21 Heidelberge SL-OCT, 26.3 μm. Orbscan II uses an acoustic factor to correct its pachymetric readings. With a factory recommended acoustic factor of 0.92, which was also used in our study, the Hashemi and Rainer groups reported Orbscan II CCT measurements 21 μm and 19.8 μm smaller, respectively, than ultrasound pachymetry. Although we showed no statistically significant difference between CCTs measured by FD-OCT and Orbscan II (mean difference: -0.3 μm). The 95% limits of agreement of the two methods had a relatively large range (from -24.0 to 23.5 μm). Therefore, we suggest that ultrasound pachymetry, OCT, and Orbscan should not be used interchangeably for the assessment of corneal thickness.
The RTVue-CAM OCT only provides a pachymetry map of the central 6 mm diameter cornea. The 6-mm map size may be sufficient for planning myopic LASIK and photorefractive keratectomy since the central cornea tissue is ablated most for myopic refractive surgery procedures. It may be sufficient for keratoconus screening because a previous study22 showed that the cone apex was located inside the central 5 mm diameter in the vast majority of keratoconic eyes. However, the 6-mm map size is a limitation for diseases involving peripheral cornea, such as pellucid and Terrien's marginal degeneration. It may not be adequate for planning procedures involving the peripheral cornea, such as Intacs implantation or astigmatic keratotomy. A separate scan covering the periphery cornea has to be made to measure the corneal thickness outside the central 6-mm zone.
In summary, FD-OCT provided highly repeatable pachymetric map measurements both centrally and peripherally. Pupil-centration provided better repeatability than vertex centration. The FD-OCT, ultrasound pachymetry and Orbscan II should not be used interchangeably for the assessment of corneal thickness.
Acknowledgments
Financial Support: R24EY13015, R01EY018184, research grant from Optovue, Inc., grant from Research to Prevent Blindness, Charles C. Manger III, MD Chair in Corneal Laser Surgery endowment
Footnotes
Proprietary interests: David Huang received stock options, patent royalty and travel support from Optovue, Inc. (Fremont, CA). David Huang, Yan Li, and Maolong Tang received research grant support from Optovue. The other authors have no proprietary interest in the topic of this manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kozak I, Hornak M, Juhas T, et al. Changes in central corneal thickness after laser in situ keratomileusis and photorefractive keratectomy. J Refract Surg. 2003;19(2):149–53. doi: 10.3928/1081-597X-20030301-10. [DOI] [PubMed] [Google Scholar]
- 2.McLaren JW, Nau CB, Erie JC, Bourne WM. Corneal thickness measurement by confocal microscopy, ultrasound, and scanning slit methods. Am J Ophthalmol. 2004;137(6):1011–20. doi: 10.1016/j.ajo.2004.01.049. [DOI] [PubMed] [Google Scholar]
- 3.Huang D, Swanson EA, Lin CP, et al. Optical coherence tomography. Science. 1991;254(5035):1178–81. doi: 10.1126/science.1957169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ho T, Cheng AC, Rao SK, et al. Central corneal thickness measurements using Orbscan II, Visante, ultrasound, and Pentacam pachymetry after laser in situ keratomileusis for myopia. J Cataract Refract Surg. 2007;33(7):1177–82. doi: 10.1016/j.jcrs.2007.03.028. [DOI] [PubMed] [Google Scholar]
- 5.Reinstein DZ, Silverman RH, Trokel SL, Coleman DJ. Corneal pachymetric topography. Ophthalmology. 1994;101(3):432–8. doi: 10.1016/s0161-6420(94)31314-5. [DOI] [PubMed] [Google Scholar]
- 6.Prisant O, Calderon N, Chastang P, et al. Reliability of pachymetric measurements using orbscan after excimer refractive surgery. Ophthalmology. 2003;110(3):511–5. doi: 10.1016/S0161-6420(02)01298-8. [DOI] [PubMed] [Google Scholar]
- 7.Khurana RN, Li Y, Tang M, et al. High-speed optical coherence tomography of corneal opacities. Ophthalmology. 2007;114(7):1278–85. doi: 10.1016/j.ophtha.2006.10.033. [DOI] [PubMed] [Google Scholar]
- 8.Li Y, Shekhar R, Huang D. Corneal pachymetry mapping with high-speed optical coherence tomography. Ophthalmology. 2006;113(5):792–9. e2. doi: 10.1016/j.ophtha.2006.01.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li EY, Mohamed S, Leung CK, et al. Agreement among 3 methods to measure corneal thickness: ultrasound pachymetry, Orbscan II, and Visante anterior segment optical coherence tomography. Ophthalmology. 2007;114(10):1842–7. doi: 10.1016/j.ophtha.2007.02.017. [DOI] [PubMed] [Google Scholar]
- 10.Christopoulos V, Kagemann L, Wollstein G, et al. In vivo corneal high-speed, ultra high-resolution optical coherence tomography. Arch Ophthalmol. 2007;125(8):1027–35. doi: 10.1001/archopht.125.8.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yasuno Y, Madjarova VD, Makita S, et al. Three-dimensional and high-speed swept-source optical coherence tomography for in vivo investigation of human anterior eye segments. Opt Express. 2005;13:10652–10664. doi: 10.1364/opex.13.010652. [DOI] [PubMed] [Google Scholar]
- 12.Huang D, Izatt JA, Yasuno Y, de Boer JF. Future direction of anterior segment optical coherence tomography. In: Steinert RF, Huang D, editors. Anterior segment optical coherence tomography. SLACK, Inc.; 2008. [Google Scholar]
- 13.Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8(2):135–60. doi: 10.1177/096228029900800204. [DOI] [PubMed] [Google Scholar]
- 14.Zeger SL, Liang KY, Albert PS. Models for longitudinal data: a generalized estimating equation approach. Biometrics. 1988;44(4):1049–60. [PubMed] [Google Scholar]
- 15.Li H, Leung CK, Wong L, et al. Comparative study of central corneal thickness measurement with slit-lamp optical coherence tomography and visante optical coherence tomography. Ophthalmology. 2008;115(5):796–801. e2. doi: 10.1016/j.ophtha.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 16.Mohamed S, Lee GK, Rao SK, et al. Repeatability and reproducibility of pachymetric mapping with Visante anterior segment-optical coherence tomography. Invest Ophthalmol Vis Sci. 2007;48(12):5499–504. doi: 10.1167/iovs.07-0591. [DOI] [PubMed] [Google Scholar]
- 17.Prakash G, Agarwal A, Jacob S, et al. Comparison of fourier-domain and time-domain optical coherence tomography for assessment of corneal thickness and intersession repeatability. Am J Ophthalmol. 2009;148(2):282–90. e2. doi: 10.1016/j.ajo.2009.03.012. [DOI] [PubMed] [Google Scholar]
- 18.Li Y, Meisler DM, Tang M, et al. Keratoconus diagnosis with optical coherence tomography pachymetry mapping. Ophthalmology. 2008;115(12):2159–66. doi: 10.1016/j.ophtha.2008.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prospero Ponce CM, Rocha KM, Smith SD, Krueger RR. Central and peripheral corneal thickness measured with optical coherence tomography, Scheimpflug imaging, and ultrasound pachymetry in normal, keratoconus-suspect, and post-laser in situ keratomileusis eyes. J Cataract Refract Surg. 2009;35(6):1055–62. doi: 10.1016/j.jcrs.2009.01.022. [DOI] [PubMed] [Google Scholar]
- 20.Zhao PS, Wong TY, Wong WL, et al. Comparison of central corneal thickness measurements by visante anterior segment optical coherence tomography with ultrasound pachymetry. Am J Ophthalmol. 2007;143(6):1047–9. doi: 10.1016/j.ajo.2007.01.050. [DOI] [PubMed] [Google Scholar]
- 21.Kim HY, Budenz DL, Lee PS, et al. Comparison of central corneal thickness using anterior segment optical coherence tomography vs ultrasound pachymetry. Am J Ophthalmol. 2008;145(2):228–32. doi: 10.1016/j.ajo.2007.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tang M, Shekhar R, Miranda D, Huang D. Characteristics of keratoconus and pellucid marginal degeneration in mean curvature maps. Am J Ophthalmol. 2005;140(6):993–1001. doi: 10.1016/j.ajo.2005.06.026. [DOI] [PubMed] [Google Scholar]