Abstract
We investigated the relationship between health care expenditures for Special Health Care Needs (SHCN) children and family perception of financial burden. Using 2005/2006 National Survey of Children with Special Health Care Needs data, a multivariate logistic regression model was used to estimate the relationship between the SHCN child’s health care expenditure and perceived financial burden, while controlling for family and child characteristics. Our analysis suggests that health care expenditures for a SHCN child of $250 and more are associated with family perception of financial burden. In addition, families with lower socioeconomic status also perceived financial burden at lower level of expenditures. Members of the health care team who treat children with SHCN have an important role in understanding and assessing family financial burden as part of the care delivery to the child and the family. Our study reinforces the need to treat the whole family as the unit of care, especially when caring for children with special health care needs.
Keywords: children with special health care needs, financial burden, National Survey of Children with Special Health Care Needs, family centered care, health expenditures
Introduction
Children with special health care needs (SHCN), i.e. those who have or are at increased risk for a variety of chronic conditions, and who require health services beyond those required by children generally, typically experience higher health care utilization and expenditures than the average pediatric population (McPherson et al., 1998). These children often use more hospital days, emergency room visits, surgical or medical procedures, medical specialist visits, and home health days than non-SHCN children (Boulet, Boyles, & Schieve, 2009; Newacheck, Inkelas, & Kim, 2004). This extensive use of services may create a financial burden for many families (Boulet et al., 2009; Newacheck & Kim, 2005).
Families incur a broad range of expenses associated with a SHCN child’s health care. Families of children with SHCN conditions such as autism, muscular dystrophy, cystic fibrosis, heart problems, and emotional problems persistently have annual out-of-pocket medical expenditures (excluding insurance premiums) ranging from $2,669 to $69,906 compared to $676 to $3,181 for families with non-SHCN children (Buescher, Brunnsen, Whitmire, & Klutz-Hile, 2006; Newacheck et al., 2004; Shenkman, Knapp, Sappington, Vogel, & Schartz, 2007). Health insurance premiums can cost the family of a SHCN child an additional $2,058.00 to $3,593 annually depending on benefit plan type (Davidoff, 2004). There are also costs incurred by the family from added electricity, heating, and water needs, special clothing, equipment, food, other drugs, and expenses associated with medical appointments (Miedema, Easley, Fortin, Hamilton, & Mathews, 2008; Steele & Davies, 2006). For example, children who are unable to regulate their body temperature may require the heat be kept high or constant use of air conditioning. Extra laundry may be required for children with incontinence, vomiting, or constant drooling problems. Special wheelchair lifts and vans to transport children can range in price from $5,000 to $30,000 (Steele & Davies, 2006). The burden of these costs is magnified when care for the child means a loss in parental income due to missed work, not being able to work regular hours, not being able to work additional hours or overtime, having to change shifts with loss of pay differential, or quitting their jobs (Friedman, Hilden, & Powaski, 2005; Miedema et al., 2008; Montes & Halterman, 2008).
Expenditures such as these have resulted in approximately 40% of families with SHCN children experiencing financial-related burden due to their child’s health condition (Kuhlthau, Hill, Yucel, & Perrin, 2005). Family financial burden is defined as the family’s perception of financial stress and worry caused by inadequate monetary resources to meet the family’s fiscal demands (McCubbin & Patterson, 1983). Financial burden often emerges as a significant concern at a time when families are already consumed with the child’s health challenges. Family members who are preoccupied with financial burden may be distracted and less attentive to the child’s care needs (Kristjanson, Nikoletti, Porock, Smith, Lobchuk, & Pedler, 1998). In addition, financial burden may have long-term effects on the financial security, quality of life, and future well-being of the entire family (Miedema et al., 2008).
Few studies have explored family financial burden, particularly for families of SHCN children. These studies have investigated the relationship of health care expenditures and perceived family financial burden to child health insurance status (Chen & Newacheck, 2006; Yu, Dick, & Szilagyi, 2008), location of family residence (Shattuck & Parish, 2008; Skinner & Slifkin, 2007), and child health status (Kuhlthau et al., 2005). Although these studies have contributed to our knowledge of family and child factors associated with expenditures and financial burden, there is a lack of knowledge about the relationship of SHCN child health care expenditures to perceived family financial burden and at what level of health care expenditures families perceive financial burden. Therefore, the aims of this study were to investigate the relationship between health care expenditures for SHCN children and family perception of financial burden and to explore the moderating effect of income.
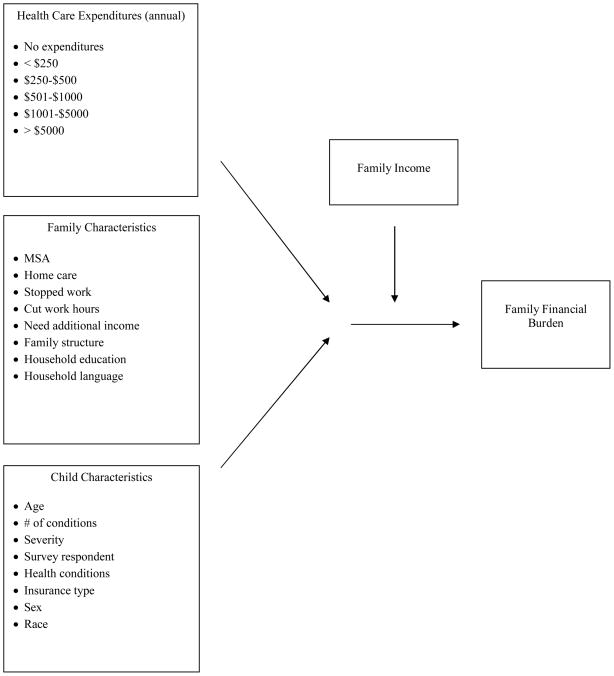
Figure 1 depicts the conceptual model of financial burden as a function of health care expenditures, family characteristics, and child characteristics. Health care expenditures require the family to have adequate monetary resources to meet these fiscal demands. When there are inadequate financial resources, families may perceive a burden (Davidoff, 2004; Kuhlthau et al, 2005; Shattuck & Parish, 2008; Skinner & Slifkin, 2007; Yu et al., 2008). In addition as expenditures increase, requiring greater financial resources, burden may also increase. Family response to the health care expenditures of the SHCN child depends on the amount of financial resources, such as income, the family has at its disposal. Those that do not have sufficient resources may perceive health care expenditures as a burden, whereas those with adequate resources may not perceive a burden (Kuhlthau et al., 2005).
Figure 1.
Conceptual Model of Family Financial Burden
The model also included selected family and child characteristics that might have a relationship to family financial burden. For example, Metropolitan statistical area was included because rural families may have limited employment opportunities, lower income, limited access to health, and limited health insurance coverage, which may increase family financial burden. (Skinner & Slifkin, 2007). Providing home care, stopped work, cut in hours worked, and need for additional income have all been shown to increase the likelihood of families perceiving or experiencing financial burden because they reflect the decreasing financial resources of the family (Heck & Makuc, 2000; Kuhlthau & Perrin, 2001; Kuhlthau et al., 2005; Vicker & Carlisle, 2000). Family structure was included because single adult families may have fewer financial resources than family structures with two adults, which may result in a greater likelihood of perceiving financial burden. Household education and household language were included because families with less education and those that lack English proficiency may have lower earning potential and fewer financial resources than those with more education and who speak English, increasing the likelihood of financial burden (Kuhlthau et al., 2005; Payne, Devol, & Smith, 2001).
Child characteristics such as age were included because younger children may utilize more health care services at the onset of their health condition causing the family to experience greater burden (Himelstein, 2006). Children with more health conditions may require more financial resources and place a greater financial burden on the family, so number of conditions was included in the model. Severity of the child’s health condition was included because a more severe condition may require more health care utilization resulting in greater financial burden for the family (Emmanuel, Fairclough, Slutsman, & Emmanuel, 2000; Kuhlthau et al., 2005; Newacheck, Hughes, Hung, Wong, & Stoddard, 2000). Because mothers are typically the caregivers to SHCN children, they may report more burden than other family members, so survey respondent was included (Buhse 2008; Knafl & Zoeller, 2000). As the number of health conditions increases, this may increase the financial burden for the family. Type of health condition was included because some health conditions such as heart problems may require more financial resources than others such as headaches/migraines and cause the family to perceive financial burden. When children have no health insurance or inadequate coverage, family financial burden may increase, so insurance type was included (Chen & Newacheck, 2006; Fox, McManus, & Reichman, 2002; Jeffrey & Newacheck, 2006). Sex and race were included because male and African-American children are more often afflicted with SHCN conditions, which has the potential to increase the likelihood of financial burden for the family (Newacheck, Strickland, Shonkoff, Perrin, McPherson, McManus, Lauver, Fox, & Arango, 1998)
Method
Design and Sample
Data from the 2005/2006 National Survey of Children with Special Health Care Needs (NS-CSHCN) were used for this analysis. The NS-CSHCN is a national telephone survey conducted during 2005–2006 of households with one or more children under 18 years old in all 50 states and the District of Columbia. A total of 364,841 children under 18 years old from 192,083 households were screened to identify those with special health care needs, and 40,723 detailed CSHCN interviews were collected. If the family had more than one child with SHCN, one child was randomly selected for completion of the survey.
Sample selection was based on the 40,723 child observations. Child observations were excluded from the sample if survey data were missing, interviewees refused to answer the survey question, or interviewees did not know the answer to the survey question. The final sample size was 18,135 children with special health care needs and their families. This sample was found to be representative of the original data set based on comparisons of respondents to non-respondents on several family and child characteristics.
Data Source
NS-CSHCN provided detailed state- and national-level parent-reported information on the health status and health care system experiences of children with special health care needs and their families (Child and Adolescent Health Measurement Initiative, 2005–2006). The NS-CSHCN is a nationwide telephone survey sponsored by the U.S. Department of Health and Human Services Administration Maternal and Child Health Bureau (MCHB), and conducted by the National Center for Health Statistics (NCHS) of the Centers for Disease Control and Prevention, using State and Local Area Integrated Telephone Survey (SLAITS) technology. Quality edits on the data included verification of the valid number of cases, assessment of the range of permissible values, and assessment of missing values.
Measures
Table 1 includes the study variables and definitions. Additional explanation of the variables of interested is discussed below.
Table 1.
Variable Definitions
| Variable | Definition |
|---|---|
| Health Care Expenditures | Any out-of-pocket payments for child’s health-related needs. |
| Family Characteristics | |
| MSA | Families reside in a rural or urban setting. (MSA 500,000 threshold) |
| Home care | Families provided health care at home. |
| Stopped work | Family member stopped working because of child’s health condition. |
| Cut work hours | Family member had to cut down on work hours because of child’shealth condition. |
| Need additional income | Family needed additional income to cover child’s medical expenses. |
| Family structure | Parental composition of family. |
| Household education | The highest level of school that anyone in the household completed or the highest degree anyone in the household received. (derived) |
| Income | Imputed poverty status of child’s household. (derived) |
| Household language | The primary language spoken in the home. |
| Child Characteristics | |
| Age | Age of child under the age of 18. |
| # of health conditions | Number of health conditions of the child. |
| Severity | A rating of the difficulties caused by child’s health condition. |
| Survey respondent | Relationship of survey respondent to child. (derived) |
| Health conditions | Child’s health conditions. |
| Insurance type | Child’s type of health insurance coverage at interview. |
| Sex | Gender of the child. |
| Race | Ethnicity of the child. (derived). |
| Financial Burden | Whether child’s condition caused financial problems for the family. |
Dependent Variable
Financial burden was measured as a yes/no response to the question of whether the SHCN child’s health condition caused financial problems for the family.
Independent Variable
Health care expenditures were defined as any out-of-pocket payments by the family for the medical care of the SHCN child. It included co-payments, dental or vision care, medications, special foods, adaptive clothing, durable equipment, home modifications, and any kind of therapy during the past 12 months. This did not include health insurance premiums or costs that were reimbursed by insurance or another source. This was measured as an ordered-categorical response from no expenses, less than $250, $250–$500, $501–$1,000, $1,001–$5,000, to more than $5,000 annually.
Control Variables - Family Characteristic
Home care was measured as a yes/no response to the question of whether the family provided any care to the child in the home such as changing bandages, care of feeding or breathing equipment, and giving medications and therapies. Family structure was defined as the parental structure of the family, and was measured as the categorical response of two biological/adopted parents, two step parents, mother only, or other structure. Income was derived from responses to the question of total combined household income for the previous calendar year. Responses were used to create an index of income relative to the Department of Health and Human Services Federal Poverty Guidelines (FPL) by the National Center for Health Statistics. This was measured as an ordered-categorical response from poor (<100% FPL), low income (100%–199% FPL), moderate income (200%–399% FPL), and high income (>400% FPL).
Control Variables - Child Characteristics
Severity of health condition was defined as the severity of the difficulties caused by the SHCN child’s health problems. Respondents were asked to rate the severity of the health condition from minor, moderate, to severe. If a child had more than one difficulty, the respondent was asked to rate the most severe difficulty rather than trying to average severity across all difficulties. Health conditions were measured as individual yes/no responses to a variety of health conditions that included asthma, attention deficit disorder/attention deficit hyperactivity disorder, autism/autism spectrum disorder, Downs syndrome, mental retardation/developmental delays, depression/anxiety/eating disorders/emotional problems, diabetes, heart problems/congenital heart disease, blood problems/anemia/sickle cell disease, cystic fibrosis, cerebral palsy, muscular dystrophy, epilepsy/seizure disorders, migraines, and arthritis/joint problems. The health condition of allergies was dropped from the model because of multicollinearity.
Data analysis
The primary question of interest was whether there was an association between SHCN child health care expenditures and family perception of financial burden. For all analyses, data were weighted to reflect the population of non-institutionalized CSHCN ages 0–17 years. Descriptive statistics were obtained on health care expenditures along with other family and child characteristics. Due to the binary nature of the financial burden variable, a multivariate logistic (logit) regression model with robust standard errors was used to estimate the relationship between the SHCN child’s health care expenditure and perceived financial burden, while controlling for family and child characteristics. Additional logistic regressions were used to explore how family income levels influenced the relationship between expenditures and burden controlling for family and child characteristics. Logistic regression analyses are presented in terms of adjusted odds ratios (ORs) and 95% confidence intervals (CIs). All analyses are conducted using Stata 10.0 software (Statcorp LP, College Station Texas, 2007).
Results
Table 2 summarizes the characteristics of 18,135 children with SHCN and their families. Over nineteen percent of the families perceived a financial burden associated the health condition of their SHCN child. Almost a quarter of the families spent over $1000 annually on their child’s medical care. Mothers completed the survey more often than fathers. A majority of families lived in urban areas and were composed of two biological or adopted parents. More than half the families were 200% of federal poverty level (FPL) or greater. English was the most common language spoken in the home, and the highest education level in the household was on average more than high school. Over 50% of the families reported that they did not provide home care, need additional income, cut work hours, or stop working because of their child’s health condition. A majority of children were male and almost 11 years old with approximately two health conditions. Sixty-three percent of the children had private insurance only and 75% were Caucasian.
Table 2.
Family and child demographic characteristics of study sample
| Variable | N | % |
|---|---|---|
| Financial Burden | ||
| No | 14562 | 80.3% |
| Yes | 3573 | 19.7% |
| Health Care Expenditures | ||
| No expenditures | 3736 | 20.6% |
| <$250 | 3681 | 20.3% |
| $250–$500 | 4443 | 24.5% |
| $501–$1000 | 2412 | 13.3% |
| $1001–$5000 | 3264 | 18.0% |
| >$5000 | 598 | 3.3% |
| MSA | ||
| Urban | 15016 | 82.8% |
| Rural | 3119 | 17.2% |
| Home Care | ||
| No | 9485 | 52.3% |
| Yes | 8650 | 47.7% |
| Stopped Work | ||
| No | 15505 | 85.5% |
| Yes | 2639 | 14.6% |
| Cut Work Hours | ||
| No | 14925 | 82.3% |
| Yes | 3210 | 17.7% |
| Need Additional Income | ||
| No | 14907 | 82.2% |
| Yes | 3228 | 17.8% |
| Family Structure | ||
| 2 biological/adopted parents | 9412 | 51.9% |
| 2 step parents | 2031 | 11.2% |
| Mother only | 5785 | 31.9% |
| Other family structure | 907 | 5.0% |
| Household Education | ||
| < High school | 1215 | 6.7% |
| High school | 4262 | 23.5% |
| > High school | 12658 | 69.8% |
| Income | ||
| Poor (<100% FPL) | 3627 | 20.0% |
| Low income (100–199% FPL) | 4135 | 22.8% |
| Moderate income (200–399% FPL) | 5441 | 30.0% |
| High income (>400% FPL) | 4915 | 27.1% |
| Household Language | ||
| English | 17373 | 95.8% |
| Non-english | 762 | 4.2% |
| Severity | ||
| Minor | 9557 | 52.7% |
| Moderate | 6909 | 38.1% |
| Severe | 1688 | 9.2% |
| Survey respondent | ||
| Mother | 15179 | 83.7% |
| Father | 2448 | 13.5% |
| Other family member | 508 | 2.8% |
| Health conditions | ||
| Asthma | 7943 | 43.8% |
| Attention deficit disorder | 6003 | 33.1% |
| Autism | 1016 | 5.6% |
| Downs syndrome | 199 | 1.1% |
| Mental retardation | 2231 | 12.3% |
| Emotional problems | 4280 | 23.6% |
| Diabetes | 236 | 1.3% |
| Heart problems | 617 | 3.4% |
| Blood problems | 472 | 2.6% |
| Cystic fibrosis | 54 | 0.3% |
| Cerebral palsy | 363 | 2.0% |
| Muscular dystrophy | 54 | 0.3% |
| Seizures | 598 | 3.3% |
| Migraines | 3210 | 17.7% |
| Joint problems | 9575 | 52.8% |
| Insurance type | ||
| Private only | 10645 | 58.7% |
| Public only | 5096 | 28.1% |
| Private/public | 1433 | 7.9% |
| Other insurance | 326 | 1.8% |
| Sex | ||
| Male | 10954 | 60.4% |
| Female | 7181 | 39.6% |
| Race | ||
| White only | 12803 | 70.6% |
| Black only | 3192 | 17.6% |
| Multi-race | 725 | 4.0% |
| Other race | 1415 | 7.8% |
Note: N=18135.
Table 3 displays the coefficients and odds ratios (OR) for the estimated logistic regression model of financial problems. Health care expenditures were positively associated with family perception of financial burden. The odds ratios on $250–$500 (OR 2.48, p=.001), $501–$1000 (OR 3.21, p=.001), $1001–$5000 (OR 5.59, p=.001) and greater than $5000 (OR 8.84, p=.001) were significantly and positively associated to family perception of financial burden. The odds of perceiving financial burden increased from 2 times for expenditures of $250–$500 (OR 2.48, p=.001) to almost 9 times for expenditures over $5000 (OR 8.84, p=.001) when compared to $0 expenditures controlling for family and child characteristics. The odds ratio on less than $250 (OR 1.23, p=.139) was not significant. This suggests that when family expenditures reach $250 or higher families perceive financial burden.
Table 3.
Logistic regression estimating family financial burden
| Variable | β | SE | Odds ratio | 95% Confidence Interval |
|---|---|---|---|---|
| Health Care Expenditures | ||||
| No expenditures | 0.00 | 1.00 | ||
| <$250 | 0.21 | (.14) | 1.23 | (0.95–1.61) |
| $250–$500 | 0.91** | (.14) | 2.48** | (1.89–3.28) |
| $501–$1000 | 1.17** | (.15) | 3.21** | (2.40–4.31) |
| $1001–$5000 | 1.72** | (.15) | 5.59** | (4.18–7.46) |
| >$5000 | 2.17** | (.19) | 8.84** | (6.08–12.85) |
| MSA | ||||
| Urban | 0.00 | 1.00 | ||
| Rural | 0.14 | (.08) | 1.15 | (0.97–1.36) |
| Home Care | ||||
| No | 0.00 | 1.00 | ||
| Yes | 0.36** | (.08) | 1.43** | (1.23–1.66) |
| Stopped Work | ||||
| No | 0.00 | 1.00 | ||
| Yes | 1.14** | (.10) | 3.14** | (2.61–3.78) |
| Cut Work Hours | ||||
| No | 0.00 | 1.00 | ||
| Yes | 0.65** | (.09) | 1.91** | (1.61–2.26) |
| Need Additional Income | ||||
| No | 0.00 | 1.00 | ||
| Yes | 2.05** | (.08) | 7.74** | (6.61–9.07) |
| Family Structure | ||||
| 2 biological/adopted parents | 0.00 | 1.00 | ||
| 2 step parents | −0.18 | (.12) | 0.84 | (0.67–1.05) |
| Mother only | 0.16 | (.09) | 1.17 | (0.98–1.40) |
| Other family structure | 0.08 | (.19) | 1.08 | (0.75–1.56) |
| Household Education | ||||
| < High school | −0.51** | (.18) | 0.60** | (0.42–0.85) |
| High school | −0.17 | (.10) | 0.85 | (0.69–1.03) |
| > High school | 0.00 | 1.00 | ||
| Income | ||||
| Poor (<100% FPL) | 1.07** | (.16) | 2.92** | (2.14–3.99) |
| Low income (100–199% FPL) | 1.16** | (.12) | 3.19** | (2.50–4.07) |
| Moderate income (200–399% FPL) | 0.86** | (.10) | 2.36** | (1.95–2.86) |
| High income (>400% FPL) | 0.00 | 1.00 | ||
| Household Language | ||||
| English | 0.00 | 1.00 | ||
| Non-english | 0.08 | (.22) | 1.08) | (0.71–1.65) |
| Age | 0.01 | (.01) | 1.01 | (1.00–1.03) |
| Number health conditions | −0.10 | (.08) | 0.97 | (0.78–1.05) |
| Severity | ||||
| Minor | 0.00 | 1.00 | ||
| Moderate | 0.54** | (.08) | 1.71** | (1.46–2.01) |
| Severe | 1.05** | (.13) | 2.87** | (2.21–3.73) |
| Survey Respondent | ||||
| Mother | 0.00 | 1.00 | ||
| Father | −0.10 | (.11) | 0.90 | (0.73–1.12) |
| Other family member | −0.38 | (.24) | 0.69 | (0.43–1.11) |
| Health Conditions | ||||
| Asthma | 0.19 | (.13) | 1.21 | (0.94–1.56) |
| Attention deficit disorder | 0.07 | (.11) | 1.07 | (0.85–1.34) |
| Autism | 0.13 | (.16) | 1.14 | (0.83–1.56) |
| Downs syndrome | 0.17 | (.32) | 1.89 | (0.64–2.21) |
| Mental retardation | −0.02 | (.15) | 0.98 | (0.74–1.31) |
| Emotional problems | 0.50** | (.11) | 1.65** | (1.32–2.09) |
| Diabetes | 0.51 | (.28) | 1.67 | (0.96–3.47) |
| Heart problems | 0.45* | (.18) | 1.57* | (1.10–2.22) |
| Blood problems | 0.33 | (.26) | 1.38 | (0.82–2.32) |
| Cystic fibrosis | 0.30 | (.46) | 1.35 | (0.55–3.33) |
| Cerebral palsy | −0.22 | (.25) | 0.80 | (0.49–1.31) |
| Muscular dystrophy | −0.17 | (.46) | 0.84 | (0.34–2.07) |
| Seizures | 0.32 | (.20) | 1.37 | (0.92–2.03) |
| Migraines | 0.23 | (.13) | 1.26 | (0.99–1.62) |
| Joint problems | 0.45** | (.17) | 1.57** | (1.12–2.20) |
| Insurance Type | ||||
| Private only | 0.00 | 1.00 | ||
| Public only | 0.10 | (.13) | 1.10 | (0.85–1.42) |
| Private/public | −0.01 | (.15) | 1.00 | (0.75–1.33) |
| Other insurance | 0.33 | (.24) | 1.39 | (0.87–2.23) |
| Sex | ||||
| Male | 0.00 | 1.00 | ||
| Female | −0.11 | (.07) | 0.89 | (0.77–1.04) |
| Race | ||||
| White only | 0.00 | 1.00 | ||
| Black only | −0.13 | (.12) | 0.88 | (0.70–1.11) |
| Multi-race | 0.31* | (.15) | 1.36* | (1.01–1.84) |
| Other race | 0.03 | (.16) | 1.03 | (0.76–1.41) |
Note: N=18135.
p<.05
p<.01
Families with lower incomes perceived financial burden at lower level of health care expenditures than families with higher income as displayed on Table 4. For poor and low income families, the odds ratios on $250–$500, $501–$1000, $1001–$5000 and greater than $5000 were significantly and positively associated to family perception of financial burden. For moderate income families, $1001–$5000 and greater than $5000 were significantly and positively associated to family perception of financial burden. For high income families, expenditures greater than $5000 were significantly and positively associated to family perception of financial burden. This suggests that as family income decreases, lower levels of expenditures are associated with financial burden.
Table 4.
Logistic regression estimating family financial burden by income status
| Variable | Overall Model O.R. (95% CI) | Poor O.R. (95% CI) | Low Income O.R. (95% CI) | Moderate Income O.R. (95% CI) | High Income O.R. (95% CI) |
|---|---|---|---|---|---|
| No expenditures | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| <$250 | 1.23 (.95–1.61) | 1.24 (.82–1.87) | 1.41 (.90–2.21) | 0.75 (.41–1.38) | 0.76 (.28–2.05) |
| $250–$500 | 2.48** (1.89–3.28) | 4.05** (2.64–6.21) | 2.59** (1.64–4.06) | 1.41 (.79–2.52) | 0.89 (.35–2.23) |
| $501–$1000 | 3.21** (2.40–4.31) | 5.13** (2.81–9.37) | 3.39** (2.03–5.64) | 1.97 (1.12–3.44) | 1.35 (.56–3.28) |
| $1001–5000 | 5.59** (4.18–7.46) | 5.78** (3.20–10.47) | 5.73** (3.40–9.66) | 3.81** (2.22–6.55) | 2.12 (.89–5.06) |
| >$5000 | 8.84** (6.08–12.85) | 4.42* (1.03–19.94) | 8.22** (3.21–21.03) | 7.18** (3.58–14.42) | 3.43** (1.38–8.54) |
Note: N=18135.
p<.05
p<.01
Several family characteristics were significantly associated with increased odds of family financial burden. These included providing home care (OR 1.42, p=.001), parents stopping work (OR 3.14, p=.001), cuts in parental working hours (OR 1.91, p=.001), the need for additional income (OR 7.74, p=.001), poor (OR 2.92, p=.001), low income FPL (OR 3.190, p=.001), moderate income (OR 2.36, p=.001). However, when household education level was less than high school, families had decreased odds of perceiving family financial burden (OR .60, p=.004).
Child characteristics significantly associated with family financial burden were moderately severe health conditions (OR 1.71, p=.001), severe health conditions (OR 2.87, p=.001) emotional problems (OR 1.65, p=.001) heart problems (OR 1.57, p=.012), joint problems (OR 1.57, p=.008), and multi-racial ethnicity (OR 1.36, p=.044). Controlling for other factors, rural, age, type of health conditions, number of health conditions, sex, insurance type, survey respondent, family structure, household language, and black/other race had no significant relationship with financial burden.
Discussion
Our analysis of the 2005/2006 National Survey of Children with Special Health Care Needs data suggests that health care expenditures for a SHCN child of $250 and more are associated with family perception of financial burden. Several studies have suggested that spending 10% of family income on health care equated to financial burden (Emmanuel et al., 2000; Yu et al, 2008); however, our study found a relatively low level of expenditure associated with the onset of financial burden, especially when compared to other household expenses like cell phones ($756 annually) or groceries ($8513 annually) (Entension, 2008; Fiercewireless, 2007). While this expenditure amount may be relatively small in comparison to other household expenses, families with SHCN may in fact be financially stretched because of many years of persistently costly care resulting in lower expenditures causing the perceptions of problems (Himmelstein, Warren, Thorne, & Woolhandler, 2005). Couple the amount of these expenditures with 2007 national trends in growing personal debt and decreased financial reserves such as savings, and these families may lack adequate financial resources to support them in the care of a SHCN child (Hoover, 2009; Kim, 2009).
We also found that whether or not the family perceived a financial burden depended on the amount of financial resources the family had at its disposal. Those that did not have sufficient resources from income perceived health care expenditures as a burden, whereas those with adequate resources did not perceive a burden. Several studies have suggested that families of low socioeconomic status have difficulties adjusting to and coping with stressors (Payne et al., 2001). These low socioeconomic status families have demonstrated decreased adherence to treatment and increased rates of anxiety and depression (Brownridge & Fielding, 1994; Fielding & Brownridge, 1999). Our findings suggest that health care expenditures may act as a family stressor, and that lower socioeconomic families may not have the skills and resources to adequately cope with the cost of caring for a SHCN child.
There were other interesting findings from our analysis regarding family characteristics. Families that experienced reduced financial resources because of lost income from either a cut in work hours or having to stop work perceived greater financial burden, and often responded that they needed additional income to cover medical expenditures. Meeting the fiscal demands of health care expenditures with decreased financial resources may result in families selling assets, taking out loans or mortgages, using savings, or seeking additional employment (Emanuel, et al., 2000). Those families unable to meet the fiscal demands may find personal bankruptcy the only remaining option (Himmelstein et al., 2005). Families may also be caught in a Catch-22. Reestablishing financial well-being may be hindered by decreased employability and loss of career advancement and mobility caused by being out of the work place for any extended period to care for the child (Miedema et al., 2008).
Several of the findings about child characteristics are also worth noting. The severity of the child’s health condition contributed significantly to the family’s perception of burden. The more severe the child’s health condition, the higher the odds of the family perceiving financial problems. This finding was congruent with those of others (Emmanuel et al., 2000; Kuhlthau et al., 2005), suggesting that children with moderate to severe SHCN may require expensive medications, medical supplies, and medical equipment (Miedema et al., 2008; Steele & Davies, 2006) which may not be fully covered by insurance and increase the family’s out-of-pocket expenditures. Child health conditions such as emotional problems, heart problems, and joint problems also influenced family perception of financial burden. This raises the question of whether insurance is adequately covering these expenses. For example, in many private benefit plans, mental health coverage for emotional problems is very limited (Martocchio, 2006). While studies have investigated the importance of insurance coverage for SCHN children, future research into specific benefit coverage levels would provide further insight into family financial burden (Chen & Newacheck, 2006; Davidoff, 2004). We were also surprised that most of the health conditions were not associated with perceived burden perhaps suggesting that families do not always perceive their child’s health as a burden (Knafl, Brietmayer, Gallo, & Zoller, 1996). As an example, families with diabetic children may have a thriving or accommodating family management style that views the health condition as life-goes-on as opposed to stressful and serious.
This study had several limitations. First, the cross-sectional nature of the survey does not allow for causal conclusions to be drawn about the relationships between the variables. Second, the data were respondent-reported and were estimates based on their recollection over the past 12 months. Therefore, reporting bias may be present. Third, there was no measure of actual family income in the NS-CSHCN. Measures of income were derived from responses to the question of total combined household income for the previous calendar year, and were used to create an index of income relative to the Department of Health and Human Services Federal Poverty Guidelines (FPL) by the National Center for Health Statistics. Thus, we were not able to calculate the relative burden or expenditures as a percentage of income, only the absolute burden (Shattuck & Parish, 2008).
The goal of this study was to improve our understanding of family financial burden by examining the relationship between health care expenditures for SHCN children and family financial burden. At a relatively low expenditure level, families perceived financial burden, which increased as expenditures increased. In addition, families with lower socioeconomic status also perceived financial burden at lower level of expenditures. We also found that based on family and child factors, these families may not have adequate financial resources either through income or insurance coverage to adequately manage the financial burden caused by caring for their SHCN child. These families may need assistance with coping and adjusting to the financial consequences of providing health care for their SHCN child (Witt-Sherman, 1998). Members of the care team who treat children with SHCN have an important role in understanding and assessing family financial burden as part of the care delivery to the child and the family. Our study reinforces the need to treat the whole family as the unit of care, especially when caring for children with special health care needs.
Acknowledgments
This publication was made possible by Grant Number T32NR008856 from the National Institute of Nursing Research (NINR). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institute of Nursing Research, National Institutes of Health.
Contributor Information
Lisa C. Lindley, Email: llindley@email.unc.edu, School of Nursing, University of North Carolina – Chapel Hill, Carrington Hall, CB 7460, Chapel Hill, NC 27599-7460
Barbara A. Mark, School of Nursing, University of North Carolina – Chapel Hill, Carrington Hall, CB 7460, Chapel Hill, NC 27599-7460
References
- Boulet S, Boyle C, Schieve L. Health Care Use and Health and Functional Impact of Developmental Disabilities Among US Children, 1997–2005. Archives of Pediatric & Adolescent Medicine. 2009;163:19–26. doi: 10.1001/archpediatrics.2008.506. [DOI] [PubMed] [Google Scholar]
- Brownbridge G, Fielding D. Psychosocial adjustment and adherence to dialysis treatment regimes. Pediatric Nephrology. 1994;8:744–749. doi: 10.1007/BF00869109. [DOI] [PubMed] [Google Scholar]
- Buescher P, Brunnsen S, Whitmire J, Klutz-Hile C. Children who are medically fragile in North Carolina: Using Medicaid data to estimate prevalence and medical care costs in 2004. Maternal Child Health. 2006;10:461–466. doi: 10.1007/s10995-006-0081-3. [DOI] [PubMed] [Google Scholar]
- Buhse M. Assessment of caregiver burden in families of persons with multiple sclerosis. Journal of Neuroscience Nursing. 2008;40:25–31. doi: 10.1097/01376517-200802000-00005. [DOI] [PubMed] [Google Scholar]
- Chen A, Newacheck P. Insurance coverage and financial burden for families of children with special health care needs. Ambulatory Pediatrics. 2006;6:204–209. doi: 10.1016/j.ambp.2006.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Child and Adolescent Health Measurement Initiative. National Survey of Children with Special Health Care Needs Indicator Data Set. Data Resource Center for Child and Adolescent Health; 2005–2006. [Google Scholar]
- Davidoff A. Insurance for children with special health care needs: Patterns of coverage and burden on families to provide adequate insurance. Pediatrics. 2004;114:394–403. doi: 10.1542/peds.114.2.394. [DOI] [PubMed] [Google Scholar]
- Emmanuel E, Fairclough D, Slutsman J, Emmanuel L. Understanding economic and other burdens of terminal illness: The experience of patients and their caregivers. Annals of Internal Medicine. 2000;132:451–459. doi: 10.7326/0003-4819-132-6-200003210-00005. [DOI] [PubMed] [Google Scholar]
- Extension. Tips to help lower the grocery bill. 2008 Retrieved February 5, 2009, from http://www.extension.org/pages/Tips_to_Help_Lower_the_Grocery_Bill.
- Fielding D, Brownbridge G. Factors related to psychosocial adjustment in children with end-stage renal failure. Pediatric Nephrology. 1999;13:766–770. doi: 10.1007/s004670050695. [DOI] [PubMed] [Google Scholar]
- Fiercewireless. J.D. Power and Associates Reports: Feature-Rich Wireless Mobile Phones Increase Average Consumer Service Spending for Both Hands. 2007 Retrieved February 5, 2009 from http://www.fiercewireless.com/press-releases/j-d-power-and-associates-reports-feature-rich-wireless-mobile-phones-increase-average?utm_medium=nl&utm_source=internal.
- Fox H, McManus M, Reichman M. The Strengths and Weaknesses of Private Health Insurance Coverage for Children with Special Health Care Needs. Maternal and Child Health Policy Research Center -Issues Brief. 2002:1–61. [Google Scholar]
- Freidman D, Hilden J, Powaski K. Issues and challenges in palliative care for children with cancer. Current Pain and Headache Reports. 2005;4:249–255. doi: 10.1007/s11916-005-0032-5. [DOI] [PubMed] [Google Scholar]
- Heck KE, Makuc DM. Parental employment and health insurance coverage among school-aged children with special health care needs. American Journal of Public Health. 2000;90:1856–1860. doi: 10.2105/ajph.90.12.1856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himelstein BP. Palliative care for infants, children, adolescents, and their families. Journal of Palliative Medicine. 2006;9:163–181. doi: 10.1089/jpm.2006.9.163. [DOI] [PubMed] [Google Scholar]
- Himmelstein DU, Warren E, Thorne D, Woolhandler S. Illness and injury as contributors to bankruptcy. Health Affairs, Suppl Web Exclusives. 2005:W65-63–W65-73. doi: 10.1377/hlthaff.w5.63. [DOI] [PubMed] [Google Scholar]
- Hoover Facts on Policy. 2009 Retrieved February 5, 2009 from http://www.hoover.org/research/factsonpolicy/facts/4250756.html.
- Jeffrey A, Newacheck P. Role of insurance for children with special health needs: A synthesis of the evidence. Pediatrics. 2006;118:1027–1038. doi: 10.1542/peds.2005-2527. [DOI] [PubMed] [Google Scholar]
- Kim K. Savings and Debt. 2009 Retrieved February 5, 2009 from http://moneycentral.msn.com/content/SavingandDebt/P70581.
- Knafl K, Brietmayer B, Gallo A, Zoeller L. Family response to childhood chronic illness: Description of management styles. Journal of Pediatric Nursing. 1996;11:315–326. doi: 10.1016/S0882-5963(05)80065-X. [DOI] [PubMed] [Google Scholar]
- Knafl K, Zoeller L. Childhood chronic illness: a comparison of mothers’ and fathers’ experiences. Journal of Family Nursing. 2000;6:287–302. [Google Scholar]
- Kristjanson L, Nikoletti S, Porock D, Smith M, Lobchuk M, Pedler P. Congruence between patients’ and family caregivers’ perceptions of symptom distress in patients with terminal cancer. Journal of Palliative Care. 1998;14:24–32. [PubMed] [Google Scholar]
- Kuhlthau K, Hill K, Yucel R, Perrin J. Financial burden for families of children with special health care needs. Maternal & Child Health Journal. 2005;9:207–218. doi: 10.1007/s10995-005-4870-x. [DOI] [PubMed] [Google Scholar]
- Kuhlthau K, Perrin J. Child health status and parental employment. Archives of Pediatric & Adolescent Medicine. 2001;155:1346–1350. doi: 10.1001/archpedi.155.12.1346. [DOI] [PubMed] [Google Scholar]
- Martocchio J. Employee Benefits. New York: McGraw-Hill; 2006. [Google Scholar]
- McCubbin I, Patteron J. The family stress process: The double ABCX model of adjustment and adaption. In: Sussman M, editor. Social Stress and the Family: Advances and Developments in family Stress Theory and Research. Philadelphia: Haworth Press; 1983. pp. 7–38. [Google Scholar]
- McPherson M, Arango P, Fox H, Lauver C, McManus M, Newacheck P, et al. A new definition of children with special health care needs. Pediatrics. 1998;102:137–139. doi: 10.1542/peds.102.1.137. [DOI] [PubMed] [Google Scholar]
- Miedema M, Easley J, Fortin P, Hamilton R, Mathews M. The economic impact on families when a child is diagnosed with cancer. Current Oncology. 2008;15:173–178. doi: 10.3747/co.v15i4.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montes G, Halterman J. Association of childhood autism spectrum disorders and loss of family income. Pediatrics. 2008;121:e821–e826. doi: 10.1542/peds.2007-1594. [DOI] [PubMed] [Google Scholar]
- Newacheck P, Hughes D, Hung Y, Wong S, Stoddard J. The unmet health needs of America’s children. Pediatrics. 2000;105:989–997. [PubMed] [Google Scholar]
- Newacheck P, Inkelas M, Kim S. Health services use and health care expenditures for children with disabilities. Pediatrics. 2004;114:79–85. doi: 10.1542/peds.114.1.79. [DOI] [PubMed] [Google Scholar]
- Newacheck P, Kim S. A national profile of health care utilization and expenditures for children with special health care needs. Archives of Pediatric & Adolescent Medicine. 2005;159:10–17. doi: 10.1001/archpedi.159.1.10. [DOI] [PubMed] [Google Scholar]
- Newacheck P, Strickland B, Shonkoff J, Perrin J, McPherson M, McManus M, Lauver C, Fox H, Arango P. An epidemiologic profile of children with special health care needs. Pediatrics. 1998;102:117–123. doi: 10.1542/peds.102.1.117. [DOI] [PubMed] [Google Scholar]
- Payne R, DeVol P, Smith T. Aha! Process. Highlands, TX: 2001. Bridges Out of Poverty. [Google Scholar]
- Shattuck P, Parish S. Financial burden in families of children with special health care needs: Variability among states. Pediatrics. 2008;122:13–18. doi: 10.1542/peds.2006-3308. [DOI] [PubMed] [Google Scholar]
- Shenkman E, Knapp C, Sappington D, Vogel B, Schatz D. Persistence of high health care expenditures among children in Medicaid. Medical Care Research and Review. 2007;64:304–330. doi: 10.1177/1077558707299864. [DOI] [PubMed] [Google Scholar]
- Steele R, Davies B. Impact on parents when a child has a progressive, life-threatening illness. International Journal of Palliative Nursing. 2006;12:576–585. doi: 10.12968/ijpn.2006.12.12.22544. [DOI] [PubMed] [Google Scholar]
- Skinner A, Slifkin R. Rural/urban differences in barriers to and burden of care for children with special health care needs. Children & Youth. 2007;23:150–157. doi: 10.1111/j.1748-0361.2007.00082.x. [DOI] [PubMed] [Google Scholar]
- Witt-Sherman D. Reciprocal suffering: The need to improve family caregivers’ quality of life through palliative care. Journal of Palliative Medicine. 1998;1:357–366. doi: 10.1089/jpm.1998.1.357. [DOI] [PubMed] [Google Scholar]
- Vickers J, Carlisle C. Choices and control: parental experiences in pediatric terminal home care. Journal of Pediatric Oncology Nursing. 2000;17:12–21. doi: 10.1177/104345420001700103. [DOI] [PubMed] [Google Scholar]
- Yu H, Dick A, Szilagyi P. Does public insurance provide better financial protection against rising health care costs for families of children with special health care need? Medical Care. 2008;46:1064–1070. doi: 10.1097/MLR.0b013e318185cdf2. [DOI] [PubMed] [Google Scholar]