Substance use disorders (SUDs), such as alcohol and cannabis, are serious addictive disorders, given their association with many adverse short-term and long-term consequences (Grant & Dawson, 1997; Hawkins, Catelano, & Miller, 1992; Hingson, Heeren, Zakocs, Kopstein, & Wechsler, 2002). Research has shown that alcohol and drug use increases during adolescence and reaches its peak in late adolescence and early adulthood (Bates & Labouvie, 1997; Chassin, Pitts, & Prost, 2002; Chassin, Flora, & King, 2004; Chen & Kandel, 1995; Winters & Lee, 2008), and that alcohol abuse and dependence are most prevalent in young adulthood (Guo, Hawkins, Hill, & Abbott, 2001). However, this period of heightened risk for intensive alcohol and other drug use often is followed by normative decreases in use during the late twenties or early thirties (Bates, 2000; Bennett, McCrady, Johnson, & Pandina, 1999; DeWit, Adlaf, Offord, & Ogborne, 2000).
Although most of the adolescent drug users do not proceed to disorders such as abuse or dependence (Jennison & Johnson, 2001), increasing attention has been given to individual differences in the paths and trajectories of developing SUDs across the life span. For example, there is growing interest in identifying trajectory patterns of SUDs as a young person ages from adolescence into adulthood (e.g., Chassin et al., 2002; Schulenberg, O’Malley, Bachman, Wadsworth, & Johnson, 1996). To date most trajectory research suggests that the long-term course of SUDs is highly variable (e.g., Brown, D’Amico, McCarthy, & Tapert, 2001; Chung, Martin, Grella, Winters, Abrantes, & Brown, 2003). In an adolescent clinical sample followed over 3 years, Martin, Maisto, Pollock, and Cornelius (2000) reported that transitions in the status of SUDs suggested particular patterns of diagnosing; that is, dependent adolescents were equally likely to remain dependent or remit to no diagnosis, adolescents with abuse were more likely to remain abusers or remit to no diagnosis, and those with no SUD at baseline had a high likelihood of maintaining this status. Transition probabilities were fairly stable across 1- and 3-year follow-ups.
One area lacking in the trajectory literature is the link between trajectories of SUDs and psychosocial risk factors. Based on risk cumulation theory, as risk factors, whether specific or nonspecific to drugs, continue to cumulate, they operate in concert in encouraging the development of an expectancy structure that is positive toward use and abuse of drugs, which ultimately may produce the outcome of earlier onset of drug use and/or developing drug abuse or dependence (Hops, Andrews, Duncan, Duncan, & Tildesley, 2000). Also, this cumulation of risk factors, considered as a “nesting structure” (Zucker, Fitzgerald, & Moses, 1995) in certain ecological and familial contexts, very likely contributes to persistence of psychopathological outcomes such as SUDs, suggesting the existence of developmental trajectories. Therefore, prevention or treatment intervention approaches may benefit from greater specificity of psychosocial factors that may act individually or together in predicting different trajectory groups of SUDs.
Thanks to the recent advances in techniques for identifying distinct developmental trajectories among a heterogeneous sample, longitudinal studies are on the increase incorporating both variable- and person-centered approaches that focus on developmental problems such as delinquent behavior (McDermott & Nagin, 2001; Nagin, 1999), binge drinking (Hill, White, Chung, Hawkins, & Catalano, 2000; Schulenberg et al., 1996; Chassin et al., 2002; Tucker, Orlando, & Ellickson, 2003), use of drugs such as cannabis (Kandel & Chen, 2000), and SUDs (Jackson, Sher, & Wood, 2000; Chassin et al., 2004). However, while many studies have focused on identifying risk factors associated with the course of drug involvement in adolescence and early adulthood (White, Xie, Thompson, Loeber, & Stouthamer-Loeber, 2001; Winters, Lee, Stinchfield, & Latimer, in press), fewer efforts examine the predictors of the course of SUDs (Flory, Lynam, Milich, Leukefeld, & Clayton, 2004; Guo et al., 2001). Also, few studies have described the course of SUDs during emerging adulthood, the years of late adolescence and early twenties when distinct changes and pursuits are experienced (e.g., career development, intimate adult relationship development) (Arnett, 2000).
Therefore, this study will examine several variables presumed to be associated with the course of SUDs. These variables were selected based on prior etiological research on drug use and abuse disorders (e.g., Hawkins et al., 1992; Tarter et al., 1999), and they include being male, dropping out of high school, being diagnosed with attention deficit hyperactivity disorder (ADHD), conduct disorder (CD), or oppositional defiant disorder (ODD) during childhood, having an early age of onset of alcohol or cannabis use, and previously using illicit drugs other than cannabis. Environmental (contextual) factors, such as family history of drug involvement, were also examined. Further, the number of risk factors was assessed, owing to the literature that the number of risk factors has been shown to be more predictive than specific factors (Latimer, Newcomb, Winters, & Stinchfield, 2000; Newcomb & Felix-Ortiz, 1992). We provide a brief overview of the literature related to the predictor variables of interest in this study.
A number of studies have consistently shown that compared to females, males report greater use of alcohol and cannabis (Baer, Kivlahan, & Marlatt, 1995; Grant & Dawson, 1998; Newcomb, Maddahian, Skager, & Bentler, 1987; Sneed, Morisky, Rotheram-Borus, Ebin, & Malotte, 2001; Wilson, Bell, & Arredondo, 1995) and are more likely to develop alcohol use disorders (Crum, Ensminger, Ro, & McCord, 1998; Guo et al., 2001). Longitudinal studies have found that gender is a factor to predict trajectory memberships among people with binge drinking problems over the transition to young adulthood (Bennett et al., 1999; Jackson et al., 2000; Schulenberg, Wadsworth, O’Malley, Bachman, & Johnston, 1996). Men and women also experienced different substance abuse trajectories (Becker & Grilo, 2006; Brook, Whiteman, & Finch, 1992; Chassin et al., 2004). In addition, dropping out of high school was also linked to drug problems (Anthony & Helzer, 1991; Kogan, Luo, Brody, & Murry, 2005). Crum et al. found that dropping out of high school was associated with an increased risk of developing alcohol use disorders in adulthood. In contrast, youths with high educational expectations during the high school period had a significantly lower probability of alcohol use disorders at age 21 (Guo et al.).
Prior research has established associations between childhood ADHD and SUDs (Carroll & Rounsaville, 1993; Kaminer, 1992; Wilens, Biederman, Spencer, & Frances, 1994) as well as between childhood conduct disorders and SUDs (Bucholz, Heath, & Madden, 2000; Merikangas & Avenevoli, 2000; Robins & Price, 1991; Slutske et al., 1998). While some studies have documented that ADHD is an independent risk factor for SUDs (Biederman, Wilens, Milberger, Sharon, Spencer, & Faraone, 1995), others have reported that the risk of children with ADHD for SUDs is mediated by comorbid conduct disorders (August, Winters, Realmuto, Fahnhorst, Botzet, & Lee, 2006; Barkley, Fischer, Edelbrock, & Smallish, 1990). Further, other research has suggested that CD increases the risk for SUDs independently of ADHD status (Biederman et al.; Wilens, Biederman, Mick, Faraone, & Spencer, 1997).
Studies have suggested that early age of onset of alcohol use is a risk factor for later heavy drinking (Barnes & Welte, 1988; Barnes, Welte, & Dintcheff, 1992) and alcohol abuse or dependence (DeWit et al., 2000; Grant & Dawson, 1997; Grant et al., 2005; McGue, Lacono, Legrand, Malone, & Elkins, 2001; Prescott & Kendler, 1999; Winters & Lee, 2008). In their large representative sample, for instance, Grant and Dawson found that for each additional year that onset of alcohol use was delayed, the odds of lifetime alcohol abuse and dependence decreased by 8% and 14%, respectively. Also, onset of cannabis use during the teenage years appears to result in a greater likelihood of developing a current cannabis use disorder compared to those who began their use after adolescence (Anthony & Petronis, 1995; Winters & Lee, 2008). Further, Clark, Jones, Wood, and Cornelius (2006) found that early age of onset of SUD symptoms was associated with more severe trajectory classes.
Contextual factors have been found to increase children’s risks of drug use, abuse, or dependence. An example was family history of alcoholism (Chassin et al., 2002; Prescott & Kendler, 1999). Bucholz et al. (2000) found that parental history of alcohol problems or excessive drinking was a significant predictor of their adolescent daughters’ transitions into more serious (moderate or dependent) classes of problem drinking. Parents’ use of cannabis was found to impact their teen’s use of cannabis (Hops, Duncan, Duncan, & Stoolmiller, 1996). Children of parents with SUDs, compared to those without, had an increased risk of SUDs (Merikangas & Avenevoli, 2000). Chassin et al. (2004) aimed to identify trajectory groups of drug use disorders from adolescence to early adulthood found that a greater proportion of children of alcoholics was observed in the diagnosed groups than in the nondiagnosed group.
Finally, results from previous etiological studies have suggested that there are multiple ways to abusing substances. Extent of substance use was found to be a function of the number of risk factors, rather than any particular set of them (Bry, McKeon, & Pandina, 1982). After identifying 12 risk factors of substance use, Newcomb and colleagues (Newcomb et al., 1987) found that increasing risk factors resulted in a marked increase of abuse. Specifically, those with 7 or more risk factors were at least 4 times more likely than the general sample to be substance abusers. Their findings suggested that the likelihood of drug use or abuse was not only directly associated with the number of risk factors to which the adolescents were exposed, but also may vary by the type of substance, such as alcohol, cannabis, and cocaine.
In sum, previous studies have observed considerable heterogeneity among individuals regarding developmental patterns over time of substance use and SUDs. Our interest is to extend this literature by investigating factors that are associated with these different trajectory group memberships. Specifically, our study has three goals. First, the study will describe the patterns of change in diagnosis of SUDs (limited to alcohol and cannabis) over time, with a focus on late adolescence to early adulthood. Second, this study extends previous studies by integrating variable-centered and person-centered approaches to identify the underlying latent trajectory classes in the study sample based on the course of alcohol or cannabis use disorders. Third, this study examines the association between a range of psychosocial factors and the latent trajectory group membership.
Method
Participants
The study sample consists of 310 individuals who were originally recruited as children and drawn from 22 suburban elementary schools in the State of Minnesota in 1991 for a research project called the Minnesota Competence Enhancement Project (MNCEP) and were participants in the long-term prospective study. They were identified as disruptive and comparison (non-disruptive) children using a multiple-gate screening procedure (August, Realmuto, Crosby, & MacDonald, 1995). Specifically, participants were identified as having cross-setting disruptive behavior if their scores derived from the teacher and parent Conners Hyperactivity Index (HI-T, HI-P; Goyette, Conners, & Ulrich, 1978) exceeding 1.75 SD units above the normative mean. In contrast, the comparison group (HI-T score below 1.1 SD above the normal mean) was obtained by using a stratified random sampling. Structured interviews were later conducted when they were 18 (T1), 20 (T2), and 22 (T3) years old. During the interviews, in addition to questions about their history of using alcohol, cannabis, and other drugs, a series of questions were also asked to see if an individual met the criteria of psychiatric disorders of a SUD according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV; American Psychiatric Association, 1994).
Slightly over three fourths of the 310 participants were male (76.3%) and almost one fourth was female (23.7%). They were predominantly Caucasian (90.8%). More than half (57.9%) of the participants had completed some years of college education. For the remaining participants, 8.9% finished a 4-year college degree or above, 26.6% only finished high school, and 6.6% had education less than a high school diploma. In terms of their marital status, most of them (75.8%) were single, with some cohabiting (15.2%) and others married (9%). The median annual income was $10,000-$20,000. About 63% of the participants was in disruptive group and 37% in comparisons.
Measures
Substance use disorders
Diagnoses of alcohol or cannabis use disorders were assessed at each of three “adolescent-young adult” waves (T1, T2, and T3) based on the DSM-IV criteria (American Psychiatric Association, 1994). Participants who were not diagnosed with alcohol abuse or dependence were coded as 0, those diagnosed with alcohol abuse were coded as 1, and those with dependence were coded as 2. Same coding was used for cannabis use disorders.
Predictors
Dummy variables were created for participants’ gender (0 = female; 1 = male) and dropping out of high school (0 = no; 1 = yes).
Diagnosis of externalizing psychiatric disorders during childhood
When the participants were originally recruited (at ages 7–9), their parents were interviewed with the Revised Parent Version of the Diagnostic Interview for Children and Adolescents (DICA-R; Reich, Shayla, & Taibelson, 1992) by trained assessment technicians. The Interview was modified to include all symptoms related to the Diagnostic and Statistical Manual of Mental Disorders (3rd ed., rev.) (DSM-III-R; American Psychiatric Association, 1987) diagnosis, including ADHD, CD, and ODD. Later when the participants were between 11 and 15 years of age, and again when they ranged in age from 12 to 16 years, they were reassessed to see if they met the criteria for disorders of ADHD, CD, or ODD. Given the literature on differential risk for SUDs for youth with a history of only ADHD versus youth with a history of CD/ODD, we created two separate dummy variables for this predictor domain: ADHD-only (0 = no; 1 = yes); CD/ODD regardless of whether ADHD diagnosis was present (0 = no; 1 = yes).
Age of onset of alcohol or cannabis use
Participants were asked at what age they first used alcohol or cannabis. Those who had an onset of alcohol or cannabis at age less than 17 were coded as "1," whereas those with onset at age 17 or older or non-users were coded as "0."
History of using illicit drugs
Participants were asked whether they had ever used any of the following illicit drugs: amphetamine, barbiturates, cocaine, opiates, hallucinogen, PCP, or inhalants (0 = no; 1 = yes).
Parental history of drug problems
Participants’ biological parents were asked whether they had a history of alcohol or other drug problems (0 = no; 1 = yes).
Number of risk factors
The eight risk factors described above were summed to form this aggregate predictor: being male, dropping out of school, having a childhood diagnosis of only ADHD, having a childhood diagnosis of CD/ODD regardless of whether ADHD was present, having an early age onset of alcohol use, having an early age onset of cannabis use, previously using illicit drugs other than cannabis, and having parents with a history of drug problems. For each risk factor an individual was exposed to, a "1" was given, and a "0" was given otherwise. The number of risk factors ranged from 0 to 8.
Statistical Analysis
Using Mplus 3.0 (Muthen & Muthen, 1998–2004), latent class regression was conducted on the data of the DSM-IV diagnoses of alcohol or cannabis use disorders (none or abuse or dependence) assessed at each of the three time points to identify the underlying latent trajectory classes among the participants as well as to examine whether each of the proposed risk factors predicted the trajectory group membership with or without statistical adjustment for covariates in regression models. Full maximum likelihood was used in all models to account for missing data. Previous research has suggested that the predictors of drug use may vary by the type of drugs (Nation & Heflinger, 2006; White et al., 2001), and that patterns of psychosocial predictors differ for alcohol and drug abuse (Becker & Grilo, 2006). Thus, the analyses for alcohol and cannabis cases were conducted separately.
Results
Patterns of change
Table 1 presents the frequencies for the participants’ diagnoses of SUDs from T1 to T3. For alcohol use disorders, while the number of participants who were without a diagnosis was steadily decreasing over time, the number of participants diagnosed with abuse increased by 60% from T1 to T2 and then decreased by about 25% at T3. However, the number of participants diagnosed with dependence decreased about half (48%) from T1 to T2 and then increased by 38% from T2 to T3. In contrast, for cannabis, the numbers for no diagnosis and a diagnosis of abuse were both increasing from T1 to T2 (17% and 13%, respectively) and decreasing from T2 to T3 (5% and 37%, respectively). The number of diagnoses of dependence decreased significantly over time (T1 to T2, 59%; T2 to T3, 19%).
Table 1.
Number of diagnosis from late adolescence to young adulthood for both drugs
| Alcohol | Cannabis | |||||
|---|---|---|---|---|---|---|
| Diagnosis | T1 | T2 | T3 | T1 | T2 | T3 |
| None | 194 | 187 | 163 | 186 | 218 | 207 |
| Abuse | 52 | 83 | 62 | 46 | 52 | 33 |
| Dependence | 50 | 26 | 36 | 64 | 26 | 21 |
Class memberships
The Bayesian Information Criteria (BIC) and the posterior probabilities of trajectory class membership were used to evaluate improvement in model fit and then select the optimal number of latent trajectory classes of both alcohol and cannabis use disorders. The goal was to find different trajectory classes that correspond to individuals following normative and non-normative developmental pathways. Smaller BIC values suggest a better fitting model when additional classes were added (Muthen & Muthen, 2000). Model estimation also provides estimates of probabilities of class membership for each individual. For instance, in a 2-class solution, two probabilities are estimated for each individual in the data, where each estimates the likelihood that an individual is a member of one of the classes. For each individual, the two probabilities sum to 1.0. In a well-fitting model, for each individual, one of the two probabilities would be very high (around 1.0) and the other very low (close to 0), indicating little ambiguity about class membership (Colder et al., 2001).
For alcohol use disorder cases, the 2-class model was found to have a lower BIC than the 3-class model (BIC = 1355.66 vs. 1379.10). Class 1 could be characterized as “very low rate” at any of the three time points (n = 185; 59.7%) and class 2 could be described as “moderate rate” (n = 125; 40.3%) at all three times points. Individuals classified to be in the very low rate class had an average posterior probability of being in the low rate class of .94, indicating a very low chance of misplacement. Similarly the average posterior probability of moderate rate class membership for those individuals classified in the moderate rate class was .95. For cannabis use disorder cases, the 2-class model fit better than the 3-class model according to the BIC values (1035.02 vs. 1064.47). Class 1 could be characterized as “very low rate” (n = 186; 60%) and class 2 could be described as “moderate rate” (n = 124; 40%) at all three time points. Individuals classified to be in the very low rate class had an average posterior probability of being in the very low rate class of .98, indicating a very low chance of misplacement. Similarly, the average posterior probability of moderate rate class membership for those individuals classified in the moderate rate class was .99. Therefore, a two-class solution was chosen for alcohol use disorders as well as for cannabis use disorders.
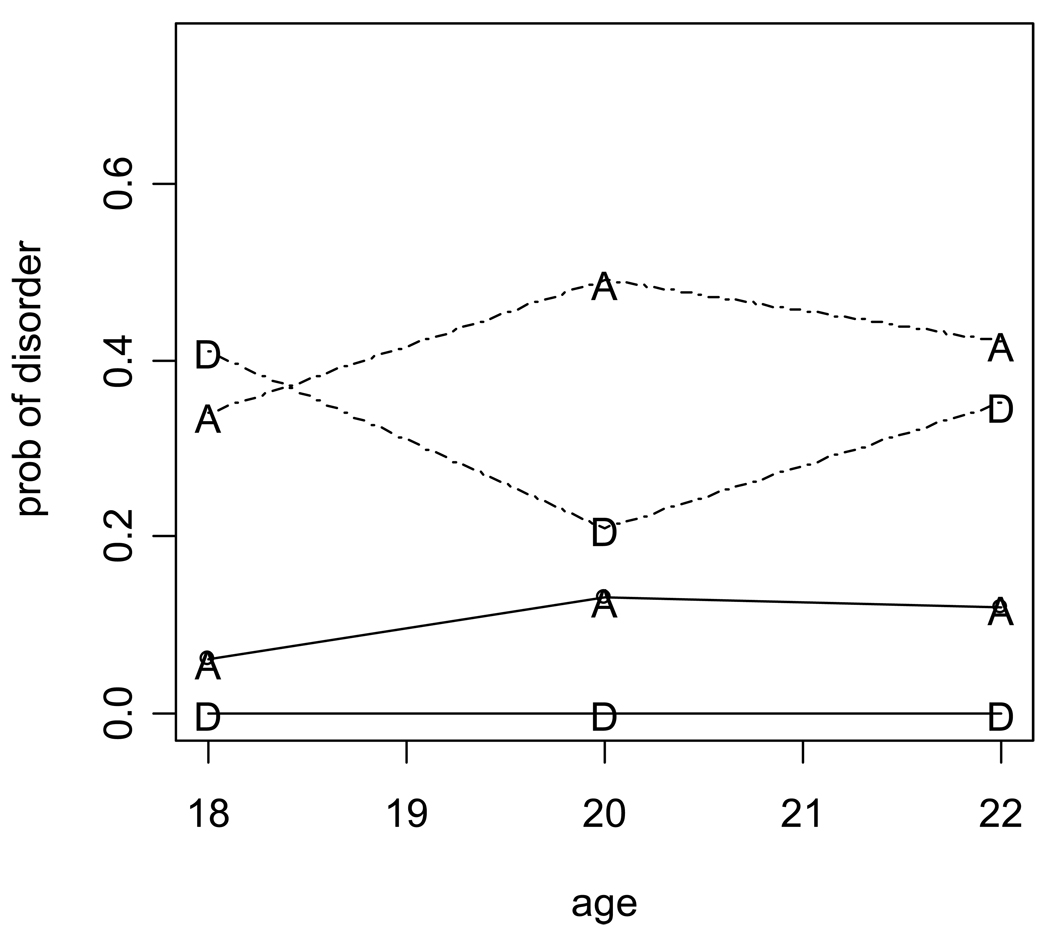
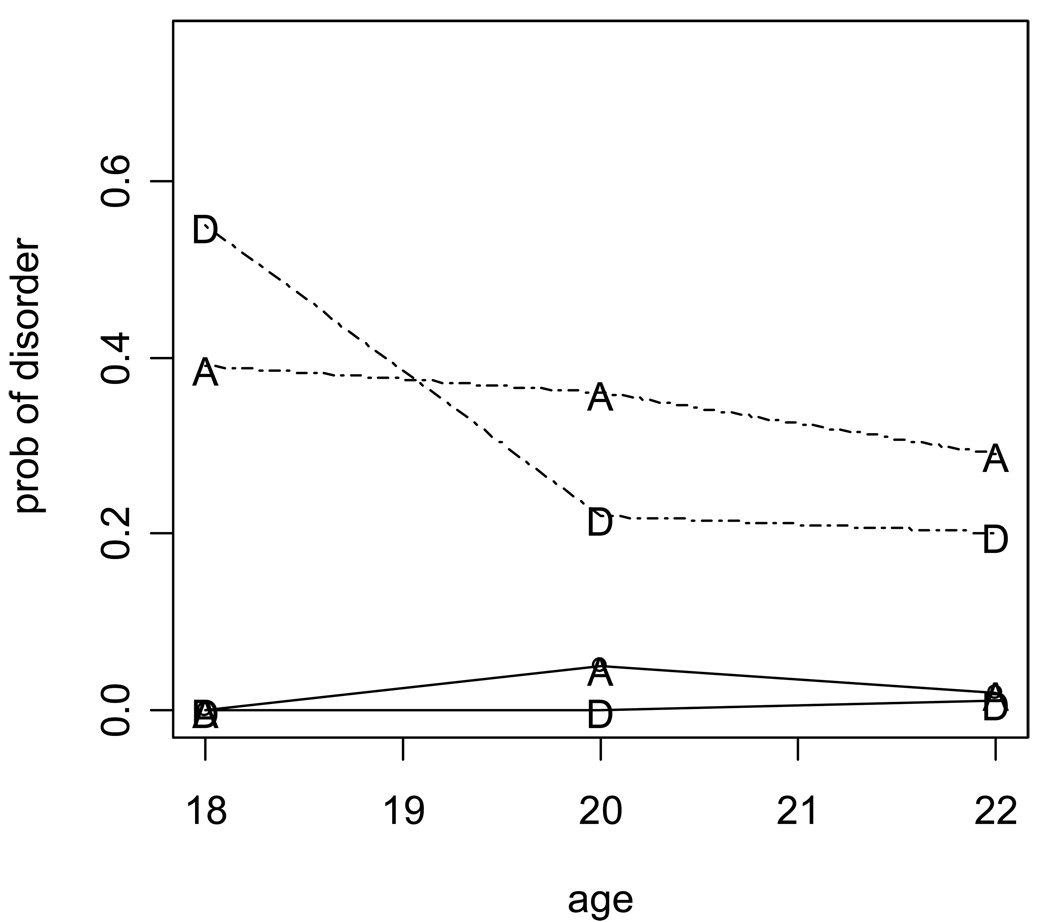
Figure 1 and Figure 2 present the estimated probabilities over the course of alcohol and cannabis use disorders, respectively, among the participants based on the two-class model. The results showed that if a given individual was in the very low rate class, the probabilities that s/he was diagnosed with alcohol abuse or dependence at T1, T2, and T3 were less than .13. In contrast, if a given individual was in the moderate rate class, the probabilities that s/he was diagnosed with alcohol abuse or dependence were between .21 and .49. Among the participants in terms of their trajectories of cannabis use disorders, the results showed that if a given individual was in the very low rate class, the probabilities that s/he was diagnosed with a cannabis use disorder at T1, T2, and T3 were less than .05. In contrast, if a given individual was in the moderate rate class, the probabilities that s/he was diagnosed with abuse or dependence were between .22 and .55.
Figure 1.
Estimated probabilities of alcohol use disorders among participants based on the two-class model
Note. A=Abuse, D=Dependence. The solid line represents the very low rate class, whereas the dotted line denotes the moderate rate class.
Figure 2.
Estimated probabilities of cannabis use disorders among participants based on the two-class model
Note. A=Abuse, D=Dependence. The solid line represents the very low rate class, whereas the dotted line denotes the moderate rate class.
Table 2 presents all the individual response patterns and their respective most likely trajectory class memberships based on the posterior prediction from the model for the 2-class model for alcohol and cannabis use disorder cases. Individuals who were diagnosed with alcohol abuse or dependence at least at two assessment times were assigned to the moderate rate class, whereas those who did not receive an alcohol use disorder at all three assessment times were allocated to the very low rate class. For individuals who were diagnosed with alcohol abuse or dependence at only one assessment time (n = 44), the majority of them (84%) were assigned to the very low rate class. The remaining individuals who were assigned to the moderate rate class tended to receive a diagnosis of dependence.
Table 2.
Response pattern and its respective class assignment based on the two-class modelsa
| Alcohol Use Disorders | Patternc | Cannabis Use Disorders | ||||
|---|---|---|---|---|---|---|
| Observed n | % | Classb | Observed n | % | Classb | |
| 116 | 37.4 | 1 | 000 | 143 | 46.1 | 1 |
| 16 | 5.2 | 1 | 001 | 3 | 1.0 | 1 |
| 3 | 1.0 | 2 | 002 | 1 | 0.3 | 1 |
| 12 | 3.9 | 1 | 010 | 9 | 2.9 | 1 |
| 9 | 2.9 | 1 | 100 | 14 | 4.5 | 2 |
| 4 | 1.3 | 2 | 200 | 17 | 5.5 | 2 |
| 120 | 1 | 0.3 | 2 | |||
| 2 | 0.6 | 2 | 121 | 2 | 0.6 | 2 |
| 2 | 0.6 | 2 | 122 | 1 | 0.3 | 2 |
| 3 | 1.0 | 2 | 220 | 3 | 1.0 | 2 |
| 6 | 1.9 | 2 | 221 | 5 | 1.6 | 2 |
| 5 | 1.6 | 2 | 222 | 8 | 2.6 | 2 |
| 5 | 1.6 | 2 | 212 | 2 | 0.6 | 2 |
| 3 | 1.0 | 2 | 112 | 4 | 1.3 | 2 |
| 8 | 2.6 | 2 | 211 | 6 | 1.9 | 2 |
| 9 | 2.9 | 2 | 111 | 6 | 1.9 | 2 |
| 2 | 0.6 | 2 | 202 | 1 | 0.3 | 2 |
| 4 | 1.3 | 2 | 102 | 2 | 0.6 | 2 |
| 9 | 2.9 | 2 | 012 | 1 | 0.3 | 2 |
| 1 | 0.3 | 2 | 022 | |||
| 1 | 0.3 | 2 | 201 | 3 | 1.0 | 2 |
| 4 | 1.3 | 2 | 101 | 2 | 0.6 | 2 |
| 12 | 3.9 | 2 | 011 | 3 | 1.0 | 2 |
| 2 | 0.6 | 2 | 210 | 6 | 1.9 | 2 |
| 9 | 0.3 | 2 | 110 | 4 | 1.3 | 2 |
Individuals without complete data in outcomes were not included in the table.
Class 1=very low rate class, class 2=moderate rate class.
Outcome patterns for a categorical repeated measure (0=no diagnosis, 1=diagnosed with abuse, 2=diagnosed with dependence) at T1, T2, and T3.
Similar patterns were found among the participants regarding their course of cannabis use disorders. Individuals diagnosed with cannabis abuse or dependence at least at two assessment times were allocated to the moderate rate class, whereas those not receiving a cannabis use disorder at all three assessment times were assigned to the very low rate class. However, different from alcohol use disorder cases, most of the individuals with only 1 diagnosis of cannabis abuse or disorder (n = 44) were assigned to the moderate rate class (n = 31; 70%). It appeared that for the moderate rate class individuals with single diagnosis, it was at T1 when they received a cannabis use disorder.
Predictors of trajectory group memberships
Table 3 presents the odds ratios (ORs) and 95% confidence intervals (CI) based on the results of the latent class regression (logistic regression of latent class membership on predictors) separately for the different predictors and then mutually adjusted. The results indicated that some of the individual factors predicted the trajectory class membership for alcohol and cannabis use disorders. The findings of the separate logistic regression models (i.e., models without statistical adjustment for other predictors) showed that being male, having been diagnosed with CD/ODD during childhood regardless of whether ADHD was present, having an early age of onset of alcohol use, having an early age of onset of cannabis use, or previously using illicit drugs other than cannabis was found to predict the trajectory class membership for alcohol (OR = 2.03–19.43) as well as for cannabis use disorders (OR = 2.69–110.61). However, none of the remaining three risk factors (i.e., dropping out of high school, receiving a diagnosis of only ADHD in childhood, and having a family history of drug problems) was found to be a predictor of the trajectory class membership.
Table 3.
Risk factors for being in class 2, with or without statistical adjustment for all listed covariates
| Alcohol | Cannabis | |||||||
|---|---|---|---|---|---|---|---|---|
| Separate predictors unadjusted |
All predictors included mutually adjusted |
Separate predictors unadjusted |
All predictors included mutually adjusted |
|||||
| Risk factors | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Being male | 3.28* | 1.50–7.18 | 4.60* | 1.69–12.46 | 3.03* | 1.33–6.86 | 2.77 | .69–11.13 |
| Dropping out of high school |
1.74 | .51–5.99 | 1.18 | .07–20.47 | 4.69 | .63–35.06 | 18.62* | 2.24–154.90 |
| Childhood ADHD diagnosis only |
1.33 | .60–2.96 | 1.15 | .36–3.72 | 1.72 | .74–3.96 | 2.31 | .64–8.33 |
| Childhood CD/ODD diagnosisa |
2.03* | 1.00–4.13 | 1.49 | .61–3.64 | 2.69* | 1.38–5.24 | 2.21 | .80–6.14 |
| Early age of onset of alcohol use |
19.43* | 8.47–44.61 | 9.72* | 3.68–25.69 | 13.40* | 5.24–34.26 | 1.10 | .27–4.39 |
| Early age of onset of cannabis use |
15.21* | 6.03–38.36 | 2.28 | .95–5.45 | 110.61* | 26.40–463.48 | 38.51* | 10.88–136.35 |
| Use of other illicit drugs | 12.33* | 5.16–29.44 | 4.88* | 1.90–12.56 | 52.72* | 23.24–119.62 | 19.75* | 7.44–52.41 |
| Positive family history of drug problems |
1.47 | .66–3.28 | 1.68 | .70–4.01 | 1.90 | .98–3.68 | 1.64 | .53–5.12 |
p< .05.
Regardless of whether ADHD diagnosis was present or not.
The results of mutually adjusted logistic regression analyses models (i.e., models including all predictors simultaneously) showed that being male, having an early age of alcohol onset, or previously using illicit drugs other than cannabis individually best predicted the trajectory class membership of alcohol use disorders. Specifically, males were 4.6 times more likely than females to be in the moderate rate class. Compared to those with an older age of alcohol use onset (17 or more), the individuals with an onset at a younger age (less than 17) were almost 10 times more likely to be in the moderate rate class. Individuals who previously used illicit drugs other than cannabis were about 5 times more likely to be in the moderate rate class than those who never did. A childhood diagnosis of CD/ODD and an early age of onset of cannabis use were found to make no unique contribution to the prediction above and beyond what they shared in the prediction with those emerged as more powerful predictors, as listed above.
Similar to the findings in alcohol use disorder cases, with mutual adjustment for other predictors some risk factors were found to best predict the trajectory class membership for cannabis use disorder cases, particularly dropping out of high school, having an early age of onset of cannabis use, and previously using illicit drugs other than cannabis. Specifically, individuals who did not finish high school were more likely to be in the moderate rate class than those who completed high school education (OR = 18.62). An early age of onset for cannabis use or previous use of illicit drugs other than cannabis was found to be associated with elevated risks of being in the moderate rate class (ORs = 38.51 and 19.75 respectively), compared to a late age of onset or never using other illicit drugs. Being male, receiving a childhood diagnosis of CD/ODD, and having an early age of onset of alcohol use were found to make no unique contribution to the prediction above and beyond what they shared in the prediction with those emerged as more powerful predictors, as listed above. In addition, the number of risk factors was found to predict the trajectory class membership for individuals’ courses of alcohol use disorders (OR = 3.53, 95% CI = 2.14, 5.80) and cannabis use disorders (OR = 5.82, 95% CI = 3.42, 9.88). Apparently, for both drug cases the more risk factors individuals were exposed to, the more likely they were to be in the moderate rate class.
Discussion
This study described the patterns of change in diagnosis of alcohol and cannabis use disorders, successfully identified two latent trajectory group memberships among individuals based on their diagnosis of alcohol and cannabis use disorders, and found several psychosocial factors that predict the trajectory group membership from late adolescence to early adulthood. Differences were shown in the patterns of change among the participants between the two drugs. We found that as individuals transitioned to adulthood, diagnosis of a SUD was more persistent for alcohol than for cannabis. This observation may be expected, as research has suggested that prevalence of disorders varies with the overall use structure of the larger social system in which it is embedded (Zucker et al., 2000). Further, moving out of adolescence may harbor more consideration that continued use of an illicit drug – cannabis – is socially unacceptable. That is, adolescence is a time of greater experimentation with a range of drugs (Hops et al., 2000), and aging into young adulthood may de-emphasize such experimentation (Arnett, 2000).
Increasing efforts have been made in identifying groups that are different in their developmental trajectories of interests. While the concept is not new, more relevant work was focused on areas such as delinquent behavior, binge drinking, and cannabis use, with little work on SUDs. By integrating variable-centered and person-centered approaches, this study extended the previous studies through examining longitudinal trajectories of alcohol and cannabis use disorders. Latent class regression analyses were used on three waves of SUD data collected during adolescence and young adulthood, and two latent trajectory classes were identified for both drug use disorders. Specifically, the individuals who were either never diagnosed or diagnosed with alcohol abuse or dependence only once were most likely to be allocated to the very low rate class, whereas those diagnosed with alcohol abuse or dependence at least at two assessment points were assigned into the moderate rate class. Given the very low chances of class misplacement, the latent trajectory class models for both drug use disorders were able to allocate with high confidence most of the response patterns in the two classes. Similar patterns were found in the course of individuals with cannabis use disorders.
Overall, the individuals assigned to the moderate rate group remained abusing or dependent on drugs during most, if not all, of the study time period, whereas most of those assigned to the low rate group remained diagnosis-free. Such stability over time among youth has been found by other researchers (Martin et al., 2000).
This study also has examined whether a select group of psychosocial factors predicts the trajectory class memberships among the participants based on their diagnostic courses of SUDs. In general, the results indicated that separately, most of the individual factors tested in the study predicted the trajectory class memberships of alcohol or cannabis use disorders. Such findings affirmed the prior research in that several factors that were related to SUDs based on one-time diagnostic assessment were associated with trajectory group membership of diagnostic SUDs over time. Specifically, being male, receiving a diagnosis of CD/ODD during childhood, having an early age of onset of alcohol or cannabis use, or using illicit drugs other than cannabis previously increased an individual’s likelihood for repeated diagnosis of alcohol or cannabis use disorders from late adolescence to early adulthood.
Furthermore, we found that when the covariance shared by the predictors was controlled for simultaneously, being male, having an early age of onset of alcohol use (i.e., before age 17), and previously using illicit drugs other than cannabis emerged to be better predictors for an individual’s likelihood of being repeatedly diagnosed with alcohol abuse or dependence during emerging adulthood than having a childhood diagnosis of CD/ODD and an early age of onset of cannabis use. We also found that dropping out of high school, having an early age of onset of cannabis use, and previously using illicit drugs other than cannabis emerged to be more powerful predictors for an individual’s likelihood for repeated diagnosis of cannabis use disorders during youth than being male, receiving a childhood diagnosis of CD/ODD, and having an early age of onset of alcohol use. In addition, the number of risk factors was also found to predict the trajectory class memberships among the individuals regarding their courses of alcohol or cannabis use disorders. As Newcomb et al. (1987) suggested, our study found that the more risk factors individuals were exposed to predicted increased odds of their being diagnosed with alcohol or cannabis use disorders repeatedly from late adolescence to early adulthood.
However, we did not find evidence for some other factors predicting the trajectory group membership, specifically receiving a diagnosis of only ADHD in childhood and parental history of drug problems. It appears that receiving a diagnosis of only ADHD does not differentiate the two trajectory classes of alcohol or cannabis use disorders among individuals. Despite prior research linking childhood ADHD to SUDs (Biederman et al., 1995; Merikangas & Avenevoli, 2000), discrepant results have been reported, particularly when externalizing problems were controlled for (Barkley et al., 2004; Molina & Pelham, 2003). August et al. (2006) found that ADHD without a comorbid externalizing disorder was not associated with an increased risk of drug abuse, suggesting that externalizing behaviors may operate to set in motion a chain of negative events that lead to experimentation and eventual use of substances.
This study also failed to support that parental history of drug problems was a significant predictor of trajectory group membership, although previous studies have found such a relationship (Chassin et al., 2004). One reason could be related to measurement issues. Parental involvement with alcohol or drugs was assessed by a single question in this study. No psychometric scales were used to measure the parents’ problems with alcohol or drug use, nor were they interviewed for their own diagnosis of psychiatric disorders, particularly SUDs. Further, Hops et al. (2000) indicated that modeling based on the social learning perspective that researchers applied to link parents’ use of substance to their adolescent offspring’s use, per se, is an insufficient explanation for the mechanism of how parent and adolescent use of substance are associated with each other, and that such a mechanism is a function of the parent-adolescent relationship process. For example, Andrews, Hops, and Duncan (1997) found that adolescent offspring are more likely to model the substance use of their parents if there is a low level of conflict displayed in their relationship. Given that we did not obtain information sufficient for testing these moderator effects, future studies are needed to explore whether the influence of parents’ use of drugs on trajectory group membership of diagnostic SUDs among their offspring is determined by their quality of relationship.
Implications
By identifying two classes for alcohol and cannabis use disorders and using a developmental perspective, we identified groups in which important changes occurred in a SUD. An appreciable percentage of youth revealed either an alcohol or cannabis use disorder with relative persistence. A more static approach would have failed to identify this important pattern across time. Further, given the persistence in diagnoses of SUDs particularly shown among the individuals in the moderate rate group as they moved through late adolescence to young adulthood, the importance of early programming efforts designed to prevent adolescents from using drugs or developing SUDs can never be stressed more. In other words, when adolescents are well along a trajectory of drug abuse or dependence, our findings suggest that the late timing of a drug abuse prevention program will likely limit its effectiveness (Hops et al., 2000).
Our findings also illustrate that several individual risk factors predict the group membership. Prevention work may benefit this type of analyses. Individuals who are exposed to risk factors are more likely to show a persistent course of SUDs into young adulthood. Also, our study provides some clarity as to specific risk factors that are related to future courses of SUDs, including being male, history of externalizing disorders, early age onset of drug use, and previous use of illicit drugs other than cannabis. Effective interventions for preventing adolescent SUDs may need to target psychosocial features that contribute to problematic behaviors (Hawkins et al., 1994). Further, these findings suggest that youth attempting to recover from a SUD during adolescence may benefit by targeting risk factors that may be amenable to change, such as presence of an externalizing disorder and staying in school.
Finally, we found that of the participants in this study, about 30% (n=92) were assigned to the moderate rate group for both drugs, about 50% (n=153) to the very low rate group for both drugs, and about 20% (n=65) to the moderate rate group for only one drug (10% for alcohol and 10% for cannabis). Such information is critical for effective preventive or intervention strategies, because individuals who remained in the very low rate group for both drugs, in the moderate rate group for only one drug, or in the moderate rate group for both drugs during emerging adulthood are likely to be different from one another, particularly in their profiles of risk or protective factors.
Limitations
Several limitations should be noted. First, given that most of the participants in this study were Caucasian, the findings may not apply to other populations such as non-whites. Second, prior research has shown that problems with alcohol or other drug use, such as cannabis, tend to decrease after the mid-twenties. Given that the last wave of data was collected when the participants were about 22 years old, it remains unknown whether the findings of this study would have been different, if more diagnosis data had been collected during the participants’ mid-twenties. Longitudinal data with more than three waves may open a window for more insightful research findings on trajectories of SUDs.
Conclusion
This study suggests different patterns of change in that overall increasing numbers of individuals were diagnosed with alcohol abuse or dependence as they transitioned to adulthood, whereas the number of those with a diagnosis of cannabis dependence was decreasing. Two groups were identified based on the individuals’ diagnostic courses from late adolescence to young adulthood, for alcohol as well as for cannabis. Finally, this study validates the previous studies by finding that several factors that are related to SUDs based on one-time diagnostic assessment continue to exert their influence on diagnostic SUDs over time. The results demonstrate that psychosocial factors, particularly being male, diagnosis of CD/ODD in childhood, early age of onset of drug use, and previous use of illicit drug use other than cannabis are associated with individuals’ trajectory group membership given their diagnoses of alcohol or cannabis use disorders during emerging adulthood. Due to the persistence in diagnosis across time among a fair amount of youths found in this study, prevention intervention should target these robust factors early to preclude the development of SUDs.
Acknowledgments
Grant: NIDA grants DA12995 and DA01534
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3rd ed., rev. Washington, DC: Author; 1987. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatry Association; 1994. [Google Scholar]
- Andrews JA, Hops H, Duncan SC. Adolescent modeling of parental substance use: The moderating effect of the relationship with the parent. Journal of Family Psychology. 1997;11:259–270. doi: 10.1037/0893-3200.11.3.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anthony JC, Helzer JE. Syndromes of drug abuse and dependence. In: Robins LN, Regier DA, editors. Psychiatric disorders in America: The epidemiologic catchment area study. New York: The Free Press; 1991. pp. 116–154. [Google Scholar]
- Anthony JC, Petronis KR. Early-onset drug use and risk of later drug problems. Drug and Alcohol Dependence. 1995;40:9–15. doi: 10.1016/0376-8716(95)01194-3. [DOI] [PubMed] [Google Scholar]
- Arnett JJ. Emerging adulthood: A theory of development from the late teens through the twenties. American Psychologist. 2000;55:469–480. [PubMed] [Google Scholar]
- August GJ, Realmuto GM, Crosby RD, MacDonald AW. Communit-based multi-gate screening procedure of children at risk for conduct disorder. Journal of Abnormal Child Psychology. 1995;23:521–544. doi: 10.1007/BF01447212. [DOI] [PubMed] [Google Scholar]
- August GJ, Winters KC, Realmuto GM, Fahnhorst T, Botzet A, Lee S. Prospective study of adolescent drug use among community sample of ADHD and non-ADHD participants. Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45:824–832. doi: 10.1097/01.chi.0000219831.16226.f8. [DOI] [PubMed] [Google Scholar]
- Baer JS, Kivlahan DR, Marlatt GA. High-risk drinking across the transition from high school to college. Alcoholism: Clinical and Experimental Research. 1995;19:54–61. doi: 10.1111/j.1530-0277.1995.tb01472.x. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Fischer M, Edelbrock CS, Smallish L. The adolescent outcome of hyperactive children diagnosed by research criteria, I: An 8-year prospective followup study. Journal of the American Academy of Child & Adolescent Psychiatry. 1990;29:546–557. doi: 10.1097/00004583-199007000-00007. [DOI] [PubMed] [Google Scholar]
- Barnes GM, Welte JM. Alcohol use and abuse among adults in New York State. Buffalo, NY: Research Institute on the Addictions; 1988. [Google Scholar]
- Barnes GM, Welte JW, Dintcheff B. Alcohol misuse among college students and other young adults: Findings from a general population study in New York State. International Journal of Addict. 1992;27:917–934. doi: 10.3109/10826089209065584. [DOI] [PubMed] [Google Scholar]
- Bates ME. Integrating person-centered and variable-centered approaches in the study of developmental courses and transitions in alcohol use: Introduction to the special section. Alcoholism: Clinical and Experimental Research. 2000;24:878–881. [PubMed] [Google Scholar]
- Bates ME, Labouvie EW. Adolescent risk factors and the prediction of persistent alcohol and drug use into adulthood. Alcoholism: Clinical and Experimental Research. 1997;21:944–950. [PubMed] [Google Scholar]
- Becker DF, Grilo CM. Prediction of drug and alcohol abuse in hospitalized adolescents: Comparisons by gender and substance type. Behaviour Research and Therapy. 2006;44:1431–1440. doi: 10.1016/j.brat.2005.10.009. [DOI] [PubMed] [Google Scholar]
- Bennett ME, McCrady BS, Johnson V, Pandina RJ. Problem drinking from young adulthood to adulthood: Patterns, predictors and outcomes. Journal of Studies on Alcohol. 1999;60:605–614. doi: 10.15288/jsa.1999.60.605. [DOI] [PubMed] [Google Scholar]
- Biederman J, Wilens T, Milberger E, Sharon DS, Spencer TJ, Faraone SV. Psychoactive substance use disorders in adults with attention deficit hyperactivity disorder (ADHD): Effects of ADHD and psychiatric comorbidity. American Journal of Psychiatry. 1995;152:1652–1658. doi: 10.1176/ajp.152.11.1652. [DOI] [PubMed] [Google Scholar]
- Brook JS, Whiteman MM, Finch S. Childhood aggression, adolescent delinquency, and drug use: A longitudinal study. Journal of Genetic Psychology. 1992;153:369–383. doi: 10.1080/00221325.1992.10753733. [DOI] [PubMed] [Google Scholar]
- Brown SA, D’Amico EJ, McCarthy DM, Tapert SF. Four-year outcomes from alcohol and drug treatment. Journal of Studies on Alcohol. 2001;62:381–388. doi: 10.15288/jsa.2001.62.381. [DOI] [PubMed] [Google Scholar]
- Bry BH, McKeon P, Pandina RJ. Extent of drug use as a function of number of risk factors. Journal of Abnormal Psychology. 1982;91:273–279. doi: 10.1037//0021-843x.91.4.273. [DOI] [PubMed] [Google Scholar]
- Bucholz KK, Heath AC, Madden PAF. Transitions in drinking in adolescent females: Evidence from the Missouri adolescent female twin study. Alcoholism: Clinical and Experimental Research. 2000;24:914–923. [PubMed] [Google Scholar]
- Carroll KM, Rounsaville BJ. History and significance and childhood attention deficit disorder in treatment-seeking cocaine abusers. Comprehensive Psychiatry. 1993;34(2):75–82. doi: 10.1016/0010-440x(93)90050-e. [DOI] [PubMed] [Google Scholar]
- Chassin L, Pitts SC, Prost J. Binge drinking trajectories from adolescence to emerging adulthood in a high-risk sample: Predictors and substance abuse outcomes. Journal of Consulting and Clinical Psychology. 2002;70:67–78. [PubMed] [Google Scholar]
- Chassin L, Flora DB, King KM. Trajectories of alcohol and drug use and dependence from adolescence to adulthood: The effects of familial alcoholism and personality. Journal of Abnormal Psychology. 2004;113:483–498. doi: 10.1037/0021-843X.113.4.483. [DOI] [PubMed] [Google Scholar]
- Chen K, Kandel DB. The natural history of drug use from adolescence to the mid-thirties in a general population sample. American Journal of Public Health. 1995;85:41–47. doi: 10.2105/ajph.85.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung T, Martin CS, Grella CE, Winters KC, Abrantes AM, Brown SA. Course of alcohol problems in treated adolescents. Alcoholism: Clinical and Experimental Research. 2003;27:253–261. doi: 10.1097/01.ALC.0000053009.66472.5E. [DOI] [PubMed] [Google Scholar]
- Clark DB, Jones BL, Wood DS, Cornelius JR. Substance use disorder trajectory classes: Diachronic integration of onset age, severity, and course. Addictive Behaviors. 2006;31:995–1009. doi: 10.1016/j.addbeh.2006.03.016. [DOI] [PubMed] [Google Scholar]
- Colder CR, Mehta P, Balanda K, Campbell RT, Mayhew KP, Stanton WR, Pentz MA, Flay BR. Identifying trajectories of adolescent smoking: An application of latent growth mixture modeling. Health Psychology. 2001;20:127–135. doi: 10.1037//0278-6133.20.2.127. [DOI] [PubMed] [Google Scholar]
- Crum RM, Ensminger ME, Ro MJ, McCord J. The association of educational achievement and school dropout with risk of alcoholism: A twenty-five-year prospective study of inner-city children. Journal of Studies on Alcohol. 1998;59:318–326. doi: 10.15288/jsa.1998.59.318. [DOI] [PubMed] [Google Scholar]
- DeWit DJ, Adlaf EM, Offord DR, Ogborne AC. Age at first alcohol use: A risk factor for the development of alcohol disorders. American Journal of Psychiatry. 2000;157:745–750. doi: 10.1176/appi.ajp.157.5.745. [DOI] [PubMed] [Google Scholar]
- Flory K, Lynam D, Milich R, Leukefeld C, Clayton R. Early adolescent through young adult alcohol and marijuana use trajectories: Early predictors, young adult outcomes, and predictive validity. Development and Psychopathology. 2004;16:193–213. doi: 10.1017/s0954579404044475. [DOI] [PubMed] [Google Scholar]
- Goyette CH, Conners CK, Ulrich RF. Normative data on Revised Conners Parent and Teacher Rating Scales. Journal of Abnormal Child Psychology. 1978;6:221–236. doi: 10.1007/BF00919127. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA. Age at onset of alcohol use and its association with DSM-IV alcohol abuse and dependence: Results from the National Longitudinal Alcohol Epidemiologic Survey. Journal of Substance Abuse. 1997;9:103–110. doi: 10.1016/s0899-3289(97)90009-2. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA. Age of onset of drug use and its association with DSM-IV drug abuse and dependence: Results from the National Longitudinal Alcohol Epidemiologic Survey. Journal of Substance Abuse. 1998;10:163–173. doi: 10.1016/s0899-3289(99)80131-x. [DOI] [PubMed] [Google Scholar]
- Grant JD, Scherrer JF, Lynskey MT, Lyons MJ, Eisen EA, Tsuang MT, True WR, Bucholz KK. Adolescent alcohol use is a risk factor for adult alcohol and drug dependence: Evidence from a twin design. Psychological Medicine. 2005;35:1–10. doi: 10.1017/S0033291705006045. [DOI] [PubMed] [Google Scholar]
- Guo J, Hawkins JD, Hill KG, Abbott RD. Childhood and adolescent predictors of alcohol abuse and dependence in young adulthood. Journal of Studies on Alcohol. 2001;62:754–762. doi: 10.15288/jsa.2001.62.754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins JD, Catelano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: Implications for substance abuse prevention. Psychological Bulletin. 1992;112:64–105. doi: 10.1037/0033-2909.112.1.64. [DOI] [PubMed] [Google Scholar]
- Hill KG, White HR, Chung I-J, Hawkins JD, Catalano RF. Early adult outcomes of adolescent binge drinking: Person- and variable-centered analyses of binge drinking trajectories. Alcoholism: Clinical and Experimental Research. 2000;24:892–901. [PMC free article] [PubMed] [Google Scholar]
- Hingson RW, Heeren T, Zakocs RC, Kopstein A, Wechsler H. Magnitude of alcohol-related mortality and morbidity among U.S. College Students ages 18–24. Journal of Studies on Alcohol. 2002;63:136–144. doi: 10.15288/jsa.2002.63.136. [DOI] [PubMed] [Google Scholar]
- Hops H, Andrews JA, Duncan SC, Duncan TE, Tildesley E. Adolescent drug use development: A social interactional and contextual perspective. In: Sameroff AJ, Lewis M, Miller SM, editors. Handbook of developmental psychopathology. New York: Kluwer Academic/Plenum; 2000. pp. 589–605. [Google Scholar]
- Hops H, Duncan TE, Duncan S, Stoolmiller M. Parent substance use as a predictor of adolescence: A six-year lagged analysis. Annals of Behavioral Medicine. 1996;18:157–164. doi: 10.1007/BF02883392. [DOI] [PubMed] [Google Scholar]
- Jackson KM, Sher KJ, Wood PK. Trajectories of concurrent substance use disorders: A developmental, typological approach to comorbidity. Alcoholism: Clinical and Experimental Research. 2000;24:902–913. [PubMed] [Google Scholar]
- Jennison KM, Johnson KA. Parental alcoholism as a risk factor for DSM-IV-defined alcohol abuse and dependence in American women: The protective benefits of dyadic cohesion in marital communication. American Journal of Drug and Alcohol Abuse. 2001;27:349–374. doi: 10.1081/ada-100103714. [DOI] [PubMed] [Google Scholar]
- Kaminer Y. Clinical implications of the relationship between attention-deficit hyperactivity disorder and psychoactive substance use disorders. American Journal of Addictions. 1992;1:257–264. [Google Scholar]
- Kandel DB, Chen K. Types of marijuana users by longitudinal course. Journal of Studies on Alcohol. 2000;61:367–378. doi: 10.15288/jsa.2000.61.367. [DOI] [PubMed] [Google Scholar]
- Kogan SM, Luo Z, Brody GH, Murry VM. The influence of high school dropout on substance use among African American youth. Journal of Ethnicity in Substance Abuse. 2005;4:35–51. doi: 10.1300/J233v04n01_04. [DOI] [PubMed] [Google Scholar]
- Latimer WW, Newcomb M, Winters KC, Stinchfield RD. Adolescent substance abuse treatment outcome: The role of substance abuse problem severity, psychosocial, and treatment factors. Journal of Consulting and Clinical Psychology. 2000;68:684–696. [PubMed] [Google Scholar]
- Martin CS, Maisto SA, Pollock NK, Cornelius JR. Changes in DSM-IV alcohol diagnostic status across three years in adolescent drinkers. Alcoholism: Clinical and Experimental Research. 2000;24 Supplement:138A. Abstract #792. [Google Scholar]
- McDermott S, Nagin DS. Same or different? Comparing offender groups and covariates over time. Sociological Methods & Research. 2001;29:282–318. [Google Scholar]
- McGue M, Lacono WG, Legrand LN, Malone S, Elkins I. Origins and consequences of age at first drink. I. Association with substance-use disorders, disinhibitory behavior and psychopathology, and P3 amplitude. Alcoholism: Clinical and Experimental Research. 2001;25:1156–1165. [PubMed] [Google Scholar]
- Merikangas KR, Avenevoli S. Implications of genetic epidemiology for the prevention of substance use disorders. Addictive Behaviors. 2000;25:807–820. doi: 10.1016/s0306-4603(00)00129-5. [DOI] [PubMed] [Google Scholar]
- Molina B, Pelham W. Childhood predictors of adolescent substance use in a longitudinal study of children with ADHD. Journal of Abnormal Psychology. 2003;112:497–507. doi: 10.1037/0021-843x.112.3.497. [DOI] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus User’s Guide. 3 th ed. Los Angeles, CA: Muthen & Muthen; 1998. 2004. [Google Scholar]
- Muthen B, Muthen LK. Integrating person-centered and variable-centered analyses: Growth mixture modeling with latent trajectory classes. Alcoholism: Clinical and Experimental Research. 2000;24:882–891. [PubMed] [Google Scholar]
- Nagin DS. Analyzing developmental trajectories: A semiparametric, group-based approach. Psychological Methods. 1999;4:139–177. doi: 10.1037/1082-989x.6.1.18. [DOI] [PubMed] [Google Scholar]
- Nation M, Heflinger CA. Risk factors for serious alcohol and drug use: The role of psychosocial variables in predicting the frequency of substance use among adolescents. The American Journal of Drug and Alcohol Abuse. 2006;32:415–433. doi: 10.1080/00952990600753867. [DOI] [PubMed] [Google Scholar]
- Newcomb MD, Felix-Ortiz M. Multiple protective and risk factors for drug use and abuse: Cross-sectional and prospective findings. Journal of Personality and Social Psychology. 1992;63:280–296. doi: 10.1037//0022-3514.63.2.280. [DOI] [PubMed] [Google Scholar]
- Newcomb MD, Maddahian E, Skager R, Bentler PM. Substance abuse and psychosocial risk factors among teenagers: Associations with sex, age, ethnicity, and type of school. American Journal of Drug and Alcohol Abuse. 1987;13:413–433. doi: 10.3109/00952998709001525. [DOI] [PubMed] [Google Scholar]
- Prescott CA, Kendler KS. Age at first drink and risk for alcoholism: A noncausal association. Alcoholism: Clinical and Experimental Research. 1999;23:101–107. [PubMed] [Google Scholar]
- Reich W, Shayla JJ, Taibelson C. The Diagnostic Interview for Children and Adolescents-Revised (DICA-R) (Structured Psychiatric Interview) St. Louis: Washington University; 1992. [Google Scholar]
- Robins LN, Price RK. Adult disorders predicted by childhood conduct problems: Results from the NIMH epidemiologic catchment area project. Psychiatry. 1991;54:116–132. doi: 10.1080/00332747.1991.11024540. [DOI] [PubMed] [Google Scholar]
- Schulenberg J, O’Malley PM, Bachman JG, Wadsworth KM, Johnson LD. Getting drunk and growing up: Trajectories of frequent binge drinking during the transition to young adulthood. Journal of Studies on Alcohol. 1996;57:289–304. doi: 10.15288/jsa.1996.57.289. [DOI] [PubMed] [Google Scholar]
- Schulenberg J, Wadsworth KM, O’Malley PM, Bachman JG, Johnson LD. Adolescent risk factors for binge drinking during the transition to young adulthood: Variable-centered and pattern-centered approaches to change. Developmental Psychology. 1996;32:659–674. [Google Scholar]
- Slutske WS, Heath AC, Dinwiddie SH, Madden PAF, Bucholz KK, Dunne MP, et al. Common genetic risk factors for conduct disorder and alcohol dependence. Journal of Abnormal Psychology. 1998;107:363–374. doi: 10.1037//0021-843x.107.3.363. [DOI] [PubMed] [Google Scholar]
- Sneed CD, Morisky DE, Rotheram-Borus MJ, Ebin VJ, Malotte CK. Patterns of adolescent alcohol, cigarette, and marijuana sue over a 6-month period. Addictive Behaviors. 2001;26:415–423. doi: 10.1016/s0306-4603(00)00134-9. [DOI] [PubMed] [Google Scholar]
- Tarter R, Vanyukov M, Giancola P, Dawes M, Blackson T, Mezzich A, Clark DB. Etiology of early age onset substance use disorder: A maturational perspective. Development and Psychopathology. 1999;11:657–683. doi: 10.1017/s0954579499002266. [DOI] [PubMed] [Google Scholar]
- Tucker JS, Orlando M, Ellickson PL. Patterns and correlates of binge drinking trajectories from early adolescence to young adulthood. Health Psychology. 2003;22:79–87. doi: 10.1037//0278-6133.22.1.79. [DOI] [PubMed] [Google Scholar]
- White HR, Xie M, Thompson W, Loeber R, Stouthamer-Loeber M. Psychopathology as a predictor of adolescent drug use trajectories. Psychology of Addictive Behaviors. 2001;15:210–218. [PubMed] [Google Scholar]
- Wilens TE, Biederman J, Spencer TJ, Frances RJ. Comorbidity of attention-deficit hyperactivity and psychoactive substance use disorders. Hospital and Community Psychiatry. 1994;45:421–423. doi: 10.1176/ps.45.5.421. 435. [DOI] [PubMed] [Google Scholar]
- Wilens TE, Biederman J, Mick E, Faraone SV, Spencer T. Attention deficit hyperactivity disorder is associated with early onset substance use disorders. Journal of Nervous and Mental Diseases. 1997;185:475–482. doi: 10.1097/00005053-199708000-00001. [DOI] [PubMed] [Google Scholar]
- Wilson SE, Bell RW, Arredondo R. Temperament, family environment, and family history of alcohol abuse. Alcoholism Treatment Quarterly. 1995;12(3):55–68. [Google Scholar]
- Winters KC, Lee S, Stinchfield RD, Latimer WW. Psychosocial factors associated with long-term outcome of drug-abusing youth following 12-Step treatment. Substance Abuse. doi: 10.1016/j.jsat.2006.12.003. in press. [DOI] [PubMed] [Google Scholar]
- Winters KC, Lee C-YS. Likelihood of developing an alcohol and cannabis use disorder during youth: Association with recent use and age. Drug and Alcohol Dependence. 2008;92:239–247. doi: 10.1016/j.drugalcdep.2007.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zucker RA, Chermack ST, Curran GM. A life span perspective on etiology and course. In: Sameroff AJ, Lewis M, Miller SM, editors. Handbook of developmental psychopathology. New York: Kluwer Academic/Plenum; 2000. pp. 569–587. [Google Scholar]
- Zucker RA, Fitzgerald HE, Moses HD. Emergence of alcohol problems and the several alcoholisms: A developmental perspective on etiologic theory and life course trajectory. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology: Vol. 2. Risk, disorder and adaptation. New York: Wiley; 1995. pp. 677–711. [Google Scholar]