Abstract
Objectives
To determine whether perinatal nutrition influences cognitive function at 7½-8 years in children born preterm.
Design
Randomised, blinded nutritional intervention trial. Blinded follow up at 7½-8 years.
Setting
Intervention phase in two neonatal units; follow up in a clinic or school setting.
Subjects
424 preterm infants who weighed under 1850 g at birth; 360 of those who survived were tested at 7½-8 years.
Interventions
Standard infant formula versus nutrient enriched preterm formula randomly assigned as sole diet (trial A) or supplements to maternal milk (trial B) fed for a mean of 1 month.
Main outcome measures
Intelligence quotient (IQ) at 7½-8 years with abbreviated Weschler intelligence scale for children (revised).
Results
There was a major sex difference in the impact of diet. At 7½-8 years boys previously fed standard versus preterm formula as sole diet had a 12.2 point disadvantage (95% confidence interval 3.7 to 20.6; P<0.01) in verbal IQ. In those with highest intakes of trial diets corresponding figures were 9.5 point disadvantage and 14.4 point disadvantage in overall IQ (1.2 to 17.7; P<0.05) and verbal IQ (5.7 to 23.2; P<0.01). Consequently, more infants fed term formula had low verbal IQ (<85): 31% versus 14% for both sexes (P=0.02) and 47% versus 13% in boys P=0.009). There was a higher incidence of cerebral palsy in those fed term formula; exclusion of such children did not alter the findings.
Conclusions
Preterm infants are vulnerable to suboptimal early nutrition in terms of their cognitive performance—notably, language based skills—at 7½-8 years, when cognitive scores are highly predictive of adult ones. Our data on cerebral palsy generate a new hypothesis that suboptimal nutritional management during a critical or plastic early period of rapid brain growth could impair functional compensation in those sustaining an earlier brain insult. Cognitive function, notably in males, may be permanently impaired by suboptimal neonatal nutrition.
Key messages
Suboptimal nutrition during sensitive stages in early brain development may have long term effects on cognitive function
In a randomised trial of early nutrition in preterm infants those fed standard rather than nutrient enriched preterm formula had reduced verbal IQ scores at 7½ to 8 years, at least in boys
In exploratory analyses on children of both sexes verbal IQ below 85 and cerebral palsy were more prevalent in the standard formula group
Our data show the potential vulnerability of the human brain to early suboptimal nutrition
Avoidance of undernutrition in sick preterm infants seems important in optimising later neurodevelopmental outcomes
Introduction
Numerous studies have examined whether suboptimal nutrition in early life, at a critical or “vulnerable” phase of brain development, could affect later cognitive function1–6—a matter of major public health and clinical concern. Most studies have been in developing countries, where malnutrition is so closely associated with poverty, poor social circumstances, and lack of stimulation that it has been difficult to extricate these influences from any potential long term effect of nutrition itself.6,7 While some recent evidence is compelling,3,8 firm conclusions are still hampered by the lack of large studies with adequate experimental design.
Clear demonstration of causal effects of early nutrition on long term neurodevelopment requires an experimental approach with strict randomisation of groups. Experimental studies in animals, mostly rodents,8–10 have shown that nutrition in early life can permanently affect brain structure and function, especially in males. Such studies in animals, however, have uncertain relevance for human cognitive development.
In humans the so called “critical” spurt in brain growth is between the third trimester and 2 years post-term.5 We have designed a series of randomised prospective studies to test the vulnerability of the brain to suboptimal nutrition during specific periods of this growth spurt. Our most longstanding studies, started in 1982, were on preterm infants11,12 and therefore designed to test effects of diet in the earliest period of the spurt in brain growth—before full term. In the early 1980s diets available for preterm infants varied greatly in nutrient content,11 and it was ethical and feasible to assign these diets randomly as there was considerable uncertainty on optimal nutritional strategies. Our outcome studies have direct application for clinical practice13 and provide a unique opportunity to test formally the hypothesis that nutrition could influence long term cognitive performance.
In 1991 we reported the first of two parallel trials comparing effects of feeding infants born preterm a standard infant formula or a special preterm formula enriched with protein, energy, and micronutrients designed to meet the calculated nutritional needs of preterm infants. Despite the brevity of the early dietary manipulation—on average only the first postnatal month12—we reported major reductions in motor and mental development indices at 18 months in the group fed on standard formula. Test scores at 18 months, however, are not strongly predictive of later cognitive development.14 We report here results of formal cognitive tests in these children at 7½-8 years, when any group differences in intelligence quotients would be likely to reflect permanent effects of early diet.15
Methods
We enrolled infants who weighed under 1850 g at birth and were admitted to the neonatal unit in Norwich throughout 1982-4 and in Sheffield during 1983-4. Ethical approval was obtained in each centre. Parental consent was always sought and was never refused. Only babies with major congenital malformations known to impair growth or development were ineligible.
Randomisation
Randomisation was as shown in figure 1. Infants of mothers who chose not to provide breast milk were randomly allocated to receive either a standard term formula (Ostermilk, previously Osterfeed, Farley Health Products) or a preterm formula designed (by us) to meet the calculated increased nutritional needs in preterm infants (Osterprem, Farley Health Products) as their sole diet (trial A). Those babies whose mothers chose to provide their breast milk were randomly allocated to receive the term or preterm formula as a supplement to breast milk (trial B). Intake of trial diet in trial B depended on the mother’s success in providing her milk. The volume of formula and breast milk (if received) were recorded daily to allow the proportional consumption of these milks to be calculated over the study. Consumption of the trial diet varied from none to 100% intake (median 39%; quartiles 5% and 76%) with no difference between babies supplemented with term (median 38%) or preterm (41%) formula.
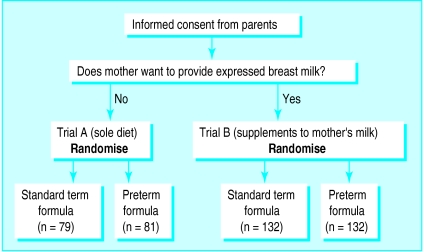
Figure 1.
Design of longitudinal study of early diet and later developmental status. Comparison of standard term versus preterm formula for 424 infants weighing under 1850 g at birth
It was planned that trials A and B would be treated independently and combined to compare babies randomly assigned a term formula (as sole diet or supplement) or preterm formula (as sole diet or supplement). Randomisation carried out in the first 48 hours after birth12 was by use of opaque sealed envelopes (numbered in consecutive order) and was conducted independently in each centre. Assignments were on the basis of permuted blocks of variable length. Within each trial randomisation was stratified by birth weight (<1200 g and 1200 g or above) to increase the likelihood of equal distribution of sick babies between groups.
Composition of formulas
The formulas were identified by numeric code so that neonatal staff, parents, and eventually follow up staff were blinded to dietary assignment. The composition of the trial formulas is shown in table 1. The quantity but not quality of protein and fat differed between the two formulas. The composition of expressed breast milk from daily analyses of samples from 24 hour milk collections was 1.5 g protein, 3.0 g fat, 7.0 g carbohydrate, 0.259 MJ (62 kcal), 23 mg sodium, 35 mg calcium, and 15 mg phosphorus per 100 ml.
Table 1.
Major constituents (per 100 ml) of trial milks
| Constituent | Preterm formula | Term formula |
|---|---|---|
| Protein (g) | 2.0 | 1.5 |
| Fat (g): | 4.9 | 3.8 |
| Saturated (%) | 39.5 | 39.5 |
| Unsaturated (%) | 60.5 | 60.5 |
| Carbohydrate (disaccharide, g): | 7.0 | 7.0 |
| Lactose (g) | 6.0 | 7.0 |
| Maltodextrin (g) | 1.0 | — |
| Energy (MJ) | 0.334 | 0.284 |
| Sodium (mg) | 45 | 19 |
| Potassium (mg) | 65 | 57 |
| Chloride (mg) | 60 | 45 |
| Calcium (mg) | 70 | 35 |
| Magnesium (mg) | 5 | 5.2 |
| Phosphorus (mg) | 35 | 29 |
| Iron (μg) | 40 | 650 |
| Copper (μg) | 120 | 43 |
| Manganese (μg) | 3 | 3.4 |
| Zinc (μg) | 1000 | 350 |
| Iodine (μg) | 7 | 4.5 |
| Vitamin A (μg) | 100 | 100 |
| Vitamin D (μg) | 8.0 | 1.0 |
| Vitamin E (μg) | 10 | 0.48 |
| Vitamin K (μg) | 7 | 2.7 |
| Vitamin B-1 (μg) | 95 | 42 |
| Vitamin B-2 (μg) | 180 | 55 |
| Niacin/niacinamide (μg) | 1000 | 690 |
| Vitamin B-6 (μg) | 100 | 35 |
| Vitamin B-12 (μg) | 0.2 | 0.14 |
| Folic acid (μg) | 50 | 3.4 |
| Pantothenic acid (μg) | 500 | 230 |
| Biotin (μg) | 2.0 | 1.0 |
| Vitamin C (μg) | 28 | 6.9 |
| Choline (mg) | 5.6 | 5* |
| Inositol (mg) | 3.2 | 5* |
| Taurine (mg) | 5.1 | Trace |
| Carnitine (mg) | 1.0 | 2* |
| Casein (whey ratio) | 40:60 | 40:60 |
Values not measured for every batch. Approximate figures are given.
After birth enteral feeds by nasogastric tube were increased according to tolerance; target intake was 180 ml/kg per day. In total 182 infants (43%) required initial parenteral nutrition including amino acid infusion (with or without lipid). Median period to full enteral feeds was 9 (quartiles 7 and 14) days with no difference between groups. Trial diets were discontinued when body weight reached 2000 g or at hospital discharge, whichever was sooner. Because of prolonged growth failure 12 infants initially assigned standard formula (six in trial A) were changed to preterm formula for at least a week. Results from these children were analysed as randomised in accordance with the trial protocol (but excluded in a further analysis, see discussion).
Data collected
Extensive demographic, social, clinical, anthropometric, and biochemical data were collected according to predefined criteria. Social class was coded into six categories (registrar general’s classification) and mother’s education according to categories published previously.16
Of the 424 infants enrolled, 377 survived. Of the 47 who died, 19 were in trial A (8/79 on term formula and 11/81 on preterm formula) and 28 in trial B (14/132 in each diet group). Appointments were sent to the 366 survivors still resident in the United Kingdom; consent for participation was refused in only six cases. Follow up thus comprised 96% survivors (360/377) and over 98% (360/366) of those still in Britain. We assessed intelligence quotient (IQ) with the Weschler intelligence scale for children (revised anglicised version: WISC-R UK).17 Because extensive additional data were collected we used an abbreviated version of the intelligence scale with five subsets: similarities, arithmetic, and vocabulary (verbal scale), and block design and object assembly (performance scale). The abbreviated revision assessed from these five subscales has a correlation coefficient with the full revised scale of over 0.96.18 Of children followed up, 24 had cerebral palsy (with neurological signs and motor impairment), and four of these and a blind child were too disabled for full IQ testing; thus full assessments were made on 99% (355/360) of those seen (of the five children not tested, three were fed preterm formula and two were fed standard formula).
Analysis
Data were analysed as randomised in accordance with the trial protocol and standard practice. Statistical analyses included Student’s t test, χ2 test, Fisher’s exact test, and multiple regression. Data from children with cerebral palsy who could be tested were included in these tests but excluded from further analyses. A sample size of 288 subjects was calculated at the outset to detect a 0.33 SD difference (5 points) in overall IQ between feed groups (A and B combined) at the 5% significance level with over 80% power. (In fact, the follow up of 360 subjects permitted a 4.5 point difference to be detected.) For trial A alone a sample size of 128 subjects was calculated to detect a 0.5 SD difference (7.5 points) in overall IQ (recruitment achieved was slightly higher than this at 133 subjects). On the basis of our previous follow up of this cohort, these hypothesised differences were plausible.12
Results
Table 2 shows characteristics of the study population. The randomised groups did not differ significantly in demographic or clinical characteristics. Those fed preterm formula had greater neonatal weight gain in trials A and B and greater gain in head circumference in trial A. Period spent on the trial diets was similar in both randomised feed groups (median 4 weeks). Detailed analyses showed no differences between groups in trials A, B, or A plus B in total intravenous volume, energy, protein, or lipid.
Table 2.
Characteristics of subjects followed up at 7½ to 8 years and early physical growth according to diet of standard term formula or preterm formula
| Characteristic | Trial A (as sole diets)
|
Trial B (as supplements to mother’s milk)
|
Trial A+B (as sole diets or supplements)
|
|||||
|---|---|---|---|---|---|---|---|---|
| Standard formula | Preterm formula | Standard formua | Preterm formula | Standard formula | Preterm formula | |||
| No of children followed up | 68 | 67 | 113 | 112 | 181 | 179 | ||
| No of children developmentally assessed | 67 | 66 | 112 | 110 | 179 | 176 | ||
| No of boys | 35 | 24 | 50 | 59 | 85 | 83 | ||
| No small for gestation (<10th centile) | 23 | 24 | 45 | 42 | 68 | 66 | ||
| Mean (SE) birth weight (g) | 1354 (66) | 1404 (38) | 1425 (28) | 1424 (29) | 1399 (22) | 1416 (23) | ||
| Mean (SE) gestation (weeks) | 30.6 (0.3) | 30.9 (0.3) | 31.2 (0.2) | 31.3 (0.3) | 31.0 (0.2) | 31.2 (0.2) | ||
| No needing mechanical ventilation for ⩾14 days | 6 | 6 | 9 | 13 | 15 | 19 | ||
| Mean (SE) time to attain full enteral feeds (days) | 13.1 (1.4) | 13.4 (1.3) | 12.4 (1.0) | 12.2 (1.1) | 12.7 (0.8) | 12.7 (0.8) | ||
| No with parents of non-manual social class | 11 | 14 | 43 | 46 | 54 | 60 | ||
| No of mothers with higher education | 4 | 1 | 27 | 30 | 31 | 31 | ||
| Mean (SE) steady state weight gain while on diet (g/kg/day) | 20.3 (0.9) | 29.8 (1.0)*** | 22.4 (0.6) | 25.2 (0.7)** | 21.6 (0.5) | 25.8 (0.6)*** | ||
| Mean (SE) head circumference gain while on diet (mm/day) | 1.2 (0.08) | 1.5 (0.08)** | 1.4 (0.06) | 1.4 (0.05) | 1.3 (0.05) | 1.4 (0.04) | ||
| Median days in study (25th, 75th centiles) | 33 (21, 49) | 26 (18, 42) | 30 (19, 52) | 28 (19, 45) | 30 (20, 50) | 28 (19, 45) | ||
P<0.005, ***P<0.001 by t test.
The incidence of intraventricular haemorrhage did not differ between groups. Larger babies were not routinely scanned, and ultrasound data were available for 59% of cases. For trials A plus B 30/126 (24%) babies had documented intraventricular haemorrhage in the standard formula group and 27/124 (22%) in the preterm formula group; for more severe, grade 3 or 4 intraventricular haemorrhage, respective numbers were 11 (8.7%) versus 10 (8.1%). For trial A alone total numbers of babies with intraventricular haemorrhage for the standard versus preterm formula groups were 14/49 (29%) versus 16/48 (33%); and six in each group had grade 3 or 4 haemorrhage.
Measurements of IQ
Table 3 shows performance, verbal, and overall IQ scores at 7½ to 8 years. In trial A verbal IQ was 4.8 points lower (P=0.8) in those fed solely a standard term formula rather than preterm formula. The differences in IQ seen between groups in trial A or B or in trial A plus B combined were not significant (p>0.05). (The higher IQ of children in trial B, who were fed their own mother’s milk, compared with IQ of those in trial A has been reported previously.19)
Table 3.
Intelligence quotients (IQs) measured by Weschler revised intelligence scale for children* (verbal, performance, and overall IQ) at 7½ to 8 years according to diet. Standard term formula and preterm formula compared as sole diets (trial A), as supplements to mother’s milk (trial B), and in trials A and B combined. Values are group means (SE)
| Detail | Milk formula
|
Advantage for preterm formula (95% CI) | |
|---|---|---|---|
| Standard | Preterm | ||
| Trial A | |||
| No of subjects† | 67 | 66 | |
| Verbal IQ | 92.7 (2.0) | 97.6 (1.8) | 4.8 (−0.6 to 10.2) |
| Performance IQ | 97.7 (1.8) | 96.0 (2.1) | −1.7 (−7.2 to 3.8) |
| Overall IQ | 94.8 (1.7) | 97.0 (1.8) | 2.2 (−2.7 to 7.0) |
| Trial B | |||
| No of subjects† | 112 | 110 | |
| Verbal IQ | 102.7 (1.7) | 103.0 (1.7) | 0.3 (−4.6 to 5.1) |
| Performance IQ | 104.0 (1.5) | 105.1 (1.5) | 1.1 (−3.1 to 5.2) |
| Overall IQ | 103.2 (1.5) | 104.2 (1.4) | 1.0 (−3.0 to 5.0) |
| Trial A and B | |||
| No of subjects† | 179 | 176 | |
| Verbal IQ | 99.0 (1.4) | 100.9 (1.3) | 2.0 (−1.7 to 5.7) |
| Performance IQ | 101.7 (1.2) | 101.6 (1.3) | 0.03 (−3.4 to 3.4) |
| Overall IQ | 100.0 (1.2) | 101.4 (1.1) | 1.4 (−1.8 to 4.6) |
Abbreviated form; see text.
Numbers vary by up to two subjects in individual cells; see text.
Some infants received little trial diet either because of early discharge or prolonged intravenous feeding. In trial B consumption of trial formula was low when mothers provided sufficient breast milk. In explanatory analyses we tested whether differences between feed groups were blunted by low intake of the trial diets. Analyses confined to 218 selected infants in trial A or B who received at least 2 weeks of full enteral feeds and to those from trial B who had received over 50% (mean 80%) of total enteral intake of trial formula generally showed accentuation of the difference between diet groups (table 4). There was a 4.6 point advantage (P=0.053) in verbal IQ and a 3.7 point advantage in overall IQ (P=0.08) for those fed preterm rather than term formula.
Table 4.
Intelligence quotients (IQs) measured by Weschler revised intelligence scale for children* (verbal, performance, and overall IQ) at 7½ to 8 years according to diet for infants who received highest intakes of trial diet. Standard term formula and preterm formula compared as sole diets (trial A), as supplements to mother’s milk (trial B), and in trials A and B combined. Values are group means (SE)
| Detail | Milk formula
|
Advantage for preterm formula (95% CI) | |
|---|---|---|---|
| Term | Preterm | ||
| Trial A | |||
| No of subjects† | 56 | 56 | |
| Verbal IQ | 93.3 (2.3) | 98.2 (1.9) | 4.9 (−0.9 to 10.7) |
| Performance IQ | 96.3 (2.0) | 96.6 (2.3) | 0.3 (−5.8 to 6.3) |
| Overall IQ | 94.6 (1.9) | 97.6 (1.9) | 3.0 (−2.3 to 8.3) |
| Trial B | |||
| No of subjects† | 55 | 51 | |
| Verbal IQ | 96.3 (2.5) | 100.7 (2.9) | 4.4 (−3.1 to 12.0) |
| Performance IQ | 100.5 (2.3) | 103.4 (2.3) | 2.9 (−3.6 to 9.5) |
| Overall IQ | 97.7 (2.2) | 102.5 (2.3) | 4.6 (−1.8 to 11.0) |
| Trial A and B | |||
| No of subjects† | 111 | 107 | |
| Verbal IQ | 94.8 (1.7) | 99.4 (1.7) | 4.6 (−0.07 to 9.3)‡ |
| Performance IQ | 98.4 (1.5) | 99.8 (1.7) | 1.4 (−3.1 to 5.9) |
| Overall IQ | 96.2 (1.5) | 99.9 (1.5) | 3.7 (−0.5 to 7.8) |
Abbreviated form; see text.
Numbers vary by up to two subjects in individual cells; see text.
P=0.053 by t test.
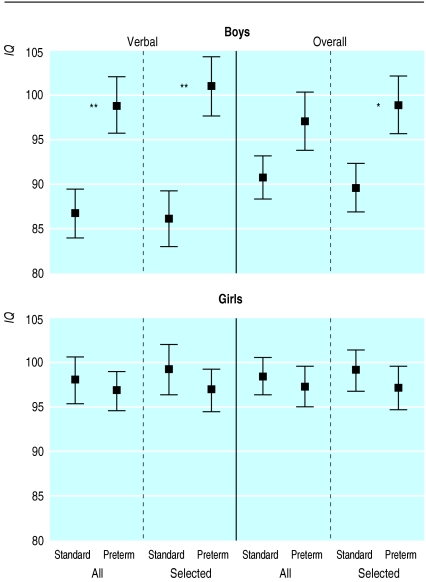
In view of our previous finding in this cohort at 18 months of age of a significant interaction between diet and sex in relation to developmental scores12 we analysed data here by sex. Table 5 shows dietary effects on verbal and overall IQ. The beneficial effect of preterm formula on verbal IQ was seen for boys but not girls and was confined to those fed exclusively on the trial diets (trial A). Boys on the preterm formula had a 12.2 (95% confidence interval 3.7 to 20.6) point advantage in verbal IQ and a 6.3 (−1.5 to 14.2) point advantage in overall IQ, whereas no effect was seen in girls (test for interaction P=0.009 and 0.09, respectively).
Table 5.
Influence of sex on beneficial effects (95% confidence intervals) of preterm formula milk on verbal and overall IQ
| Trial (sex) | Gain in verbal IQ
|
Gain in overall IQ
|
|||
|---|---|---|---|---|---|
| All | Selected† | All | Selected† | ||
| Trial A | |||||
| Boys | 12.2** (3.7 to 20.6) | 14.4** (5.7 to 23.2) | 6.3 (−1.5 to 14.2) | 9.5* (1.2 to 17.7) | |
| Girls | −2.2 (−9.0 to 4.6) | −3.4 (−10.7 to 3.9) | −2.2 (−8.4 to 4.1) | −2.8 (−9.5 to 3.9) | |
| Trial B | |||||
| Boys | −3.7 (−10.6 to 3.2) | −0.7 (−10.5 to 12.0) | −1.0 (−6.4 to 4.4) | 2.7 (−6.1 to 11.5) | |
| Girls | 4.4 (−2.4 to 11.3) | 7.7 (−2.8 to 18.2) | 3.0 (−3.1 to 9.1) | 6.3 (−3.1 to 15.7) | |
| Trial A+B | |||||
| Boys | 2.9 (−2.7 to 8.4) | 7.9* (0.8 to 15.0) | 2.6 (−2.0 to 7.2) | 6.5* (0.5 to 12.5) | |
| Girls | 1.2 (−3.8 to 6.2) | 1.8 (−4.4 to 8.1) | 0.3 (−4.1 to 4.8) | 1.3 (−4.3 to 6.9) | |
P<0.05, **P<0.01 by t test.
Infants who received highest intakes of trial diet (see text).
Advantages in verbal and overall IQ were even larger among boys who received the highest intake of trial diet. The advantage in verbal IQ was 14.4 (5.7 to 23.2) and in overall IQ was 9.5 (1.2 to 17.7) points for boys with the highest intakes of preterm formula. No effect was seen in girls (test for interaction P=0.002 and 0.02, respectively).
Children with cerebral palsy and low IQ scores
The analyses above included children with cerebral palsy whose IQ was measured. In trial A, however, cerebral palsy was significantly more common among those fed standard rather than preterm formula (8/67 v 1/66; P=0.03 by Fisher’s exact test). To explore whether this imbalance could explain the disadvantageous outcome of those fed the standard formula, further analyses were performed with exclusion of data from those children with cerebral palsy. The disadvantage for the standard formula remained—for example, verbal IQ in boys fed standard versus preterm formula was 9.7 points lower (95% confidence interval 1.1 to 18.3; P=0.03).
Significantly more children fed standard versus preterm formula had low verbal IQ (<85). Table 6 shows this analysis both including and excluding subjects with cerebral palsy. In children previously fed standard formula the proportion with low verbal IQ was over twice that in the group fed with preterm formula; in boys the difference was over threefold. Not all children with cerebral palsy had low IQ. To derive an overall category of children with poor outcome we calculated the proportion of children with either low verbal IQ scores (<85) or cerebral palsy as these outcomes were separately affected by diet. Table 6 shows the greater proportion of infants in this category from trial A had been fed term rather than preterm formula (38% v 15%; P=0.003)—a difference most pronounced in boys (54% v 17%; P=0.004). In corresponding analyses for trials A plus B (n=360; not tabulated) boys and girls were again more likely to be in the category with poor outcome if they had received the standard versus preterm formula (25% (45/181, including 16 children with cerebral palsy) versus 16% (29/179, including eight children with cerebral palsy); P=0.05); the effect was greatest in boys (33% (28/85) versus 18% (15/83); P=0.027).
Table 6.
Proportions (percentages) of children with low verbal IQ (<85*), cerebral palsy, or combination (low verbal IQ or cerebral palsy) according to diet in trial A† (standard term formula and preterm formula compared as sole diets)
| Detail | Milk formula
|
Odds ratio (95% CI) | P value by Fisher’s exact test | |
|---|---|---|---|---|
| Term | Preterm | |||
| No (%) with verbal IQ <85‡: | ||||
| All | 21/67 (31) | 9/66 (14) | 2.9 (1.2 to 6.9) | 0.022 |
| Boys | 16/34 (47) | 3/24 (13) | 6.2 (1.6 to 24.8) | 0.009 |
| Girls | 5/33 (15) | 6/42 (14) | 1.1 (0.2 to 3.9) | 1.0 |
| No (%) with verbal IQ <85 excluding children with cerebral palsy‡: | ||||
| All | 18/60 (30) | 9/65 (14) | 2.7 (1.1 to 6.5) | 0.03 |
| Boys | 13/29 (45) | 3/23 (13) | 5.4 (1.3 to 22.3) | 0.02 |
| Girls | 5/31 (16) | 6/42 (14) | 1.2 (0.3 to 4.2) | 1.0 |
| No (%) with cerebral palsy: | ||||
| All | 8/68 (12) | 1/67 (1.5) | 8.8 (1.1 to 72.4) | 0.03 |
| Boys | 6/35 (17) | 1/24 (4.2) | 4.7 (0.5 to 41.5) | 0.13 |
| Girls | 2/33 (6.1) | 0/43 | 0.19 | |
| No (%) with cerebral palsy or verbal IQ <85‡: | ||||
| All | 26/68(38) | 10/66 (15) | 3.4 (1.5 to 8.0) | 0.003 |
| Boys | 19/35 (54) | 4/24 (17) | 5.9 (1.7 to 21.0) | 0.004 |
| Girls | 7/33 (21) | 6/42 (14) | 1.6 (0.5 to 5.4) | 0.54 |
Weschler abbreviated scale, revised, see text.
See text for data on trials A and B combined.
One child who did not have cerebral palsy could not be psychometrically assessed.
Discussion
In this prospective, blinded, randomised outcome trial, with follow up of 98% of survivors still in Britain, the diet assigned to a premature baby for an average of just 4 weeks after birth had a significant effect on IQ—notably verbal IQ in boys—7½-8 years later when IQ scores are highly predictive of subsequent ones.14 Our findings suggest that suboptimal early nutrition in preterm infants can have a permanent effect on their cognitive function, emphasising the potential importance of dietary management decisions in this population. In biological terms our findings now provide “experimental” evidence in humans to support the long debated hypothesis that nutrition during critical or vulnerable periods of brain growth may have lasting consequences for cognition.5,10
Apart from its broader biological purpose, this study examined the practical question of whether early diet influences outcome in a typical, unselected, and heterogeneous preterm population in a neonatal unit. We did not study whether the perinatal sensitivity to nutrition identified extended beyond full term. While many other investigators have approached this1–6 there is still a paucity of formal randomised studies.8 The only strictly randomised study of post-term nutrition on long term outcome is that by Grantham-McGregor et al on 127 subjects. They showed a small increase in cognitive function at follow up in nutritionally supplemented stunted children in a developing country.20
Our data also show (tables 2 and 3) the higher IQ in children whose early diet included their own mother’s milk (trial B) versus those fed solely on formula (trial A). This non-randomised comparison has been published elsewhere19 and does not confound the present study, which considers the randomised comparison of standard infant formula versus nutrient enriched preterm formula used either as sole diets (trial A), as supplements to mother’s milk (trial B), or in the balanced addition of trials A and B which preserves randomisation.
Sex differences in the effect of diet
Previously and in another cohort (comparing preterm formula with banked donor breast milk) we found that effects on development induced by early diet were most prominent for language development.21 Again at 7½-8 years verbal or language based skills were predominantly affected. Lack of dietary effect on performance skills, however, might reflect our choice of only two performance subscales (block design and object assembly) in this abbreviated form of the Weschler intelligence scale for children (revised). This issue will be resolved at future planned follow up.
In animal studies long term consequences of early malnutrition on learning and behaviour are seen predominantly in males.22 Also, in the study by Fitzhardinge and Steven on full term infants who are small for gestational age only boys had later cognitive deficits.23 Our analysis according to sex was the principal preplanned subgroup analysis and was further justified by the significant interaction between sex and diet (significantly different impact of diet on development). Interestingly, the observed dietary effects on cognitive scores were significant only in boys. Also, although an effect of diet on the proportion of children with “poor outcome” was seen in both boys and girls, again the dominant effect was in boys. There was no cognitive disadvantage for boys versus girls when a nutrient enriched preterm formula was used (fig 2); only when boys were fed suboptimally (on standard formula) was there a major loss of cognitive potential. Why the male brain should be so vulnerable to early nutritional insults is an unresolved biological issue. We found no sex difference in mean gestation or birth weight. Boys, however, as expected, were sicker with 25% (42/168) requiring ventilation for more than 7 days compared with 16% (30/190) in girls. This could in part explain the sex effect if diet had more impact on later cognitive development in sicker individuals; indeed, a previous analysis provided some evidence for this.21
Figure 2.
Mean (SE) verbal intelligence quotient (IQ) and overall IQ in boys and girls fed standard versus preterm formula as their sole diet. Dietary comparison is made for all boys and also for those receiving highest intakes of trial diets (see text).*P<0.05; **P<0.01
As the principal effects were seen in boys and in trial A our data may reflect a chance finding in a subpopulation of our cohort. Several factors, however, argue against this. As trial B reflected a comparison of trial diets substantially blunted by use of human milk in both groups it is not surprising that the effects of diet are seen in trial A. Furthermore, when we selected subjects for the highest intakes of the trial formulas (given for at least 2 weeks and, in trial B, at least 50% of enteral intake as formula) dietary effects were more distinct (for instance, boys selected in this way and fed solely on term rather than preterm formula had a major disadvantage of around 10 points in overall IQ versus 6 points in non-selected boys). This relation between the effect size and amount of trial diets consumed favours a causal relation. We also found an advantage of preterm formula over banked donated breast milk at a 9 month follow up in an entirely different though parallel cohort; this study also showed an effect predominantly in boys, as in the numerous animal and human studies cited above.
Diet and cerebral palsy
Unexpectedly, among infants fed the standard rather than preterm formula cerebral palsy was significantly more common, and we explored whether the lower cognitive scores seen in those fed standard formula were due to this imbalance. This proved not to be the case; even with specific analysis of data from children with cerebral palsy, low verbal scores (<85; over 1 SD below the mean) were seen over twice as commonly in both boys and girls previously fed the term rather than preterm formula and over three times as commonly in boys (45% v 13%).
The association between diet and cerebral palsy (largely spastic diplegia) was a post hoc finding but raises a clinically important hypothesis for formal testing. There is evidence from newborn rats and preterm monkeys that the brain may reorganise to achieve complete functional compensation if cortical damage occurs sufficiently early.24 It is plausible that, although cerebral palsy in prematurely born children might originate prenatally or at least before enteral feeding has commenced, whether the brain can subsequently achieve functional compensation at a time of rapid brain growth and development might depend on the provision of adequate nutrient substrates. Indeed, in the average period on the trial diets (4 weeks) the preterm infant’s brain should increase by 50% in weight at “in utero” rates.25 We showed here a major deficit in head12 and therefore brain25 growth during the neonatal period in those fed the term formula. Further studies are needed, however, to investigate the issues here.
Clinical implications
The two trial formulas (table 1) differed in their contents of protein, energy, calcium, phosphorus, iron, zinc, copper, and several other micronutrients, though not in quality of protein or fat. Our trial was not designed to explore which nutrients influenced neurodevelopment. Broadly our findings support the generic hypothesis that failure to meet overall nutrient needs during this critical period of brain growth has significant consequences for cognitive development. While standard “term” formulas, widely used when our cohort was recruited, are now infrequently fed to very low birthweight preterm infants, poor nutritional status remains common in these babies; our findings therefore have contemporary relevance in emphasising the importance of avoiding this.
In conclusion, we have shown that brief early dietary manipulation in preterm infants has major effects on later cognitive function. The study provides further support for our more general thesis26 that early nutrition during critical windows in early life may have “programming” effects on long term outcomes and provides some of the first evidence from a strictly randomised, blinded, and long term trial with near complete follow up that early nutrition may have persistent effects on the human brain.
Acknowledgments
We thank the Medical Research Council for its core support; the staff of the neonatal units in Norwich and Sheffield; Drs C E S Leeson-Payne and G Lister for their major contribution in developmental testing of the subjects; Drs P M Crowle and RJ Pearse for their collaboration; Evelyn Smith for preparing the manuscript; and, in particular, the children taking part in the study, their families, and the schools which provided accommodation.
Footnotes
Funding: Contribution from Farley Health Products (a division of H J Heinz). The preterm formula was designed by us for this study and manufactured and supplied by Farleys.
Competing interests: None declared.
References
- 1.Gardner JM, Grantham-McGregor SM. Physical activity, undernutrition and child development (review) Proc Nutr Soc. 1994;53:241–248. doi: 10.1079/pns19940025. [DOI] [PubMed] [Google Scholar]
- 2.Pollitt E, Gorman KS, Engle PL, Martorell R, Rivera J. Early supplementary feeding and cognition: effects over two decades. Monogr Soc Res Child Dev 1993;58. [PubMed]
- 3.Grantham-McGregor SM, Powell CA, Walker SP, Himes JH. Nutritional supplementation, psychosocial stimulation and mental development of stunted children: the Jamaican study. Lancet. 1991;338:1–5. doi: 10.1016/0140-6736(91)90001-6. [DOI] [PubMed] [Google Scholar]
- 4.Husaini MA, Karyadi L, Husaini YK, Sandjaja B, Karyadi D, Pollitt E. Developmental effects of short-term supplementary feeding in nutritionally at-risk Indonesian infants. Am J Clin Nutr. 1991;54:799–804. doi: 10.1093/ajcn/54.5.799. [DOI] [PubMed] [Google Scholar]
- 5.Dobbing J. Nutritional growth restriction and the nervous system. In: Davison AN, Thompson RHS, editors. The molecular basis of neuropathology. London: Edward Arnold; 1981. pp. 221–223. [Google Scholar]
- 6.Grantham-McGregor S. Field studies in early nutrition and later achievement. In: Dobbing J, editor. Early nutrition and later achievement. London: Academic Press; 1987. pp. 128–174. [Google Scholar]
- 7.Richardson SA. The relation of severe malnutrition in infancy to the intelligence of school children with differing life histories. Pediatr Res. 1976;10:57–61. doi: 10.1203/00006450-197601000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Smart JL. Malnutrition, learning and behavior: 25 years on from the MIT symposium. Proc Nutr Soc. 1993;52:189–199. doi: 10.1079/pns19930051. [DOI] [PubMed] [Google Scholar]
- 9.Katz HG. The influence of undernutrition on learning performance in rodents. Nutr Abs Rev. 1980;50:767–783. [Google Scholar]
- 10.Smart JL. Early life malnutrition and later learning ability—critical analysis. In: Oliverio A, editor. Genetics, environment and intelligence. Amsterdam: Elsevier; 1977. pp. 215–235. [Google Scholar]
- 11.Lucas A, Gore SM, Cole TJ, Bamford MF, Dossetor JF, Barr I, et al. Multicentre trial on feeding low birthweight infants: effects of diet on early growth. Arch Dis Child. 1984;59:722–730. doi: 10.1136/adc.59.8.722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lucas A, Morley R, Cole TJ, Gore SM, Lucas PJ, Crowle P, et al. Early diet in preterm babies and developmental status at 18 months. Lancet. 1990;335:1477–1481. doi: 10.1016/0140-6736(90)93026-l. [DOI] [PubMed] [Google Scholar]
- 13.Lucas A. Enteral nutrition. In: Tsang R, Lucas A, Uauy R, Zlotkin S, editors. Nutritional needs of the preterm infant. Pawling, United States: Caduceus Medical Publishers; 1993. pp. 209–223. [Google Scholar]
- 14.McCall RB. The development of intellectual functioning in infancy and the prediction of later IQ. In: Osofsky JD, editor. The handbook of infant development. New York: Wiley; 1979. pp. 707–741. [Google Scholar]
- 15.Cronbach LJ. Essentials of psychological testing. New York: Harper Collins; 1990. p. 284. [Google Scholar]
- 16.Morley R, Cole TJ, Powell R, Lucas A. Mother’s choice to provide breast milk and developmental outcome. Arch Dis Child. 1988;63:1382–1385. doi: 10.1136/adc.63.11.1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Psychological Corporation. Wechsler intelligence scale for children, Anglicised. Rev ed. Sidcup: Psychological Corporation; 1974. [Google Scholar]
- 18.McNemar Q. Correction to a correction. J Consult Clin Psychol. 1974;42:145–146. [Google Scholar]
- 19.Lucas A, Morley R, Cole TJ, Lister G, Leeson-Payne C. Breast milk and subsequent intelligence quotient in children born preterm. Lancet. 1992;339:261–264. doi: 10.1016/0140-6736(92)91329-7. [DOI] [PubMed] [Google Scholar]
- 20.Grantham-McGregor SM, Walker SP, Chang SM, Powell CA. Effects of early childhood supplementation with and without stimulation on later development in stunted Jamaican children. Am J Clin Nutr. 1997;66:247–253. doi: 10.1093/ajcn/66.2.247. [DOI] [PubMed] [Google Scholar]
- 21.Lucas A, Morley R, Cole TJ, Bamford MF, Boon A, Crowle P, et al. Early diet in preterm babies and developmental status in infancy. Arch Dis Child. 1989;11:1570–1578. doi: 10.1136/adc.64.11.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smart JL. Undernutrition, learning and memory: review of experimental studies. In: Taylor TG, Jenkins NK, editors. Proceedings of XIII international congress of nutrition. London: John Libbey; 1986. pp. 74–78. [Google Scholar]
- 23.Fitzhardinge PM, Steven EM. The small-for-date infant. II. Neurological and intellectual sequelae. Pediatrics. 1972;50:50–57. [PubMed] [Google Scholar]
- 24.Kolb B, Whishaw IQ. Fundamentals of neuropsychology. 3rd ed. New York: Freeman; 1990. Development and recovery; pp. 679–711. [Google Scholar]
- 25.Cooke RWI, Lucas A, Yudkin PLN, Pryse-Davies J. Head circumference as an index of brain weight in the fetus and newborn. Early Hum Dev. 1977;1/2:145–149. doi: 10.1016/0378-3782(77)90015-9. [DOI] [PubMed] [Google Scholar]
- 26.Lucas A. Programming by early nutrition in man. In: Barker D, editor. The childhood environment and adult disease. Chichester: Wiley; 1991. pp. 38–55. . (CIBA Foundation Symposium 156.) [Google Scholar]