Abstract
Background
Gait disturbances are among the more common symptoms in the elderly. Reduced mobility markedly impairs quality of life, and the associated falls increase morbidity and mortality.
Methods
Review of the literature based on a selective search (PubMed) on the terms “gait,” “gait disorder,” “locomotion,” “elderly,” “geriatric” and “ageing” (2000–11/2009) and the findings of the authors’ own studies on gait changes in old age and on the functional brain imaging of gait control.
Results
Gait disturbances in the elderly are often of multifactorial origin. The relevant pathogenetic factors include sensory deficits (visual, vestibular, somatosensory), neurodegenerative processes (cortical, extrapyramidal motor, cerebellar), toxic factors (medications, alcohol), and anxiety (primary or concerning falls). A clinically oriented classification of gait disorders is proposed, which, on the basis of the characterization of gait and the accompanying clinical findings, enables identification of the etiological factors and points the way to rational therapy. Current research topics in the study of gait disturbances are also discussed, including quantitative gait analysis, interactions between locomotion and cognition (dual tasking), and functional imaging approaches.
Conclusions
The evaluation of elderly patients whose chief complaint is a gait disturbance should be directed toward the identification of specific deficits. This is the prerequisite for rational therapy, even when the problem is of multifactorial origin. The preservation of mobility is important in itself, and also because the ability to walk is closely correlated with cognitive performance.
Gait disturbances are a common medical problem in old age. Among the patients of a hospital department of acute neurology, old age is the most important risk factor for a gait disturbance (1). A variety of diseases can cause gait disturbances; some, like Parkinson’s disease, have well-established treatments according to the principles of evidence-based medicine, while for others, like cerebrovascular gait disturbance, too little evidence is available to support any particular form of treatment. A population-based study has shown a 35% prevalence of gait disorders among persons over age 70 (2). 85% of 60-year-olds still walk normally, but only 20% of 85-year-olds do (3). The latter fact also implies, however, that gait disturbances are not an inevitable accompaniment of old age. Problems of balance and gait are associated with immobility and falls, which markedly impair the quality of life (4). About 30% of persons over age 65 living at home fall at least once per year; among nursing home residents, the corresponding figure is about 50% (5). Mobility is often restricted still further by the fear of falling (6). Patients visiting their family physician because of gait disturbances complain most often of pain, joint stiffness, numbness, weakness, and an abnormal pattern of gait (7).
The learning goals for readers of this article are
to know the different methods used in the diagnostic assessment of gait disturbances,
to be able to identify the factors that contribute to the (multifactorial) gait disturbances of old age, and
to be acquainted with the effective treatments that are available for certain types of gait disturbance.
Prevalence.
The prevalence of gait disturbances is 35% in persons over age 70.
This article is based on a selective review of the literature in the PubMed database. The clinical overview also incorporates the authors’ own findings on age-related changes in gait and on the functional cerebral imaging of gait control.
The definition of gait disturbances in old age
Definition of gait disturbance in the elderly.
Demonstrable gait abnormality beyond the normal age-related slowing
Presence of a qualitative impairment of walking
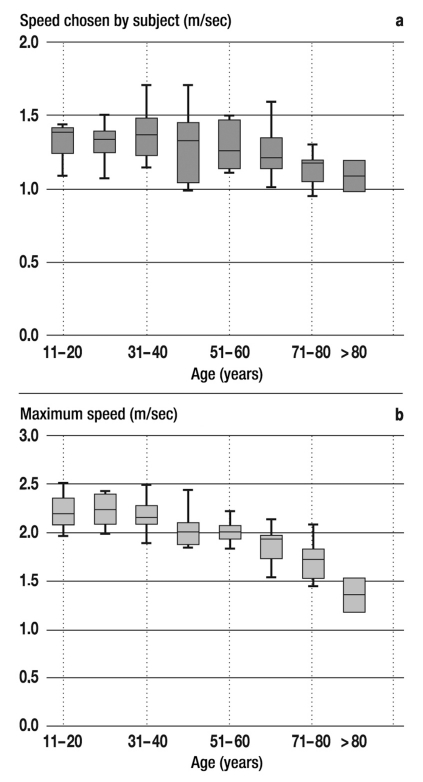
Walking is one of the more frequently performed sensorimotor tasks in everyday life. It relies on a complex, simultaneous interaction of the motor system, sensory control, and cognitive functions. The diagnostic assessment of gait disturbances in old age requires a clear distinction of pathological findings from the normal, physiological changes of aging. Spontaneous walking speed normally decreases by about 1% per year from age 60 onward (8), and the observed decline of maximum walking speed is even greater (figure 1). On the other hand, a gait disturbance in old age is said to be present when the patient walks even more slowly than expected for age, or when there are qualitative abnormalities of locomotion, such as disturbances of the initiation of gait or of balance while walking (9). The patient’s gait should be observed in standardized fashion, and the findings should be compared to age-specific norms. Gait disturbances in old age should be clinically classified in purely descriptive terms at first; deficits should be recorded as deviations of the main quantitative parameters of gait—speed, step size, and breadth of stance—from the corresponding age-specific norms. Blanket terms such as “senile gait disturbance” should be avoided, because specific treatment cannot be provided if the relevant deficits underlying the gait disturbance have not been identified.
Figure 1.
Changes in walking speed with increasing age. Walking speed with eyes open was measured twice in each of 70 normal subjects: a speed chosen spontaneously by the subject, and the maximum speed of which the subject was capable (Gaitrite walkway system, www.gaitrite.com). Ten persons in each decade were studied (exceptions: 6 persons aged 11–20 and 4 persons aged over 80). The subjects walked a test distance of approximately 14 meters, i.e., one roundtrip to the end of the walkway and back. The temporal and spatial gait parameters were registered for each step. The means and 25th and 75th percentiles are indicated by boxes with a line in the middle, and standard deviations are shown as error bars. (a) The spontaneous speed of gait diminishes slightly with advancing age; (b) the maximum speed diminishes to a more marked extent (data collected by the authors).
Overview of the physiology of gait control
The physiology of gait control.
The rhythmic pattern of the human gait is established at the level of the spinal cord.
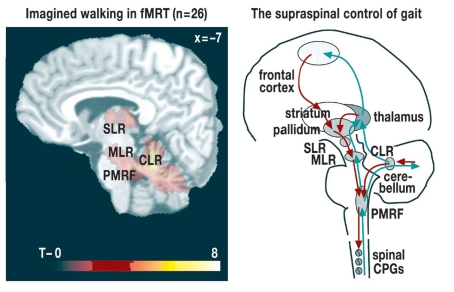
The rhythmic movement pattern of human gait is established at the level of the spinal cord, where so-called central pattern generators, i.e., coordinated groups of interneurons, control the alternating activation of agonist and antagonist muscles during the gait cycle (e1, e2). The existence of autonomous spinal rhythm generators was postulated about 100 years ago, when Thomas Graham Brown demonstrated the persistence of locomotor movements in cats after decerebration, i.e., complete transection of the brainstem. The existence of rhythm generators in man as well is supported by the presence of spinal locomotor movements in paraplegic patients, and by the presence of coordinated movements in all four limbs (arms as well as legs) during bipedal gait (e3, e4). It remains unknown, however, how autonomously the spinal generators control normal human gait; supraspinal control is presumably more important for human, bipedal gait than it is for the quadrupedal gait of the cat. The centers in the spinal cord interact with sensory systems (in particular, the somatosensory afferent pathways) and are under the control of locomotor regions in the brain that enable the initiation of gait, standing still, changes of speed and direction, and reactions to interference with gait. The cerebral control network for gait is schematically shown in Figure 2. Gait is mainly controlled by the premotor and motor areas of the frontal cortex; these areas project fibers to the basal ganglia and onward to the locomotor centers of the brainstem and cerebellum, which, in turn, control the spinal generators. Functional imaging studies have revealed the regions in the human brain that are important for the control of gait (10, 11).
Figure 2.
The supraspinal control of gait in man. The figure at left shows the areas in the cerebellum and brainstem that are revealed to be active by fMRI during imagined walking; the superimposed designations are those of the locomotor areas that are known from experimental studies in animals (p<0.05 FDR, from [11]. The diagram at right shows the current concept of the supraspinal control of human gait. Impulses from the motor and premotor areas of the frontal cortex disinhibit brainstem locomotor areas by way of the basal ganglia. The signal to initiate or alter the pattern of movement travels from the midbrain via the pontomedullary reticular formation to the spinal generators. The rhythm and speed of gait are modulated by the cerebellum. Afferent signals from the limbs (blue) can modulate the pattern of gait through feedback loops, mainly by way of spinocerebellothalamic connections. CLR, cerebellar locomotor region; CPG, central pattern generator; MLR, midbrain locomotor region; PMRF, pontomedullary reticular formation; SLR, subthalamic locomotor region
Classification of gait disturbances
Classification.
A clinically oriented classification is most useful.
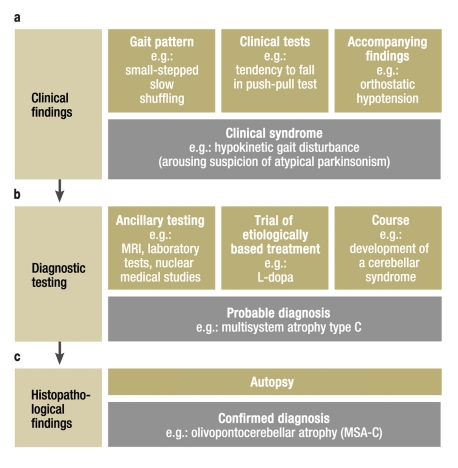
Nutt and Marsden’s proposed classification of gait disturbances into higher-, intermediate-, and lower-level disturbances is in wide use (12). In this scheme, lower-level disturbances involve the peripheral effector organs of locomotion (e.g., arthritis, myopathy, and polyneuropathy); intermediate-level disturbances involve the efferent and afferent sensorimotor pathways of the central nervous system (e.g., paresis after stroke, extrapyramidal manifestations in Parkinson’s disease, and incoordination due to cerebellar dysfunction); and higher-level disturbances involve a deficit of the cortical control of gait (e.g., frontal, anxiety-related, and psychogenic gait disorders). This three-level classification, however, provides only limited help in the clinical setting. The authors prefer to classify gait disorders on the basis of the clinical findings alone, as proposed by Snijders et al. (13), because such a classification is easier to apply in practice (figure 3). Clinical classification is the first of several well-defined steps toward the establishment of a diagnosis. The clinical examination suffices for an initial classification that resists premature anatomical, pathological, or etiological inferences, yet nonetheless points the way to further diagnostic evaluation.
Figure 3.
The diagnostic approach to the classification of gait disturbances
(a) Classification is initially based on the clinical description of the gait disturbances
(b) A probable diagnosis is formulated on the basis of the results of ancillary testing and of the patient’s further course
(c) The definite diagnosis can only be established by autopsy
In this approach, anatomical and etiological classifications are not attempted in stage (a), as these cannot be securely established on clinical grounds alone (e.g., frontal gait disturbance). On the other hand, a correct descriptive designation of the gait disturbance is possible at the beginning, before the ancillary findings and further course are known (e.g., ataxic gait disturbance). Classification modified from Snijders et al. (13)
History, physical examination, and additional diagnostic tests
History
History-taking in elderly patients with gait disturbances enables the physician to assess certain factors that would not be evident from the physical examination alone; some important ones are listed in Table 1. Medications, in particular, often cause dizziness, fluctuating gait unsteadiness, and falls. It can also be very helpful to know what factors tend to precipitate and/or exacerbate the gait disturbance; such information might, for example, reveal that anxiety is a component of the problem.
Table 1. Important aspects of the clinical history in patients with gait disturbances.
| Duration and course |
|
| Precipitating and exacerbating factors |
|
| Accompanying symptoms and signs |
|
| Medications and alcohol |
|
| Comorbidities |
|
| Falls |
|
Clinical presentation
Medications.
These often cause fluctuating gait unsteadiness, dizziness, and falls.
The common types of abnormal gait, whose recognition is the first step in clinical classification (figure 3), are summarized in Table 2. The following types are particularly common among elderly patients seen by neurologists:
Table 2. Descriptive clinical classification of gait disturbances.
| Gait disturbance | Description of gait | Accompanying symptoms and signs |
| Antalgic | Limping, short standing phase on affected leg | Pain, limitation of passive range of movement |
| Paretic | Asymmetry, characteristic motor deficit findings (e.g., steppage gait, Trendelenburg sign) | Paresis, atrophy, reflex asymmetry, radicular/peripheral sensory deficit |
| Spastic | Non-fluent gait, circumduction of the legs, stiffness, scissors gait, forward rotation of the lateral edge of the foot | Elevated muscle tone, brisk reflexes, pyramidal tract signs (Babinski), urge incontinence |
| Ataxic | Broad-based, variable, uncoordinated; worsens when the eyes are closed (proprioceptive-deficit ataxia) | Cerebellar: other cerebellar signs (limb dysmetria, oculo-motor disturbances, dysarthria); Proprioceptive-deficit ataxia: demonstrable proprioceptive deficit |
| Sensory deficit | Broad-based, variable, diminished swing phase, worsens when another system is impaired (e.g., with eyes closed) | BVP: oscillopsia, pathological head-impulse test; PNP: diminished reflexes, sensory deficit |
| Hypokinetic | Small-stepped, slow, shuffling; difficulty initiating movement in parkinsonism; diminished arm swing, worsening with cognitive dual-tasking | Parkinsonism: rigidity, tremor, akinesia; Vascular/NPH: cognitive impairment, incontinence |
| Dyskinetic | Involuntary movements during ambulation | Dystonia, chorea, myoclonus, tics |
| Anxious | Slow, broad-based (“walking on ice”); search for something to hold on to; improvement with minimal assistance or with dual-tasking (distraction) | Fear of falling, intolerance of standing without holding on to something |
| Psychogenic | Multiple patterns: bizarre, variable, exhausting, very slow, sudden buckling without falling | Affect (“la belle indifférence”), possible precipitating life situations, prior psychiatric history |
BVP, bilateral vestibulopathy; NPH, normal-pressure hydrocephalus; PNP, polyneuropathy
sensory (e.g., polyneuropathy),
hypokinetic (e.g., Parkinson’s disease),
ataxic (e.g., degenerative cerebellar atrophy),
anxiety-related (e.g., fear of falling).
Antalgic gait disturbances (e.g., arthritis) and paretic gait disturbances (e.g., radiculopathy after disk herniation) account for a considerable percentage of the gait disturbances seen by general practitioners, orthopedists, and neurologists. Spastic, dyskinetic, and psychogenic gait disturbances are found in old age, but no more commonly than at any other time of life.
The patient’s gait can be analyzed in a number of ways. The simplest is clinical observation of the patient, who is asked to walk a certain distance with the eyes open and closed, as well as during distraction and/or performance of a cognitive task. The examiner should note the patient’s posture, speed of gait, any asymmetry, the width and length of steps, the height of the feet above the ground in each step, the variability of steps, disequilibrium with gait deviation and/or tendency to fall, and the accompanying arm swing. Experienced examiners can usually classify the gait disturbance correctly by observation alone (table 2).
Alongside various tests of stance and gait (walking with the eyes closed, tandem stance/gait, standing on one leg, heel and toe walking), the clinical assessment of gait disturbances in old age also includes the evaluation of sensory deficits (visual, vestibular, somatosensory). Further important components are a complete neurological examination (including eye movements and the motor function of the limbs), an assessment of the active and passive ranges of motion of the large joints, and a general medical examination.
Timed tests, such as the timed up-and-go test, involve measuring the time it takes for the patient to carry out a given motor sequence. Such tests are commonly used, easy to perform, and thus useful for longitudinal assessment (14). They yield numerical parameters of mobility beyond the simple ability to walk. In the timed up-and-go test, the patient sits on a standard armchair. When the signal is given, he or she stands up, walks three meters, turns around, walks back to the chair, and sits down again. The time it takes to do this is recorded.
The pull test of righting reflexes provides a very useful index of the risk of falling. This test exists in many variants (15). Most commonly, the examiner stands behind the patient and exerts a sudden, brief backward pull on the shoulders. The patient is warned beforehand of what is going to happen; the eyes are open, and the feet are a comfortable distance apart (16).
Clinical gait assessment.
Observe the patient walking, first with the eyes open and then with the eyes closed.
The examiner assesses the patient’s ability to respond to this interference by rapidly correcting stance and/or by taking a step backward. If a disease is present that impairs the righting reflexes (e.g., progressive supranuclear palsy), the patient will respond inadequately and will have to be caught, no matter whether the perturbation was expected.
Additional diagnostic tests
Test procedures.
The “pull” test of the righting reflex is useful for assessing the patient’s risk of falling.
Ancillary tests are used to provide specific confirmation for the provisional diagnosis that has already been formulated on the basis of the history and physical examination, and they should thus be performed selectively. Sensory testing is often a useful component of basic neurological assessment in elderly patients with gait disturbances. It includes testing of the visual acuity and fields (visual testing), the head-impulse test for the vestibulo-ocular reflex and caloric testing for vestibular inner ear function (vestibular testing), and measurement of nerve conduction velocities (somatosensory testing). The type and extent of neuroimaging studies that are required depend on the abnormalities disclosed by the clinical assessment.
Important aspects of the clinical history.
Comorbidities, medications, alcohol, accompanying signs and symptoms, and precipitating/exacerbating factors.
Newer diagnostic procedures
Dual-tasking ability
The reciprocal interaction of cognitive function and gait is a fascinating area of research, with practical clinical implications. Tests of dual-tasking ability are relatively easy to integrate in the clinical examination. The patient should be asked to walk while performing either a cognitive task (e.g., backward calculations, listing words in a particular category) or a motor task (e.g., carrying an object or performing a specific movement with the hands). The “stop walking while talking” sign is a typical finding when the interaction between gait and cognition is disturbed (17) and can also be used as a clinical test (18, 19). Worsening gait during dual tasking is characteristic of gait disturbances whose cause lies at the cortical or subcortical level (e.g., neurodegenerative dementia, vascular gait disturbances), as well as of parkinsonism. Many patients show a paradoxical reversal of the normal “posture first” strategy, instead interrupting walking in order to perform the second task (13). On the other hand, patients whose gait disturbance is anxiety-related or psychogenic tend to walk better when they are distracted by a second task.
Gait analysis
Video systems have been introduced for clinical gait analysis; ideally, video recordings should be made both from the front and from the side (9). Recordings enable multiple, observer-independent assessments of gait. Quantitative gait analysis, up to and including the three-dimensional registration of all joint movements, is the most precise method of gait assessment. Quantitative analysis is a useful aid in the differential diagnostic classification of gait disturbances, because the highly standardized measurements and the performance of the test under various different conditions give it a higher diagnostic value than mere observation. Nevertheless, this comes at the price of labor-intensive analysis. Simplified systems (video systems, pressure-sensitive floor mats) are useful for the intra-individual longitudinal assessment of patients with certain types of disorders (e.g., normal-pressure hydrocephalus before and after the removal of cerebrospinal fluid [CSF], Parkinson’s disease before and after a change of medication schedule).
Functional imaging
Newer diagnostic methods.
The history and physical examination should both include an assessment of the patient’s dual-tasking ability.
Functional magnetic resonance imaging (fMRI) and nuclear medical methods such as 18FDG-PET can be used to demonstrate the supraspinal activity associated with different patterns of gait and the cortical correlates of sensory control (10). These methods can reveal, for example, the human correlates of the cerebellar and brainstem locomotor centers known from animal research, whose function may be impaired in gait disturbances of central origin (figure 2) (11). They do not yet have any clinical application. fMRI and 18FDG-PET provide complementary information: the former is used to study imagined walking, which can be modified at will, while the latter is used to study actual walking. Findings obtained during actual walking are less dependent on the subject’s ability to cooperate; this is an important consideration for elderly patients with gait disturbances of neurodegenerative origin (20).
The main types of gait disturbance in old age
Physiotherapy includes:
Directed sensory exercises, balance and coordination training, biomechanical training
The neurological diseases that arise mainly in old age and have a gait disturbance as their major clinical manifestation are listed in Table 3, along with the basic components of the treatment for each. Gait disturbances in old age are often of multifactorial origin. The treatment consists of specific therapy for each of the identified components and may include physiotherapy, medications, behavioral therapy, and, in rare cases, surgery. Although physiotherapy is an important part of treatment for nearly all types of gait disorders, its efficacy has not been demonstrated in controlled studies, even for common disorders (21). Particular varieties of physiotherapy can be applied specifically only when the patient’s deficits have been appropriately diagnostically categorized; sensory exercises, balance and coordination training, and biomechanical training can then be used as indicated. Fall prevention measures for patients at risk of falling include patient education, training, and instruction (e.g., regarding suitable shoes). Patients at very high risk of falling should be given appropriate mechanical aids. Whenever parkinsonism (either idiopathic Parkinson’s disease or an atypical parkinsonian syndrome) is suspected, a therapeutic trial with an L-dopa preparation should be performed. The dose should be slowly increased over a period of two weeks to a maximum of about 1000 mg/day in 3 to 5 divided doses, until the therapeutic effect is adequate or side effects arise. If there is still no effect, or only a questionable effect, at two weeks, then the medication should be discontinued; it is important that this should be done gradually. Three specific diagnoses merit special emphasis in the following sections, because they are clinically important, albeit relatively little known: bilateral vestibulopathy, normal-pressure hydrocephalus, and anxiety-related gait disturbance.
Table 3. Some neurological gait disturbances that are more common in the elderly.
| Diagnosis | Clinical manifestations | Treatment options |
| Sensory deficits | ||
| Polyneuropathy |
|
|
| Bilateral vestibulopathy |
|
|
| Visual impairment |
|
|
| Neurodegenerative disorders | ||
| Parkinsonism |
|
|
| Cerebellar ataxia |
|
|
| Dementing syndromes |
|
|
| Other | ||
| Vascular encephalopathy (MRI, Figure 1b) |
|
|
| Normal-pressure hydrocephalus (MRI, Figure 1a) |
|
|
| Anxious gait disorder (fear of falling) |
|
|
| Toxic (medications, alcohol) |
|
|
PNP, polyneuropathy; SSRI, selective serotonin reuptake inhibitor
Bilateral vestibulopathy
Treatment.
Treatment is directed against the particular problems that are identified and consists of physiotherapy, medications, and behavioral therapy.
Bilateral, usually incomplete peripheral vestibular deficits are often overlooked in patients whose presenting manifestations are less than dramatic. The typical symptoms are
gait unsteadiness that worsens in the dark and on uneven ground,
unsteadiness of the visual image (oscillopsia) and blurred vision during walking, as if the environment were in motion relative to the patient, and
impaired spatial orientation.
Common in old age:
Sensory deficits
Neurodegenerative disorders
Important diagnoses and risk factors:
Vascular encephalopathy
Normal-pressure hydrocephalus
Anxiety-related gait disturbances
Toxic causes
The diagnosis is confirmed by the demonstration of bilateral dysfunction of the vestibulo-ocular reflex (head-impulse test, caloric irrigation of the external auditory canals [22, e5]). The most common cause is ototoxic medication (aminoglycosides); degenerative disorders are another common cause in old age, often combined with peripheral neuropathy (22). The initial goal of treatment is to counteract the progressive loss of vestibular function, if possible. Thus, it is important to identify treatable and reversible causes (avoidance of ototoxic medications, supplementation of vitamin B12 deficiency, adequate attack prophylaxis in Ménière’s disease). Regular physiotherapy with gait and balance training is important to promote visual and somatosensory compensation for the deficit (e6). About 50% of patients experience some degree of improvement, although clinical studies have not shown to date that physiotherapy leads to any objective improvement of balance (e7).
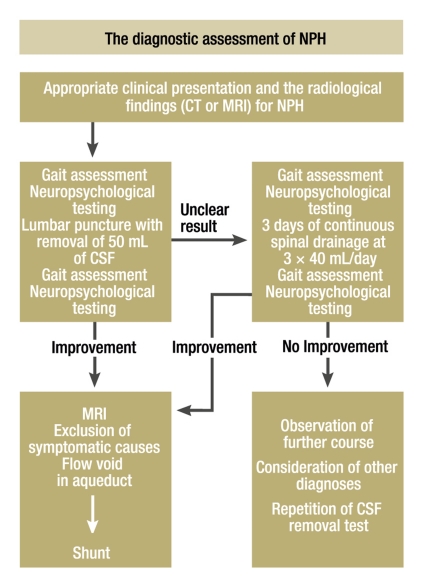
Normal-pressure hydrocephalus
This disease, which classically presents with the clinical triad of gait disturbance, dementia, and urinary incontinence, is important because it is treatable (23). Neuroimaging studies (CT, MRI) show dilated internal CSF spaces and relatively narrow external CSF spaces. Aqueductal stenosis should be excluded by MRI. The gait is typically small-stepped, shuffling, with little rolling of the balls of the feet on each step; the accompanying arm swing is normal, unlike in hypokinetic parkinsonism. The main clinical differential diagnosis is vascular encephalopathy (figure 4), which can present very similarly.
Figure 4.

Typical MRI findings in patients with a “frontal gait disturbance” (axial T2-weighted images):
(a) A man with normal-pressure hydrocephalus (ventriculomegaly, narrow sulci)
(b) A man with vascular encephalopathy (marked white-matter hyperintensities, normal ventricular size)
Patient A could benefit from the insertion of a ventriculoperitoneal shunt, while Patient B could benefit from tight medical treatment of his blood pressure.
Bilateral vestibulopathy.
Typical symptoms include unsteady gait that worsens in the dark and movement of the visual image while walking.
The diagnostic assessment is shown in Figure 5. A single CSF removal test is of low specificity (30% to 60%), but repeated tests over several days are much more specific (60% to 100%) (e8). The reported success rate of ventriculoperitoneal shunting varies considerably from study to study (30% to 100%), and appropriate patient selection is the key. The results tend to be best when the gait disturbance is the patient’s main problem and when other potential causes for it are not simultaneously present (e9). When rational diagnostic assessment yields the diagnosis of normal-pressure hydrocephalus, surgery is advisable because it can lead to improvement both of the gait disturbance and of the cognitive deficits, which would otherwise progress.
Figure 5.
A diagnostic algorithm for cases of suspected normal-pressure hydrocephalus. Important differential diagnoses include other central gait disorders, such as vascular gait disturbance in cerebral microangiopathy and hypokinetic parkinsonian syndromes.
Normal-pressure hydrocephalus.
The typical clinical triad consists of gait disturbance, dementia, and urinary incontinence.
Anxiety-related gait disturbance
Many elderly patients with gait disturbances are afraid of falling, and this fear itself can be a major contributor to gait impairment. The prevalence of anxiety-related gait disturbance in elderly patients is said to be as high as 85% when milder forms are included (24). Anxious patients walk more slowly than age-matched controls, yet their gait parameters are in the physiological range when normed for speed (24). The fear of falling is associated with anxiety disorders and depression, and it considerably impairs the quality of life (25). Increasingly avoidant behavior further lowers these patients’ confidence in their own walking ability, with the result that the symptoms worsen, in a downward spiral (13). The gait disturbance does not worsen during dual tasking and improves with minimal assistance. As these patients’ anxiety tends to increase and their mobility tends to decrease over time, it is important to provide timely behavior-therapeutic and pharmacological treatment of their psychiatric comorbidity.
Anxiety-related gait disturbances.
Increasingly avoidant behavior further lessens the patient’s confidence in his or her own balancing ability; thus, the symptoms worsen in a downward spiral.
A trial of medication with a selective serotonin reuptake inhibitor to treat anxiety and depression is often useful, although there are no controlled studies with anxiety-related gait disorders as the indication. Behavioral therapy can be provided, with the aim of helping patients regain confidence in their own ability to stand and walk safely by means of education and desensitization (e10). Although a relatively large number of studies of behavioral therapy for this indication have been published, there are still no prospective, long-term studies available.
Further Information on CME.
This article has been certified by the North Rhine Academy for Postgraduate and Continuing Medical Education.
Deutsches Ärzteblatt provides certified continuing medical education (CME) in accordance with the requirements of the Medical Associations of the German federal states (Länder). CME points of the Medical Associations can be acquired only through the Internet, not by mail or fax, by the use of the German version of the CME questionnaire within 6 weeks of publication of the article. See the following website: cme.aerzteblatt.de
Participants in the CME program can manage their CME points with their 15-digit “uniform CME number” (einheitliche Fortbildungsnummer, EFN). The EFN must be entered in the appropriate field in the cme.aerzteblatt.de website under “meine Daten” (“my data”), or upon registration. The EFN appears on each participant’s CME certificate.
The solutions to the following questions will be published in issue 25/2010.
The CME unit “Child Abuse and Neglect: Diagnosis and Management” (issue 13/2010) can be accessed until 14 May 2010.
For issue 21/2010 we plan to offer the topic “Endometriosis.”
Solutions to the CME questionnaire in issue 9/2010: Michael JWP, Schlüter-Brust KU, Eysel P: The Epidemiology, Etiology, Diagnosis, and Treatment of Osteoarthritis of the Knee.
1e, 2d, 3c, 4d, 5a, 6e, 7a, 8a, 9b, 10a
Please answer the following questions to participate in our certified Continuing Medical Education program. Only one answer is possible per question. Please select the answer that is most appropriate.
Question 1
What is the prevalence of gait disturbances in persons over age 70, according to a population-based study?
15%
25%
35%
45%
55%
Question 2
A 78-year-old man presents with a small-stepped, broad-based gait with good arm swing. His cognitive function is impaired; in particular, his dual-tasking ability is reduced. What is the most likely diagnosis?
Cerebellar ataxia
Parkinson’s disease
Bilateral vestibulopathy
Vascular encephalopathy
Polyneuropathy
Question 3
What is the characteristic clinical triad of normal-pressure hydrocephalus?
Unsteady gait, impaired dual tasking, ulcerative colitis
Hypokinetic gait, limb ataxia, constipation
Fluctuating gait disturbance, impaired vision, parkinsonism
Anxiety-related gait disorder, aphasia, Crohn’s disease
Apraxic gait, dementia, urinary incontinence
Question 4
Which medications frequently cause bilateral vestibulopathy?
Aminoglycosides
Selective serotonin reuptake inhibitors
Benzodiazepines
Beta-blockers
Nonsteroidal anti-inflammatory drugs
Question 5
Which of the following is an uncommon treatment for gait disturbances in the elderly?
Behavioral therapy
Physiotherapy
Surgery
Medications
Biomechanical training
Question 6
A 63-year-old woman with diabetes mellitus has developed an increasingly unsteady gait in recent months. Physical examination reveals a primarily distal sensory deficit and a loss of the ankle-jerk reflexes. What is the diagnosis?
Cerebellar ataxia
Anxiety-related gait disorder
Toxic cause
Parkinsonism
Polyneuropathy
Question 7
What deficits and deviations from the age-specific norm should be taken into account in the clinical classification of a gait disturbance in an elderly patient?
Speed, length of steps, breadth of stance
Reaction time, stability of stance, breadth of steps
Coordination, center of gravity of body, ability to sway back and forth
Biometric data, impulse, foot posture
Tangential speed, hand and foot coordination
Question 8
What form of treatment for anxiety-related gait disturbances has been relatively well documented in clinical studies?
Hypnosis
Talk therapy
Psychoanalysis
Behavioral therapy
Gestalt therapy
Question 9
What part of the brain modulates the rhythm and speed of gait?
Striatum
Midbrain
Pallidum
Cerebellum
Parietal cortex
Question 10
In what type of gait disturbance does the patient’s gait actually improve during dual tasking?
Psychogenic
Vascular
Dyskinetic
Spastic
Ataxic
Case.
A 67-year-old retired white-collar worker complains of progressively severe dizziness and gait unsteadiness over the past two years. On questioning, he says that he feels fine at rest but senses a continuous swaying while he walks. His gait is most unsteady in the dark or when he goes for a hike in the woods. His vision is normal, except for presbyopia; nonetheless, he has to stand still to read street signs, because the writing jumps around if he attempts to read while walking. He finds the gait unsteadiness disturbing, but has not fallen because of it. His other medical conditions are arterial hypertension and chronic gastritis. He is taking pantoprazole, ramipiril, and hydrochlorothiazide.
The clinical examination reveals only mild gait unsteadiness, with normal-sized steps and a mildly broad base. The accompanying arm swing is normal. The pattern and speed of gait do not change when he has to perform a cognitive task while walking (dual-task subtraction test). On the other hand, the gait disturbance worsens markedly when he is asked to stand, and then to walk, with the eyes closed: there is then a tendency to fall in all directions. The head-impulse test for the horizontal vestibule-ocular reflex induces pathological saccadic movements on both sides. The remainder of the examination reveals a mild polyneuropathic syndrome, with unelicitable ankle-jerk reflexes and loss of vibration sense in the feet.
The typical history (unsteady gait in the dark and on uneven ground, oscillopsia) and the findings on clinical examination (pathological head-impulse test) enable the examiner to diagnose a bilateral disturbance of peripheral vestibular function (bilateral vestibulopathy). This diagnosis is confirmed by caloric testing (no nystagmus is generated when the external ear canals are irrigated with either cold or warm water). Vestibular nystagmus cannot be induced by spinning the patient in a rotating chair. Laboratory tests are performed to investigate the underlying cause of the disturbance: they reveal a marked deficiency of vitamin B12 (less than 100 pg/mL) and microcytic anemia. Vitamin B12 deficiency is a possible cause of bilateral vestibulopathy. The patient is treated with vitamin B12 supplementation and physiotherapeutic balance training for stance and gait. Within a few months, his gait stabilizes. He feels better because he knows the cause of the problem, experiences less dizziness, and knows how to avoid unfavorable situations (he has given up evening strolls along the beach). His peripheral vestibular function remains impaired.
Acknowledgments
Translated from the original German by Ethan Taub. M.D.
Footnotes
Conflict of interest statement
The authors declare that they have no conflict of interest as defined by the guidelines of the International Committee of Medical Journal Editors.
References
- 1.Stolze H, Klebe S, Baecker C, et al. Prevalence of gait disorders in hospitalized neurological patients. Mov Disord. 2005;20:89–94. doi: 10.1002/mds.20266. [DOI] [PubMed] [Google Scholar]
- 2.Verghese J, Levalley A, Hall CB, Katz MJ, Ambrose AF, Lipton RB. Epidemiology of gait disorders in community-residing older adults. J Am Geriatr Soc. 2006;54:255–261. doi: 10.1111/j.1532-5415.2005.00580.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sudarsky L. Gait disorders: prevalence, morbidity, and etiology. Adv Neurol. 2001;87:111–117. [PubMed] [Google Scholar]
- 4.Stolze H, Klebe S, Zechlin C, Baecker C, Friege L, Deuschl G. Falls in frequent neurological diseases - prevalence, risk factors and aetiology. J Neurol. 2004;251:79–84. doi: 10.1007/s00415-004-0276-8. [DOI] [PubMed] [Google Scholar]
- 5.Alexander NB. Definition and epidemiology of falls and gait disorders. In: Sirven JI, Malamut BL, editors. Clinical neurology of the older adult. Philadelphia: Lippincott Williams & Wilkins; 2002. pp. 108–116. [Google Scholar]
- 6.Jorstad EC, Hauer K, Becker C, Lamb SE. Measuring the psychological outcomes of falling: a systematic review. J Am Geriatr Soc. 2005;53:501–510. doi: 10.1111/j.1532-5415.2005.53172.x. [DOI] [PubMed] [Google Scholar]
- 7.Hough JC, McHenry MP, Kammer LM. Gait disorders in the elderly. Am Fam Physician. 1987;35:191–196. [PubMed] [Google Scholar]
- 8.Ashton-Miller JA. Age-associated changes in the biomechanics of gait and gait-related falls in older adults. In: Hausdorff JM, Alexander NB, editors. Gait disorders: evaluation and management. Boca Raton: Taylor & Francis; 2005. pp. 63–100. [Google Scholar]
- 9.Stolze H, Vieregge P, Deuschl G. Gait disturbances in neurology. Nervenarzt. 2008;79:485–499. doi: 10.1007/s00115-007-2406-x. [DOI] [PubMed] [Google Scholar]
- 10.Jahn K, Deutschlander A, Stephan T, Strupp M, Wiesmann M, Brandt T. Brain activation patterns during imagined stance and locomotion in functional magnetic resonance imaging. Neuroimage. 2004;22:1722–1731. doi: 10.1016/j.neuroimage.2004.05.017. [DOI] [PubMed] [Google Scholar]
- 11.Jahn K, Deutschlander A, Stephan T, et al. Imaging human supraspinal locomotor centers in brainstem and cerebellum. Neuroimage. 2008;39:786–792. doi: 10.1016/j.neuroimage.2007.09.047. [DOI] [PubMed] [Google Scholar]
- 12.Nutt JG, Marsden CD, Thompson PD. Human walking and higher-level gait disorders, particularly in the elderly. Neurology. 1993;43:268–279. doi: 10.1212/wnl.43.2.268. [DOI] [PubMed] [Google Scholar]
- 13.Snijders AH, van de Warrenburg BP, Giladi N, Bloem BR. Neurological gait disorders in elderly people: clinical approach and classification. Lancet Neurol. 2007;6:63–74. doi: 10.1016/S1474-4422(06)70678-0. [DOI] [PubMed] [Google Scholar]
- 14.Yelnik A, Bonan I. Clinical tools for assessing balance disorders. Clin Neurophysiol. 2008;38:439–445. doi: 10.1016/j.neucli.2008.09.008. [DOI] [PubMed] [Google Scholar]
- 15.Hunt AL, Sethi KD. The pull test: a history. Mov Disord. 2006;21:894–899. doi: 10.1002/mds.20925. [DOI] [PubMed] [Google Scholar]
- 16.Munhoz RP, Li JY, Kurtinecz M, Piboolnurak P, et al. Evaluation of the pull test technique in assessing postural instability in Parkinson’s disease. Neurology. 2004;62:125–127. doi: 10.1212/wnl.62.1.125. [DOI] [PubMed] [Google Scholar]
- 17.Lundin-Olsson L, Nyberg L, Gustafson Y. “Stops walking when talking” as a predictor of falls in elderly people. Lancet. 1997;349 doi: 10.1016/S0140-6736(97)24009-2. [DOI] [PubMed] [Google Scholar]
- 18.Verghese J, Kuslansky G, Holtzer R, et al. Walking while talking: effect of task prioritization in the elderly. Arch Phys Med Rehabil. 2007;88:50–53. doi: 10.1016/j.apmr.2006.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hausdorff JM, Schweiger A, Herman T, Yogev-Seligmann G, Giladi N. Dual-task decrements in gait: contributing factors among healthy older adults. J Gerontol A Biol Sci Med Sci. 2008;63:1335–1343. doi: 10.1093/gerona/63.12.1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.La Fougère C, Zwergal A, Rominger A, et al. Real versus imagined locomotion: a [18F]-FDG PET - fMRI comparison. Neuroimage. 2010 doi: 10.1016/j.neuroimage.2009.12.060. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 21.Morris ME. Locomotor training in people with Parkinson disease. Phys Ther. 2006;86:1426–1435. doi: 10.2522/ptj.20050277. [DOI] [PubMed] [Google Scholar]
- 22.Zingler VC, Cnyrim C, Jahn K, et al. Causative factors and epidemiology of bilateral vestibulopathy in 255 patients. Ann Neurol. 2007;61:524–532. doi: 10.1002/ana.21105. [DOI] [PubMed] [Google Scholar]
- 23.Vanneste JA. Diagnosis and management of normal-pressure hydrocephalus. J Neurol. 2000;247:5–14. doi: 10.1007/s004150050003. [DOI] [PubMed] [Google Scholar]
- 24.Reelick MF, van Iersel MB, Kessels RP, Rikkert MG. The influence of fear of falling on gait and balance in older people. Age Ageing. 2009;38:435–440. doi: 10.1093/ageing/afp066. [DOI] [PubMed] [Google Scholar]
- 25.van Haastregt JC, Zijlstra GA, van Eijk JT, et al. Feelings of anxiety and symptoms of depression in community-living older persons who avoid activity for fear of falling. Am J Geriatr Psychiatry. 2008;16:186–193. doi: 10.1097/JGP.0b013e3181591c1e. [DOI] [PubMed] [Google Scholar]
- e1.Grillner S, Brooks VB. Control of locomotion in bipeds, tetrapods and fish. Handbook of physiology, the nervous system, vol. II, motor control, part 2. Bethesda, MD: American Physiological Society. 1981:1179–1236. [Google Scholar]
- e2.Dietz V. Spinal cord pattern generators for locomotion. Clin Neurophysiol. 2003;114:1379–1389. doi: 10.1016/s1388-2457(03)00120-2. [DOI] [PubMed] [Google Scholar]
- e3.Dietz V, Colombo G, Jensen L. Locomotor activity in spinal man. Lancet. 1994;344:1260–1263. doi: 10.1016/s0140-6736(94)90751-x. [DOI] [PubMed] [Google Scholar]
- e4.Dietz V. Do human bipeds use quadrupedal coordination? Trends Neurosci. 2002;25:462–467. doi: 10.1016/s0166-2236(02)02229-4. [DOI] [PubMed] [Google Scholar]
- e5.Strupp M, Brandt T. Diagnosis and treatment of vertigo and dizziness [Leitsymptom Schwindel: Diagnose und Therapie] Deutsches Ärzteblatt Int. 2008;105:173–180. doi: 10.3238/arztebl.2008.0173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e6.Krebs DE, Gill-Body KM, Parker SW, et al. Vestibular rehabilitation: useful but not universally so. Otolaryngol Head Neck Surg. 2003;128:240–250. doi: 10.1067/mhn.2003.72. [DOI] [PubMed] [Google Scholar]
- e7.Herdman SJ. 3rd edition. Philadelphia: FA Davis Company; 2007. Vestibular rehabilitation. [Google Scholar]
- e8.Gallia GL, Rigamonti D, Williams MA. The diagnosis and treatment of idiopathic normal pressure hydrocephalus. Nature Clin Pract Neurol. 2006;2:375–381. doi: 10.1038/ncpneuro0237. [DOI] [PubMed] [Google Scholar]
- e9.Tsakanikas D, Relkin N. Normal pressure hydrocephalus. Seminars Neurol. 2007;27:58–65. doi: 10.1055/s-2006-956756. [DOI] [PubMed] [Google Scholar]
- e10.Legters K. Fear of falling. Phys Ther. 2002;82:264–272. [PubMed] [Google Scholar]