Abstract
Osteotomies around hip acetabulum have become a routine surgical intervention in cases with constant pain without joint degeneration in adult dysplasia. However, it remains a challenge to plan and realign optimally the joint after osteotomy to reach best function and longevity in the clinical outcome. Tool tracking navigation systems have been available for many years but they have not become popular among surgeons because they extend operation time, require preoperative CT scan and, on the other hand, produce only marginal advantage in hands of an experienced surgeon. Real-time biomechanical assessment, based on computer analysis using preoperative CT-scanning, has become an interesting means to adjust the acetabular reorientation during surgery according to the patient’s individual structure and loading conditions. Further, real-time feedback allows the surgeon to foresee radiographic angles while performing fixation of the osteotomized fragment. Assessment of peak pressure and potential weight bearing area in real-time allows prospective and retrospective systematic biomechanical studies of patient outcomes. To conclude, a major development in navigation software is under way and we have so far seen a spectrum of new features like loading condition assessment in real time for osteotomies. This is, however, merely the start of a revolutionary change in operative planning in orthopaedics with the help of computer aided guiding and bioengineering.
Challenges in Periacetabular Hip Osteotomies
The original idea to develop navigational means for acetabular osteotomies comes from the facts that this type of operation is technically extremely challenging and for the patient it poses more risks than e.g. regular hip arthroplasties. In this article the surgical bony cuts made to release the acetabular fragment are built on technical modification of the Bernese type of osteotomy (1), which maintains the integrity of posterior pillar, but does not break the acetabular contact surface covered with cartilage within the joint.
Indications for acetabular realignment lie not only in hip dysplasia but in any structural changes that tend to cause repeated subluxation of the joint resulting in hip pain without joint degeneration. It is widely accepted that optimal cases for surgical correction do not have femoral deformities since congruency of the joint after osteotomy is a prerequisite for good clinical outcome. In our practice nowadays, after experiences since 1991 with more than 350 cases, we do not recommend overlooking joint congruency or major radiographic degeneration.
The challenge of periacetabular osteotomy is to cut bone around the joint but maintain intact muscle insertions. The exposure technique has developed remarkably since the beginning of 1990s leaving e.g. rectus femoris muscle’s upper regions intact. The exposure size can probably be further reduced in the future by using computerized tool-tracking that may allow safe and accurate cutting of bone inferior to acetabulum. The danger zone lies laterally below the acetabulum due to the close vicinity of the sciatic nerve. In our patient series, there have been two permanent but partial sciatic palsies after osteotomy (unpublished observation).
The major challenge is to reach optimal joint loading conditions despite variations in the grade of dysplasia and variations in individual pelvic structure. It is self-evident that optimal loading conditions can be achieved only if we can provide the capability to assess these loading conditions before and/or during the procedure. Radiographic angles depicting joint contact surface orientation do not necessarily coincide with biomechanically assessed parameters (2). Therefore, it remains unclear whether we can perform periacetabular osteotomy optimally with preoperative radiographic angles alone.
The first generation computer aided navigation
History
Since the very first computer aided navigation tools appeared in neurosurgery and later in spine surgery, tool-tracking became the first computer-aided means also in acetabular osteotomies (3,4). Later, in knee surgery, a major breakthrough was achieved by introducing an algorithm for real time assessment of the mechanical axis of femur, three dimensionally. This was the first example of computer-based help in terms of loading conditions and it nowadays can be used during surgery to guide the surgeon in cases of femoral shaft deformities. The algorithm was based on finding the rotational center of the upper femur without anatomical considerations; i.e. no preoperative CT scan was needed.
Successful registration of the anatomical landmarks with ones corresponding to those in virtual, computer tomography based, three dimensional images, made it possible to achieve reliable tool tracking during periacetabular osteotomy. This allowed the surgeon to check that the tip of the chisel was safely placed and properly directed against the bone before hammering the chisel and checking its cutting progress between hits. It also allowed the surgeon to get familiar with anatomical variations intraoperatively.
In preoperative planning, assessment of the acetabular contact surface has been described that estimates weight bearing using an alternative to biomechanical finite element analysis (5).
Drawbacks
This so-called first generation of navigation techniques has its drawbacks. The major one is the need to reserve extra time both before and during surgery. This extra time effort outweighed the possible benefits since surgeons performing these osteotomies were mostly experienced and did not feel that navigation presented any major surgical benefit. Also, clinically, there is no expected improvement in final outcome since experienced surgeons can reach acceptable safety level repeatedly without simultaneous tool tracking.
Developing the second generation navigation – real-time biomechanical feedback (BGS)
A surprisingly wide spectrum of joint contact surfaces appear in patients with hip dysplasia with significant variation in shape, size and overall alignment of the joint contact surface in relation to the pelvic structures (Fig. 1). Therefore, to reach optimal fixation and simultaneously be able to correct joint stability and cartilage weight bearing, one somehow needs to take into consideration these individual variations. Many times even indications for this type of surgery are in question. CT-scan (6,7) helps the surgeon not only to redefine the presence of arthritic changes but allows estimation of femoral coverage in three dimensions (Fig. 2). This has led us to strive to develop a software system with intraoperative means to measure contact surface opening angles in three dimensions and to produce simultaneous estimates of biomechanically measured loading pattern (Fig. 3). To take into account different joint loading situations experienced during activities of daily living, we added an estimate of joint loading measures typical in standing, but also those loads seen during walking and lowering oneself into a chair (Fig. 4).
Fig. 1.
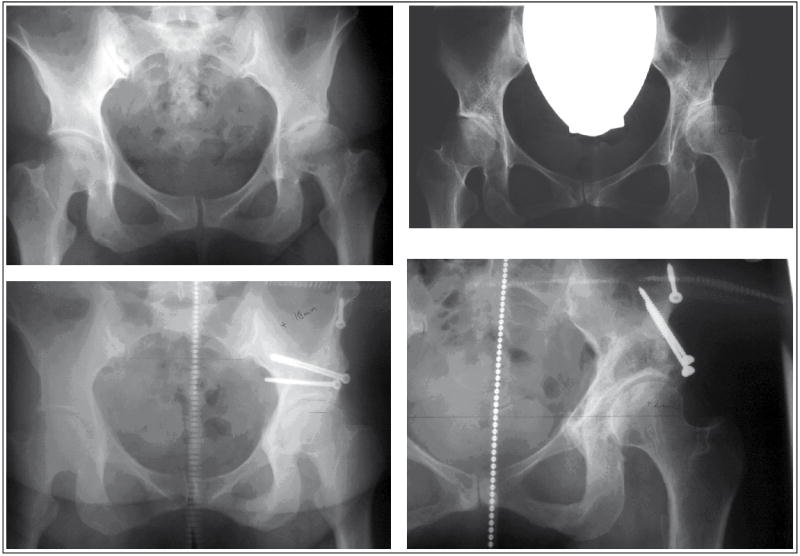
On the left side a case with only slightly from normal deviated AC angle pre- and postoperatively. However, femoral coverage is deficient. On the right hand side there is an example of a case with markedly abnormal AC angle and CE angle and hence a true subluxation of the femur.
Fig. 2.
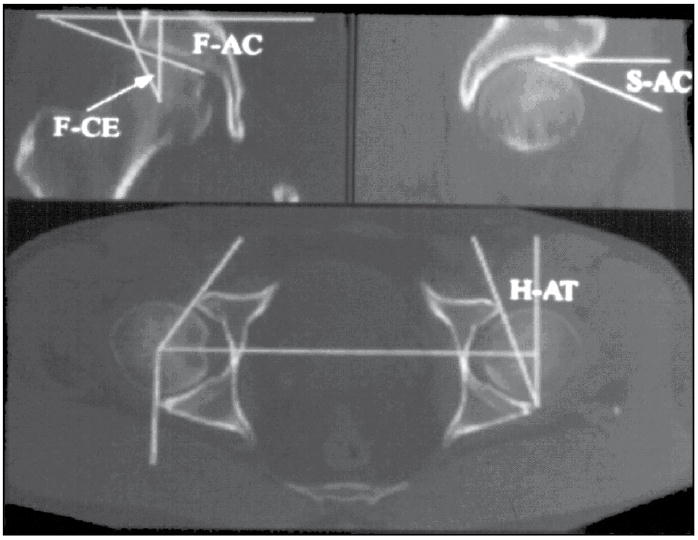
An illustration showing the angles in reformatted CT scan depicting orientation of acetabular contact surface in relation to other pelvic structures (6,7).
Fig. 3.
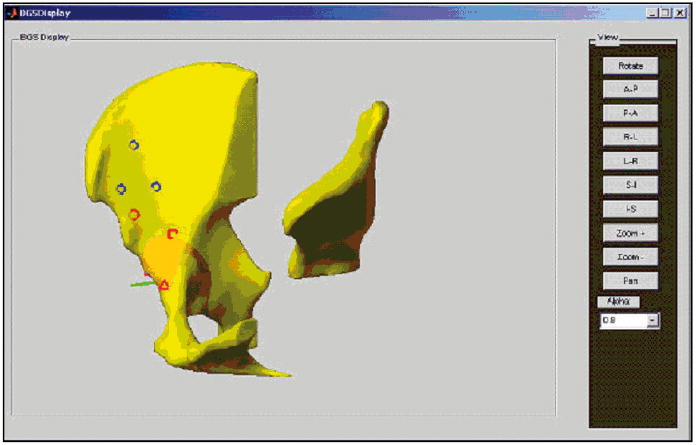
An illustration showing spots for landmarks on bone during matching. The prerequisite for successful matching was to find a way to define landmarks on the osteotomized fragment and on the pelvic structures. We have burred small holes on the surface of the bone to avoid another reference base which would have interfered with surgery itself. Surgical exposure with BGS has been exactly the same as usual.
Fig. 4.
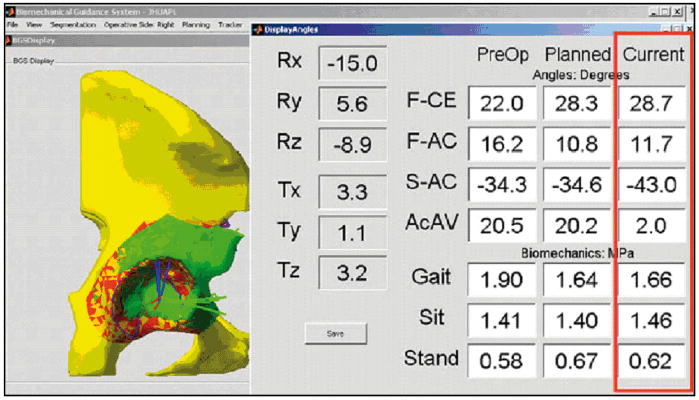
View of the computer monitor during surgery. BGS shows a real time estimate of the angles and biomechanical situation with peak pressure at the acetabular contact surface (9). Note that peak pressure is presented in three different clinical situations namely gait, sit and stand. Predicted radiographic angles are presented along with the biomechanical estimate.
Fixing the fragment during surgery is always more or less affected by the shape of the bone cuts and the quality of bone. Often the situation requires the surgeon to evaluate trade-offs between firm fixation and good alignment. If the surgeon is shown in real time the radiographic angles three dimensionally, it helps him to find the optimal positioning for osteotomized joint. Therefore, it has become important for us to be able to find out the relation between radiologic angles and biomechanically assessed parameters in individual cases (Fig. 4).
Third generation navigation
Features to help in clinical practice
Impingement before or after acetabular osteotomy is surprisingly frequent and one needs to be aware of the risk and be able to avoid it. In many patients femoroacetabular impingement (FAI) presents itself as a separate entity without predisposing acetabular dysplasia (8). Optimally, real-time navigation includes a built-in threshold and warns the surgeon about impingement before fragment fixation. Adding this type of feature is an extensive project itself due to the fact that one should be able to include femoral structure and produce simulation of the joint’s ranges of motion. In addition, it will make it necessary to fix a second dynamic reference base to the femur.
Information about the structure of the femur in conjunction with the acetabular contact surface would allow us to set a goal for minimal congruency after surgery. It is has been shown that femoral deformities may act as a contraindication for reorienting acetabular osteotomy or make it necessary to perform double osteotomy, i.e. simultaneous femoral trochanteric osteotomy to maintain congruency.
Further, preoperative MRI is many times available for these young individuals since they have been thoroughly examined by other doctors prior the referral to surgeons. Adding information about thickened labral tissue from MR images may potentially help us assess joint stability and therefore could serve the purpose of finding the optimal individual loading conditions.
Potentials for outcome studies
Not only real-time navigation, but also prospective patient series with CT-images are important in producing the self-evident link needed between radiographic angles and biomechanical parameters such as peak pressure and weight bearing area. Prospective series with reproducible measurements help us to increase our understanding about variations in 3D structure and biomechanical measures.
Retrospective evaluation with preoperative CT images and angle measurements can help us to understand the relationship between individual variations in joint anatomy and corresponding optimal joint alignment.
Conclusions
Situation today
The disadvantage is that computer assisted guidance requires CT scanning of the pelvic structure. However, real-time navigation offers a tool to improve surgical techniques of the surgeon and creates proper understanding of various anatomies and the risks they pose for surgery. Further, retrospective series of patients analyzed with biomechanical tools can help us to choose in the future the right patients for acetabulum reorienting surgery.
Future prospects
In the near future, we expect to see osteotomies being performed routinely with computer aided real-time navigation with an optional tool tracking system. Further development of instruments and registration techniques is a prerequisite for improving system feasibility and bringing navigation to routine practice in treatment of adult hip dysplasia. Third generation navigation systems possibly combine tracking, biomechanical assessment and MRI.
Acknowledgments
The work performed by our group on computer-aided hip osteotomy with real-time biomechanical guidance was supported by National Institutes of Health / National institute for Biomedical Imaging and Bioenginerring (NIH/NIBIB) under grant numbers 1R01EB006839-01A1 and 1R21EB007747-01.
References
- 1.Ganz R, Klaue K, Vinh T, Mast J. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin OrthopRelat Res. 1988;232:26–36. [PubMed] [Google Scholar]
- 2.Armand M, Lepistö J, Tallroth K, Elias J, Chao E. Outcome of periacetabular osteotomy: joint contact pressure calculation using standing AP radiographs, 12 patients followed for average 2 years. Acta Orthop. 2005;76(3):303–313. [PMC free article] [PubMed] [Google Scholar]
- 3.Langlotz F, Stucki M, Bachler R, Scheer C, Ganz R, Berlemann U. ym: The first twelve cases of computer assisted periacetabular osteotomy. Comput Aided Surg. 1997;2(6):317–326. doi: 10.1002/(SICI)1097-0150(1997)2:6<317::AID-IGS1>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 4.Langlotz F, Bachler R, Berlemann U, Nolte LP, Ganz R. Computer assistance for pelvic osteotomies. Clin Orthop Relat Res. 1998;354:92–102. doi: 10.1097/00003086-199809000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Hipp JA, Sugano N, Millis MB, Murphy SB. Planning acetabular redirection osteotomies based on joint contact pressures. Clin Orthop Relat Res. 1999;364:134–143. doi: 10.1097/00003086-199907000-00018. [DOI] [PubMed] [Google Scholar]
- 6.Lepistö J, Tallroth K, Alho A. Three-dimensional measures of acetabulum in periacetabular osteotomy. Orthopaedic Research Society 44th Annual Meeting. 1998 [Google Scholar]
- 7.Tallroth K, Lepistö J. Computed tomography measurement of acetabular dimensions: Normal values for correction of dysplasia. Acta Orthop. 2006;77:598–602. doi: 10.1080/17453670610012665. [DOI] [PubMed] [Google Scholar]
- 8.Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip – A technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83-B:1119–1124. doi: 10.1302/0301-620x.83b8.11964. [DOI] [PubMed] [Google Scholar]
- 9.Armiger ES, Armand M, Lepisto J, Minhas D, Tallroth K, Mears SC. ym: Evaluation of a computerized measurement technique for joint alignment before and during periacetabular osteotomy. Comput Aided Surg. 2007;12:215–224. doi: 10.1080/10929080701541855. [DOI] [PMC free article] [PubMed] [Google Scholar]


