Abstract
Objective
Quadriceps weakness has been reported with incident but not progressive knee osteoarthritis (OA) in longitudinal studies. This study examined the relationship between quadriceps strength and worsening of knee joint space narrowing (JSN) over 30 months.
Methods
Longitudinal, observational study of adults aged 50-79 years with OARSI JSN score <3 at baseline. Baseline measures included bilateral weight-bearing fixed flexion radiographs, isokinetic concentric quadriceps and hamstring strength, height and weight, and physical activity. Hamstring:quadriceps (H:Q) strength ratios also were evaluated. Worsening was defined as an increase in JSN score in the tibiofemoral and/or patellofemoral compartments on 30-month radiographs or total knee replacement. Knee-based analyses used generalized estimating equations, stratified by sex, to assess relationships between strength and knee JSN while controlling for covariance between knees within subjects as well as age, BMI, history of knee injury and/or surgery, physical activity level and alignment.
Results
3856 knees (1602 male and 2254 female) with JSN score <3 at baseline and no missing follow-up data were included. Mean±SD age was 61.6±8.1 in men and 62.2±7.7 in women. Women in the lowest tertile of quadriceps strength had an increased risk of whole knee JSN (OR=1.66, 95% CI=1.26, 2.19) and tibiofemoral JSN (OR=1.69, 95% CI=1.26, 2.28). However, no associations were found between strength and JSN in men or H:Q<0.6 and JSN in men or women.
Conclusions
In women but not in men, quadriceps weakness was associated with increased risk for tibiofemoral and whole knee JSN.
Keywords: quadriceps muscle strength, hamstring:quadriceps ratio, knee osteoarthritis, rehabilitation
INTRODUCTION
Quadriceps muscle weakness is a common finding in patients with knee osteoarthritis (OA) and has been reported by some,1, 2 but not all3 to be associated with incident knee OA. However, quadriceps weakness has not been found to be associated with progression of knee OA. Risk factors for incident and progressive knee OA can differ, indicating that potentially different mechanisms may be involved.4-6 Although factors such as body weight in the context of malalignment have been found to increase risk for knee OA progression,7 both body weight and knee alignment have proven to be difficult to modify. In contrast, if weakness were a risk factor for knee OA progression, it would be a modifiable risk factor that could be more easily ameliorated. Therefore, there is a need to evaluate whether quadriceps strength alters risk for progression of knee OA.
Quadriceps weakness has been strongly associated with prevalent knee OA,8-12 and evidence suggests that thigh muscle strength may protect against knee joint damage and progression of existing OA. Recent data showed greater lower limb muscle mass was positively associated with medial tibial cartilage volume,13 and lower limb muscle strength at baseline was positively associated with total cartilage volume changes.14 Moreover, there is considerable evidence that lower limb strengthening exercise may improve symptoms.15 Quadriceps weakness potentially could contribute to increased impulse loading of the knee joint.16, 17 The quadriceps muscle also is the primary dynamic stabilizer of the knee in the sagittal plane. Therefore it is possible that weakness of the quadriceps, either absolute or relative to the hamstrings, may adversely redistribute compressive and shear stress at the knee joint.
There have been few longitudinal studies of the relationship between quadriceps weakness and progression of knee OA. Brandt and colleagues found no association between quadriceps strength and knee OA progression in women, despite an earlier report of an association between quadriceps weakness and incident radiographic knee OA in the same cohort.18 Similarly, another longitudinal study of men and women demonstrated no relationship in neutrally aligned knees, although greater quadriceps strength at baseline was reported to increase the likelihood of tibiofemoral OA progression in malaligned and lax knees but have no effect on patellofemoral OA progression.19
A randomized, controlled trial of strength training in individuals over 55 years old found that strength training did not protect against tibiofemoral joint space narrowing over 30 months in subjects with definite knee OA at baseline.20 However, a more recent report found greater quadriceps strength was protective against lateral patellofemoral cartilage loss and did not increase risk for tibiofemoral cartilage loss.21 Discordance in these results may be due to differing outcome measures between the studies - joint space narrowing in the former and cartilage loss (WORMS score) in the latter – or possibly to the smaller sample size in the former. In addition, joint space narrowing is a continuum from a normal knee to one with severe OA, so it may be important to examine the entire continuum, rather than just knees that already have radiographic features of knee OA at baseline assessment. The high prevalence of knee OA in the context of the current low level of understanding of treatment suggests a compelling need for means of reducing risk for progression of knee OA. Therefore, we conducted a multicenter longitudinal study, with sample sizes sufficient to assess the potential modifying effects of sex and lower limb alignment, to evaluate whether quadriceps weakness predicts risk for worsening of knee joint space narrowing.
METHODS
Study Population
The Multicenter Osteoarthritis (MOST) Study is an NIH-funded longitudinal observational study of 3026 community-dwelling men and women age 50-79 with knee osteoarthritis or known risk factors for knee osteoarthritis. Subject enrollment has been previously described.22 Potential subjects were identified by mass mailings or advertisements, screened by telephone for known knee OA risk factors including knee injury or surgery or obesity. Potential participants were excluded for a history of (or planned) bilateral knee replacement, cancer with the exception of non-melanoma skin cancer or breast, cervical, colon, prostate, rectal, or uterine cancer successfully treated with surgery, history of chemotherapy or radiation therapy, rheumatologic disease, or plan to move out of the area in the within 3 years of enrollment. All subjects provided written informed consent using forms approved by the investigators’ institutional review boards. Participating institutions’ review boards approved this study. Only knees with an OARSI joint space narrowing score <3 were eligible for inclusion.23 Knees with pain that “prevented pushing or pulling as hard as” a participant could during the strength test were excluded. Presence of a knee joint injury was assessed by asking participants whether they had ever injured a knee badly enough to limit the ability to walk for at least 2 days.
Baseline Assessments
Anthropometric Measures
Body mass index (BMI, kg/m2) was calculated from baseline weight in kilograms divided by the square of the height in meters (stadiometer, Holtain, Wales, UK), as measured by trained and certified staff.24
Physical Activity
The Physical Activity Scale for the Elderly questionnaire (PASE: New England Research Institute, Watertown, MA) was used for estimating baseline activity level.25-27 The PASE is a validated questionnaire that evaluates frequency and time spent doing specific leisure time, household and work activities in the past 7 days.
Isokinetic Quadriceps and Hamstring Strength Measurement
Isokinetic quadriceps and hamstrings strength for each lower limb was measured using a Cybex 350 computerized dynamometer (HUMAC software version 4.3.2/Cybex 300 for Windows98, Avocent, Huntsville, AL).28 Testing was completed at 60 degrees per second with a chair back angle of 85 degrees by certified examiners using a standardized protocol to assure uniformity among the two test sites. Subjects completed three repetitions at 50% effort to become familiar with the test. After practice trials, four repetitions were completed at maximum effort and the peak torque (N•m) was recorded. To avoid potential pain or injury associated with a maximal eccentric contraction, peak torque was recorded concentrically. The equipment was calibrated monthly according to manufacturer's guidelines. Staff underwent annual recertification to assure uniformity in following the strength testing protocol and standardized script for subject testing. Examiners calibrated the isokinetic dynamometer position, angular velocity, and torque (at 25 and 245 N•m) monthly. The strength testing protocol had a month-to-month test-retest reliability (intraclass correlation coefficient) of .94 (.82-.99), a coefficient of variation of 8% (6-12%) and a within subject variation of 6.3 N•m (4.7-9.6). Following the strength test, participants were asked whether they experienced pain during the test. If the response was affirmative, the participant was then asked “Did this pain prevent you from pushing or pulling as hard as you can?” Participants who responded affirmatively to this second specific question were excluded due to inability to obtain a reliable strength measurement.
Hamstring:Quadriceps muscle strength (H:Q) ratio
The H:Q ratio was calculated by dividing peak concentric hamstring torque by peak concentric quadriceps torque. The H:Q ratio cut-off for lower limb muscle imbalance was set at <0.6 as this is an accepted threshold for normal in young adults.29-31 As we are not aware of normative data for H:Q ratio in older adults, we also conducted secondary analyses dichotomizing H:Q ratio at <0.8.
Baseline and Follow-up Assessments
Knee radiograph assessments
Testing procedures: At baseline, a full lower limb radiograph incorporating both the hip joint and the tibio-talar joint for assessment of knee alignment was obtained. At both baseline and 30-month follow-up examinations, a bilateral, standing fixed flexion posteroanterior view of the tibiofemoral compartments of the knee joint and a unilateral weight-bearing, fixed flexion lateral view of the knees were obtained for assessment of the patellafemoral and TF joint spaces.32 Subjects with unilateral knee replacement did not undergo the lateral x-ray of that side.
Two independent readers, a musculoskeletal radiologist and a rheumatologist experienced in reading study films, assessed PA films for individual radiographic feature scores.32 Joint space narrowing was scored using a modified version of the OARSI criteria on a scale of 0-3.23, 32 The inter-rater reliability of the joint space narrowing score (kappa) was 0.66 (95%CI: 0.61-0.70). Cases of discordant findings were adjudicated by a panel of 3 readers.
Definition of Worsening
At baseline, all eligible knees had a joint space narrowing score of less than 3. Knee OA worsening was defined for 1) the tibiofemoral joint, as an increase in joint space narrowing score of at least 0.5 grades, 2) the patellofemoral joint, as an increase in patellofemoral joint space narrowing score of at least 0.5 grades, and 3) for the whole knee, as an increase in either the tibiofemoral and/or patellofemoral joint space narrowing score of at least 0.5 grades at 30-month follow-up.32 Total knee replacement between baseline and follow-up was also considered worsening. Reports of total knee replacement at follow-up were confirmed by obtaining medical records.
Statistical Methods
All analyses were stratified by sex, due to differences in both strength and OA worsening in men and women. Subject characteristics were summarized with frequencies and means. Since data for the H:Q ratio in older adults with knee osteoarthritis has not been available to date, medians and interquartile ranges were calculated for each knee OA grade and for those with and without joint space narrowing on follow-up. Subjects were grouped into sex-specific tertiles of baseline quadriceps strength (peak torque over 4 trials) and dichotomous H:Q ratios. A normalized measure of quadriceps strength was calculated from the regression line of a scatter plot of strength and weight × height to obtain an index of strength independent of BMI and body-size.33-36 The potential relationships between baseline quadriceps strength, H:Q ratio, and knee joint space narrowing worsening were assessed using a logistic regression model after adjusting for age, BMI, lower limb alignment (≤2° varus, neutral, ≥2° valgus), history of knee injury and/or surgery, and physical activity level (PASE) at baseline. Generalized estimating equations were used in all models to adjust for correlations between knees and visits within each subject. Analyses were performed using SAS software version 9.1 (SAS Institute Inc., Cary, NC) and alpha level for significance set at < .05.
RESULTS
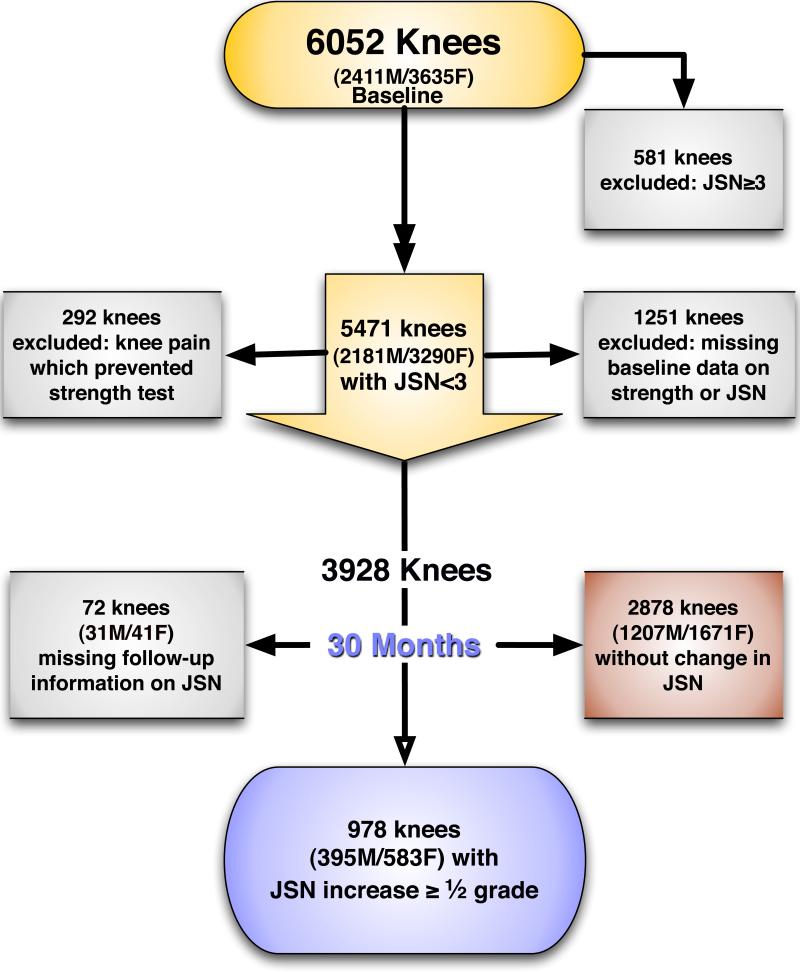
A total of 6052 knees were considered for inclusion (Figure 1). Of these, 3856 knees with complete 30-month follow-up data and a JSN score <3 at baseline were eligible for this study. Excluded from the study were 72 knees due to missing 30-month follow-up joint space narrowing data, 292 knees due to self-report of pain that interfered with strength measurement at baseline, 1251 knees with missing data at baseline, and 581 knees with a JSN score of 3 at baseline. Subjects’ baseline characteristics are presented in Table 1. Men were more active (PASE=209.1 ± 98.3), and had greater mean ± SD quadriceps (125.7 ± 41.4 N•m) and hamstrings strength (80.6±28.1 N•m) than women (PASE score=162.1 ± 77.8, quadriceps strength=72.0 ± 24.0 N•m, hamstrings strength=47.1±15.4 N•m, all p<.0001). Men and women were similar in age (61.6±8.1 vs. 62.2±7.7) and BMI (30.3±4.9 vs. 30.3±6.0 kg/m2, all p>0.05). Approximately 34.3% of male knees and 31.4% of female knees had a H:Q ratio <0.6.
Figure 1.
Participant Inclusion
Table 1.
Baseline characteristics in men and women* (N=2182 subjects, 3856 knees.)
| Age (years) | BMI (Kg/m2) | Quadriceps Strength (N•m) | Hamstring Strength (N•m) | % H:Q Ratio <0.6 | PASE score | Knee malalignment (% varus) | History of knee injury/surgery (%) | |
|---|---|---|---|---|---|---|---|---|
| Men 892 participants, 1602 knees | 61.6± 8.1 | 30.3 ± 4.9 | 125.7 ± 41.4 | 80.6±28.1 | 34.3 % | 209.1 ± 98.3 | 58.1% | 12.4% |
| Women 1290 participants, 2254 knees | 62.2 ± 7.7 | 30.3 ± 6.0 | 72.0 ± 24.0 | 47.1±15.4 | 31.4 % | 162.1 ± 77.8 | 38.8% | 7.0% |
Mean±SD or frequencies
Knee joint space narrowing
Whole knee
At 30 months, 395 (24.7%) of 1602 knees in men and 583 (25.9%) of 2254 knees in women had whole knee joint space narrowing. Baseline characteristics of participants who were found to have JSN progression and those without evidence of JSN progression are presented in Table 2. Women, but not men, in the lowest tertiles of quadriceps strength were at increased risk for knee joint space narrowing compared with those in the highest tertiles (Table 3). Similar results were obtained when treating peak quadriceps strength as a continuous variable (p=0.7400 in men and p<0.0001 in women). Men and women with a H:Q ratio <0.6 did not have an increased risk of whole knee joint space narrowing compared with those who had a H:Q ratio ≥0.6 (Table 4) and this remained unchanged when 0.8 was used as the cutoff. Results of all analyses also remained unchanged after adjusting for age, BMI, activity level, and malalignment.
Table 2.
Baseline characteristics of participants with and without worsening of joint space narrowing (JSN)*
| % female | Age (years) | BMI (Kg/m2) | Quadriceps Strength (N•m) | Hamstring Strength (N•m) | % H:Q Ratio <0.6 | PASE score | Knee malalignment (% varus) | History of knee injury/surgery (%) | |
|---|---|---|---|---|---|---|---|---|---|
| JSN worsening (576 participants, 978 knees) | 61.6% | 63.6 ± 7.9 | 31.9 ± 5.9 | 89.2 ± 41.4 | 58.6±27.5 | 31.3% | 176.3 ± 89.0 | 58.2% | 16.0% |
| No worsening (1606 participants, 2878 knees) | 58.2% | 61.3 ± 7.8 | 29.7 ± 5.3 | 96.1 ± 41.8 | 61.8±27.1 | 33.0% | 183.1 ± 90.0 | 43.0% | 7.0% |
| p-value | 0.0654 | <0.0001 | <0.0001 | <0.0001 | <0.0015 | 0.3220 | 0.0530 | <0.0001 | <0.0001 |
Mean±SD or frequencies
Table 3.
Association between peak quadriceps strength and whole knee joint space narrowing
| Sex-specific tertiles of KES | N of cases (%) | OR (95% CI) for worsening, adjusted for baseline age, BMI, malalignment, surgery and PASE | |
|---|---|---|---|
| Men | Highest, 142~270 N•m (n=541) | 126 (23.3) | 1.0 |
| Middle, 108~141 N•m (n=524) | 127(24.2) | 0.99 (0.73, 1.34) | |
| Lowest, 22~107 N•m (n=537) | 142 (26.4) | 1.08 (0.77, 1. 51) | |
| P for linear trend | 0.7410 | ||
| Women | Highest, 82~206 N•m (n=756) | 146 (19.3) | 1.0 |
| Middle 61~80N•m (n=739) | 181 (24.5) | 1.19 (0.90, 1.55) | |
| Lowest, 20~60 N•m (n=759) | 256 (33.7) | 1.66 (1.26, 2.19) | |
| P for linear trend | <0.0001 | ||
• using generalized estimating equations to adjust for correlations between knees within subjects
Table 4.
Association between hamstring:quadriceps ratio and whole knee joint space narrowing
| Sex-specific cut-offs | N of cases (%) | OR (95% CI), adjusted for baseline age, BMI, malalignment, surgery and PASE | |
|---|---|---|---|
| Men | ≥0.6 (1052) | 257 (24.4) | 1.0 |
| <0.6 (550) | 138 (25.1) | 1.00 (0.78, 1.28) | |
| Women | ≥0.6 (1547) | 415 (26.8) | 1.0 |
| <0.6 (707) | 168 (23.8) | 0.94 (0.77, 1.15) |
• using generalized estimating equations to adjust for correlations between knees within subjects
Tibiofemoral joint
Tibiofemoral joint space narrowing was found in 359 (22.4%) of 1602 male knees and 503 (22.3%) of 2254 female knees. Male knees in the lowest compared with the highest tertile of quadriceps strength did not differ in risk for tibiofemoral joint space narrowing with OR (95% CI ) of 1.20 (0.85, 1.70). In contrast, female knees in the lowest tertile of quadriceps strength were at increased risk compared with the highest tertile with OR of 1.69 (1.26, 2.28). Muscle imbalance at a cutoff of <0.6 did not alter risk for tibiofemoral joint space narrowing in men, OR=1.06 (0.82, 1.37) or women, OR=1.02 (0.82, 1.26). In addition, no significant effect was present when <0.8 was used as the cutoff. Adjusting for age, BMI, activity level, and malalignment yielded similar results.
Patellofemoral joint
Patellofemoral joint space narrowing was found in 46 (2.9%) of 1602 male knees and 114 (5.1%) of 2254 female knees. Men and women in the lowest tertiles of quadriceps strength were not at increased risk for patellofemoral joint space narrowing compared with those in the highest tertiles, OR=0.67 (0.30, 1.48) in men and OR=1.53 (0.90, 2.62) in women respectively, although women in the middle compared with the highest tertile were at increased risk for patellofemoral joint space narrowing, OR=1.64 (1.03, 2.62). In addition, neither men nor women with a H:Q ratio <0.6 had an increased risk of patellofemoral joint narrowing compared with those who had a H:Q ratio ≥0.6, OR=0.79 (0.38, 1.62) and OR=0.66 (0.44, 1.01) respectively. When 0.8 was used as the cutoff, men but not women with an H:Q ratio <0.8 were protected against JSN worsening with OR=0.48 (0.24, 0.93). Results of all analyses remained unchanged after adjusting for age, BMI, activity level and malalignment.
DISCUSSION
The results of this study revealed that women in the lowest tertile of quadriceps strength were at elevated risk of whole knee and tibiofemoral joint space narrowing over 30 months compared with those in the highest tertile. However, in men, no associations were found between quadriceps strength or H:Q ratio and knee joint space narrowing. To our knowledge, this is the largest study to evaluate these relationships in both women and men.
The positive findings in women but not men are in concordance with previous findings for incident symptomatic knee OA from the MOST study.37 In that study women to a greater extent than men with low quadriceps strength were found to be at increased risk for incident symptomatic whole knee OA. However, low quadriceps strength was not identified as a risk factor for incident radiographic knee OA in either women or men. In men, the current study findings are also consistent with the lack of a significant change in joint space narrowing or grade following strength training, in comparison with a control program in subjects with pre-existing knee OA.20 Similarly, a review of observational studies of risk factors for progression of knee OA found no evidence to support a significant association with quadriceps weakness.38 One potential explanation for the association between quadriceps weakness and incident symptomatic as well as progressive worsening knee OA in women, but not in men, may relate to strength capacity being closer to a threshold for risk.39, 40 For example, men have higher strength and this may provide greater reserve, so that even with some loss of strength, the degree of weakness may be insufficient to result in risk for these outcomes. In contrast, women have less strength (57% that of men in this study despite no significant difference in BMI), so weakness may result in sufficient cause for knee joint damage.
Our findings differ from those of Brandt, et al18 and Thorstensson, et al41 who found no significant differences in mean quadriceps strength between women with and without tibiofemoral OA worsening. It is possible that the lack of agreement between those and the present study may have been due to different methods for measuring knee OA progression. In the present study, progression was defined as an increase in joint space narrowing in participants having a JSN score <3 at baseline. In the prior studies, progression was based on increasing KL grade. The development of KL grade 2 is characterized by osteophyte formation while progression from KL grade 2 is mainly characterized by joint space narrowing and it is plausible that these may result from different mechanisms. In addition, the study by Thorstensson, et al used more functional measures of strength than the present study (single-leg rise/stance and 300 m walk time). Differences in results also may exist due to larger sample sizes and a greater number of subjects with progression in the present study.
We found a significant trend for a relationship between patellofemoral joint space narrowing and quadriceps strength in women (p=.0400) but not in men (p=0.7106). This result in women is consistent with a recent study that found greater quadriceps strength protective against cartilage loss on the lateral patellofemoral facet.21 In addition, cross-sectional data from a study evaluating the relationship between quadriceps weakness and prevalent tibiofemoral, patellofemoral, and mixed OA (presence of both patellofemoral and tibiofemoral OA) also showed a relationship between lateral patellofemoral OA and quadriceps strength, though this relationship lost significance after analyses were adjusted for knee pain.42 These authors suggested that quadriceps strength may prevent excessive lateral movement of the patella during knee flexion, which in the presence of weakness could lead to disproportionate compressive forces across the lateral patellofemoral joint.
In contrast, we did not find that a H:Q ratio of either <0.6 or <0.8, indicating greater quadriceps relative to hamstrings strength, protected against joint space narrowing. This result suggests that overall quadriceps strength may be more important than the balance of knee flexor to extensor strength for preventing knee joint space narrowing. As mentioned previously, a concentric:concentric H:Q ratio cutoff of 0.6 was prospectively selected, as this has been reported to be normal in studies of younger subjects.30, 43, 44 Recognizing that this cutoff may not be appropriate for older adults, we conducted secondary analyses using 0.8 as a cutoff and did not find a strong effect at this cutoff either.
We are not aware of normative H:Q radio data for adults age 50-79 years. However, based on the reported more rapid decline in isokinetic hamstring strength in comparison with quadriceps strength with aging,45 we might expect the H:Q ratio to slightly decrease in older adults. Extrapolating from that report of mean strength data for adults in the same age range as MOST participants, using similar methods, suggests H:Q ratios in men and women of 0.55 and 0.58, which declined to 0.52 and 0.57 respectively over 10 year follow-up. The HealthABC study also reported grouped mean±SD isokinetic hamstring and quadriceps strength data for high functioning eighth decade adults.46 In that study, the ratio between these was 0.74 for men and 0.79 for women. However, since H:Q ratio data were not presented, it is not possible to determine the H:Q ratio for individuals or whether those data would represent normative data for older adults in other decades or who were not selected for high mobility function. In the absence of normative H:Q ratio data for older adults, we assessed whether there was any cutoff or range of values that appeared to be associated with more severe knee OA or JSN outcome. As seen in Table 5, there did not appear to be any relationship between the median or interquartile range of H:Q ratio and a) sex, b) decade, c) knee OA (KL) grade, or d) JSN outcome. Although it was not feasible to assess peak eccentric strength in older adults with knee OA, an Hecc:Qcon ratio may be a more functional means of assessing muscle balance.30, 44
Table 5.
H:Q Ratio median (IQR) by sex, decade, KL grade and outcome
| Sex | Decade (N) | H:Q ratio Median (IQR) | ||
|---|---|---|---|---|
| Women | 50's (916) | 0.65 (0.57, 0.75) | 0.67 (0.57, 0.75) | 0.66 (0.57, 0.75) |
| 60's (908) | 0.67 (0.57, 0.75) | |||
| 70's (430) | 0.67 (0.56, 0.78) | |||
| Men | 50's (676) | 0.65 (0.57, 0.73) | 0.64 (0.56, 0.73) | |
| 60's (628) | 0.64 (0.56, 0.73) | |||
| 70's (298) | 0.64 (0.53, 0.76) | |||
| Baseline KL Grade | Median (IQR) | |||
| 0 | 0.65 (0.74, 0.56) | |||
| 1 | 0.67 (0.75, 0.58) | |||
| 2 | 0.66 (0.76, 0.58) | |||
| 3 | 0.67 (0.77, 0.57) | |||
| Outcome | Median (IQR) | |||
| No JSN Worsening | 0.65 (0.74, 0.57) | |||
| JSN Worsening | 0.67 (0.77, 0.57) | |||
Results from the present and the aforementioned study of the MOST cohort indicate that quadriceps weakness is a risk factor for progressive and incident symptomatic but not incident radiographic knee OA for women in this cohort.47 Though a mechanism that could explain this finding was not the focus of this study, knee OA risk factors previously have been acknowledged to differ between women and men due to biochemical and biomechanical differences that, in this case, could also result in differences in risk for knee OA progression (hormonal and anthropometric factors and/or ligamentous laxity). One potential limitation was the inability to correct for gravity during the isokinetic testing, which could have reduced the raw quadriceps strength data for participants with heavier calves. However, the inter-participant differences in calf mass were found to be small and would be unlikely to alter the tertile of strength to which participants were assigned.
Several aspects of our longitudinal study design strengthen our findings. First, the MOST cohort is made up of individuals with radiographically-documented knee osteoarthritis or known risk factors for knee osteoarthritis such as elevated BMI or history of knee surgery or injury. Therefore, if quadriceps weakness plays a significant role in the pathogenesis of knee OA, it is likely to be detected in this cohort. In support of this, we found men and women with KL grade ≥ 2 in MOST had lower quadriceps strength cross-sectionally than those without radiographic knee OA (KES=123.8 vs. 131.3 N•m in men and KES=69.3 vs. 75.6 N•m in women). Additionally, rates of knee joint space narrowing in the study population were similar to or higher than those reported for progression in other studies with similar inclusion criteria. Thus, there was a sufficient amount of time for worsening to occur in an adequate number of study participants, suggesting that our findings may be generalizable.
Knee OA is one of the leading causes of disability in the United States 48 and identification of modifiable risk factors is a significant public health concern. Though this study identified quadriceps weakness as a risk factor for knee joint worsening in women only, lower limb function in older men and women is highly dependent on quadriceps muscle strength.49, 50 Quadriceps strength is known to decline with age.51 Muscle atrophy from inactivity or knee pain may further contribute to this decline in older adults with knee OA. Therefore, quadriceps strength is functionally significant in men despite the lack of association with joint space narrowing and may have a dual importance in women to prevent worsening knee OA as well as minimize physical functional limitations. Therefore, we would not interpret the results as an indication that only women with weakness should participate in lower limb strengthening activity, but rather that in addition to the known benefits on minimizing impairments, functional limitations and disability in men and women, women may attain an additional protection against worsening of joint space narrowing through maintaining higher quadriceps strength. Longitudinal studies are necessary in order to better understand whether strengthening of weak quadriceps muscles is protective.
Conclusion
In women but not in men, quadriceps weakness appears to increase risk of joint space narrowing over 30 months in the MOST study. This is the largest longitudinal study evaluating this relationship to date and provided adequate power for investigating a relationship between quadriceps muscle weakness and worsening of knee joint space narrowing. Future studies should evaluate other means of measuring anatomic and symptomatic worsening, such as cartilage thickness, symptoms or functional limitations as well as assessing whether strengthening of lower limb muscles can protect against knee OA worsening.
Acknowledgments
The authors thank the participants and staff of the Multicenter Osteoarthritis (MOST) Study.
Disclosures: This study was supported by NIH grants to: Boston University (David Felson, MD - AG18820);University of Iowa (James Torner, PhD - AG18832); University of Alabama (Cora E. Lewis, MD MSPH - AG18947); University of California San Francisco (Michael Nevitt, PhD - AG19069); and a Beeson Career Development Award (Neil Segal, MD – K23AG030945). The authors have no professional relationships with companies or manufacturers who will benefit from the results of the present study. An abstract of this data was presented at the 2008 annual meeting of the American College of Rheumatology.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
The authors report no conflicts of interest.
References
- 1.Slemenda C, Heilman DK, Brandt KD, Katz BP, Mazzuca SA, Braunstein EM, et al. Reduced quadriceps strength relative to body weight: a risk factor for knee osteoarthritis in women? Arthritis Rheum. 1998;41:1951–9. doi: 10.1002/1529-0131(199811)41:11<1951::AID-ART9>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 2.Hootman JM, FitzGerald S, Macera CA, Blair SN. Lower extremity muscle strength and risk of self-reported hip/knee osteoarthritis. Journal of Physical Activity and Health. 2004;4:321–30. [Google Scholar]
- 3.Segal NA, Torner JC, Felson D, Niu J, Sharma L, Lewis CE, et al. Effect of Thigh Strength on Incident Radiographic and Symptomatic Knee Osteoarthritis in a Longitudinal Cohort. Arthritis Care Res. 2009:61. doi: 10.1002/art.24541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cooper C, Snow S, McAlindon TE, Kellingray S, Stuart B, Coggon D, et al. Risk factors for the incidence and progression of radiographic knee osteoarthritis. Arthritis Rheum. 2000;43:995–1000. doi: 10.1002/1529-0131(200005)43:5<995::AID-ANR6>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 5.McAlindon TE, Felson DT, Zhang Y, Hannan MT, Aliabadi P, Weissman B, et al. Relation of dietary intake and serum levels of vitamin D to progression of osteoarthritis of the knee among participants in the Framingham Study. Ann Intern Med. 1996;125:353–9. doi: 10.7326/0003-4819-125-5-199609010-00001. [DOI] [PubMed] [Google Scholar]
- 6.Zhang Y, Hannan MT, Chaisson CE, McAlindon TE, Evans SR, Aliabadi P, et al. Bone E320 mineral density and risk of incident and progressive radiographic knee osteoarthritis in women: the Framingham Study. J Rheumatol. 2000;27:1032–7. [PubMed] [Google Scholar]
- 7.Felson DT, Goggins J, Niu J, Zhang Y, Hunter DJ. The effect of body weight on progression of knee osteoarthritis is dependent on alignment. Arthritis Rheum. 2004;50:3904–9. doi: 10.1002/art.20726. [DOI] [PubMed] [Google Scholar]
- 8.Hurley MV. The role of muscle weakness in the pathogenesis of osteoarthritis. Rheum Dis Clin North Am. 1999;25:283–98. vi. doi: 10.1016/s0889-857x(05)70068-5. [DOI] [PubMed] [Google Scholar]
- 9.Sharma L, Pai YC, Holtkamp K, Rymer WZ. Is knee joint proprioception worse in the arthritic knee versus the unaffected knee in unilateral knee osteoarthritis? Arthritis Rheum. 1997;40:1518–25. doi: 10.1002/art.1780400821. [DOI] [PubMed] [Google Scholar]
- 10.Slemenda C, Brandt KD, Heilman DK, Mazzuca S, Braunstein EM, Katz BP, et al. Quadriceps weakness and osteoarthritis of the knee. Ann Intern Med. 1997;127:97–104. doi: 10.7326/0003-4819-127-2-199707150-00001. [DOI] [PubMed] [Google Scholar]
- 11.Hall MC, Mockett SP, Doherty M. Relative impact of radiographic osteoarthritis and pain on quadriceps strength, proprioception, static postural sway and lower limb function. Ann Rheum Dis. 2006;65:865–70. doi: 10.1136/ard.2005.043653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fisher NM, Pendergast DR. Reduced muscle function in patients with osteoarthritis. Scand J Rehabil Med. 1997;29:213–21. [PubMed] [Google Scholar]
- 13.Cicuttini FM, Teichtahl AJ, Wluka AE, Davis S, Strauss BJ, Ebeling PR. The relationship between body composition and knee cartilage volume in healthy, middle-aged subjects. Arthritis Rheum. 2005;52:461–7. doi: 10.1002/art.20791. [DOI] [PubMed] [Google Scholar]
- 14.Foley S, Ding C, Cicuttini F, Jones G. Physical activity and knee structural change: a longitudinal study using MRI. Med Sci Sports Exerc. 2007;39:426–34. doi: 10.1249/mss.0b013e31802d97c6. [DOI] [PubMed] [Google Scholar]
- 15.Baker K, McAlindon T. Exercise for knee osteoarthritis. Curr Opin Rheumatol. 2000;12:465–63. doi: 10.1097/00002281-200009000-00020. [DOI] [PubMed] [Google Scholar]
- 16.Radin EL, Burr DB, Caterson B, Fyhrie D, Brown TD, Boyd RD. Mechanical determinants of osteoarthrosis. Semin Arthritis Rheum. 1991;21:12–21. doi: 10.1016/0049-0172(91)90036-y. [DOI] [PubMed] [Google Scholar]
- 17.Jefferson RJ, Collins JJ, Whittle MW, Radin EL, O'Connor JJ. The role of the quadriceps in controlling impulsive forces around heel strike. Proc Inst Mech Eng [H] 1990;204:21–8. doi: 10.1243/PIME_PROC_1990_204_224_02. [DOI] [PubMed] [Google Scholar]
- 18.Brandt KD, Heilman DK, Slemenda C, Katz BP, Mazzuca SA, Braunstein EM, et al. Quadriceps strength in women with radiographically progressive osteoarthritis of the knee and those with stable radiographic changes. J Rheumatol. 1999;26:2431–7. [PubMed] [Google Scholar]
- 19.Sharma L, Dunlop DD, Cahue S, Song J, Hayes KW. Quadriceps strength and osteoarthritis progression in malaligned and lax knees. Ann Intern Med. 2003;138:613–9. doi: 10.7326/0003-4819-138-8-200304150-00006. [DOI] [PubMed] [Google Scholar]
- 20.Mikesky AE, Mazzuca SA, Brandt KD, Perkins SM, Damush T, Lane KA. Effects of strength training on the incidence and progression of knee osteoarthritis. Arthritis Rheum. 2006;55:690–9. doi: 10.1002/art.22245. [DOI] [PubMed] [Google Scholar]
- 21.Amin S, Baker K, Niu J, Clancy M, Goggins J, Guermazi A, et al. Quadriceps strength and the risk of cartilage loss and symptom progression in knee osteoarthritis. Arthritis and rheumatism. 2009;60:189–98. doi: 10.1002/art.24182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Segal NA, Torner J, Felson D, Nevitt M. Knee extensor weakness is more strongly related to reduced muscle mass than to reduced activity levels or bone mineral density in adults over age 50. Arthritis and Rheumatism. 2005;52:S300–S00. [Google Scholar]
- 23.Altman RD, Hochberg M, Murphy WA, Jr., Wolfe F, Lequesne M. Atlas of individual radiographic features in osteoarthritis. Osteoarthritis Cartilage. 1995;3(Suppl A):3–70. [PubMed] [Google Scholar]
- 24.Segal NA, Felson DT, Torner JC, Zhu Y, Curtis JR, Niu J, et al. Greater trochanteric pain syndrome: epidemiology and associated factors. Archives of Physical Medicine and Rehabilitation. 2007;88:988–92. doi: 10.1016/j.apmr.2007.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dinger MK, Oman RF, Taylor EL, Vesely SK, Able J. Stability and convergent validity of the Physical Activity Scale for the Elderly (PASE). J Sports Med Phys Fitness. 2004;44:186–92. [PubMed] [Google Scholar]
- 26.Martin KA, Rejeski WJ, Miller ME, James MK, Ettinger WH, Jr., Messier SP. Validation of the PASE in older adults with knee pain and physical disability. Med Sci Sports Exerc. 1999;31:627–33. doi: 10.1097/00005768-199905000-00001. [DOI] [PubMed] [Google Scholar]
- 27.Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): development and evaluation. Journal of Clinical Epidemiology. 1993;46:153–62. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- 28.Segal NA, Torner JC, Felson DT, Niu J, Sharma L, Lewis CE, et al. Knee Extensor Strength does not Protect Against Incident Knee Symptoms at 30 Months in the Multicenter Knee Osteoarthritis (MOST) Cohort. PM&R. 2009;1:459–65. doi: 10.1016/j.pmrj.2009.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Read MT, Bellamy MJ. Comparison of hamstring/quadriceps isokinetic strength ratios and power in tennis, squash and track athletes. Br J Sports Med. 1990;24:178–82. doi: 10.1136/bjsm.24.3.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aagaard P, Simonsen EB, Magnusson SP, Larsson B, Dyhre-Poulsen P. A new concept for isokinetic hamstring: quadriceps muscle strength ratio. Am J Sports Med. 1998;26:231–7. doi: 10.1177/03635465980260021201. [DOI] [PubMed] [Google Scholar]
- 31.Aagaard P, Simonsen EB, Trolle M, Bangsbo J, Klausen K. Isokinetic E386 hamstring/quadriceps strength ratio: influence from joint angular velocity, gravity correction and contraction mode. Acta Physiol Scand. 1995;154:421–7. doi: 10.1111/j.1748-1716.1995.tb09927.x. [DOI] [PubMed] [Google Scholar]
- 32.Felson DT, Nevitt MC, Yang M, Clancy M, Niu J, Torner JC, et al. A new approach yields high rates of radiographic progression in knee osteoarthritis. The Journal of rheumatology. 2008;35:2047–54. [PMC free article] [PubMed] [Google Scholar]
- 33.Jaric S. Muscle strength testing: use of normalisation for body size. Sports Med. 2002;32:615–31. doi: 10.2165/00007256-200232100-00002. [DOI] [PubMed] [Google Scholar]
- 34.Jaric S, Radosavljevic-Jaric S, Johansson H. Muscle force and muscle torque in humans require different methods when adjusting for differences in body size. Eur J Appl Physiol. 2002;87:304–7. doi: 10.1007/s00421-002-0638-9. [DOI] [PubMed] [Google Scholar]
- 35.Tanner JM. Fallacy of per-weight and per-surface area standards, and their relation to spurious correlation. J Appl Physiol. 1949;2:1–15. doi: 10.1152/jappl.1949.2.1.1. [DOI] [PubMed] [Google Scholar]
- 36.Nevill AM, Holder RL. Scaling, normalizing, and per ratio standards: an allometric modeling approach. J Appl Physiol. 1995;79:1027–31. doi: 10.1152/jappl.1995.79.3.1027. [DOI] [PubMed] [Google Scholar]
- 37.Segal NA, Torner JC, Felson D, Niu J, Sharma L, Lewis CE, et al. Effect of thigh strength on incident radiographic and symptomatic knee osteoarthritis in a longitudinal cohort. Arthritis and rheumatism. 2009;61:1210–7. doi: 10.1002/art.24541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Belo JN, Berger MY, Reijman M, Koes BW, Bierma-Zeinstra SM. Prognostic factors of progression of osteoarthritis of the knee: a systematic review of observational studies. Arthritis Rheum. 2007;57:13–26. doi: 10.1002/art.22475. [DOI] [PubMed] [Google Scholar]
- 39.Ploutz-Snyder LL, Manini T, Ploutz-Snyder RJ, Wolf DA. Functionally relevant thresholds of quadriceps femoris strength. J Gerontol A Biol Sci Med Sci. 2002;57:B144–52. doi: 10.1093/gerona/57.4.b144. [DOI] [PubMed] [Google Scholar]
- 40.Buchner D, de Lateur BJ. The importance of skeletal muscle strength to physical function in older adults. Annals of Behavioral Medicine. 1991;13:91–98. [Google Scholar]
- 41.Thorstensson CA, Petersson IF, Jacobsson LT, Boegard TL, Roos EM. Reduced functional performance in the lower extremity predicted radiographic knee osteoarthritis five years later. Ann Rheum Dis. 2004;63:402–7. doi: 10.1136/ard.2003.007583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Baker KR, Xu L, Zhang Y, Nevitt M, Niu J, Aliabadi P, et al. Quadriceps weakness and its relationship to tibiofemoral and patellofemoral knee osteoarthritis in Chinese: the Beijing osteoarthritis study. Arthritis & Rheumatism. 2004;50:1815–21. doi: 10.1002/art.20261. [DOI] [PubMed] [Google Scholar]
- 43.Rosene JM, Fogarty TD, Mahaffey BL. Isokinetic Hamstrings:Quadriceps Ratios in Intercollegiate Athletes. J Athl Train. 2001;36:378–83. [PMC free article] [PubMed] [Google Scholar]
- 44.Coombs R, Garbutt G. Developments in the use of the hamstring/quadriceps ratio for the assessment of muscle balance. Journal of Sports Science & Medicine. 2002;1:56–62. [PMC free article] [PubMed] [Google Scholar]
- 45.Hughes VA, Frontera WR, Wood M, Evans WJ, Dallal GE, Roubenoff R, et al. Longitudinal muscle strength changes in older adults: influence of muscle mass, physical activity, and health. J Gerontol A Biol Sci Med Sci. 2001;56:B209–17. doi: 10.1093/gerona/56.5.b209. [DOI] [PubMed] [Google Scholar]
- 46.Katsiaras A, Newman AB, Kriska A, Brach J, Krishnaswami S, Feingold E, et al. Skeletal muscle fatigue, strength, and quality in the elderly: the Health ABC Study. Journal of applied physiology (Bethesda, Md. 2005;99:210–6. doi: 10.1152/japplphysiol.01276.2004. [DOI] [PubMed] [Google Scholar]
- 47.Nevitt MC, Zhang Y, Javaid MK, Neogi T, Curtis JR, Niu J, et al. High systemic bone mineral density increases the risk of incident knee OA and joint space narrowing, but not radiographic progression of existing knee OA: The MOST study. Annals of the rheumatic diseases. 2009 doi: 10.1136/ard.2008.099531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Guccione AA, Felson DT, Anderson JJ, Anthony JM, Zhang Y, Wilson PW, et al. The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. American Journal of Public Health. 1994;84:351–8. doi: 10.2105/ajph.84.3.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Visser M, Kritchevsky SB, Goodpaster BH, Newman AB, Nevitt M, Stamm E, et al. Leg muscle mass and composition in relation to lower extremity performance in men and women aged 70 to 79: the health, aging and body composition study. J Am Geriatr Soc. 2002;50:897–904. doi: 10.1046/j.1532-5415.2002.50217.x. [DOI] [PubMed] [Google Scholar]
- 50.Visser M, Goodpaster BH, Kritchevsky SB, Newman AB, Nevitt M, Rubin SM, et al. Muscle mass, muscle strength, and muscle fat infiltration as predictors of incident mobility limitations in well-functioning older persons. J Gerontol A Biol Sci Med Sci. 2005;60:324–33. doi: 10.1093/gerona/60.3.324. [DOI] [PubMed] [Google Scholar]
- 51.Schiller BC, Casas YG, Tracy BL, DeSouza CA, Seals DR. Age-related declines in knee extensor strength and physical performance in healthy Hispanic and Caucasian women. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2000;55:B563–9. doi: 10.1093/gerona/55.12.b563. [DOI] [PubMed] [Google Scholar]