The adult population in the United States 65 years and older increased to 35 million in 2000 and is projected to be 71 million by 2030 (Administration on Aging, 2007). The aging of the U.S. population is a major health challenge as older adults are likely to live alone, suffer from chronic illness, spend more years and a greater percentage of their lifetime disabled, and live in poverty, and are at risk for losing their independence as their health declines (Administration on Aging, 2007).
Older adults with declining health related to chronic conditions often have multiple unmet needs (Wolff, Starfield, & Anderson, 2002). Studies suggest that older adults prefer to stay in their homes--aging in place--for as long as possible, but are often unaware of resources in their community to help them remain in their home (Eckert, Morgan, & Swamy, 2004). In addition, it is often difficult for older adults to manage their health, including accessing the kind and level of health care needed (Shearer, 2004, 2007; Shearer & Fleury, 2006; Shearer, Fleury, & Reed, 2009). Awareness of personal and social contextual resources appears to play an important role in promoting well-being in older adults who experience chronic illness (Boland, 2000; Shearer, 2007, 2008). However, as older adults age, their health needs become more complex, and recognition of personal resources and social contextual resources as a basis for purposeful participation in the attainment of health goals may be limited (Shearer, 2009). Access to resources may be particularly important among older adults, representing a critical area for intervention. The challenge for health care providers, however, is to facilitate awareness of and access to personal resources and social contextual resources effectively.
Empowerment has been conceptualized as a framework for understanding the process and consequences of efforts to exert control and influence over the decisions that affect one’s life, including perceptions of personal control and behaviors to realize control (Perkins & Zimmerman, 1995; Rappaport, 1984). The empowerment process has been focused on relationships with others as well as on “liberation, emancipation, energy and sharing power” (Leyshon, 2002, p. 467). There is much recent discussion regarding the increasing numbers of older adults and the need to explore efforts consistent with empowerment to promote health and well-being among the aged (Keller & Fleury, 2000). Itzhaky and Schwartz (1998) suggest that an empowerment approach may nurture well-being in vulnerable individuals such as homebound older adults. Given the basic assumptions in nursing regarding the importance of human potential and development, connectedness, and the social context of health, facilitating health empowerment (Shearer & Reed, 2004) may provide nurses with new insights for research and practice.
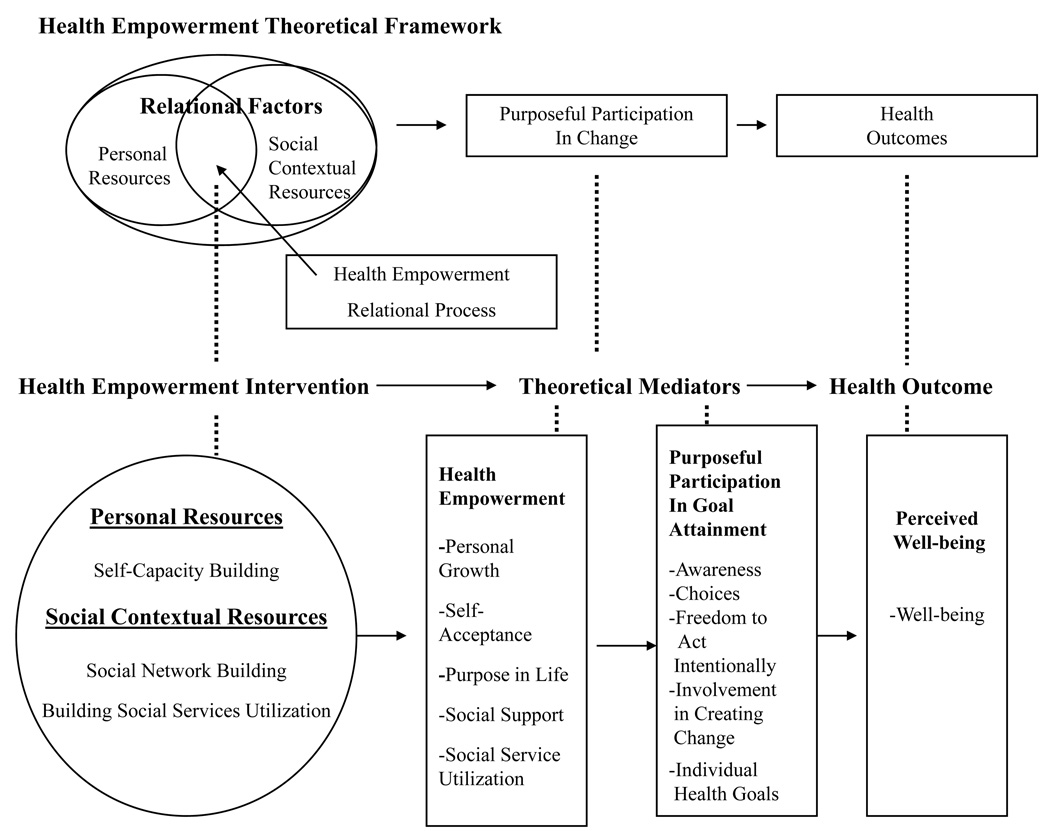
The Health Empowerment Intervention (HEI) is a theory-based program designed to promote the use of personal resources and social contextual resources with the goal of enhancing well-being in homebound older adults (Shearer, 2009). Building upon the middle-range health empowerment theory (Shearer, 2004, 2007; Shearer & Reed, 2004), health empowerment is expressive of a human health pattern of well-being and is viewed as a relational process that emerges from the recognition of personal resources and social contextual resources. This process facilitates purposeful participation in the attainment of health goals and the promotion of individual well-being (Shearer, 2009).
The aim of this study was to evaluate the feasibility of the HEI and to explore the impact of the HEI on the theoretical mediating variables of health empowerment and purposeful participation in goal attainment and the outcome variable of well-being with homebound older adults. The study was designed to compare an intervention group receiving the HEI intervention with an attentional comparison group receiving a newsletter focused on health and safety issues relevant to older adults. It was hypothesized that older adults receiving the HEI would have significantly improved health empowerment, purposeful participation in goal attainment, and well-being compared with those in the attentional comparison group.
Methods
Participants
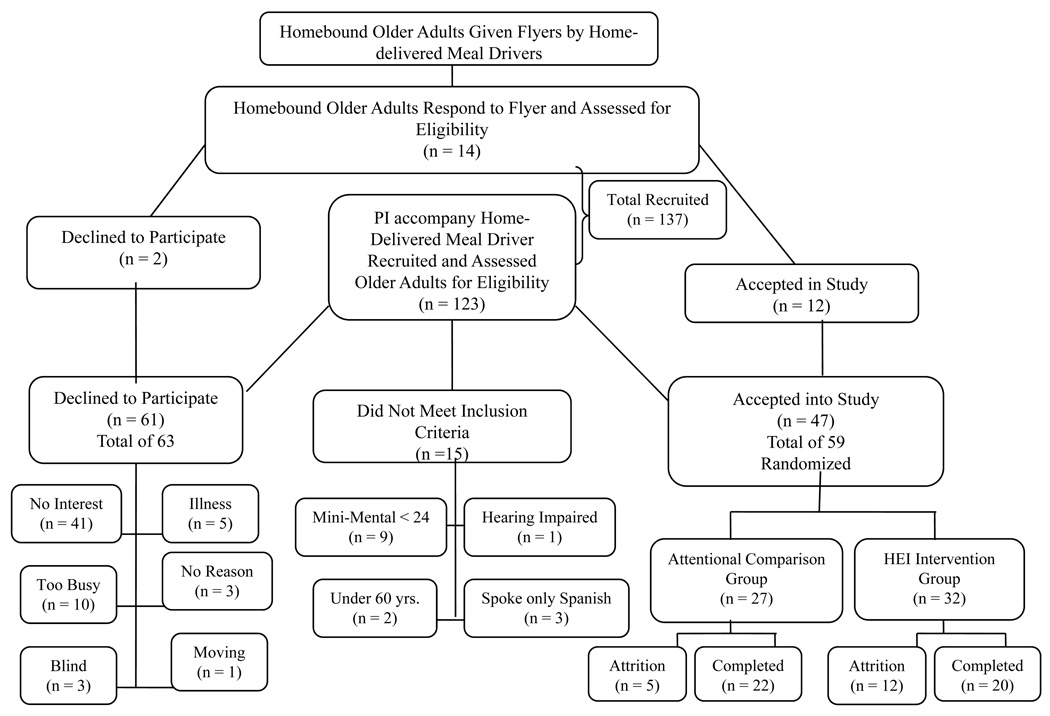
Eligible participants: (a) were aged 60 years and above; (b) received home-delivered meals through the local Community Action Agency; (c) were able to speak and understand English; (d) were able to hear; and (e) had the cognitive capacity to respond accurately to questionnaires and to give informed consent to participate in the HEI. Cognitive capacity was determined as evaluated by the Mini-Mental State Examination (MMSE; Folstein, Folstein, & McHugh, 1975). A total of 137 homebound older adults were screened for study participation, which yielded 59 consenting participants (Figure 1). A priori power analysis was performed as part of the design of the experiment to estimate the required total sample size of 42 as a function of power (.80) with a large effect size (µ1–µ2/σ = 1.0) and α = .05.
Figure 1.
Recruitment Flow Chart
After receiving study approval from the university institutional review board, participants were recruited through the meal delivery program affiliated with a Community Action Agency located in a southwestern metropolitan area of the US. The principal investigator (PI) and research team presented the study to the home-delivered meal program staff associated with the Community Action Agency. A flyer describing the study was distributed to potential participants by the home-delivered meal drivers and through face-to-face contact with the study team when team members accompanied the drivers on their delivery route (Shearer, Fleury, & Belyea, in press). The older adults interested in participating in the study were screened for eligibility by the PI. After providing written informed consent, eligible participants were assigned randomly to either the HEI or an attentional comparison group. Random assignment to the intervention group or attentional comparison group was accomplished using SAS software.
The HEI and measurement visits took place in the home of the participant. The three measurement visits for the intervention group and attentional comparison group and six intervention sessions were scheduled at a time convenient for each participant. Participants were contacted by mail and telephone prior to each scheduled visit. If participants were not available to meet at a scheduled time, the visit was rescheduled as convenient for the participant. Participants were measured at baseline (Time 1), following the 6-week protocol (Time 2), and at 12 weeks (Time 3). The people conducting the measures were blinded to the group assignment.
Intervention
The HEI consisted of weekly (approximately 60 minutes in length) visits for 6 consecutive weeks delivered in the home of the participant by the trained nurse intervener (NI). Each session followed a standardized format. Theory-based content and goals for each session were provided in a written manual; intervention fidelity was maintained by evaluating the extent to which the HEI as delivered adhered to the manualized protocol by randomly reviewing the taped intervention sessions. The objective of the intervention was to facilitate the engagement of the participant in the process of recognizing personal resources, social contextual resources, and the identification of desired health goals and the means to attain these goals (Shearer, 2009). The six weekly visits consisted of integrated components of the HEI focused on: (a) personal resources and building self-capacity; (b) building self-capacity through the recognition of one’s strengths, self-talk, purpose in life, personal growth, and self-acceptance; (c) recognizing and building social networks directed at enhancing awareness of social support and techniques to connect with social networks; (d) identifying and building social service utilization; (e) communicating to build social networks and access social service providers; and (f) reviewing progress toward the attainment of identified health goals, positive changes that occurred, opportunities for building self-capacity, social networks, and accessing social services, and reviewing goals for the future (Figure 2). During each of the six sessions, progress toward individual health goals were reviewed and discussed as a basis for moving forward with intervention content.
Figure 2.
Health Empowerment Framework and Health Empowerment Intervention
Before beginning the study, the NI and research assistants (RAs) were oriented to methods for participant recruitment and tracking, data collection materials, methods for data collection, questions that might be raised by participants, and teaching methods to clarify use of the Goal Attainment Scale. In addition, the NI was trained in the implementation of the HEI. Training lasted approximately 2 weeks. The NI and RAs were trained what to do if they suspected malnutrition, illness, or abuse.
Intervention sessions were audiotaped with permission of the participants to provide a basis for ensuring fidelity to intervention implementation. Detailed notes about the treatment process were kept by the study personnel to track any difficulties encountered and any problems reported by the participants. The NI kept a log of each session, including the duration and nature of contact with participants. The PI listened to random audio-tapes of the intervention sessions and evaluated the fidelity of the intervention sessions to determine if the core components of the session were followed. A checklist with the core components was used to evaluate the extent to which each part of the session was addressed. The PI met with the NI weekly for debriefing to strengthen fidelity by reinforcing the intervention core components and to note needed modifications for future studies.
The attentional comparison group was mailed a first newsletter 1 week after the collection of Time 1 data. The six newsletters provided information on home safety, medication safety, aging and skin care, aging and vision, dental care, and bone health. The information provided to the attentional comparison group did not include theoretically active components of the intervention.
To demonstrate appreciation for participants’ involvement and to enhance retention, $20.00 was given to participants in both groups following each of the three data collection points.
Variables
The participants were assessed at three time points: baseline (Time 1), prior to the first intervention session; 6 weeks (Time 2), after the completion of the intervention; and 12 weeks (Time 3), 6 weeks after Time 2 data collection. The variables of interest included: (a) screening; (b) intervention feasibility (attendance at intervention sessions, attrition, and the participants’ evaluation of acceptability of the intervention); (c) theoretical mediating variables (health empowerment as the recognition of personal resources and social contextual resources; purposeful participation in goal attainment including awareness, choices, freedom to act intentionally, and involvement in creating change); and (d) the outcome of well-being (Table 1).
Table 1.
Schedule of Measurements
| Measure | Time Point | ||||
|---|---|---|---|---|---|
| Prior to Enrollment |
After Missing 2 Consecutive Intervention Contacts |
Week 0 (Time 1) |
Week 6 (Time 2) |
Week 12 (Time 3) |
|
| Screening: Mini-Mental State Examination |
HEI C |
||||
| Intervention Feasibility: Attrition Survey |
HEI | ||||
| Intervention Acceptability: Assessment of Intervention Acceptability |
HEI | ||||
| Participant Characteristics: Demographic Information |
HEI C |
||||
| Health Empowerment Variable: Psychological Scales |
HEI C |
HEI C |
HEI C |
||
| Health Empowerment Variable: Social Services Utilization Data Sheet |
HEI C |
HEI C |
HEI C |
||
| Purposeful Participation in Goal Attainment Variable: Power as Knowing Participation in Change Tool |
HEI C |
HEI C |
HEI C |
||
| Purposeful Participation in Goal Attainment Variable: Goal Attainment Scale |
HEI C |
HEI C |
HEI C |
||
| Ultimate Outcome Measure, Well-being: Well-being Picture Scale |
HEI C |
HEI C |
HEI C |
||
Notes. HEI = Health Empowerment Intervention group, C = Attentional Comparison group
Participant burden was an acknowledged concern as completion of the instruments took approximately 60 minutes at each time point. Therefore, questionnaires were read to the participants as they followed along and frequent breaks were offered to avoid fatigue.
Descriptive information was collected from all participants during Time 1 data collection. Information gathered was information on age, marital status, nationality or ethnic group, level of education in years of schooling, ZIP code, chronic illness information related to diagnosis and date of diagnosis, health insurance, and questions regarding having enough money to meet monthly needs.
Screening Measure
Participants were screened for: (a) age; (b) ability to speak and understand English; (c) ability to hear to respond to questions; and (d) cognitive status. The ability to speak and understand English and the ability to hear and respond to questions were evaluated by personal interaction during the screening and consent process. The MMSE was administered during the screening phase to determine the participant’s cognitive status for entry into the study (Folstein et al., 1975). The MMSE comprises 11 items to assess for orientation, registration, attention, calculation, and recall. A score below 24 out of a possible score of 30 denotes cognitive impairment. Estimates of test-retest reliability in elderly patients revealed correlations between test 1 and test 2 of .98 the MMSE (Folstein et al., 1975).
Intervention Feasibility Measures
Intervention feasibility was conceptualized as the rate of attendance at the planned six HEI sessions, attrition, and participant acceptability of the HEI. Rates of attendance and attrition, as well as reasons for attrition, were reported through visit logs kept by the NI. For the purpose of this study, two consecutive HEI intervention contacts missed constituted attrition, due to the need for continuity in the intervention content to effect change in outcome measures.
Intervention acceptability was assessed using a brief questionnaire to evaluate perceived acceptability and effectiveness of the HEI sessions. The intervention acceptability questionnaire was focused on terms of content, length, format, and timing, as well as acceptability in general. The questions ranged from 1 (not at all) to 4 (very well). This questionnaire was administered after the last intervention session to minimize participant burden. A high score indicates overall acceptability of the intervention in the area of content, length, format and timing.
Theoretical Mediating Variables
Health empowerment
Perceived self-capacity building, a dimension of health empowerment, was operationalized using Ryff’s (1989, 1991) psychological scale measuring the dimensions of personal growth, purpose in life, and self-acceptance. Each dimension consists of 14 items, measured on a 6-point Likert scale ranging from strongly disagree (1) to strongly agree (6). Subscale scores range from 14 to 84. A high score for personal growth indicates a high level of continued development; self as growing and expanding; openness to new experiences; sense of realizing his or her potential; improvement in self; and change in ways that reflect more self-knowledge. A high score for purpose in life indicates that the person has goals in life and a sense of directedness; feels there is meaning to present and past life; holds beliefs that give life purpose; and has aims and objectives for living. A high score for self-acceptance indicates that one possesses a positive attitude toward the self; acknowledges and accepts multiple aspects of self, including good and bad qualities; and feels positive about life. The scales demonstrate convergent and discriminant validity when correlated with existing measures of positive functioning such as life satisfaction and self-esteem and negatively with measures of negative functioning such as control and powerful others (Ryff & Singer, 1996, p. 16). The dimensions have demonstrated validity and internal consistency, with estimates ranging from .85 (personal growth), .88 (purpose in life), to .91 (self-acceptance; Ryff, 2004). Ryff’s (1989) psychological scale has been tested with older adults (n = 80, mean age = 74.96 years, SD = 7.11) with internal consistency coefficients: .87 (personal growth), .90 (purpose in life), and .93 (self-acceptance).
Social network building, as an aspect of health empowerment, was operationalized through Ryff’s (1989, 1991) psychological scale measuring social support as positive relations with others. The scale consists of 14 items, measured on a 6-point Likert scale rated from strongly disagree (1) to strongly agree (6). Total scale scores range from 14 to 84, with a high score indicating positive relations with others as: warm, satisfying, trusting relationships with others; is concerned about the welfare of others; capable of strong empathy, affection, and intimacy; and understands give and take of human relationships. The scale’s demonstrated validity and internal consistency estimates were .88 (Ryff, 2004) and .91 for older adults (Ryff, 1989).
Social services utilization of community services, as another aspect of health empowerment, was measured through the Social Services Utilization Data Sheet in which the participant was asked to list community resources currently used and those used during the past 6 weeks. Both intervention and attentional comparison groups received home-delivered meals at baseline, allowing a test of the intervention related to identification and use of resources consistent with this outcome measure over time.
Purposeful participation in goal attainment
Purposeful participation in goal attainment as a theoretical mediator was operationalized through the Power as Knowing Participation in Change Tool (PKPCT; Barrett, 1986). The PKPCT is a 48-item semantic differential scale, 1- to 7-point interval rating anchored by bipolar adjectives reflecting feelings about awareness, choices, freedom to act intentionally, and involvement in creating change. Scores on the subscale range from 12 to 84. Total scale scores range from 48 to 336; a higher score indicates a greater degree of purposefully participating in change. The measure has demonstrated internal consistency with estimates ranging from .59 to .92 for awareness, .75 to .92 for choices, .71 to .91 for freedom to act intentionally, .57 to .93 for involvement in creating change, and .80 to .97 for the total scale (Caroselli & Barrett, 1998). For the purpose of analysis, a total scale score will be used. Construct validity was supported through factor analysis with item loadings ranging from .56 to .70 on four factors (Barrett & Caroselli, 1998).
Attainment of personally relevant health goals as a dimension of purposeful participation in goal attainment was operationalized using the Goal Attainment Scale (GAS; Kiresuk & Sherman, 1968). According to Rockwood, Stolee, and Fox (1993), the GAS is an individualized outcome measurement technique that has been tested for use in geriatric medicine. The GAS is a 5-point scale with ratings based on the achievement of one or more desired goals that are realistic to achieve in a given time frame. Each goal comprises a set of likely treatment outcomes that are assigned numerical values, with −2 representing the least favorable outcome, +2 representing the most favorable outcome, and 0 assigned to the outcome considered most likely. For each goal, at least two scale points should be identified, with precise, identifiable descriptions that enable an unfamiliar observer to determine whether the participant falls above or below that point (Kiresuk & Sherman, 1968). Interrater reliability of goal attainment scaling with elderly patients was reported as excellent (k > 0.80; Rockwood et al., 1993); a minimum of one to three goals is recommended as older adults may have multiple health concerns. For this study, the participants in the intervention group and attentional comparison group had the opportunity to identify one to three goals to attain.
Health Outcome
The health outcome of well-being was operationalized using the Well-being Picture Scale (WPS; Gueldner et al., 2005). The WPS is a general index of well-being integral to the person-environment process, containing 10 pairs of bipolar drawings. The paired drawings are arranged on white paper, at opposite ends of a seven-choice, unnumbered semantic differential scale. The total scale score ranges from 10 to 70; a high score indicates a higher level of perceived well-being. The WPS is designed for use in adult populations including persons who have limited education, speak English as a second language, may not be able to see well, or are too sick or frail to respond to a lengthy and complex measure. Psychometric properties were established in a sample of more than 2,000 participants from the US and other countries including Taiwan, Japan, and in Africa. The measure has demonstrated validity and internal consistency estimates with an overall Cronbach’s alpha ranging from .88 to .94 (Gueldner et al., 2005). Internal validity of the WPS was assessed through item analysis, with item-to-total correlations ranging from .411 to .785.
Statistical Analysis
Data were double-entered and data sets were compared for completeness, accuracy, and inconsistency. If discrepancies were identified, data entries were compared to the raw data. Missing data ranged from 0 to 7.1%, with the vast majority of variables having no missing values. Because of this low percentage, the expectation-maximization (EM) algorithm was used to impute the missing values.
Analysis of covariance (ANCOVA) using linear mixed models were conducted for Ryff’s Psychological Scale total and subscales (personal growth, positive relations, purpose in life, and self-acceptance), Barrett’s PKPCT total and subscales (awareness, choices, freedom to act intentionally, involvement in creating change), goal attainment, and well-being, as a function of time, treatment group, and time by treatment interaction effects. To look at patterns of change over time, planned contrasts between Time 1 and Time 2, Time 2 and Time 3, and Time 1 and Time 3 were constructed to test for both initial and delayed impact of the intervention. Analyses were performed using all available data (i.e., intent to treat), including participants who subsequently dropped out. Statistical analyses were done using SAS PROC Mixed, Version 9.1.3.
Given the few studies on well-being from an empowerment perspective, and particularly with homebound older adults, any noticeable statistical trend in the desired direction from the intervention is valuable; therefore, the significance level used in the analysis was less than .10. These findings are useful for an initial understanding of treatment efficacy and for providing direction for further studies. While it is understood that these findings will require further investigation, the risk of rejecting important research hypotheses was judged more important than the risk of Type I error. Probability values greater than .05 but less than .10 are reported here as trends.
Results
Flow of Participants and Feasibility as Rate of Attendance, Attrition, and Acceptability
Recruitment began in April 2007 and ended in January 2008. The HEI was run for 3 months for each participant, and data collection ended in May 2008. The flow of sample selection and allocation of participants through the study is shown in Figure 1; 42 participants completed the study. The measures of feasibility as rate of attendance and attrition were whether participants were willing and able to complete the six sessions and three data collection times. In the HEI group (32 participants), 12 participants were lost to attrition (37.5%), 20 participants completed the three data collection times (62.5%), 18 completed all six HEI sessions, and 2 completed four HEI sessions. In the attentional comparison group (27 participants), all participants received the six weekly newsletters. Five participants in the attentional comparison group were lost to attrition; 22 participated in the three data collection times.
The reasons for attrition varied across groups. In the intervention group, two participants were hospitalized, two moved to assisted living, two died, four became too ill to participate, one dropped due to the weekly time commitment, and one wanted assignment to the attentional control group. In the comparison group, one participant was hospitalized, two died, and two wanted assignment to the HEI group. Reviewing the reasons given by participants for not completing the intervention, most were related to the frailty of participants, which contributed to participant dropout.
The majority of participants in the HEI group found the sessions to be very helpful to pretty helpful in helping them to: (a) recognize their personal resources (95%); (b) recognize people to turn to for support (75%); (c) access needed social services (65%); and (d) progress toward the attainment of health goals (75%). On a scale of 1 to 4, the means were 3.75, 3.30, 3.00, and 3.00, respectively. Given the high acceptability scores and the high number of participants that completed the intervention, HEI is an acceptable and feasible intervention for homebound older adults. The intervention sessions lasted an average of 74 minutes.
Description of Participants at Baseline
Demographic characteristics of the participants are summarized in Table 2. Participants were primarily White and female. The average age was 77.77 years (SD = 9.25), the average number of years of schooling was 14.17 (SD = 3.68), and the average number of comorbid conditions per participant was 2.8 (SD = 1.5). Almost half of the participants stated that they did not have enough money. Demographic characteristics of the participants were compared using a t-test for continuous variables and chi-square test for categorical variables to check the randomization procedure. The only significant difference was education, measured by number of years of schooling completed (t = 2.07, p = .04), where the attentional comparison group had a higher mean educational level (15 years) as compared to the intervention group (13 years). Therefore, education was included as a covariate in all analyses.
Table 2.
Demographics of Study Participants
| Comparison n (%) |
Intervention n (%) |
Total n (%) |
|
|---|---|---|---|
| Gender | |||
| Male | 6 (10.2) | 11 (18.6) | 17 (28.8) |
| Female | 21 (35.6) | 21(35.6) | 42(71.2) |
| Total | 27(45.8) | 32(54.2) | 59(100) |
| Marital Status | |||
| Married | 4 (6.8) | 5 (8.5) | 9 (15.3) |
| Separated | 1 (1.7) | 0(0) | 1(1.7) |
| Divorced | 8 (13.6) | 13(22.0) | 21(35.6) |
| Widowed | 13(22.0) | 9(15.3) | 22(37.3) |
| Single | 1 (1.7) | 5(8.5) | 6(10.2) |
| Total | 27(45.8) | 32(54.2) | 59(100) |
| Income | |||
| I do not have enough money | 10 (16.9) | 17 (28.8) | 27(45.8) |
| I have enough money to meet needs | 14 (23.7) | 15(25.4) | 29(49.2) |
| I have more than enough money to meet needs | 3 (5.1) | 0(0.0) | 3(5.1) |
| Total | 27(45.8) | 32(54.2) | 59(100) |
| Ethnicity | |||
| White | 26 (44.1) | 29 (49.2) | 55 (93.2) |
| Hispanic | 1 (1.7) | 0(0) | 1(1.7) |
| Other | 0 (0.0) | 3(5.1) | 3(35.6) |
| Total | 27(45.8) | 32(54.2) | 59(100) |
Changes in Theoretical Mediating Variables and Outcomes
The means for the theoretical mediators and outcome measures for the intervention and control groups at Time 1, Time 2, and Time 3 are displayed in Table 3. There was a significant increase over time in the mediator variable Purposeful Participation in Goal Attainment measured using the GAS (F2,83 = 3.71, p = .03). Follow-up analyses revealed that the intervention group had significantly higher scores at 6 weeks (F1,83 = 10.92, p = .001 ) and at 12 weeks (F1,83 = 5.08, p = .03).
Table 3.
Means and Standard Deviations for Theoretical Mediators and Outcome Measure
| Baseline |
6 Weeks |
12 Weeks |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HEI (n = 32) |
Comparison (n = 27) |
HEI (n = 20) |
Comparison (n = 25) |
HEI (n = 20) |
Comparison (n = 22) |
|||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Ryff Psychological Scale: | ||||||||||||
| Total | 283.34 | 63.84 | 273.59 | 52.33 | 286.90 | 60.64 | 273.68 | 60.27 | 287.90 | 70.86 | 273.41 | 57.35 |
| Personal Growth | 66.89 | 9.03 | 67.98 | 8.38 | 68.13 | 11.21 | 67.80 | 8.62 | 69.63 | 13.89 | 66.35 | 11.04 |
| Purpose in Life | 61.96 | 12.69 | 59.72 | 10.78 | 63.51 | 13.31 | 62.22 | 10.30 | 62.83 | 19.56 | 60.77 | 11.51 |
| Self Acceptance | 62.40 | 14.86 | 61.54 | 13.53 | 62.30 | 13.97 | 61.81 | 15.88 | 63.64 | 16.33 | 63.49 | 15.09 |
| Social Support | 66.34 | 9.94 | 66.36 | 10.65 | 65.75 | 11.33 | 67.94 | 12.11 | 66.00 | 12.06 | 65.38 | 12.61 |
| Social Service Utilization | 1.69 | 0.78 | 1.70 | 0.72 | 1.65 | 0.59 | 1.72 | 0.79 | 1.50 | 0.69 | 1.68 | 0.65 |
| Barrett PKPCT | ||||||||||||
| Total | 283.34 | 63.84 | 273.59 | 52.33 | 286.90 | 60.64 | 273.68 | 60.27 | 287.90 | 70.86 | 273.41 | 57.35 |
| Awareness | 67.22 | 17.70 | 68.52 | 13.76 | 69.55 | 15.71 | 69.08 | 12.87 | 71.70 | 19.77 | 70.14 | 14.58 |
| Choices | 70.03 | 16.57 | 67.11 | 14.96 | 72.40 | 15.18 | 68.28 | 15.90 | 71.10 | 18.26 | 66.77 | 16.90 |
| Freedom to Act Intentionally | 73.41 | 16.09 | 68.67 | 14.81 | 71.60 | 17.31 | 70.04 | 16.88 | 72.10 | 17.28 | 68.77 | 16.20 |
| Involvement in Creating Change | 72.69 | 16.58 | 69.30 | 13.38 | 73.35 | 16.54 | 66.28 | 18.18 | 73.00 | 18.45 | 67.73 | 15.19 |
| Goal Attainment Scale | 51.06 | 8.28 | 43.33 | 10.07 | 46.56 | 12.13 | 41.55 | 13.75 | ||||
| Well-being Picture Scale | 52.56 | 12.65 | 50.81 | 13.69 | 53.75 | 15.42 | 54.04 | 10.06 | 53.35 | 13.78 | 51.95 | 14.29 |
Notes. HEI = Health Empowerment Intervention, PKPCT = Power as Knowing Participation in Change Tool
There was no significant main effect for the theoretical mediator health empowerment operationalized through Ryff’s Psychological Scale total. However, the subscale personal growth showed significant difference between the attentional comparison and intervention groups from Time 1 to Time 3 (F1,83 =3.88, p =.05). Whereas the attentional comparison group decreased from baseline to Time 3, the intervention group increased in personal growth. In addition, there were subgroups which benefited significantly from the intervention for several of the subscales. Low-income subjects (1 standard deviation below the mean) in the intervention group tended to do better than the low-income subjects in the attentional comparison group on the personal growth subscale at Time 3 (F1,79 = 3.26, p = .07). Subjects with a high number of comorbid conditions (1 standard deviation above the mean) in the intervention group did better than their counterparts in the attentional comparison group on the subscale of self-acceptance. Those with greater numbers of comorbid conditions in the intervention group had higher scores on the self-acceptance subscale than those in the attentional comparison group from Time 2 to Time 3 (F1,79 = 5.13, p = .03).
There was no significant main effect for the Barrett’s PKPCT total score. However, there were significant differences by gender. Males in the intevention group (n = 11) had significantly higher scores compared to the males in the attentional comparison group (n = 6) at Time 2 (F1,79 = 4.94, p = .03 ) and Time 3 (F1,79 = 4.26, p = .04 ). Likewise, there were significant differences between the males in the intervention group and the males in the attentional comparison group for the subscales of awareness, choices, and involvement in creating change. There was a significant difference between intervention males and attentional comparison males at both Time 3 (F1,79 = 4.43, p = .04 ) and between Time 1 and Time 3 (F1,79 = 4.38, p = .04) for the subscale of awareness. Males in the intervention group had borderline higher scores than males in the control group for the choices subscale at Time 2 (F1,79 = 3.79, p = .06) and Time 3 (F1,79 = 3.48, p = .07). Similarly, there was a significant difference between the males in the intervention and attentional comparison groups for the subscale of involvement in creating change, with a significant difference at Time 2 (F1,79 = 9.24, p = .003) and a borderline difference at Time 3 (F1,79 = 3.19, p = .08) and a difference over time between Time 1 and Time 2 (F1,79 = 6.25, p = .02). There was no significant difference for the freedom to act intentionally subscale. Also, there were no significant differences for the females on the Barrett’s PKPCT.
There were no significant main effects between the intervention and attentional comparison group for the Well-Being Picture scale. However, there were significant differences between the groups for well-being among those who were older; the intervention group increased in well-being between Time 2 and Time 3 (F1,79 = 6.79, p = .01) compared to the attentional comparison group.
Discussion
This randomized control trial provided initial support for the hypothesis that homebound older adults receiving the HEI would find the intervention acceptable and have significantly improved health empowerment, purposeful participation in goal attainment, and well-being than an attentional comparison group receiving a weekly newsletter. In addition, the results provide a beginning understanding of the effects of the intervention in promoting health empowerment in homebound older adults.
Incorporated in the HEI was an innovative approach that acknowledged and built on inherent self-capacity. Despite the vulnerabilities of homebound older adults, in the intervention, older adult strengths’ were acknowledged and developed to promote their awareness and engagement of their self-capacity. In this sample of homebound older adults, participants in the intervention group increased their self-capacity, including the perception of self as growing and expanding; open to new experiences; realizing potential; improving; and changing in ways that reflect self-knowledge. These findings are congruent with the qualitative findings of Shearer (2008) and Shearer et al. (2009).
Homebound older adults receiving the intervention were more successful in attaining their personally relevant health goals, suggesting that while older adults have multiple health concerns, they are able to engage in identifying and working toward the attainment of individual health goals. The sensitivity to change in health goals found in the intervention group is congruent with the findings of Rockwood et al. (1993), in which the goal attainment measure was sensitive to change and was an efficient measure of health status of frail older adults.
While no main effects were found for the theoretical mediating variables of health empowerment and purposeful participation in goal attainment, or the outcome of well-being, there were significant subscale differences found in the intervention group by income, age, number of chronic conditions, and gender, supporting the theory-based intervention. That is, the older, frailer male participants with more chronic conditions and less money seemed to benefit the most from the intervention.
As people age, they are at risk for developing chronic conditions. According to Wolff et al. (2002), older adults with four or more chronic conditions report more hospitalizations than those without a chronic condition. The findings of this study support the HEI as increasing self-acceptance and well-being in the older homebound participant. The intervention may have the potential for helping older adults attain their health goals and potentially promoting aging in place.
Health empowerment was enhanced in the males participating in the intervention group as supported by the higher scores in Barrett’s PKPCT subscales of awareness, choices, and involvement in creating change. These findings support the intervention as facilitating males’ awareness that they had a choice and could be involved in determining and attaining their health goals. For some men, this may have been the first time that they engaged in determining and attaining their health goals. That is, women are often responsible and recognized as the gatekeepers of the family’s health, limiting the opportunity for men to determine and attain their healthcare goals.
Social network building, as an aspect of health empowerment, was not found to be significant; the importance of social support in the promotion of well-being of older adults has been supported in other studies (Boland, 2000; Shearer, 2007; Shearer & Fleury, 2006). The Ryff (Ryff & Singer, 1996) subscale used to measure social network seemed to be congruent with the Health Empowerment theory as it is focused on positive relations with others and the importance of positive relations with others in promoting well-being. In addition, the participants in this study scored fairly high on both social support and well-being, leaving little room for improvement.
Caution should be exercised regarding the findings due to several limitations. Homebound older adults were recruited from a home-delivered meal program located in a metropolitan area that serves a greater percentage of older White adults, limiting the generalizability of the findings to other ethnic groups. However, few studies have been focused on this vulnerable population. Future studies are needed to look at a more diverse older population.
The research findings from this study represent the first step within a program of research aimed at determining the effectiveness of the HEI in producing the desired theoretical mediating and ultimate outcomes. The theory of health empowerment postulates that emerging from the health empowerment process is a transformation, in which the older adult recognizes his or her ability to participate purposefully in goal attainment and facilitates awareness of and access to needed resources, thereby promoting well-being. Overall, the findings support a strength-based approach to facilitating health empowerment in homebound older adults. The findings of this study quantitatively support prior qualitative findings that older adults have personal strengths (Shearer, 2008) and social contextual resources (Shearer & Fleury, 2006) that play an important role in promoting well-being in older adults.
Acknowledgments
This study was funded by the National Institutes of Health, National Institute of Nursing Research, # 1 R15 NR009225-01A2.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Nelma B. Crawford Shearer, Associate Professor and Co-Director, Hartford Center of Geriatric Nursing Excellence, College of Nursing & Health Innovation, Arizona State University, Phoenix, AZ.
Julie D. Fleury, Hanner Professor, Associate Dean for Research, Director, PhD Program, College of Nursing & Health Innovation, Arizona State University, Phoenix, AZ.
Michael Belyea, Research Professor, College of Nursing & Health Innovation, Arizona State University, Phoenix, AZ.
References
- Administration on Aging, Department of Health and Human Services. A profile of older Americans: 2007. Washington, DC: 2007. Author. Retrieved from http://www.agingcarefl.org/aging/AOA-2007profile.pdf. [Google Scholar]
- Barrett EAM. Investigation of the principle of helicy: The relationship of human field motion and power. In: Malinski V, editor. Explorations on Martha Rogers’ science of unitary human beings. Norwalk, CT: Appleton-Century-Crofts; 1986. pp. 173–184. [Google Scholar]
- Barrett EA, Caroselli C. Methodological ponderings related to the power as knowing participation in change tool. Nursing Science Quarterly. 1998;11(1):17–22. doi: 10.1177/089431849801100106. [DOI] [PubMed] [Google Scholar]
- Boland CS. Social support and spiritual well-being: Empowering older adults to commit to health-promoting behaviors. The Journal of Multicultural Nursing & Health. 2000;6(3):12–23. [Google Scholar]
- Caroselli C, Barrett EA. A review of the power as knowing participation in change literature. Nursing Science Quarterly. 1998;11(1):9–16. doi: 10.1177/089431849801100105. [DOI] [PubMed] [Google Scholar]
- Eckert JK, Morgan LA, Swamy N. Preferences for receipt of care among community-dwelling adults. Journal of Aging & Social Policy. 2004;16(2):49–65. doi: 10.1300/J031v16n02_04. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state.” A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Gueldner SH, Michel Y, Bramlett MH, Liu C, Johnston LW, Endo E, et al. The well-being picture scale: A revision of the index of field energy. Nursing Science Quarterly. 2005;18(1):42–50. doi: 10.1177/0894318404272107. [DOI] [PubMed] [Google Scholar]
- Itzhaky H, Schwartz C. Empowering the disabled: A multidimensional approach. International Journal of Rehabilitation Research. 1998;21(3):301–310. [PubMed] [Google Scholar]
- Keller C, Fleury J. Health promotion for the elderly. Thousand Oaks, CA: Sage; 2000. [Google Scholar]
- Kiresuk TJ, Sherman RE. Goal attainment scaling: A general method for evaluating comprehensive community mental health programs. Community Mental Health Journal. 1968;4:443–453. doi: 10.1007/BF01530764. [DOI] [PubMed] [Google Scholar]
- Leyshon S. Empowering practitioners: An unrealistic expectation of nurse education? Journal of Advanced Nursing. 2002;40(4):466–474. doi: 10.1046/j.1365-2648.2002.02395.x. [DOI] [PubMed] [Google Scholar]
- Perkins DD, Zimmerman MA. Empowerment theory, research, and application. American Journal of Community Psychology. 1995;23(5):569–579. doi: 10.1007/BF02506982. [DOI] [PubMed] [Google Scholar]
- Rappaport J. Studies in empowerment: Introduction to the issue. Prevention in Human Services. 1984;3:1–7. [Google Scholar]
- Rockwood K, Stolee P, Fox RA. Use of goal attainment scaling in measuring clinically important change in the frail elderly. Journal of Clinical Epidemiology. 1993;46(10):1113–1118. doi: 10.1016/0895-4356(93)90110-m. [DOI] [PubMed] [Google Scholar]
- Ryff CD. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. Journal of Personality and Social Psychology. 1989;57(6):1069–1081. [Google Scholar]
- Ryff CD. Possible selves in adulthood and old age: A tale of shifting horizons. Psychology and Aging. 1991;6(2):286–295. doi: 10.1037//0882-7974.6.2.286. [DOI] [PubMed] [Google Scholar]
- Ryff CD. Description of scales of psychological well-being. 2004 Unpublished raw data. [Google Scholar]
- Ryff CD, Singer B. Psychological well-being: Meaning, measurement, and implications for psychotherapy research. Psychotherapy and Psychosomatics. 1996;65(1):14–23. doi: 10.1159/000289026. [DOI] [PubMed] [Google Scholar]
- Shearer NBC. Relationships of contextual and relational factors to health empowerment in women. Research and Theory for Nursing Practice. 2004;18(4):357–370. doi: 10.1891/rtnp.18.4.357.64094. [DOI] [PubMed] [Google Scholar]
- Shearer NBC. Toward a nursing theory of health empowerment in homebound older women. Journal of Gerontological Nursing. 2007;33(12):38–45. doi: 10.3928/00989134-20071201-05. [DOI] [PubMed] [Google Scholar]
- Shearer NBC. Hair, hands, and oxygen tanks: Embodiment and health empowerment in homebound older women. Visions: The Journal of Rogerian Nursing Science. 2008;15(1):18–27. [Google Scholar]
- Shearer NBC. Health empowerment theory as a guide for practice. Geriatric Nursing. 2009;30(2 Suppl.):4–10. doi: 10.1016/j.gerinurse.2009.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shearer NBC, Fleury J. Social support promoting health in older women. Journal of Women & Aging. 2006;18(4):3–17. doi: 10.1300/J074v18n04_02. [DOI] [PubMed] [Google Scholar]
- Shearer N, Fleury J, Belyea M. Research in Gerontological Nursing. An innovative approach to recruiting homebound older adults. (In press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shearer NBC, Fleury JD, Reed PG. The rhythm of health in older women with chronic illness. Research and Theory for Nursing Practice. 2009;23(2):148–160. doi: 10.1891/1541-6577.23.2.148. [DOI] [PubMed] [Google Scholar]
- Shearer NBC, Reed PG. Empowerment: Reformulation of a non-Rogerian concept. Nursing Science Quarterly. 2004;17(3):253–259. doi: 10.1177/0894318404266325. [DOI] [PubMed] [Google Scholar]
- Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Archives of Internal Medicine. 2002;162(20):2269–2276. doi: 10.1001/archinte.162.20.2269. [DOI] [PubMed] [Google Scholar]