Abstract
Objective
To identify intrapartum predictors of newborn encephalopathy in term infants.
Design
Population based, unmatched case-control study.
Setting
Metropolitan area of Western Australia, June 1993 to September 1995.
Subjects
All 164 term infants with moderate or severe newborn encephalopathy; 400 randomly selected controls.
Main outcome measures
Adjusted odds ratio estimates.
Results
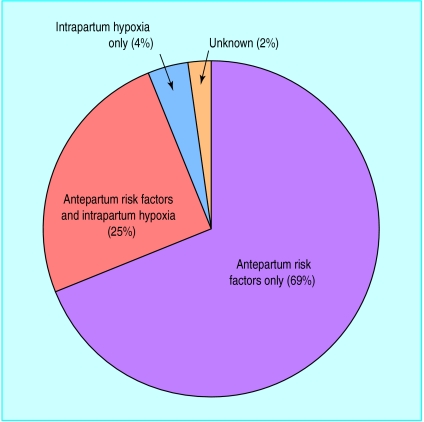
The birth prevalence of moderate or severe newborn encephalopathy was 3.8/1000 term live births. The neonatal fatality was 9.1%. Maternal pyrexia (odds ratio 3.82), a persistent occipitoposterior position (4.29), and an acute intrapartum event (4.44) were all risk factors for newborn encephalopathy. More case infants than control infants were induced (41.5% and 30.5%, respectively) and fewer case infants were delivered by caesarean section without labour (3.7% and 14.5%, respectively). Operative vaginal delivery (2.34) and emergency caesarean section (2.17) were both associated with an increased risk. There was an inverse relation between elective caesarean section (0.17) and newborn encephalopathy. After application of a set of consensus criteria for elective caesarean section only three (7%) eligible case mothers compared with 33 (65%) eligible control mothers were sectioned electively. Of all the case infants, 113 (69%) had only antepartum risk factors for newborn encephalopathy identified; 39 (24%) had antepartum and intrapartum factors; eight (5%) had only intrapartum factors; and four (2%) had no recognised antepartum or intrapartum factors.
Conclusions
The causes of newborn encephalopathy are heterogeneous and many relate to the antepartum period. Elective caesarean section has an inverse association with newborn encephalopathy. Intrapartum hypoxia alone accounts for only a small proportion of newborn encephalopathy. These results question the view that most risk factors for newborn encephalopathy lie in the intrapartum period.
Key messages
Intrapartum risk factors for newborn encephalopathy include maternal pyrexia, persistent occipitoposterior position, and acute intrapartum events
Operative vaginal delivery and emergency caesarean section were both associated with an increased risk whereas there was an inverse relation with elective caesarean section
There was no evidence of intrapartum hypoxia in over 70% of cases of newborn encephalopathy
The causes of newborn encephalopathy are heterogeneous and many relate to the antepartum period
These findings bring into question the view that most risk factors for newborn encephalopathy lie in the intrapartum period
Introduction
Previous studies of newborn encephalopathy have focused almost exclusively on the intrapartum causes of “hypoxic ischaemic encephalopathy.”1–7 The contribution of intrapartum events to newborn encephalopathy remains unclear. We report the intrapartum findings from the Western Australian case-control study of newborn encephalopathy.8
Subjects and methods
The subjects and methods are as reported in the accompanying paper.8
Results
Intrapartum period
Maternal pyrexia, a persistent occipitoposterior position, and an acute intrapartum event were all labour related events associated with a significantly increased risk of newborn encephalopathy (table 1). Only nine of the 18 affected infants and none of the nine control infants whose mothers had experienced pyrexia had a pathogenic organism isolated from mother or baby. A prolonged interval from rupture of membranes to delivery, abnormalities in blood pressure, a nuchal cord, cord prolapse, and shoulder dystocia were associated with a non-significantly increased risk.
Table 1.
Risk factors for newborn encephalopathy present in intrapartum period and adjusted for factors before birth and antepartum
| Risk factor | No (%) of cases (n=164) | No (%) of controls (n=400) | Unadjusted odds ratio | Adjusted odds ratio* (95% CI) |
|---|---|---|---|---|
| Occipitoposterior presentation: | ||||
| No | 147 (89.6) | 385 (96.2) | 1† | 1† |
| Yes | 17 (10.4) | 15 (3.8) | 2.97 | 4.29 (1.74 to 10.54) |
| Maternal pyrexia (⩾37.5°C): | ||||
| No | 146 (89.0) | 391 (97.8) | 1† | 1† |
| Yes | 18 (11.0) | 9 (2.2) | 5.34 | 3.82 (1.44 to 10.12) |
| Acute intrapartum event‡: | ||||
| No | 151 (92.1) | 395 (98.8) | 1† | 1† |
| Yes | 13 (7.9) | 5 (1.2) | 6.80 | 4.44 (1.30 to 15.22) |
| Membrane rupture to delivery interval >12 hours: | ||||
| No | 132 (80.5) | 347 (86.7) | 1† | 1† |
| Yes | 32 (19.5) | 53 (13.2) | 1.59 | 1.31 (0.69 to 2.47) |
| Blood pressure abnormalities: | ||||
| No | 154 (93.9) | 383 (95.8) | 1† | 1† |
| Yes | 10 (6.1) | 17 (4.2) | 1.46 | 1.78 (0.61 to 5.15) |
| Nuchal cord: | ||||
| No | 142 (86.6) | 369 (92.2) | 1† | 1† |
| Yes | 22 (13.4) | 31 (7.8) | 1.84 | 1.81 (0.85 to 3.86) |
| Cord prolapse: | ||||
| No | 163 (99.4) | 399 (99.8) | 1† | 1† |
| Yes | 1 (0.6) | 1 (0.2) | 2.45 | 4.71 (0.21 to 105.02) |
| Onset of labour: | ||||
| Spontaneous | 90 (54.9) | 220 (55.0) | 1† | 1† |
| Induced | 68 (41.5) | 122 (30.5) | 1.36 | 0.97 (0.57 to 1.68) |
| None | 6§ (3.7) | 58 (14.5) | 0.25 | 0.17 (0.06 to 0.49) |
| Mode of delivery: | ||||
| Spontaneous vaginal | 49 (29.9) | 261 (40.3) | 1† | 1† |
| Induced vaginal | 32 (19.5) | 80 (20) | 1.31 | 1.10 (0.55 to 2.18) |
| Instrumental vaginal | 42 (25.6) | 62 (15.5) | 2.23 | 2.34 (1.16 to 4.70) |
| Elective caesarean section | 4 (2.4) | 58 (14.5) | 0.23 | 0.17 (0.05 to 0.56) |
| Emergency caesarean section | 34 (20.7) | 38 (9.5) | 2.94 | 2.17 (1.01 to 4.64) |
| Breech manoeuvre | 3 (1.8) | 1 (0.3) | 9.86 | 1.54 (0.10 to 25.14) |
| Shoulder dystocia: | ||||
| No | 155 (94.5) | 393 (98.3) | 1† | 1† |
| Yes | 9 (5.5) | 7 (1.7) | 3.26 | 3.0 (0.77 to 11.67) |
| General anaesthesia: | ||||
| No | 146 (89.0) | 389 (97.2) | 1† | 1† |
| Yes | 18 (11.0) | 11 (2.8) | 4.40 | 3.08 (1.16 to 8.17) |
| Epidural anaesthesia: | ||||
| No | 145 (88.4) | 331 (82.8) | 1† | 1† |
| Yes | 19 (11.6) | 69 (17.2) | 0.64 | 0.51 (0.26 to 1.02) |
Adjusted for maternal age, parity, employment status, health insurance status, race, family history of epilepsy and other neurological disease, infertility treatment, hypertension, height, thyroid disease, pre-eclampsia, moderate or severe bleeding, viral illness, alcohol consumption, gestational age, centile birth weight, infant sex, appearance of placenta, late or no antenatal care, hospital of delivery, and plurality.
Baseline comparison group. ‡Haemorrhage (n=7), maternal convulsions (n=2), rupture of uterus (n=1), snapped cord (n=1), and birth of baby before arrival at obstetric facility (n=2). §Includes two women who had emergency caesarean sections before onset of labour.
Onset of labour and final mode of delivery
The final mode of delivery is determined by the delivery plan and response to intrapartum events. As the delivery plan could not be determined onset of labour was investigated as a surrogate (table 1). The same proportion of cases and controls had spontaneous onset of labour. More case infants than control infants, however, were induced and fewer case infants were delivered by caesarean sections without labour.
Overall, a similar proportion of case and control infants were delivered by caesarean sections (23% (38) and 24% (96), respectively). Relative to spontaneous vaginal delivery, instrumental vaginal delivery and emergency section were associated with over a twofold increased risk of encephalopathy. Only 2.4% (four) affected infants compared with 14.5% (58) of control infants were delivered by elective section, defined as one planned at least 24 hours before the procedure (adjusted odds ratio relative to spontaneous vaginal delivery 0.17; 95% confidence interval 0.05 to 0.56). This inverse relation was not explained by social factors, including health insurance status, as these had been adjusted for. The documented indications for elective sections among case and control infants are shown in table 2; previous caesarean section was the most common.
Table 2.
Indications for elective caesarean section documented by midwife according to whether baby had newborn encephalopathy (cases) or not (controls)
| Indication | No delivered by caesarean |
|---|---|
| Controls (n=58) | |
| Previous caesarean section | 32 |
| Malpresentations | 9 |
| Previous difficult labour | 4 |
| Intrauterine growth retardation | 2 |
| Placenta previa | 2 |
| Other reasons* | 9 |
| Cases (n=4) | |
| Two previous caesarean sections | 2 |
| One previous caesarean section | 1 |
| Intrauterine growth retardation | 1 |
One each of antepartum fetal tachycardia, active herpes infection, nephrotic syndrome, cephalopelvic disproportion, pre-eclampsia with inflammatory bowel syndrome, oligohydramnios, macrosomia, maternal request, reason not given.
To ascertain whether different risk factor profiles explained the differences in proportion of emergency and elective caesarean sections, 14 practising consultant obstetricians from Perth were asked to develop a set of criteria which would lead them to recommend an elective section at term in the interest of the baby. The consensus, which was developed without knowledge of the study results, comprised intrauterine growth restriction, malpresentation, abnormal antepartum cardiotocography, two previous sections, macrosomia with diabetes or gestational diabetes, active herpes, and a previous difficult labour. When we applied these consensus criteria to mothers of case and control infants (table 3) eligible mothers of case infants were 24 times less likely (unadjusted odds ratio relative to spontaneous vaginal delivery 24.2; 6.61 to 90.1) than eligible mothers of control infants to have been sectioned electively. Nearly 40% of the eligible case infants were eventually delivered by an emergency section and nearly 20% were delivered instrumentally or by vaginal breech delivery. The consensus criteria met by eligible mothers are summarised in table 4. This shows that even in the group that met the consensus criteria there was a difference in antepartum risk factor profiles between cases and controls.
Table 3.
Details of onset of labour and final mode of delivery in cases (babies with newborn encephalopathy) and controls by eligibility for elective caesarean section according to consensus criteria.* Values are numbers (percentages) of subjects
| Detail | Cases
|
Controls
|
|||
|---|---|---|---|---|---|
| Elective section candidates (n=43) | Others (n=121) | Elective section candidates (n=51) | Others (n=349) | ||
| Labour onset: | |||||
| Spontaneous | 19 (44.2) | 71 (58.7) | 9 (17.7) | 211 (60.5) | |
| Induced | 20 (46.5) | 48 (39.7) | 9 (17.7) | 113 (32.4) | |
| None | 4† (9.3) | 2 (1.7) | 33 (64.7) | 25 (7.2) | |
| Final mode of delivery: | |||||
| Elective caesarean | 3 (7.0) | 1 (0.8) | 33 (64.7) | 25 (7.2) | |
| Non-elective caesarean | 17 (39.5) | 17 (14.1) | 7 (13.7) | 31 (8.9) | |
| Instrumental and breech | 8 (18.6) | 37 (30.6) | 4 (7.8) | 59 (16.9) | |
| Induced vaginal | 8 (18.6) | 24 (19.8) | 5 (9.8) | 75 (21.5) | |
| Spontaneous vaginal | 7 (16.3) | 42 (34.7) | 2 (3.9) | 159 (45.6) | |
Eligiblity defined by consensus opinion of 14 obstetricians. Consensus list was intrauterine growth retardation, malpresentation, abnormal antepartum cardiotocogram, two previous caesarean sections, macrosomia with diabetes or gestational diabetes, active herpes, and previous difficult labour.
Includes two women who had emergency caesarean sections before onset of labour.
Table 4.
Consensus criteria met by mothers of cases (babies with newborn encephalopathy) and controls eligible for elective caesarean section.* Values are numbers (percentages) of subjects
| Consensus criteria* | Eligible cases (n=43) | Eligible controls (n=51) |
|---|---|---|
| Predicted infant weight <3rd centile | 21 (48.8) | 5 (9.8) |
| Abnormal antepartum cardiotocogram | 14 (32.6) | 8 (15.7) |
| Breech and other malpresentations | 9 (20.9) | 21 (41.2) |
| Two previous caesareans | 3 (7.0) | 12 (23.5) |
| Previous difficult labour | 0 (0) | 4 (7.8) |
| Gestational diabetes and macrosomia | 1 (2.3) | 0 (0) |
| Active herpes | 0 (0) | 2 (3.9) |
These criteria are not mutually exclusive.
Other intrapartum factors
The presence of an abnormal intrapartum cardiotocogram, meconium stained liquor, and fetal distress are usually considered to reflect intrapartum hypoxia and were not included in the adjusted analyses as they were likely to be along a causal pathway for, or the first signs of, newborn encephalopathy or were markers of encephalopathy. Inclusion of these variables in the adjusted analysis would have masked the effects of other variables that were working through them. Half the affected infants had intrapartum cardiotocography performed compared with 30% of control infants. The cardiotocogram was described as abnormal in 61% of affected infants compared with 37% of control infants (unadjusted odds ratio 4.43; 1.81 to 10.85). Meconium was described more commonly in case infants than control infants (33% v 12%; 3.72; 2.33 to 5.95) and grade III meconium in particular was much more common in case infants (13% v 1.0%; 16.7; 5.76 to 50.0). Finally, fetal distress during labour was recorded by the midwife more often in case infants than control infants (21% v 8%; 3.16; 1.84 to 5.43). For the same reason we did not include immediate characteristics of the newborn (table 5) in the adjusted analysis.
Table 5.
Immediate characteristics of babies with encepalopathy (cases) and controls. Values are numbers (percentages) of subjects
| Characteristic | Cases (n=164) | Controls (n=400) |
|---|---|---|
| Apgar at 1 minute: | ||
| <3 | 50 (30.5) | 3 (0.7) |
| 3-6 | 46 (28.1) | 37 (9.2) |
| >6 | 67 (40.8) | 359 (89.7) |
| Missing | 1 (0.6) | 1 (0.2) |
| Apgar at 5 minutes: | ||
| <3 | 14 (8.5) | 0 |
| 3-6 | 40 (24.4) | 5 (1.2) |
| >6 | 108 (65.9) | 394 (98.5) |
| Missing | 2 (1.2) | 1 (0.2) |
| Onset of respiration: | ||
| ⩽2 minutes | 83 (50.6) | 373 (93.2) |
| >2 minutes | 68 (41.5) | 15 (3.7) |
| Not established | 6 (3.7) | 0 |
| Missing | 7 (4.2) | 12 (3.0) |
| Airway resuscitation: | ||
| None | 30 (18.3) | 283 (58.2) |
| Suction alone | 15 (9.1) | 82 (20.5) |
| Oxygen | 29 (17.7) | 49 (12.2) |
| Bag and mask | 35 (21.3) | 30 (7.5) |
| Intubation | 44 (26.8) | 4 (1.0) |
| Intubation and CPR* | 10 (6.2) | 0 |
| Missing | 1 (0.6) | 2 (0.5) |
| Cord pH: | ||
| Not measured | 135 (82.4) | 391 (97.7) |
| <7.0 | 5 (3.0) | 0 |
| 7.0-7.1 | 14 (8.5) | 2 (0.5) |
| ⩾7.2 | 9 (5.5) | 6 (1.5) |
| Missing | 1 (0.6) | 1 (0.2) |
| Birth trauma: | ||
| Present | 17 (10.4) | 0 |
Cardiopulmonary resuscitation.
Contribution of possible intrapartum hypoxia
In an attempt to estimate the proportion of infants who had been exposed to possible intrapartum hypoxia we used the following modified criteria: presence of an abnormal intrapartum cardiotocogram or abnormal fetal heart rate on auscultation or fresh meconium in labour, or both, together with a 1 minute Apgar score of less than 3 and a 5 minute Apgar score of less than 7.9 Cord pH measurements were not included because they were performed so infrequently. Thirty one affected infants (19%) and two control infants (0.5%) fulfilled these criteria. A further 16 cases did not strictly fulfil the definition, but there was evidence that they had experienced a significant intrapartum event which may have been associated with intrapartum hypoxia (for example, breech presentation, birth before arrival at hospital, head stuck, Apgar scores not measured). Therefore, a total of 47 case infants (29%) had evidence of having experienced intrapartum hypoxia. Only seven of these (4% of all cases), however, fulfilled the criteria of possible intrapartum hypoxia in the absence of preconceptional or antepartum abnormalities. Four case infants (2%) had no recognised antepartum risk factors or evidence of intrapartum hypoxia and 113 (69%) had only antepartum factors identified (figure 1). Only 15 of these 47 case infants met the consensus eligibility criteria for an elective caesarean section.
Figure 1.
Distribution of risk factors for newborn encephalopathy
Discussion
Our results indicate that intrapartum hypoxia alone accounts for only a small proportion of cases of newborn encephalopathy, and elective caesarean section had an unexpected inverse association with newborn encephalopathy.
Role of intrapartum hypoxia
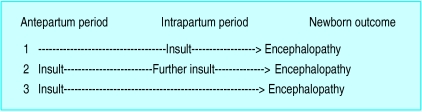
Although 29% of affected infants experienced events traditionally indicative of birth asphyxia, it does not necessarily follow that asphyxia was the primary cause of the encephalopathy. While some intrapartum factors may be single causes—that is, a previously normal baby who becomes encephalopathic in labour (fig 2, pathway 1)—this was an uncommon scenario in our study (see fig 1). Other factors may be on a causal pathway that starts before birth but which includes intrapartum hypoxia as a contributor (figure 2, pathway 2). For example, growth restriction alone is associated with newborn encephalopathy8 and exposure to labour may compound that damage.10 A further possibility is that the intrapartum factors are merely markers of damage associated with adverse events before birth (fig 2, pathway 3). Abnormality on a cardiotocogram, meconium stained liquor, low Apgar scores, or the need for active resuscitation may simply reflect previous neurological compromise.11
Figure 2.
Theoretical scenarios for timing of neurological insult in newborn encephalopathy
A very small proportion of infants had no recognised antepartum risk factors nor evidence of intrapartum hypoxia, and it remains unclear as to when their encephalopathy started and what caused it. Over two thirds of affected infants had only antepartum factors identified. Together these two groups represent over 70% of cases among which there was no evidence of adverse intrapartum events. This points to the antepartum period being of prime aetiological importance in most cases of newborn encephalopathy.
Infection
Maternal pyrexia in labour was a significant risk factor, confirming our previous finding.12 Prolonged interval between rupture of membranes and delivery, a risk factor for ascending infection, was more common in cases compared with controls but not significantly so. Chorioamnionitis is of current interest as a cause of cerebral palsy in both term13 and preterm14 infants. The mechanisms of fetal damage, however, are not known but could include cerebral sepsis, hyperthermia, or action via inflammatory mediators.15
Caesarean section
The most striking finding relates to mode of delivery. These data suggest an important inverse association between elective caesarean section and newborn encephalopathy. There are several possible explanations for this finding. Chance alone is an unlikely explanation, as shown by the 95% confidence interval, although mode of delivery was not one of the initial study hypotheses.12 The results are also unlikely to be due to biased selection of control subjects. The control subjects were randomly selected and their final mode of delivery and all 21 other characteristics of pregnancy, labour, and infant available for comparison were the same as for all term live births in Western Australia during the study period.16 There was no evidence of case selection bias as all affected infants were included and none died before transfer.8 We therefore conclude that our findings are real.
A vital distinction, not made in most other studies, is the differentiation between elective and non-elective sections.2,12,17,18 Had we failed to make this distinction we would have concluded that caesarean section had no effect on the risk of newborn encephalopathy. When we applied the eligibility criteria for elective sections we found that eligible case infants were more than 20 times less likely to be delivered by elective section than eligible control infants. The reasons for the apparent differences in the management of labour in the cases and controls are undoubtedly complex and may reflect genuine differences (see table 4). Unrecognised high risk features, alternatives to the consensus view, women’s choice of vaginal delivery, or perhaps some undefined factors which led a pregnancy to result in a baby with encephalopathy may also have operated to affect the management of delivery. As the definition of an elective caesarean section was one in which there were 24 hours between the decision and delivery, it is also possible that some of these women had been booked for an elective section which they did not receive because they went into labour. On close review of the eligible cases, however, a maximum of only 20% could possibly fall into this category.
It is of note that even in those women not meeting the consensus criteria for elective section, mothers of control infants were electively sectioned much more commonly than mothers of case infants. Furthermore, eligible mothers of case infants did not avoid operative and instrumental delivery but had emergency rather than elective procedures. Non-elective sections involve inherently more operative and postoperative risk, reflected in the lower maternal morbidity after elective sections.19 In addition, the baby delivered by a non-elective section has usually been exposed to the stresses of labour, and this may have an independent impact on outcome.
Elective caesarean sections may exert their apparent beneficial effects by avoiding some of the intrapartum risk factors for encephalopathy. For example, elective sections prevent exposure to post-maturity, persistent occipitoposterior position, intrapartum maternal pyrexia, and catastrophic events in labour. It may be the avoidance of these factors other than caesarean section per se which contributes to its apparent benefit.
We readily recognise that there is no “correct rate” of elective caesarean sections, but it is pertinent to ask whether women who would benefit most are being identified and given access to this method of delivery. It is not possible to say from this observational study whether elective section would have actually changed the outcome in any of the cases, but it is an obvious question and one worthy of further investigation. As a trial to answer this question is unlikely ever to be performed,20 however, observational studies such as this would probably be our only source of information. It is, however, pertinent to note that our findings cannot be used to argue on a very wide basis that disability can be prevented by elective caesarean section.
Increasingly, the debate about the aetiology of perinatal brain injury emphasises the relatively small contribution of the intrapartum period. The presence of antepartum events does not mean that the intrapartum course did not contribute to the final outcome. Nevertheless, even with the best care not all potentially damaging intrapartum events are avoidable. It seems likely, however, that many babies already have encephalopathy before labour and others, whose reserve is diminished at the onset of labour, may have less capacity to cope with hypoxia when it occurs during labour. Elucidating these multiple pathways will be the only way we can go forward in the prevention of newborn encephalopathy.
Acknowledgments
For acknowledgements and details of contributors, funding, and competing interests please see the accompanying paper.8
Editorial by Edwards
Footnotes
Dr Alessandri died in August 1997
References
- 1.Nelson KB, Leviton A. How much of neonatal encephalopathy is due to birth asphyxia? Am J Dis Child. 1991;145:1325–1331. doi: 10.1001/archpedi.1991.02160110117034. [DOI] [PubMed] [Google Scholar]
- 2.Finer NN, Robertson CM, Richards RT, Pinnell LE, Peters KL. Hypoxic-ischemic encephalopathy in term neonates: perinatal factors and outcome. J Pediatr. 1981;98:112–117. doi: 10.1016/s0022-3476(81)80555-0. [DOI] [PubMed] [Google Scholar]
- 3.Ergander U, Eriksson M, Zetterstrom R. Severe neonatal asphyxia. Incidence and prediction of outcome in the Stockholm area. Acta Paediatr. 1983;72:321–325. doi: 10.1111/j.1651-2227.1983.tb09722.x. [DOI] [PubMed] [Google Scholar]
- 4.Levene ML, Kornberg J, Williams THC. The incidence and severity of post-asphyxial encephalopathy in full-term infants. Early Hum Develop. 1985;11:21–26. doi: 10.1016/0378-3782(85)90115-x. [DOI] [PubMed] [Google Scholar]
- 5.Hull J, Dodd KL. Falling incidence of hypoxic-ischaemic encephalopathy in term infants. Br J Obstet Gynaecol. 1992;99:386–391. doi: 10.1111/j.1471-0528.1992.tb13754.x. [DOI] [PubMed] [Google Scholar]
- 6.Thornberg E, Thiringer K, Odeback A, Milsom I. Birth asphyxia: incidence, clinical course and outcome in a Swedish population. Acta Paediatr. 1995;84:927–932. doi: 10.1111/j.1651-2227.1995.tb13794.x. [DOI] [PubMed] [Google Scholar]
- 7.Sarnat HB, Sarnat MS. Neonatal encephalopathy following fetal distress. Arch Neurol. 1976;33:696–705. doi: 10.1001/archneur.1976.00500100030012. [DOI] [PubMed] [Google Scholar]
- 8.Badawi N, Kurinczuk JJ, Keogh JM, Alessandri LM, O’Sullivan F, Burton PR, et al. Antepartum risk factors for newborn encephalopathy: the Western Australian case-control study. BMJ. 1998;317:1549–1553. doi: 10.1136/bmj.317.7172.1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Committee on Fetus and Newborn; American Academy of Paediatrics; Committee on Obstetric Practice; American College of Obstetricians and Gynecologists. Use and abuse of the Apgar score. Pediatrics. 1996;98:141–142. [PubMed] [Google Scholar]
- 10.Berg AT. Indices of fetal growth retardation, perinatal hypoxia-related factors and childhood neurological morbidity. Early Hum Dev. 1989;19:271–283. doi: 10.1016/0378-3782(89)90062-5. [DOI] [PubMed] [Google Scholar]
- 11.Spencer JAD, Badawi N, Burton PR, Keogh JM, Pemberton PJ, Stanley FJ. The intrapartum CTG prior to neonatal encephalopathy at term: a case control study. Br J Obstet Gynaecol. 1997;104:25–28. doi: 10.1111/j.1471-0528.1997.tb10643.x. [DOI] [PubMed] [Google Scholar]
- 12.Adamson SJ, Alessandri LM, Badawi N, Burton PR, Pemberton PJ, Stanley FJ. Predictors of neonatal encephalopathy in full term infants. BMJ. 1995;311:598–602. doi: 10.1136/bmj.311.7005.598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grether JK, Nelson KB. Maternal infection and cerebral palsy in infants of normal birth weight. JAMA. 1997;278:207–211. [PubMed] [Google Scholar]
- 14.Murphy DJ, Hope PL, Johnson A. Neonatal risk factors for cerebral palsy in very preterm babies: case-control study. BMJ. 1997;314:404–408. doi: 10.1136/bmj.314.7078.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leviton A. Preterm birth and cerebral palsy: is tumour necrosis factor the missing link? Dev Med Child Neurol. 1993;35:553–558. doi: 10.1111/j.1469-8749.1993.tb11688.x. [DOI] [PubMed] [Google Scholar]
- 16.Gee V. Perinatal statistics in Western Australia: 12th Annual Report of the Western Australian Midwives Notification System for 1994. Perth: Health Department of Western Australia; 1995. [Google Scholar]
- 17.Ziegler AL, Calame A, Marchand C, Passera M, Reymond-Goni I, Prod’Hom LS. Cerebral distress in full-term newborns and its prognostic value. A follow-up study of 90 infants. Helvetica Paediatrica Acta. 1976;31:299–317. [PubMed] [Google Scholar]
- 18.De Souza SW, Richards B. Neurological sequelae in newborn babies after perinatal asphyxia. Arch Dis Child. 1978;53:564–569. doi: 10.1136/adc.53.7.564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van Ham MAPC, van Dongen PWJ, Mulder J. Maternal consequences of caesarean section. A retrospective study of intra-operative and post-operative maternal complications of caesarean section during a 10 year period. Eur J Obstet Gynecol Reprod Biol. 1997;74:1–6. doi: 10.1016/s0301-2115(97)02725-5. [DOI] [PubMed] [Google Scholar]
- 20.Lumley J, Lester A, Renou P, Wood C. A failed RCT to determine the best method of delivery for very low birth weight infants. Cont Clin Trials. 1985;6:120–127. doi: 10.1016/0197-2456(85)90117-5. [DOI] [PubMed] [Google Scholar]