Abstract
Nonalcoholic fatty liver disease is increasingly regarded as a hepatic manifestation of metabolic syndrome, and the severity of nonalcoholic fatty liver disease seems to increase in parallel with other features of metabolic syndrome. Excess lipid accumulation in the liver cells is not only a mediator of Metabolic Syndrome and indicator of a lipid overload but also accompanied by a range of histological alterations varying from 'simple' steatosis to nonalcoholic steatohepatitis, with time progressing to manifest cirrhosis. Hepatocellular carcinoma may also occur in nonalcoholic steatohepatitis -related cirrhosis with a mortality rate similar to or worse than for cirrhosis associated with hepatitis C. This review summarizes the knowledge about the causal relationship between hepatic fat accumulation, insulin resistance, liver damage and the etiological role of hepatic fat accumulation in pathogenesis of extra- and intra-hepatic manifestations. Special emphasis is given suggestions of new targets treatment and prevention of nonalcoholic fatty liver disease.
Introduction
Nonalcoholic fatty liver disease (NAFLD), no more than 15 years ago considered as rare, has now reached epidemic propertions in China and has a major clinical and research priority [1]. It is only since a decade or so that nonalcoholic fatty liver disease is considered to be a manifestations of insulin resistance[2,3]. The fact that insulin resistance and compensatory hyperinsulinaemia have central etiologic roles in the development of both metabolic syndrome and NAFLD makes the excessive accumulation of triglycerides (TG) in the liver especially interesing [4]. The severity of NAFLD increases in parallel with other features of the metabolic syndrome, supporting that NAFLD is its hepatic manifestation [5].
Although current therapy presently is limited to suggestions of lifestyle changes and control of associated metabolic disorders, experimental studies and clinical observations do suggest also other modalities of treatment. As an example, a proof-of-concept study suggest that administration of pioglitazone improvements in both metabolic and histological manifestations of disease in subjects with nonalcoholic steatohepatitis[6].
NAFLD has the potential to progress through the inflammatory phase of nonalcoholic steatohepatitis (NASH) to fibrosis, cirrhosis (20%), and in some cases (9%) to liver failure or hepatocellular carcinoma (HCC) (1%) [7,8]. The reasons why some patients develop advanced disease while others have non- och less progressive liver disease are not fully understood. The mechanism of liver injury in NAFLD/NASH is suggested to be a 'two hit phenomenon' where the 'first hit' consists in inflammation and development of steatosis, which sensitizes the liver to a variety of 'second hits' lead to fibrosis [7,9]. It is also increasingly recognized that fat-induced insulin resistance in the liver causes activation of proinflammatory pathways, which will lead to modification of this 'two hit' process.
Identifying patients at risk for transition from hepatic steatosis to NASH and fibrosis with noninvasive techniques are the great challenges in hepatology [9]. Therefore, combining of the hepatologist's knowledge of human hepatic pathology and pathophysiology with the endocrinologist's knowledge of insulin signaling and the regulation of glucose and lipid metabolism in the liver will help to better understand the process, and hopefully also, help to find new targets for the treatment and prevention of NAFLD.
The causal relationship between hepatic fat accumulation and insulin resistance
Hepatocellular steatosis is the hallmark of NAFLD. The histological criterion for the diagnosis of NAFLD is the presence of fat in more than 5% of the hepatocytes. The accumulation of fat usually starts in zone 3 and will in more severe cases may occupy whole acinus[10-12]. The lipid droplets in liver consist mainly in triglycerides. The contribution of different non-esterified fatty acids (NEFA) sources to hepatic triglycerides parallel to the VLDL triglycerides, includes: circulating NEFA pool contributed 81% of hepatic and VLDL triglycerides in fasting conditions and 61% postprandially, dietary NEFA pool contributed 10% in fasting conditions and 26% postprandially, whereas de novo fatty acid(DNL) contributed 7% in fasting and 9% postprandially[13](Fig 1).
Figure 1.
Sources of fatty acids stored in liver and secreted via lipoproteins in patients with nonalcoholic fatty liver disease (Kerry L. Donnelly, et al, J. Clin. Invest. 2005;115:1343-1351).
Insulin resistance is defined as an inadequate response to the physiologic effects of circulating insulin in specific target tissues, such as skeletal muscle, liver, and adipose tissue,. The subjects with impaired glucose tolerance (IGT) demonstrate a marked muscle insulin resistance but only mild hepatic insulin resistance. Subjects with impaired fasting glucose (IFG), however, demonstrate severe hepatic insulin resistance but normal or near-normal muscle insulin sensitivity[14]. Epidemiological studies demonstrate that the two categories constitute two distinct populations, which only partially overlap, suggesting that IGT and IFG represent two distinctly different metabolic abnormalities [15]. However, it must be regarded as undisputable, that a strong association exists between insulin resistance and excess lipid accumulation in nonadipose tissues, particularly muscle and liver.
Although an association between NAFLD and insulin resistance is well accepted, it remains unclear whether insulin resistance causes the excessive accumulation of TG in liver, or it is the increase in TG itself or of its metabolite intermediates that plays the most causal role in the development of hepatic or systemic insulin resistence [16]. Some investigators postulate that liver fat accumulation is a result, rather than cause, of peripheral insulin resistance in obesity. In skeletal muscle, peripheral IR will primarily affect a large portion of the total glucose uptake (>80-90%), while in adipose tissue, insulin resistance will induce an impaired anti-lipolytic action of insulin and increased release of NEFA [17,18]. Elevated plasma concentrations of glucose and fatty acids may promote hepatic fatty acid and triglyceride uptake and synthesis and impair β-oxidation [19]. As a result, an accumulation of triglycerides in the liver will occurs, leading to hepatic steatosis. The proposed mechanism for insulin resistance leading to diabetes is thus: IR in skeletal muscle → peripheral and portal vein hyperinsulinemia → hepatic steatosis → hepatic IR → DM2.
However, several observations indicate that steatosis can be caused also by intra-hepatic alterations in glucose and fat metabolism, which are independent of extrahepatic conditions[20,21]. Three consecutive days of feeding a high fat diet is known, also in the absence of significant peripheral fat accumulation to cause hepatic fat accumulation and hepatic insulin resistance and this prior to the development of peripheral insulin resistence[22]. This study demonstrated that short term fat feeding will cause a 3-fold increase in liver and fatty acyl-CoA content, but not alter fasting plasma glucose concentration and the basal rate of endogenous glucose production (EGP), indicating that hepatic fat accumulation from dietary NEFA pool is not necessarily associated with insulin resistance[23].
Decreased insulin clearance has also been suggested as another pathway for hyperinsulinemia in liver. Insulin clearance is decreased in advanced liver disease, which is regarded as one of the main causes of hyperinsulinemia in iver cirrhosis [24]. The first organ to be impacted following insulin secretion is the liver, where a substantial proportion of secreted insulin is cleared via receptor mediated process [25,26], estimated in dogs to be app 50% [27,28] and in humans 40-80% [25,29-32]. Both hepatic insulin sensitivity and whole body insulin clearance were in this study measured directly by the euglycemic hyperinsulinemic insulin clamp technique and liver fat measured by proton magnetic resonance spectroscopy in a group of nondiabetic subjects. The content of liver fat correlated significantly with impaired clearance of insulin (r = 0.43, P < 0.0001) and with hepatic insulin sensitivity (r = -0.40, P = 0.0002) [33,34]. The extent to which hepatic fat accumulation and impaired insulin clearance contribute to hyperinsulinemia can not yet be regarded as fully understood.
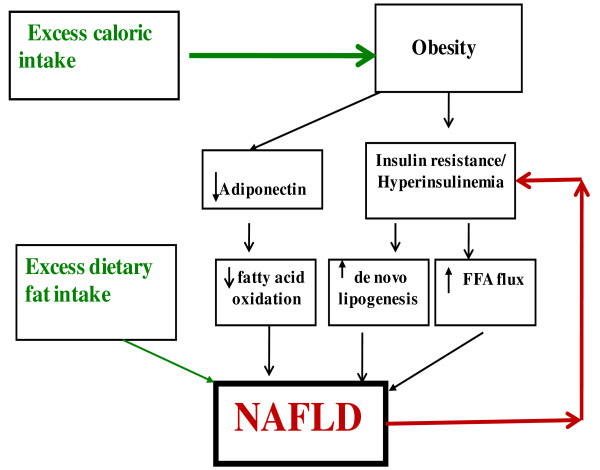
As discussed above (Fig 2), the peripheral insulin resistance could well contribute to a causal role for hepatic steatosis, but NAFLD and hepatic insulin resistance is also regarded as a primary cause of of T2 MD.
Figure 2.
Diagram of potential sources of and mechanisms for the accumulation of fat in the liver. Excess caloric intake plays a central role for inducing obesity and thus contributing to insulin resistance. Obesity may additionally impact fat accumulation in the liver by decreasing adiponectin levels and insulin resistance contributes to NAFLD directly by increasing de novo lipogenesis and indirectly by increasing FFA flux to the liver via decreased inhibition of lipolysis. In addition, excess dietary fat intake directly could also contribute to a causal role in hepatic steatosis(modified from Kristina M. The Journal of Clinical Endocrinology & Metabolism 2006; 91: 4753-4761).
The symptoms of NAFLD vary considerably from person to person, as some individuals may have few or no noticeable symptoms until they are incidentally diagnosed by elevated levels of aminotransferase and by ultrasound. Other individuals will present with extremely high levels of hyperglycemia and classical symptoms of diabetes such as thirst, frequent urination, and weight loss.
The accumulation of triglycerides in liver is not equal to increased liver damage
Minimal histopathology criteria are used for diagnosis of NAFLD. Assessment of steatosis with reproducible semiquantitative methods use a three-stage scale to evaluate the percentage of liver parenchyma occupied by steatotic hepatocytes: I. 0-33% (or 0-5%, 5-33%), II 33-66%and III more than 66%[12]. Although hepatic steatosis is a key component of steatohepatitis, it is not known if patients with greater amounts of steatosis are more likely to develop steatohepatitis than those with mild steatosis. The histological definition of steatohepatitis does not require a particular amount of steatosis, and, steatosis will often decrease and may even be completely absent in cases with advanced fibrosis and cirrhosis [11,35].
Several findings suggest that hepatic triglycerides per se are not toxic and may, in fact, even protect the liver from lipotoxicity by buffering the accumulation of fatty acid[36,37]. Yamaguchi et al [38] demonstrated that inhibition of TG synthesis (mediated through the reduction in DGAT2 activity) will improve liver steatosis, but at a price of increased liver damage. Levels of hepatic fatty acids, cytochrome P450, and markers of lipid peroxidation and oxidant stress, as well as fibrosis, were in this study all markedly increased, Recent findings confirm that the ability to synthesize triglycerides may, in fact, be protective in obesity. When hepatocyte triglyceride synthesis is inhibited, free fatty acids will accumulate in the liver, and swtimulate oxidizing systems that increase hepatic oxidative stress and liver damage[39,40]. Furthermore, feeding an n-3 PUFA-enriched diet failed to prevent lipotoxic hepatocellular injury and inflammatory recruitment, although activated PPAR alpha and suppressed hepatic de novo lipogenesis[39].
The differential toxicity of various FAs is relate directly to its ability to promote triglyceride accumulation[39]. The exogenous or endogenous generated unsaturated FAs will reduce palmitate-induced apoptosis by promoting palmitate incorporation into triglycerides. Moreover, oleic acid, as well as palmitic acid, is toxic to cells with impaired capacity to synthesize triglycerides. Exposure of human hepatocytes to monounsaturated fatty acids (MUFAs) results in lipid accumulation without any changes in cell viability. In contrast, cells incubated with saturated fatty acids (SFAs) decrease significantly their viability in addition yo increasing their caspase activation and degree of apoptosis, parallel to only minor lipid droplet accumulation[39].
Stearoyl-CoA desaturase-1 (SCD-1), the enzyme that converts SFA to MUFA, appears to provide an important metabolic control mechanism in the biochemistry and physiology of lipid metabolism. Genetic or pharmacological inhibition of SCD1, sensitizes hepatic cells to SFA-induced apoptosis. SCD1-/- mice on the MCD diet demonstrate decreased steatosis and markedly increased hepatocellular apoptosis, liver injury, and fibrosis compared to SCD1+/+ mice, whereas feeding MUFA prevents the MCD-induced injury[41].
The studies referred to above clearly show that increased serum free fatty acid, rather than the excess lipid accumulation in liver cells serves as a parameter of degree of liver damage, and might be considered as a future target for preventing and therapy of steatohepatitis in patients with NAFLD. Findings that inhibition of the expression of SCD-1 might also be beneficial in the treatment of obesity, diabetes, and other metabolic diseases [42-45].
However, it is still quite possible that under the conditions of enhanced TG synthesis, the capacity will be insufficient to buffer detoxifying of excess fatty acids. Liver damage could then occur as a result of fatty acid-induced lipotoxicity and/or of a combination of both lipotoxicity and severe steatosis. A recent study shows that the severity of steatosis in NAFLD on histopathology is positively associated with lobular inflammation, zone 3 fibrosis and definite steatohepatitis, suggesting that NAFLD patients with severe steatosis (affecting >66% of liver parenchyma) are most likely to have NASH [46]. We currently mainly relying on liver biopsies to confirm the diagnosis and indicate prognosis, as this far hepatic ultrasound and serum transaminases are of limited value in estimation of hepatic inflammation and fibrosis, However, ultrasonography is still by far the most common method of diagnosing NAFLD in clinical practice, especially as it has a very good sensitivity and specificity in detecting severe steatosis(>33% fat on liver biopsy), although the sensitivity of ultrasonography is not satisfactory, particularly when hepatic fat infiltration is above 33% [47,48]. The positive relationship between the severity of steatosis and other elements of NASH (i.e. inflammation, ballooning, and fibrosis) provides noninvasive techniques to identify patients at risk for transition from hepatic steatosis to NASH and fibrosis. However, we are still unable to determine if patients with severe steatosis do faster progress to full blown steatohepatitis than those with milder forms of steatosis.
Fat-induced activation of chronic SIRS and NASH in the progression of NAFLD
NAFLD is a liver disease with a wide histological spectrum ranging from 'simple' steatosis with a generally benign course to nonalcoholic steatohepatitis (NASH), which usually is a more progressive form of the disease [11]. Progressive fibrosis occurs in 10-15% of patients with NASH and cirrhosis may develop in 15-25% of the cases [49,50]. Once developed, 30% to 40% of these patients succumb a liver-related death over a 10-year period [51,52], a mortality rate similar to[53,54] or worse than cirrhosis associated with hepatitis C. NASH-associated cirrhosis can also develop into into a subacute liver failure, or progress to hepatocellular cancer [55], as well as reoccur after liver transplantation.
The reasons why some patients develop advanced disease, while others have indolent liver disease, are not fully understood. The mechanism of liver injury in NAFLD/NASH is thought to follow, as mentioned above, a 'two hit pathway during which the steatosis sensitizes the liver to a variety of second hits, which lead to fibrosis and inflammation[7]. The 'first hit', hepatic triglyceride accumulation, or steatosis, increases the susceptibility of the liver to injury- mediated 'second hits'-changes, such as inflammatory cytokines/adipokines, mitochondrial dysfunction and oxidative stress, which in turn promote the development to steatohepatitis and/or fibrosis [9,56]. There is an increasing recognition of the fact that fat-induced insulin resistance causes activation of proinflammatory pathways in the liver, which with time might lead to modification of the theory.
Most studies on the role of hepatic innate immunity in NAFLD has been generated by studying leptin-deficient (ob/ob) mice and leptin-resistant (fa/fa) rats, animals, which spontaneously develop fatty livers and naturally exhibit features, such as insulin resistance, obesity, and dyslipidemia, which in its turn in humans are strongly correlated with NAFLD [57-60]. It is increasingly documented that obesity without simultaneous inflammation does not result in peripheral insulin resistance, and similarly, the steatosis will not lead to liver inflammation (NASH) and/or hepatic insulin resistance [57]. Wild type mice fed a high-fat diet, will normally develop obesity with simultaneous inflammation, insulin resistance and mild Type 2 diabetes. On the contrast, chimerical mice, lacking immune cells will become obese, but have a striking absence of insulin resistance. In addition, their livers will remain normal [61-63]. Among the proinflammatory molecules, TNF-α has been proposed to be the key link between obesity and insulin resistance. TNF-α is usually over- expressed in adipose tissues of obese animals and humans, and obese mice lacking TNF-α and/or its receptor demonstrate protection against development of insulin resistance[64,65].
To date, many lines of evidence seem to show that in humans chronic activation of proinflammatory pathways of insulin targetted cells can result in obesity/steatosis -related insulin resistance. The influence of circulating and hepatic levels of proinflammatory cytokines TNF-α, IL-6, and C-reactive protein (CRP) in patients with NAFLD and their correlation with disease severity are well studied. Patients with NASH have generally significantly higher levels of serum TNF-α and IL-6 than seen in patients with simple steatosis. NASH is, when compared to simple steatosis, associated with higher levels of soluble TNF receptor 1 (sTNFR1) and soluble IL-6 receptor (sIL-6R) [66,67]. In addition, the expression is higher in those patients with more severe NASH. The findings that inflammation and insulin resistance often seem to occur in parallel and to reinforce each other via positive feedback mechanisms, suggesting that disruption of the interface between inflammatory and metabolic pathways is central in the pathogenesis and progression (second hit) of NAFLD and also increase the risk of development of insulin resistance (Type 2 diabetes). Given the role of TNF-α in inducing both necroinflammation and IR, anti-TNF agents have been considered for treatment of NASH. Reducing TNF-α signaling either by TNF-α knocking out mechanisms or by infusion of blocking antibodies reduces insulin resistance in obese rodents [68]. Pentoxifylline, a TNF-α inhibitor, has also been used for the same purpose in patients with NASH. Two smaller studies in NASH patients report significant improvements in AST and ALT and also significant improvement in insulin resistant after pentoxyfylline treatment [69,70], supporting the hypothesis that anti-inflammatory treatments have favorable effects on NASH. However, TNF-α antibody treatment will not alter insulin sensitivity in humans [71]. Attempts in this study to over a period of 4 weeks neutralize TNF-alpha with an engineered human anti-TNF-alpha antibody (CDP571) had no effect on insulin sensitivity in obese non-insulin-dependent diabetes subjects with rheumatic diseases.
Fat can cause insulin resistance by prompting the activation of select serine kinases within a variety of insulin sensitive cells. The three serine kinases most strongly implicated in the pathogenesis of fat-induced insulin resistance are Jun N-terminal kinase (JNK), inhibitor of nuclear factor κB (NF-κB) kinase(IKK), and novel isoforms of protein kinase C (PKC) [72-74]. These enzymes will, alone or in combination, phosphorylate regulatory serine residues on the insulin receptor substrates IRS-1 and IRS-2, leading to the downmodulation of normal insulin-stimulated tyrosine phosphorylation and interfering with physiologic insulin [57]. Among these, JNK and IKK are significantly effective proinflammatory signaling molecules. IKK and JNK cause inflammation by promoting formation of the transcription factors AP-1 and NF-κB, which activate transcription of a multitude of proinflammatory genes, cytokines, chemokines, and cell adhesion molecules[75]. A causal connection between fat-related activation of serine kinases and insulin resistance has been demonstrated in adipose tissue [76] and muscle [77] as well as liver [78-81]. Mice heterozygous for IKKβ are protected against the negative effects of a high-fat diet-associated obesity as well as development of insulin resistance [82]. Silencing of IKKβ will also prevent TNF-alpha-induced impairments in the action of insulin on Akt phosphorylation and glucose uptake in primary human skeletal muscle myotubes from non-diabetic subjects [83,84].
Also, fatty acids and high-fat feeding can, even in the absence of obesity or systemic insulin resistance, directly induce inflammatory signaling through mammalian toll-like receptors (TLRs) in the liver [85,86]. TLRs are cellular pattern-recognizing receptors (PRRs) that recognize the molecular patterns of pathogens, such as Gram-negative endotoxin. After engaging the pathogenic patterned ligands via a receptor-driven signaling cascade do they activate the transcription factor NF-κB, resulting in increased expression of proinflammatory cytokines, which in its turn trigger inflammation. Such rapid, innate cellular responses serve as the first line of host defense against infection by pathogens. Increasing evidence suggests that TLRs also recognize host-derived ligands and interact with these endogenous ligands, generating tissue injury and cell death [87]. Thus TLRs will act as PRRs that paralle with the lipotoxicity and stress of endoplasmic reticulumt, use signaling mechanisms to solicit inflammation and fat-induced insulin resistance (Fig 3). Such efforts should also reveal a wealth of potential targets for interventions and drug development that prevent NASH[88]. Probiotics, which reportedly suppress TLR-related responses by altering the intestinal flora [89,90], reduce inflammation and improve the liver in animals and humans with fatty livers[91,92]. Similarly, dietary n-3 polyunsaturated fatty acids, which are known inhibitors of TLR signaling[93], will have the capacity to suppress necro-inflammation and fibrosis in experimental fatty liver disease[94].
Figure 3.
Activation of inflammatory signaling pathways by fat(Hepatology. 2008;48:670-8).
FoxO1 is a forkhead transcriptional factor that acts to mediate insulin action on target gene expression in peripheral cells [95-97]. More recent studies show that FoxO1 signaling through NF-kB plays a significant role in proinflammatory cytokine production and insulin resistance (Fig 4). FoxO1 stimulate selectively macrophage production of IL-1β, but not IL-6, TNFα, and IFN-γ.
Figure 4.
Convergence of the FoxO1 and NFκB pathways in IL-1β gene expression: FoxO1 targets at the IRE DNA motif of the IL-1β promoter for trans-activation. This effect along with the activation of the NFκB pathways synergistically promotes macrophage production of proinflammatory cytokine IL-1β. (Dongming Su et al. FoxO1 Links Insulin Resistance to Proinflammatory Cytokine IL-1beta Production in Macrophages. in Press).
FoxO1 is known to mediate the inhibitory effect of insulin on target gene expression. In the absence of insulin, FoxO1 acts in the nucleus as an enhancer of target gene expression, whereas in the presence of insulin, FoxO1, phosphorylated by Akt/PKB, will contribute to inhibition of target gene expression. The phosphorylation-dependent protein trafficking mechanism is crucial for the regulation of FoxO1 transcriptional activity within cells [98-100]. The IL-1β promoter contains sites for both FoxO1 and NFkB target that are juxtapositioned within the promoter-proximal region of the Il1b gene in mice, rats and humans, implying evolutionally conserved mechanisms or FoxO1 signaling through the NFkB pathway in regulation of proinflammatory cytokines. Amelioration of insulin resistance with blockage of IL-1β signaling via its receptor antagonist is associated with improving diabetes [101].
Conclusion
The molecular mechanisms underlying NAFLD and treatment options are this far poorly understood. Clearly, numerous factors are associated with increased activation of hepatic innate immune system, which is central to the development of fat-related insulin resistance and also plays an important role in fat-related liver damage (NASH). NASH is seemingly a much multifactorial condition with some pathological end points such as increased hepatic oxidative stress, increased hepatic cytokine expression, direct "lipotoxicity" of excess circulating NEFAs and insulin resistance. Especilly are the serine kinases key factors in the development of insulin resistance within hepatocytes and in other insulin sensitive cells. Especially IKK and JNK, are important components what is described as the two major proinflammatory pathways.
Future exploration of the signaling routes from fat to NF-κB might provide information about hitherto unknown etiological factors behind chronic diseases in addition to those already known. It might also provide information about potentially new targets for drug development and treatment of these diseases.
Abbreviations
BMI: body mass index; NAFLD: nonalcoholic fatty liver disease; NASH: nonalcoholic steatohepatitis; DNL: de novo lipogenesis; NEFA: non-esterified fatty acids; LDL: very low density lipoproteins; TG: triglycerides; CVD: cardiovascular disease; IFG: impaired fasting glucose; IGT: impaired glucose tolerance; SCD1: stearoyl-CoA desaturase-1; IR: insulin resistance; DM2: diabetes Mellitus Type 2; CRP: C-reactive protein; IL-6: interleukin-6; sTNFR1: TNF receptor 1; sIL-6R: soluble IL-6 receptor; TLRs: Toll-like receptors; RAGE: receptor for advanced glycation end products; SIRS: systemic inflammatory response syndrome; JNK: Jun N-terminal kinase; NF-κB: nuclear factor κB; IKK: IκB kinase; PKC: protein kinase C.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
QL, SB and SQ conceived the study, its design and drafted the manuscript. All authors read and approved the final manuscript.
Contributor Information
Qing Liu, Email: liuqing777@gmail.com.
Stig Bengmark, Email: s.bengmark@ucl.ac.uk.
Shen Qu, Email: qushencn@hotmail.com.
References
- Farrell GC, Chitturi S, Lau GK, Sollano JD. Asia-Pacific Working Party on NAFLD. Guidelines for the assessment and management of non-alcoholic fatty liver disease in the Asia-Pacific region: executive summary. J Gastroenterol Hepatol. 2007;22:775–7. doi: 10.1111/j.1440-1746.2007.05002.x. [DOI] [PubMed] [Google Scholar]
- Adams LA, Angulo P. Recent concepts in non-alcoholic fattyliver disease. Diabet Med. 2005;22:1129–1133. doi: 10.1111/j.1464-5491.2005.01748.x. [DOI] [PubMed] [Google Scholar]
- Raman M, Allard J. Non alcoholic fatty liver disease: a clinical approach and review. Can J Gastroenterol. 2006;20:345–9. doi: 10.1155/2006/918262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan JG. Impact of non-alcoholic fatty liver disease on accelerated metabolic complications. J Dig Dis. 2008;9:63–7. doi: 10.1111/j.1751-2980.2008.00323.x. [DOI] [PubMed] [Google Scholar]
- Boppidi H, Daram SR. Nonalcoholic fatty liver disease: hepatic manifestation of obesity and the metabolic syndrome. Postgrad Med. 2008;120:E01–7. doi: 10.3810/pgm.2008.07.1800. [DOI] [PubMed] [Google Scholar]
- Belfort R, Harrison SA, Brown K, Darland C, Finch J, Hardies J, Balas B, Gastaldelli A, Tio F, Pulcini J, Berria R, Ma JZ, Dwivedi S, Havranek R, Fincke C, DeFronzo R, Bannayan GA, Schenker S, Cusi K. A placebo-controlled trial of pioglitazone in subjects with nonalcoholic steatohepatitis. N Engl J Med. 2006;355:2297–307. doi: 10.1056/NEJMoa060326. [DOI] [PubMed] [Google Scholar]
- Chávez-Tapia NN, Uribe M, Ponciano-Rodríguez G, Medina-Santillán R, Méndez-Sánchez N. New insights into the pathophysiology of nonalcoholic fatty liver disease. Ann Hepatol. 2009;8:S9–S17. [PubMed] [Google Scholar]
- Abrams GA, Kunde SS, Lazenby AJ, Clements RH. Portal fibrosis and hepatic steatosis in morbidly obese subjects: a spectrum of nonalcoholic fatty liver disease. Hepatology. 2004;40:475–83. doi: 10.1002/hep.20323. [DOI] [PubMed] [Google Scholar]
- Chavez-Tapia NC, Tiribelli C. Are non-invasive tests accurate enough to predict hepatic fibrosis in non-alcoholic fatty liver disease (NAFLD)? Gut. 2008;57:1351–3. doi: 10.1136/gut.2008.154435. [DOI] [PubMed] [Google Scholar]
- Brunt EM. Nonalcoholic steatohepatitis: pathologic features and differential diagnosis. Semin Diagn Pathol. 2005;22:330–338. doi: 10.1053/j.semdp.2006.04.002. [DOI] [PubMed] [Google Scholar]
- Yeh MM, Brunt EM. Pathology of nonalcoholic fatty liver disease. Am J Clin Pathol. 2007;128:837–847. doi: 10.1309/RTPM1PY6YGBL2G2R. [DOI] [PubMed] [Google Scholar]
- Tiniakos DG. Nonalcoholic fatty liverdisease/nonalcoholic steatohepatitis: Histological diagnostic criteria and scoring systems. European Journal of Gastroenterology & Hepatology. 2009;00 doi: 10.1097/MEG.0b013e32832ca0cb. [DOI] [PubMed] [Google Scholar]
- Donnelly KL, Smith CI, Schwarzenberg SJ, Jessurun J, Boldt MD, Parks EJ. Sources of fatty acids stored in liver and secreted via lipoproteins in patients with nonalcoholic fatty liver disease. J Clin Invest. 2005;115:1343–1351. doi: 10.1172/JCI23621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abdul-Ghani MA, Tripathy D, DeFronzo RA. Contributions of beta-cell dysfunction and insulin resistance to the pathogenesis of impaired glucose tolerance and impaired fasting glucose. Diabetes Care. 2006;29:1130–9. doi: 10.2337/dc05-2179. [DOI] [PubMed] [Google Scholar]
- Hanefeld M, Koehler C, Fuecker K, Henkel E, Schaper F, Temelkova-Kurktschiev T. Impaired Glucose Tolerance for Atherosclerosis and Diabetes study. Insulin secretion and insulin sensitivity pattern is different in isolated impaired glucose tolerance and impaired fasting glucose: the risk factor in Impaired Glucose Tolerance for Atherosclerosis and Diabetes study. Diabetes Care. 2003;26:868–74. doi: 10.2337/diacare.26.3.868. [DOI] [PubMed] [Google Scholar]
- Postic C, Girard J. The role of the lipogenic pathway in the development of hepatic steatosis. Diabetes & Metabolism. 2008;34:643–648. doi: 10.1016/S1262-3636(08)74599-3. [DOI] [PubMed] [Google Scholar]
- Koch L, Wunderlich FT, Seibler J, Könner AC, Hampel B, Irlenbusch Brabant G, Kahn CR, Schwenk F, Brüning JC. Central insulin action regulates peripheral glucose and fat metabolism in mice. J Clin Invest. 2008;118:2132–47. doi: 10.1172/JCI31073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blüher M, Michael MD, Peroni OD, Ueki K, Carter N, Kahn BB, Kahn CR. Adipose tissue selective insulin receptor knockout protects against obesity and obesity-related glucose intolerance. Dev Cell. 2002;3:25–38. doi: 10.1016/S1534-5807(02)00199-5. [DOI] [PubMed] [Google Scholar]
- Reddy JK, Rao MS. Lipid Metabolism and Liver Inflammation. II. Fatty liver disease and fatty acid oxidation. Am J Physiol Gastrointest Liver Physiol. 2006;290:G852–G858. doi: 10.1152/ajpgi.00521.2005. [DOI] [PubMed] [Google Scholar]
- den Boer M, Voshol PJ, Kuipers F, Havekes LM, Romijn JA. Hepatic steatosis: a mediator of the metabolic syndrome. Lessons from animal models. Arterioscler Thromb Vasc Biol. 2004;24:644–9. doi: 10.1161/01.ATV.0000116217.57583.6e. [DOI] [PubMed] [Google Scholar]
- Schonfeld G, Yue P, Lin X, Chen Z. Fatty liver and insulin resistance: not always linked. Trans Am Clin Climatol Assoc. 2008;119:217–23. [PMC free article] [PubMed] [Google Scholar]
- Samuel VT, Liu ZX, Qu X, Elder BD, Bilz S, Befroy D, Romanelli AJ, Shulman GI. Mechanism of hepatic insulin resistance in non-alcoholic fatty liver disease. Biol Chem. 2004;279:32345–53. doi: 10.1074/jbc.M313478200. [DOI] [PubMed] [Google Scholar]
- Saito T, Misawa K, Kawata S1. Fatty liver and non-alcoholic steatohepatitis. Intern Med. 2007;46:101–3. doi: 10.2169/internalmedicine.46.1784. [DOI] [PubMed] [Google Scholar]
- Duckworth WC, Bennett RG, Hamel FG. Insulin degradation: progress and potential. Endocr Rev. 1998;19:608–624. doi: 10.1210/er.19.5.608. [DOI] [PubMed] [Google Scholar]
- Meier JJ, Veldhuis JD, Butler PC. Pulsatile insulin secretion dictates systemic insulin delivery by regulating hepatic insulin extraction in humans. Diabetes. 2005;54:1649–56. doi: 10.2337/diabetes.54.6.1649. [DOI] [PubMed] [Google Scholar]
- Field JB. Extraction of insulin by liver. Annu Rev Med. 1973;24:309–314. doi: 10.1146/annurev.me.24.020173.001521. [DOI] [PubMed] [Google Scholar]
- Polonsky K, Jaspan J, Emmanouel D. Differences in the hepatic and renal extraction of insulin and glucagon in the dog: evidence for saturability of insulin metabolism. Acta Endocrinol. 1983;102:420–427. doi: 10.1530/acta.0.1020420. [DOI] [PubMed] [Google Scholar]
- Kaden M, Harding P, Field JB. Effect of intraduodenal glucose administration on hepatic extraction of insulin in the anesthetized dog. J Clin Invest. 1973;52:2016–2028. doi: 10.1172/JCI107386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meistas MT, Rendell M, Margolis S, Kowarski AA. Estimation of the secretion rate of insulin from the urinary excretion rate of C-peptide: study in obese and diabetic subjects. Diabetes. 1982;31:449–453. doi: 10.2337/diabetes.31.5.449. [DOI] [PubMed] [Google Scholar]
- Eaton RP, Allen RC, Schade DS. Hepatic removal of insulin in normal man:dose response to endogenous insulin secretion. J Clin Endocrinol Metab. 1983;56:1294–1300. doi: 10.1210/jcem-56-6-1294. [DOI] [PubMed] [Google Scholar]
- Waldhäusl W, Bratusch-Marrain P, Gasic S, Korn A, Nowotny P. Insulinproduction rate following glucose ingestion estimated by splanchnic C-peptide output in normal man. Diabetologia. 1979;17:221–227. doi: 10.1007/BF01235858. [DOI] [PubMed] [Google Scholar]
- Polonsky KS, Rubenstein AH. C-peptide as a measure of the secretion and hepatic extraction of insulin: pitfalls and limitations. Diabetes. 1984;33:486–494. doi: 10.2337/diabetes.33.5.486. [DOI] [PubMed] [Google Scholar]
- Kotronen A, Vehkavaara S, Seppälä-Lindroos A, Bergholm R, Yki-Järvinen H. Effect of liver fat on insulin clearance. Am J Physiol Endocrinol Metab. 2007;293:E1709–15. doi: 10.1152/ajpendo.00444.2007. [DOI] [PubMed] [Google Scholar]
- Kotronen A, Juurinen L, Tiikkainen M, Vehkavaara S, Yki-Järvinen H. Increased liver fat, impaired insulin clearance, and hepatic and adipose tissue insulin resistance in type 2 diabetes. Gastroenterology. 2008;135:122–30. doi: 10.1053/j.gastro.2008.03.021. [DOI] [PubMed] [Google Scholar]
- Chalasani N, Wilson L, Kleiner DE, Cummings OW, Brunt EM, Unalp A. NASH Clinical Research Network. Relationship of steatosis grade and zonal location to histological features of steatohepatitis in adult patients with non-alcoholic fatty liver disease. J Hepatol. 2008;48:829–834. doi: 10.1016/j.jhep.2008.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Postic C, Girard J. Contribution of de novo fatty acid synthesis to hepatic steatosis and insulin resistance: lessons from genetically engineered mice. J Clin Invest. 2008;118:829–38. doi: 10.1172/JCI34275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi SS, Diehl AM. Hepatic triglyceride synthesis and nonalcoholic fatty liver disease. Curr Opin Lipidol. 2008;19:295–300. doi: 10.1097/MOL.0b013e3282ff5e55. [DOI] [PubMed] [Google Scholar]
- Yamaguchi K, Yang L, McCall S, Huang J, Yu XX, Pandey SK, Bhanot S, Monia BP, Li YX, Diehl AM. Inhibiting triglyceride synthesis improves hepatic steatosis but exacerbates liver damage and fibrosis in obese mice with nonalcoholic steatohepatitis. Hepatology. 2007;45:1366–74. doi: 10.1002/hep.21655. [DOI] [PubMed] [Google Scholar]
- Li ZZ, Berk M, McIntyre TM, Feldstein AE. Hepatic lipid partitioning and liver damage in nonalcoholic fatty liver disease: role of stearoyl-CoA desaturase. J Biol Chem. 2009;284:5637–44. doi: 10.1074/jbc.M807616200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paton CM, Ntambi JM. Biochemical and physiological function of stearoyl-CoA desaturase. Am J Physiol Endocrinol Metab. 2009;297:E28–37. doi: 10.1152/ajpendo.90897.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotronen A, Seppänen-Laakso T, Westerbacka J, Kiviluoto T, Arola J, Ruskeepää AL, Oresic M, Yki-Järvinen H. Hepatic stearoyl-coa desaturase (scd)-1 activity and diacylglycerol but not ceramide concentrations are increased in the nonalcoholic human fatty liver. Diabetes. 2009;58:203–8. doi: 10.2337/db08-1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimano H, Yahagi N, Amemiya-Kudo M, Hasty AH, Osuga J, Tamura Y, Shionoiri F, Iizuka Y, Ohashi K, Harada K, Gotoda T, Ishibashi S, Yamada N. Sterol regulatory element-binding protein-1 as a key transcription factor for nutritional induction of lipogenic enzyme genes. J Biol Chem. 1999;274:35832–9. doi: 10.1074/jbc.274.50.35832. [DOI] [PubMed] [Google Scholar]
- Brown JM, Chung S, Sawyer JK, Degirolamo C, Alger HM, Nguyen T, Zhu X, Duong MN, Brown AL, Lord C, Shah R, Davis MA, Kelley K, Wilson MD, Madenspacher J, Fessler MB, Parks JS, Rudel LL. Combined therapy of dietary fish oil and stearoyl-CoA desaturase 1 inhibition prevents the metabolic syndrome and atherosclerosis. Arterioscler Thromb Vasc Biol. 2010;30:24–30. doi: 10.1161/ATVBAHA.109.198036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown JM, Chung S, Sawyer JK, Degirolamo C, Alger HM, Nguyen T, Zhu X, Duong MN, Wibley AL, Shah R, Davis MA, Kelley K, Wilson MD, Kent C, Parks JS, Rudel LL. Inhibition of stearoyl-coenzyme A desaturase 1 dissociates insulin resistance and obesity from atherosclerosis. Circulation. 2008;118:1467–75. doi: 10.1161/CIRCULATIONAHA.108.793182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flowers MT, Ntambi JM. Role of stearoyl-coenzyme A desaturase in regulating lipid metabolism. Curr Opin Lipidol. 2008;19:248–56. doi: 10.1097/MOL.0b013e3282f9b54d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chalasani N, Wilson L, Kleiner DE, Cummings OW, Brunt EM, Unalp A. NASH Clinical Research Network. Relationship of steatosis grade and zonal location to histological features of steatohepatitis in adult patients with non-alcoholic fatty liver disease. J Hepatol. 2008;48:829–834. doi: 10.1016/j.jhep.2008.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vuppalanchi R, Cummings OW, Saxena R, Ulbright TM, Martis N, Jones DR, Bansal N, Chalasani N. Hepatic steatosis relationship among histological, radiological and biochemical assessments. J Clin Gastroenterol. 2007;41:206–210. doi: 10.1097/01.mcg.0000225515.28536.3a. [DOI] [PubMed] [Google Scholar]
- Rinella ME, McCarthy R, Thakrar K, Finn JP, Rao SM, Koffron AJ, Abecassis M, Blei AT. Dual-echo, chemical shift gradient-echo magnetic resonance imaging to quantify hepatic steatosis: Implications for living liver donation. Liver Transplantation. 2003;9:851–856. doi: 10.1053/jlts.2003.50153. [DOI] [PubMed] [Google Scholar]
- Zhang B, Menzin J, Friedman M, Korn JR, Burge RT. Predicted coronary risk for adults with coronary heart disease and low HDL-C: an analysis from the US National Health and Nutrition Examination Survey. Curr Med Res Opin. 2008;24:2711–7. doi: 10.1185/03007990802363198. [DOI] [PubMed] [Google Scholar]
- Adams LA, Waters OR, Knuiman MW, Elliott RR, Olynyk JK. NAFLD as a risk factor for the development of diabetes and the metabolic syndrome: an eleven-year follow-up study. Am J Gastroenterol. 2009;104:861–7. doi: 10.1038/ajg.2009.67. [DOI] [PubMed] [Google Scholar]
- Mills SJ, Harrison SA. Comparison of the natural history of alcoholic and nonalcoholic fatty liver disease. Curr Gastroenterol Rep. 2005;7:32–6. doi: 10.1007/s11894-005-0063-4. [DOI] [PubMed] [Google Scholar]
- Liou I, Kowdley KV. Natural history of nonalcoholic steatohepatitis. J Clin Gastroenterol. 2006;40(Suppl 1):S11–6. doi: 10.1097/01.mcg.0000168644.23697.31. [DOI] [PubMed] [Google Scholar]
- Farrell GC, Larter CZ. Nonalcoholic fatty liver disease: from steatosis to cirrhosis. Hepatology. 2006;43:S99–S112. doi: 10.1002/hep.20973. [DOI] [PubMed] [Google Scholar]
- Rubinstein E, Lavine JE, Schwimmer JB. Hepatic, cardiovascular, and endocrine outcomes of the histological subphenotypes of nonalcoholic fatty liver disease. Semin Liver Dis. 2008;28:380–5. doi: 10.1055/s-0028-1091982. [DOI] [PubMed] [Google Scholar]
- Yatsuji S, Hashimoto E, Tobari M, Taniai M, Tokushige K, Shiratori K. Clinical features and outcomes of cirrhosis due to non-alcoholic steatohepatitis compared with cirrhosis caused by chronic hepatitis C. J Gastroenterol Hepatol. 2009;24:248–54. doi: 10.1111/j.1440-1746.2008.05640.x. [DOI] [PubMed] [Google Scholar]
- Dowman JK, Tomlinson JW, Newsome PN. Pathogenesis of non-alcoholic fatty liver disease. QJM. 2010;103:71–83. doi: 10.1093/qjmed/hcp158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maher JJ, Leon P, Ryan JC. Beyond insulin resistance: Innate immunity in nonalcoholic steatohepatitis. Hepatology. 2008;48:670–8. doi: 10.1002/hep.22399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diehl AM. Nonalcoholic Steatosis and Steatohepatitis IV. Nonalcoholic fatty liver disease abnormalities in macrophage function and cytokines. Am J Physiol Gastrointest Liver Physiol. 2002;282:G1–G5. doi: 10.1152/ajpgi.00384.2001. [DOI] [PubMed] [Google Scholar]
- Li Z, Diehl AM. Innate immunity in the liver. Curr Opin Gastroenterol. 2003;19:565–71. doi: 10.1097/00001574-200311000-00009. [DOI] [PubMed] [Google Scholar]
- Choi S, Diehl AM. Role of inflammation in nonalcoholic steatohepatitis. Curr Opin Gastroenterol. 2005;21:702–7. doi: 10.1097/01.mog.0000182863.96421.47. [DOI] [PubMed] [Google Scholar]
- Perseghin G, Petersen K, Shulman GI. Cellular mechanism of insulin resistance: potential links with inflammation. Int J Obes Relat Metab Disord. 2003;27(Suppl 3):S6–S11. doi: 10.1038/sj.ijo.0802491. [DOI] [PubMed] [Google Scholar]
- Lee JY, Hwang DH. The modulation of inflammatory gene expression by lipids: mediation through Toll-like receptors. Mol Cell. 2006;21:174–185. [PubMed] [Google Scholar]
- Kim JK, Kim YJ, Fillmore JJ, Chen Y, Moore I, Lee J, Yuan M, Li ZW, Karin M, Perret P, Shoelson SE, Shulman GI. Prevention of fat-induced insulin resistance by salicylate. J Clin Invest. 2001;108:437–446. doi: 10.1172/JCI11559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borst SE, Lee Y, Conover CF, Shek EW, Bagby GJ. Neutralization of tumor necrosis factor-alpha reverses insulin resistance in skeletal muscle but not adipose tissue. Am J Physiol Endocrinol Metab. 2004;287:E934–8. doi: 10.1152/ajpendo.00054.2004. [DOI] [PubMed] [Google Scholar]
- Lorenzo M, Fernández-Veledo S, Vila-Bedmar R, Garcia-Guerra L, De Alvaro C, Nieto-Vazquez I. Insulin resistance induced by tumor necrosis factor-alpha in myocytes and brown adipocytes. J Anim Sci. 2008;86(14 Suppl):E94–104. doi: 10.2527/jas.2007-0462. [DOI] [PubMed] [Google Scholar]
- Abiru S, Migita K, Maeda Y, Daikoku M, Ito M, Ohata K, Nagaoka S, Matsumoto T, Takii Y, Kusumoto K, Nakamura M, Komori A, Yano K, Yatsuhashi H, Eguchi K, Ishibashi H. Serum cytokine and soluble cytokine receptor levels in patients with non-alcoholic steatohepatitis. Liver Int. 2006;26:39–45. doi: 10.1111/j.1478-3231.2005.01191.x. [DOI] [PubMed] [Google Scholar]
- Bahcecioglu IH, Yalniz M, Ataseven H, Ilhan N, Ozercan IH, Seckin D, Sahin K. Levels of serum hyaluronic acid, TNF-alpha and IL-8 in patients with nonalcoholic steatohepatitis. Hepatogastroenterology. 2005;52:1549–53. [PubMed] [Google Scholar]
- Grabig A, Paclik D, Guzy C, Dankof A, Baumgart DC, Erckenbrecht J, Raupach B, Sonnenborn U, Eckert J, Schumann RR, Wiedenmann B, Dignass AU, Sturm A. Escherichia coli strain Nissle 1917 ameliorates experimental colitis via toll-like receptor 2- and toll-like receptor 4-dependent pathways. Infect Immun. 2006;74:4075–4082. doi: 10.1128/IAI.01449-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satapathy SK, Garg S, Chauhan R, Sakhuja P, Malhotra V, Sharma BC, Sarin SK. Beneficial effects of tumor necrosis factor-alpha inhibition by pentoxifylline on clinical, biochemical, and metabolic parameters of patients with nonalcoholic steatohepatitis. Am J Gastroenterol. 2004;99:1946–52. doi: 10.1111/j.1572-0241.2004.40220.x. [DOI] [PubMed] [Google Scholar]
- Adams LA, Zein CO, Angulo P, Lindor KD. A pilot trial of pentoxifylline in nonalcoholic steatohepatitis. Am J Gastroenterol. 2004;99:2365–8. doi: 10.1111/j.1572-0241.2004.40064.x. [DOI] [PubMed] [Google Scholar]
- Ofei F, Hurel S, Newkirk J, Sopwith M, Taylor R. Effects of an engineered human anti-TNF-alpha antibody (CDP571) on insulin sensitivity and glycemic control in patients with NIDDM. Diabetes. 1996;45:881–5. doi: 10.2337/diabetes.45.7.881. [DOI] [PubMed] [Google Scholar]
- Hotamisligil GS. Role of endoplasmic reticulum stress and c-Jun NH2-terminal kinase pathways in inflammation and origin of obesity and diabetes. Diabetes. 2005;54(Suppl 2):S73–S78. doi: 10.2337/diabetes.54.suppl_2.S73. [DOI] [PubMed] [Google Scholar]
- Perseghin G, Petersen K, Shulman GI. Cellular mechanism of insulin resistance: potential links with inflammation. Int J Obes Relat Metab Disord. 2003;27(Suppl 3):S6–S11. doi: 10.1038/sj.ijo.0802491. [DOI] [PubMed] [Google Scholar]
- Shoelson SE, Lee J, Goldfine AB. Inflammation and insulin resistance. J Clin Invest. 2006;116:1793–1801. doi: 10.1172/JCI29069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malhi H, Bronk SF, Werneburg NW, Gores GJ. Free fatty acids induce JNK-dependent hepatocyte lipoapoptosis. J Biol Chem. 2006;281:12093–12101. doi: 10.1074/jbc.M510660200. [DOI] [PubMed] [Google Scholar]
- Feldstein AE, Canbay A, Angulo P, Taniai M, Burgart LJ, Lindor KD, Gores GJ. Hepatocyte apoptosis and fas expression are prominent features of human nonalcoholic steatohepatitis. Gastroenterology. 2003;125:437–443. doi: 10.1016/S0016-5085(03)00907-7. [DOI] [PubMed] [Google Scholar]
- Schattenberg JM, Singh R, Wang Y, Lefkowitch JH, Rigoli RM, Scherer PE, Czaja MJ. JNK1 but not JNK2 promotes the development of steatohepatitis in mice. Hepatology. 2006;43:163–172. doi: 10.1002/hep.20999. [DOI] [PubMed] [Google Scholar]
- Gao Z, Zhang X, Zuberi A, Hwang D, Quon MJ, Lefevre M, Ye J. Inhibition of insulin sensitivity by free fatty acids requires activation of multiple serine kinases in 3T3-L1 adipocytes. Mol Endocrinol. 2004;18:2024–2034. doi: 10.1210/me.2003-0383. [DOI] [PubMed] [Google Scholar]
- Samuel VT, Liu ZX, Qu X, Elder BD, Bilz S, Befroy D, Romanelli AJ, Shulman GI. Mechanism of hepatic insulin resistance in non-alcoholic fatty liver disease. J Biol Chem. 2004;279:32345–32353. doi: 10.1074/jbc.M313478200. [DOI] [PubMed] [Google Scholar]
- Samuel VT, Liu ZX, Wang A, Beddow SA, Geisler JG, Kahn M, Zhang XM, Monia BP, Bhanot S, Shulman GI. Inhibition of protein kinase Cepsilon prevents hepatic insulin resistance in nonalcoholic fatty liver disease. J Clin Invest. 2007;117:739–745. doi: 10.1172/JCI30400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai D, Yuan M, Frantz DF, Melendez PA, Hansen L, Lee J, Shoelson SE. Local and systemic insulin resistance resulting from hepatic activation of IKKbeta and NF-kappaB. Nat Med. 2005;11:183–190. doi: 10.1038/nm1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter-Kent C, Zein NN, Feldstein AE. Cytokines in the pathogenesis of fatty liver and disease progression to steatohepatitis: implications for treatment. Am J Gastroenterol. 2008;103:1036–42. doi: 10.1111/j.1572-0241.2007.01709.x. [DOI] [PubMed] [Google Scholar]
- Austin RL, Rune A, Bouzakri K, Zierath JR, Krook A. siRNA-mediated reduction of inhibitor of nuclear factor-kappaB kinase prevents tumor necrosis factor-alpha-induced insulin resistance in human skeletal muscle. Diabetes. 2008;57:2066–73. doi: 10.2337/db07-0763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouzakri K, Zierath JR. MAP4K4 gene silencing in human skeletal muscle prevents tumor necrosis factor-alpha-induced insulin resistance. J Biol Chem. 2007;282:7783–9. doi: 10.1074/jbc.M608602200. [DOI] [PubMed] [Google Scholar]
- Song MJ, Kim KH, Yoon JM, Kim JB. Activation of Toll-like receptor 4 is associated with insulin resistance in adipocytes. Biochem Biophys Res Commun. 2006;4;346(3):739–45. doi: 10.1016/j.bbrc.2006.05.170. [DOI] [PubMed] [Google Scholar]
- Shi H, Kokoeva MV, Inouye K, Tzameli I, Yin H, Flier JS. TLR4 links innate immunity and fatty acid-induced insulin resistance. J Clin. 2006;116(11):3015–25. doi: 10.1172/JCI28898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medzhitov R, Janeway C Jr. Innate immunity. N Engl J Med. 2000;343:338–344. doi: 10.1056/NEJM200008033430506. [DOI] [PubMed] [Google Scholar]
- Tsukumo DM, Carvalho-Filho MA, Carvalheira JB, Prada PO, Hirabara SM, Schenka AA, Araújo EP, Vassallo J, Curi R, Velloso LA, Saad MJ. Loss-of-function mutation in Toll-like receptor 4 prevents diet-induced obesity and insulin resistance. Diabetes. 2007;56(8):1986–98. doi: 10.2337/db06-1595. [DOI] [PubMed] [Google Scholar]
- Grabig A, Paclik D, Guzy C, Dankof A, Baumgart DC, Erckenbrecht J, Raupach B, Sonnenborn U, Eckert J, Schumann RR, Wiedenmann B, Dignass AU, Sturm A. Escherichia coli strain Nissle 1917 ameliorates experimental colitis via toll-like receptor 2- and toll-like receptor 4-dependent pathways. Infect Immun. 2006;74:4075–4082. doi: 10.1128/IAI.01449-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rachmilewitz D, Katakura K, Karmeli F, Hayashi T, Reinus C, Rudensky B, Akira S, Takeda K, Lee J, Takabayashi K, Raz E. Toll-like receptor 9 signaling mediates the anti-inflammatory effects of probiotics in murine experimental colitis. Gastroenterology. 2004;126:520–528. doi: 10.1053/j.gastro.2003.11.019. [DOI] [PubMed] [Google Scholar]
- Li Z, Yang S, Lin H, Huang J, Watkins PA, Moser AB, Desimone C, Song XY, Diehl AM. Probiotics and antibodies to TNF inhibit inflammatory activity and improve nonalcoholic fatty liver disease. Hepatology. 2003;37:343–350. doi: 10.1053/jhep.2003.50048. [DOI] [PubMed] [Google Scholar]
- Loguercio C, Federico A, Tuccillo C, Terracciano F, D'Auria MV, De Simone C, Del Vecchio Blanco C. Beneficial effects of a probiotic VSL#3 on parameters of liver dysfunction in chronic liver diseases. J Clin Gastroenterol. 2005;39:540–543. doi: 10.1097/01.mcg.0000165671.25272.0f. [DOI] [PubMed] [Google Scholar]
- Lee JY, Zhao L, Youn HS, Weatherill AR, Tapping R, Feng L, Lee WH, Fitzgerald KA, Hwang DH. Saturated fatty acid activates but polyunsaturated fatty acid inhibits Tolllike receptor 2 dimerized with Toll-like receptor 6 or 1. J Biol Chem. 2004;279:16971–16979. doi: 10.1074/jbc.M312990200. [DOI] [PubMed] [Google Scholar]
- Svegliati-Baroni G, Candelaresi C, Saccomanno S, Ferretti G, Bachetti T, Marzioni M, De Minicis S, Nobili L, Salzano R, Omenetti A, Pacetti D, Sigmund S, Benedetti A, Casini A. A model of insulin resistance and nonalcoholic steatohepatitis in rats: role of peroxisome proliferator-activated receptor-alpha and n-3 polyunsaturated fatty acid treatment on liver injury. Am J Pathol. 2006;169:846–860. doi: 10.2353/ajpath.2006.050953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Accili D, Arden KC. FoxOs at the crossroads of cellular metabolism, differentiation, and transformation. Cell. 2004;117:421–426. doi: 10.1016/S0092-8674(04)00452-0. [DOI] [PubMed] [Google Scholar]
- Barthel A, Schmoll D, Unterman TG. FoxO proteins in insulin action and metabolism. Trends Endocrinol Metab. 2005;16:183–189. doi: 10.1016/j.tem.2005.03.010. [DOI] [PubMed] [Google Scholar]
- Kamagate A, Dong HH. FoxO1 integrates insulin signaling to VLDL production. Cell Cycle. 2008;7:3162–3170. doi: 10.4161/cc.7.20.6882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altomonte J, Cong L, Harbaran S, Richter A, Xu J, Meseck M, Dong HH. Foxo1 Mediates Insulin Action on ApoC-III and Triglyceride Metabolism. J Clin Invest. 2004;114:1493–1503. doi: 10.1172/JCI19992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qu S, Altomonte J, Perdomo G, He J, Fan Y, Kamagate A, Meseck M, Dong HH. Aberrant Forkhead box O1 function is associated with impaired hepatic metabolism. Endocrinology. 2006;147:5641–5652. doi: 10.1210/en.2006-0541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamagate A, Qu S, Perdomo G, Su D, Kim DH, Slusher S, Meseck M, Dong HH. FoxO1 mediates insulin-dependent regulation of hepatic VLDL production in mice. J Clin Invest. 2008;118:2347–2364. doi: 10.1172/JCI32914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen CM, Faulenbach M, Vaag A, Volund A, Ehses JA, Seifert B, Mandrup-Poulsen T, Donath MY. Interleukin-1-receptor antagonist in type 2 diabetes mellitus. N Engl J Med. 2007;356:1517–1526. doi: 10.1056/NEJMoa065213. [DOI] [PubMed] [Google Scholar]