Abstract
We investigated whether uncertainty about the impact of children’s chronic health conditions on their daily lives leads to changes in mothers’ and fathers’ mental and physical health. Three waves of data were collected over three years from parents of 228 children with chronic health conditions. Parents reported their level of uncertainty about how the child’s health condition affected the child’s daily life, as well as measures of their own mental and physical health at each wave of data collection. Results of structural equation models indicate that, among mothers, more illness-related uncertainty was associated with a subsequent increase in psychological symptoms relative to other mothers in the study. Psychological symptoms, in turn, were associated with a subsequent increase in physical symptoms among mothers. Uncertainty did not affect fathers’ health. Illness-related uncertainty may be a risk factor for psychological and physical symptoms in mothers of children with chronic health conditions. As such, interventions that address uncertainty related to the child’s chronic health condition may improve psychological and physical well-being of mothers of children with chronic health conditions.
Keywords: childhood chronic health conditions, parent adjustment, uncertainty
Health
Due to advances in medicine and technology, children with previously fatal diseases now survive and have chronic health conditions with no cure. Between 10% and 30% of children in the U.S. have a chronic illness or disability (Davidoff, 2004; Van Dyck, Kogan, McPherson, Weissman, & Newacheck, 2004). A substantial body of research indicates that parents of children with chronic health conditions are at risk for symptoms of psychological distress (e.g., Mastroyannopoulou, Stallard, Lewis, & Lenton, 1997; Nagy & Ungerer, 1990; Silver, Westbrook, & Stein, 1998). Theory and research provide some guidance regarding which factors are likely to put parents at risk for distress. Uncertainty arising in the context of chronic illness is an important component of family stress, with two primary branches of investigation. These branches of investigation stem from family stress theory (Boss, 2002; Boss & Greenberg, 1984) and uncertainty in illness theory (Mishel, 1981, 1983, 1984, 1993).
Family stress theory has focused on boundary ambiguity. Boundary ambiguity is a specific aspect of uncertainty that is defined as “a state in which family members are uncertain in their perception about who is in or out of the family and who is performing what roles and tasks within the family system” (Boss & Greenberg, 1984, p. 536). Thus, boundary ambiguity has two dimensions: membership ambiguity and role ambiguity (Berge & Holm, 2007). Membership ambiguity can occur when parents have difficulty incorporating an ill child into the family. For example, parents may have difficulty becoming emotionally connected with a child who has a limited life expectancy. Role ambiguity can occur when parents have difficulty determining what their parental role is vis-à-vis the ill child. For example, parents may feel more like a medical assistant than a parent to their child. The boundary ambiguity aspect of uncertainty has been investigated in illnesses across the life span—from chronic illnesses in children (Mu, Kuo, & Chang, 2005) to dementia (Boss, Caron, Horbal, & Mortimer, 1990; Caron, Boss, & Mortimer, 1999). See Carroll et al. (2007) for a review of boundary ambiguity research that includes a summary of research on boundary ambiguity in the context of chronic illness.
The second branch of research stems from uncertainty in illness theory (Mishel, 1981, 1983, 1984, 1993). Mishel defines uncertainty as the inability to assign meaning to illness-related events, which occurs when a person cannot adequately categorize information and/or predict outcomes due to a lack of sufficient cues (Mishel, 1981). Uncertainty related to children’s chronic health conditions has been associated with parent mental health in several cross-sectional studies (Bonner, Hardy, Guill, et al., 2006; Grootenhuis & Last, 1997; Mu, 2005; Mu, Ma, Hwang, & Chao, 2002; Mu, Ma, et al., 2001; Mu, Wong, Chang, & Kwan, 2001). For example, Jessop and Stein (1985) found that the need to expect changes in the child’s condition was associated with psychiatric symptoms reported by mothers of children with a variety of chronic conditions. Another study found that illness-related factors that increase parental uncertainty (such as the need to watch for sudden changes in the condition) had indirect effects on maternal mental health via their influence on mothers’ perception of the impact on the family (Ireys & Silver, 1996).
Prior research on the impact of uncertainty on parents of children with chronic health conditions has several limitations. First, research has primarily been cross-sectional. Second, research has emphasized the mental health of parents, with little investigation of physical health. Third, most research has focused on mothers. The present study addressed each of these limitations by utilizing longitudinal data to assess changes in mothers’ and fathers’ mental and physical health. The conceptual model for this study was based on uncertainty in illness theory and specifically focused on parental uncertainty about the impact of the health condition on the child’s daily life, which is also referred to as “daily living uncertainty” (Mishel, 1993). Two aspects of uncertainty were the focus of this study: uncertainty regarding the impact of the condition on mood and uncertainty regarding the impact of the condition on sleep and energy.
This study proposed and tested a “cascade of distress” in which uncertainty leads to a relative increase in psychological symptoms, which over time leads to a relative increase in physical symptoms. Psychological and physical symptoms at time one were included in analyses as control variables for symptoms at times two and three. The model was the same for mothers and for fathers, and was run separately for each gender. Two specific hypotheses were tested. Hypothesis 1: Parents who experience the highest amount of uncertainty about the impact of their child’s health condition on his/her daily life will have a greater relative increase in psychological symptoms over time. Hypothesis 2: Parents who have greater psychological symptoms will subsequently experience a greater relative increase in physical symptoms.
METHOD
Sample
This study involved secondary analysis of data from Project Resilience (Dodgson et al., 2000; Garwick, Patterson, Meschke, Bennett, & Blum, 2002), a longitudinal study of families of 327 infants and preadolescents with a variety of chronic health conditions. Project Resilience used a noncategorical approach grounded in the premise that children and families living with a wide variety of chronic health conditions experience common stressors (Perrin et al., 1993; Stein et al., 1993). Research supports this premise: the psychosocial impact of child chronic conditions on children and families is more similar across conditions than different (Gartstein, Short, Vannatta, & Noll, 1999).
Three waves of data were collected at 12–18 month intervals beginning in 1991. The cross sequential design of the original study called for inclusion of two cohorts of children: a cohort that was 6–26 months old (n=186) and a cohort that was 8–11 years old (n=141) at enrollment. Participants were recruited from two metropolitan areas in the United States: Minneapolis-St. Paul, Minnesota and Seattle, Washington. Researchers collaborated with all 13 hospitals and health maintenance organizations in these two geographic areas that provided care for children with chronic health conditions. All children were identified from medical records using ICD-9 codes that met the following definition of a chronic health condition: (a) having a biological, physiological, or anatomical basis; (b) lasting, or expected to last, for a minimum of 1 year; and (c) producing, or very likely to produce, long-term sequelae (e.g., ongoing treatments, use of medical technology, or disability; Stein et al., 1993). In addition, the child’s health condition had to have been diagnosed at least 6 months prior to recruitment for the study. Given that the research team was highly committed to a noncategorical approach, efforts were not made to ensure that the medical diagnoses in the sample reflected the prevalence of these diagnoses in the general population. Approval to conduct the research was granted by the institutional review boards of the University of Minnesota, the University of Washington, and each of the 13 clinical sites from which participants were recruited. The family income and ethnic composition of the entire sample are representative of the geographic areas from which the participants were drawn.
By the third wave of data collection, 35 families had withdrawn from the study and 7 children had died, producing a retention rate of 87.2%. Two cases were excluded from the sample because the caregivers were grandparents. An additional 55 cases were excluded from the current study due to missing data, resulting in a final sample of parents of 228 children (220 mothers and 188 fathers). The vast majority of parents were biological parents of the children (97.3% of both mothers and fathers). The sample also included adoptive parents (2.3% of mothers, 2.1% of fathers) and stepparents (.5% of both mothers and fathers). There were no significant differences in demographics or chronic conditions represented among participants in the two states and hence data from the states were combined for all analyses.
Because the focus of this study was on parent health, the two cohorts were combined to increase the sample size. Cohort was examined as a potential moderator and was not significant, thus supporting the decision to combine cohorts for analyses. The combined sample was composed of 104 girls and 124 boys. Ninety-three percent of the children were Caucasian, and 7% were from ethnic minority groups. Mean family size was four (M = 4.1, SD = 1.1). Table 1 provides additional demographic information about the sample.
Table 1.
Demographic Characteristics of the Sample
| Total Sample (n = 228 children) | ||
|---|---|---|
| Variable | N | % |
| Yearly household income (1991 – 1992)* | ||
| < $20,000 | 18 | 8.1% |
| $20,000 - $39,999 | 69 | 31.2% |
| $40,000 - $59,999 | 78 | 35.3% |
| > $60,000 | 56 | 25.3% |
|
| ||
| Highest level of education completed (mothers) | ||
| Did not graduate from high school | 4 | 1.8% |
| High school graduate | 50 | 22.7% |
| Vocational-technical school | 87 | 39.5% |
| College | 63 | 28.6% |
| Graduate/Professional school | 16 | 7.3% |
| Highest level of education completed (fathers) | ||
| Did not graduate from high school | 5 | 2.6% |
| High school graduate | 28 | 14.9% |
| Vocational-technical school | 71 | 37.8% |
| College | 58 | 30.9% |
| Graduate/Professional school | 26 | 13.8% |
|
| ||
| Type of chronic condition (children) | ||
| Developmental disability | 52 | 22.8% |
| Neurological | 49 | 21.5% |
| Cardiovascular | 30 | 13.2% |
| Pulmonary | 26 | 11.4% |
| Endocrine/Metabolic | 21 | 9.2% |
| Maxillofacial/Orthopedic | 19 | 8.3% |
| Ear, nose, and throat/Opthalmology | 11 | 4.8% |
| Hematology/Oncology | 10 | 4.4% |
| Gastroenterology/Urology/Nephrology | 10 | 4.4% |
| Infant Cohort (n = 142 children) | ||
|---|---|---|
| Variable | Mean | SD |
| Mother’s age at Time 1 | 31.6 years | 4.8 years |
| Father’s age at Time 1 | 34.7 years | 5.1 years |
| Child’s age at Time 1 | 16.1 months | 4.7 months |
| Preadolescent Cohort (n = 86 children) | ||
|---|---|---|
| Variable | Mean | SD |
| Mother’s age at Time 1 | 38.7 years | 4.8 years |
| Father’s age at Time 1 | 40.4 years | 5.2 years |
| Child’s age at Time 1 | 9.5 years | 0.7 years |
The counts for household income do not sum to 228 due to missing data for this variable
Procedures
The child’s physician mailed information about the study to potential participants who met criteria for inclusion in the study as described above. Parents who were interested in participating returned a postcard or called the project coordinator. More than one-third of the families who received a letter agreed to participate in the study. A requirement for protecting human subjects was that the investigators could not know the names of potential participants until after they had expressed an interest in taking part in the study. As such, it was only possible to test for differences between respondents and nonrespondents on gender of child and an approximation of socioeconomic status based on parents’ zip code. There were no statistically significant differences between respondents and nonrespondents on these variables. Data were collected in the family’s home by trained interviewers. Parents completed self-report assessments of their own and their chronically ill child’s functioning.
Measures
Parental Uncertainty due to the Child’s Chronic Condition
Uncertainty was measured by two indicators created from the Functional Status Questionnaire (FS II [R]; Stein & Jessop, 1990): uncertainty regarding impact on (a) mood and (b) sleep and energy. This instrument was completed via interview with the parent(s) who knew the child best. In 61.2% of the families, mothers and fathers completed this instrument together. Mothers completed the instrument independently in 35.4% of the families and fathers completed the instrument independently in 2.9% of the families. The uncertainty regarding impact on mood measure was created by summing responses to five items on the FS II (R). If the parent endorsed a limitation related to the child’s mood and then indicated that the limitation was partly due to the chronic condition (as compared to fully or not at all due to the chronic condition), a score of 1 was assigned for that item. The five items that assessed limitations related to the child’s mood asked whether the child was cheerful, moody, irritable or cross, difficult, or having frequent temper tantrums. This measure had good internal consistency (alpha = .79 for both the sample of mothers and the sample of fathers). The indicator of uncertainty regarding impact on sleep and energy was created by summing responses to four items on the FS II (R). If the parent endorsed a limitation related to the child’s sleep or energy and then indicated that the limitation was partly due to the chronic condition, a score of 1 was assigned for that item. The four items that assessed limitations related to the child’s sleep and energy asked whether the child was sleeping well, sleeping through the night, interested in what was going on around him/her, or cutting down on his/her usual level of play activity. This measure had adequate internal consistency (alpha = .58 in the sample of mothers and .62 in the sample of fathers). We interpreted a response of “partly due to the chronic condition” as an indication of uncertainty as to whether the chronic condition or some other factor was responsible for the child’s behavior.
Psychological Symptoms
Mothers’ and fathers’ psychological symptoms at time 1 and time 2 were measured by three indicators: the Beck Depression Inventory (Beck, Ward, Mendelson, Mock, & Erbaugh, 1961) and the mental health and energy subscales from the Short-Form Health Survey (SF-36; Ware & Sherbourne, 1992). Mothers and fathers independently completed measures for all indicators of psychological symptoms. Raw scores for the mental health and energy subscales were transformed via instrument norms such that scores range from 0 to 100 and scores represent the percentage of total possible points that the person scored. For all indicators of psychological symptoms, responses were coded such that a higher score is indicative of more symptoms. The internal consistency reliability for all indicators of psychological symptoms was adequate; the alpha value was above .76 for both parents at both time points.
Physical Symptoms
Mothers’ and fathers’ physical symptoms at time 1 and time 3 were measured by three indicators, all of which are subscales of the Short-Form Health Survey (SF-36; Ware & Sherbourne, 1992). Mothers and fathers independently completed the SF-36. Raw scores for all subscales were transformed via instrument norms such that scores range from 0 to 100 and scores represent the percentage of total possible points that the person scored. For all indicators of physical symptoms, responses were coded such that a higher score is indicative of more symptoms. The internal consistency reliability for all indicators of physical symptoms was adequate; the alpha value was above .73 for both parents are both time points.
RESULTS
Comparison of Study Sample and the Full Sample
Not-included families refers to families who had withdrawn from the study (n=35), families of children who had died (n=7), families in which the caregivers were grandparents (n=2), and families for which data were missing (n=55). Included and not-included families did not differ significantly by mean family size. Included families had higher incomes and parents with higher education than not-included families. Included mothers were older and had fewer problems with general health than not-included mothers. Included mothers had children where there was less uncertainty about the impact of the condition on the child’s mood. Included fathers reported fewer depressive symptoms than not-included fathers.
Preliminary Analyses
Paired samples t tests were conducted to compare mothers and fathers on measures of psychological and physical symptoms. These tests indicate that mothers endorsed significantly more psychological symptoms than fathers on five of the six indicators of psychological symptoms. Mothers and fathers did not differ significantly from each other on any indicator of physical symptoms. See Table 2 for results of the paired samples t tests.
Table 2.
Results of Paired Samples T Tests Comparing Mothers and Fathers on Measures of Psychological and Physical Symptoms
| M (SD) for: |
t | ||
|---|---|---|---|
| Variable | Mothers | Fathers | (179 df) |
| Psychological Symptoms | |||
| Depressive symptoms time 1 | 5.61 (4.65) | 3.74 (3.94) | 4.71* ** |
| Mental health symptoms time 1 | 27.76 (14.68) | 23.44 (12.31) | 3.44* ** |
| Lack of Energy time 1 | 42.94 (17.64) | 38.28 (16.28) | 2.92** |
| Depressive symptoms time 2 | 5.18 (5.09) | 3.82 (4.49) | 3.14** |
| Mental health symptoms time 2 | 25.40 (14.23) | 23.87 (13.57) | 1.25 |
| Lack of energy time 2 | 42.39 (19.81) | 38.03 (16.09) | 2.69** |
|
| |||
| Physical Symptoms | |||
| Problems with physical function time 1 | 7.17 (13.83) | 5.89 (11.54) | .96 |
| Pain time 1 | 16.60 (19.21) | 17.28 (19.73) | −.33 |
| General health problems time 1 | 22.84 (18.19) | 23.58 (15.86) | −.44 |
| Problems with physical function time 3 | 7.06 (12.93) | 6.61 (13.51) | .33 |
| Pain time 3 | 18.95 (21.55) | 16.05 (17.35) | 1.53 |
| General health problems time 3 | 23.07 (17.18) | 26.13 (16.70) | −1.94 |
significant at p ≤ .05
significant at p ≤ .01
significant at p ≤ .001
Correlations between the indicators are reported in Table 3 and are mostly consistent with expectations. The variables that measure uncertainty have statistically significant correlations with most measures of psychological symptoms at time 2 for mothers. Of note, uncertainty regarding the impact of the condition on sleep and energy consistently has a stronger correlation than uncertainty regarding the impact on mood with the measures of psychological symptoms for mothers. The indicators for uncertainty do not have statistically significant associations with the measures of psychological symptoms at time 2 for fathers, which suggests that hypothesis 1 will not be supported for fathers. With regard to hypothesis two, which addresses the relation between psychological symptoms at time 2 and physical symptoms at time 3, the correlations between psychological symptoms at time 2 and physical symptoms at time 3 were statistically significant for all variables for mothers and most of the variables for fathers.
Table 3.
Correlations among Indicators for Mothers (N=220) and Fathers (N=188)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Indicators at Time 1 | ||||||||||||||
|
| ||||||||||||||
| 1 Impact on mood | 1.00 | .26 ** | .10 | .10 | .10 | .08 | .14 | .07 | .03 | .09 | .01 | .13 | .10 | .19 ** |
| 2 Impact on sleep/energy | .25** | 1.00 | −.01 | .00 | .03 | .03 | .03 | .06 | .06 | .07 | .06 | .07 | −.04 | .12 |
| 3 Depressive symptoms | .27** | .18** | 1.00 | .52 ** | .42 ** | .29 ** | .27 ** | .38 ** | .69 ** | .55 ** | .36 ** | .30 ** | .32 ** | .42 ** |
| 4 Mental health symptoms | .17* | .21** | .55** | 1.00 | .52 ** | .14 | .15 * | .38 ** | .37 ** | .46 ** | .28 ** | .09 | .13 | .30 ** |
| 5 Lack of energy | .16* | .18** | .47** | .61** | 1.00 | .29 ** | .22 ** | .50 ** | .30 ** | .30 ** | .50 ** | .15 * | .11 | .36 ** |
| 6 Problems with physical function | .07 | .03 | .22** | .31** | .34** | 1.00 | .51 ** | .35 ** | .29 ** | .16 * | .22 ** | .63 ** | .31 ** | .27 ** |
| 7 Pain | .15* | .06 | .26** | .35** | .43** | .44** | 1.00 | .36 ** | .25 ** | .18 * | .20 ** | .28 ** | .56 ** | .38 ** |
| 8 General health problems | .15* | .11 | .27** | .45** | .51** | .49** | .49** | 1.00 | .33 ** | .25 ** | .23 ** | .23 ** | .16 * | .51 ** |
| Indicators at Time 2 | ||||||||||||||
|
| ||||||||||||||
| 9 Depressive symptoms | .13 | .27** | .61** | .48** | .51** | .14* | .26** | .35** | 1.00 | .65 ** | .53 ** | .24 ** | .20 ** | .42 ** |
| 10 Mental health symptoms | .21** | .30** | .53** | .59** | .46** | .15* | .24** | .30** | .72** | 1.00 | .58 ** | .17 * | .19 ** | .35 ** |
| 11 Lack of energy | .13 | .19** | .37** | .40** | .56** | .16* | .25** | .35** | .59** | .61** | 1.00 | .18 * | .11 | .36 ** |
| Indicators at Time 3 | ||||||||||||||
|
| ||||||||||||||
| 12 Problems with physical function | .09 | .02 | .19** | .29** | .32** | .50** | .45** | .49** | .26** | .27** | .27** | 1.00 | .31 ** | .31 ** |
| 13 Pain | .19** | .06 | .22** | .22** | .31** | .26** | .45** | .33** | .32** | .31** | .26** | .60** | 1.00 | .39 ** |
| 14 General health problems | .13* | .10 | .29** | .37** | .43** | .35** | .39** | .66** | .48** | .41** | .36** | .64** | .52** | 1.00 |
significant at p < .05
significant at p < .01
The multivariate tests of skewness and kurtosis were both statistically significant at p < .01 for both mothers and fathers. Violating the assumption of multivariate normality creates a more conservative test of the model, as skewness and kurtosis may obscure potential relationships between constructs and produce an inflated chi-square value. Thus, data are less likely to yield a model with statistically significant path coefficients and high fit indices when the data are skewed and kurtotic (Kline, 1998).
Results of Testing the Theoretical Models
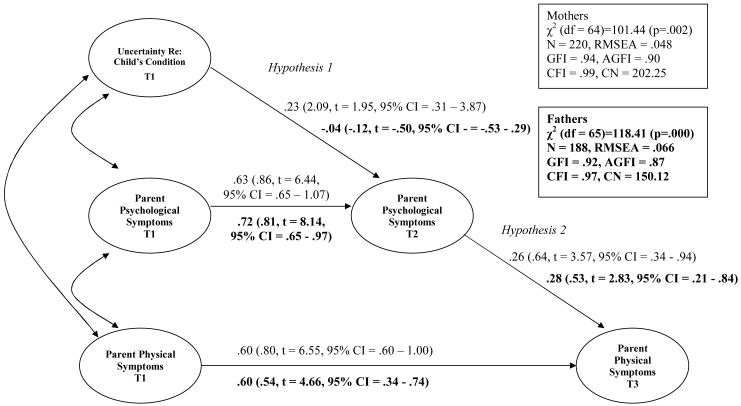
Structural equation modeling (SEM) was used to test the model, using LISREL 8.53 (Jöreskog & Sörbom, 1997). The model for mothers was run separately from the model for fathers. The Figure depicts the results of analyzing the model for mothers and for fathers.
Figure.
Maximum Likelihood Estimates of the Associations among Uncertainty, Psychological Symptoms, and Physical Symptoms for Mothers and Fathers
Note: Standardized path coefficients outside parentheses, unstandardized within parentheses.
Model for Mothers
Potential moderating effects of cohort and child gender were examined to determine whether it was necessary to run separate models based on cohort or child gender. Given that cohort and child gender did not moderate the relations among latent variables for mothers, only one model was run for mothers, regardless of child age or gender. The goodness of fit indices reported in the Figure indicate that the data adequately fit the model. The one exception is the statistically significant chi-square, which often will be statistically significant even with a well-fitting model when the sample size is greater than 200 (Kline, 1998). The model explained 59% of the variance in psychological symptoms at time 2 and 58% of the variance in physical symptoms at time 3.
Our first hypothesis predicted that parents who experience the most uncertainty will experience increasing psychological symptoms over time relative to other parents in the study. This hypothesis was supported, as the relevant path coefficient in the Figure was statistically significant at the p < .05 level for a one-tailed test. Our second hypothesis predicted that parents who have greater psychological symptoms at time 2 will subsequently experience a greater increase in physical symptoms at time 3 relative to other parents in the study. This hypothesis was also supported, as the relevant path coefficient in the Figure was statistically significant at the p < .05 level for a one-tailed test. Both of these paths were significant even though the model simultaneously controlled for psychological and physical symptoms at time 1.
Model for Fathers
Once again potential moderating effects of cohort and child gender were examined. This time the model failed to converge for the adolescent cohort, for sons, and for daughters; thus it was not possible to test for moderating effects of cohort and child gender with the sample of fathers. The indicator for uncertainty regarding impact of the condition on child’s mood had a negative variance in the original model. To overcome that, a known value of the variance for that indicator was used from the model for fathers in the infant cohort. Hence, all results based on this model are tentative and are most useful for attempting to understand what aspects of the model do not fit well for fathers.
Several results suggest that the indicators for uncertainty do not represent fathers’ experiences well. First, as described above, the indicator for uncertainty regarding impact on mood had a negative variance in the original model. Second, results suggest that the two indicators of uncertainty did not load similarly on the latent factor for uncertainty. Uncertainty regarding impact on mood had a much higher standardized factor loading (.84) than the indicator for uncertainty regarding impact on sleep and energy (.31), again suggesting that the indicators for uncertainty do not represent fathers’ experiences well.
With regard to the hypotheses, the path coefficient for the relation between uncertainty at time 1 and psychological symptoms at time 2 was not statistically significant, indicating that uncertainty was not associated with increases in psychological symptoms for fathers. With regard to the second hypothesis, the path coefficient for the relation between psychological symptoms at time 2 and physical symptoms at time 3 was statistically significant at the p < .05 level for a one-tailed test. Thus, results suggest that the model overall and in particular the measure for uncertainty did not capture fathers’ experiences well. The second hypothesis was supported, but this result should be interpreted with caution.
DISCUSSION
Contributions/Extension of Existing Knowledge
The current study makes several contributions to understanding the impact of uncertainty associated with childhood chronic health conditions on parents’ health. This study extends existing cross-sectional research by examining: (1) the longitudinal process of change in mothers’ and fathers’ health during the course of children’s chronic conditions and (2) the mental and physical health of both mothers and fathers. These two features are discussed below.
Existing cross-sectional research indicates that uncertainty is associated with parent psychological distress (Grootenhuis & Last, 1997; Mu, 2005; Mu, Ma, et al., 2001; Mu, Ma, Hwang, & Chao, 2002; Mu, Wong, Chang, & Kwan, 2001). The present study extended this research by identifying a longitudinal process through which mothers who experienced the highest amount of uncertainty about the impact of the condition on their child’s daily life reported more change in psychological symptoms at time 2 relative to other mothers in the study. The process of change in parents’ health was further explored by examining the impact of psychological symptoms at time 2 on physical symptoms at time 3.
Previous research has emphasized the impact of children’s chronic conditions on parents’ mental health, with little investigation of the impact on their physical health. The few studies that have been conducted suggest that symptoms of depression (Tong et al., 2002) and depressive coping style (Staab et al., 1998) are associated with health-related quality of life and physical functioning among parents of children with chronic health conditions. The present study extends these findings by demonstrating that parents with greater psychological symptoms subsequently experience greater relative increase in physical symptoms.
The current study also looked into gender differences in parental adaptation in the context of children’s chronic health conditions. Several prior studies have found heightened levels of distress for mothers of children with chronic health conditions, but not fathers (Mastroyannopoulou et al., 1997; Nagy & Ungerer, 1990; Svavarsdottir & Rayens, 2005). In the present study, fathers reported significantly fewer psychological symptoms than mothers, but fathers and mothers did not differ significantly with regard to physical symptoms. Previous research has also revealed gender differences in the factors that are associated with parental adaptation to children’s chronic health conditions (Nagy & Ungerer, 1990; Svavarsdottir, Rayens, & McCubbin, 2005). In the present study, uncertainty about the impact of the condition on the child’s daily life was related to subsequent psychological symptoms for mothers but not fathers. However, this finding may be due the way in which uncertainty was measured, as discussed in more detail below.
Limitations
The major findings should be interpreted in light of limitations of the study. The primary limitation concerns the measurement of uncertainty. Project Resilience did not use an established measure of uncertainty such as the Parental Perception of Uncertainty Scale (Mishel, 1983). However, we were able to construct a novel measure of uncertainty as described in the methods section. In addition, mothers and fathers did not always rate uncertainty independently. In more than half of the cases, both parents completed the measure of uncertainty together. While it was a step forward that fathers were included in providing input, the extent to which each parent had influence on the scores that were jointly assigned by the parents is unclear. In particular, fathers may have had less input in determining the scores for uncertainty, in which case a better model of the relationship between uncertainty and subsequent psychological and physical symptoms for fathers might exist when the measure of uncertainty is based solely on fathers’ perceptions.
A second limitation concerns our use of a noncategorical approach to recruitment. Since the noncategorical approach is based on the premise that families living with a wide variety of chronic health conditions experience common stressors, sample recruitment was not designed to reflect the actual prevalence of chronic health conditions in the population. Hence, the chronic health conditions that were most prevalent in Project Resilience are not the most prevalent chronic conditions in childhood, which might limit the generalizability of findings. Generalizability is further limited by the fact that less than half of the eligible families participated in the study. Despite these limitations, results have implications for future research and clinical work.
Implications
Implications for Future Research
Future research is needed to continue to investigate the impact of uncertainty on fathers. In the present study, the indicators for uncertainty did not appear to capture fathers’ experience very well. One solution would be to have fathers and mothers independently complete measures of uncertainty. Such a procedure would also enable researchers to investigate the implications of differing levels of uncertainty within couples to determine whether discrepancy within couples in extent of uncertainty leads to parental distress. In addition, future research might profitably utilize qualitative methods to investigate uncertainty in addition to quantitative measures of uncertainty. This is consistent with Boss’ recommendation of the use of a multimethod approach that incorporates both qualitative and quantitative methods to investigate different aspects of uncertainty (Boss, 2007). Qualitative research may be especially useful for better understanding fathers’ experiences of uncertainty, and providing clues in terms of how fathers and mothers differently experience uncertainty in the context of childhood chronic illness.
Future research could also investigate factors that could replace uncertainty in the cascade of distress. For both mothers and fathers, parents who had greater psychological symptoms at time 2 subsequently experienced greater change in physical symptoms. Uncertainty was predictive of change in psychological symptoms at time 2 for mothers, and as such, uncertainty was a catalyst for the cascade of distress for mothers. Uncertainty is only one possible catalyst for the cascade. The salience of any given catalyst may differ by parent gender. Indeed, some prior research suggests that factors such as financial concerns and increased hours at work (Chesler & Parry, 2001; Goble, 2004; Neil-Urban, 2002; Svavarsdottir, 2005) may be more salient than uncertainty for fathers. An important possible catalyst for the cascade of distress is the boundary ambiguity aspect of uncertainty that has been identified by family stress theory (Boss, 2002; Boss & Greenberg, 1984). Research that focuses on boundary ambiguity would differ from the present research in its focus on the extent to which parents have difficulty incorporating the ill child into the family and determining their parental roles vis-à-vis the ill child.
Another avenue for future research is to extend the linear cascade of distress model used in this study by testing circular models that include both parental and child adjustment. Circular models can test the extent to which parental and child adjustment mutually influence each other. Aspects of the child’s health condition (such as uncertainty) likely affect parental adjustment, and parental adjustment in turn is likely to affect the child’s adjustment. Research on adjustment among individuals with Alzheimer’s disease and their family caregivers provides initial support for circular models of adjustment. This research suggests that caregiver behavior affects patient behavior, which in turn affects caregiver behavior (Caron et al., 1999). Research that tests circular models of adjustment among both parents and children is consistent with Boss’s (2007) emphasis that family adjustment is a systemic process rather than a linear process.
Clinical Implications
The present research identifies uncertainty about a child’s chronic condition as a risk factor for subsequent psychological symptoms for mothers. Further, these psychological symptoms are a risk factor for subsequent changes in mothers’ physical health. These findings suggest that it may be useful to prepare parents to experience uncertainty. Clinicians may work with parents to identify coping skills that they typically use to manage stressful situations, and can identify ways that parents can plan to use these coping skills to manage the distress they are likely to experience as a result of the uncertain impact of the condition on their child. It may be useful to develop interventions to help parents identify and utilize coping skills that are specific to dealing with uncertainty. Such interventions are already being developed to teach skills for managing uncertainty to parents of children with diabetes (Hoff et al., 2005).
Interventions are likely to be most useful if they are based on an understanding of factors that contribute to parental uncertainty. Previous research indicates that lack of trust and confidence in medical professionals is associated with uncertainty (Casiday, 2006; Mishel, 1993). Thus, coping skills that are specific to dealing with chronic health conditions and uncertainty may involve parents working closely with medical professionals that they trust to gather and share information. By gathering information from trusted health professionals, parents may be able to reduce the extent to which they experience uncertainty. In addition, parents themselves can be encouraged to self-identify as experts on their particular child and the impact of the condition on their child. By working closely with medical professionals, the amount of information that is available to both parents and medical professionals may be maximized as well as the experience of alliance and partnership. This may reduce uncertainty, which could in turn reduce parent psychological and physical distress.
In conclusion, uncertainty about the impact of the health condition on the child’s daily life appears to lead over time to psychological symptoms, particularly for mothers. In turn, psychological symptoms lead to physical symptoms among parents of children with chronic health conditions.
Acknowledgments
Collection of the data used in this article was supported by a grant from the National Institute on Disability and Rehabilitation Research (H133890012). This research was supported by a Doctoral Dissertation Fellowship from the University of Minnesota awarded to the first author and by postdoctoral training grants from the National Institute of Mental Health (T32-MH15442) and the National Heart, Lung, and Blood Institute (F32-HL083687).
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/fsh.
REFERENCES
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Berge JM, Holm KE. Boundary ambiguity and parents with chronically ill children: Integrating theory and research. Family Relations. 2007;56:123–143. [Google Scholar]
- Bonner MJ, Hardy KK, Guill AB, McLaughlin C, Schweitzer H, Carter K. Development and validation of the Parent Experience of Child Illness. Journal of Pediatric Psychology. 2006;31:310–321. doi: 10.1093/jpepsy/jsj034. [DOI] [PubMed] [Google Scholar]
- Boss PG. Family Stress Management: A Contextual Approach. 2nd ed. Sage Publications; Thousand Oaks, CA: 2002. [Google Scholar]
- Boss P. Ambiguous loss theory: Challenges for scholars and practitioners. Family Relations. 2007;56:105–111. [Google Scholar]
- Boss P, Caron W, Horbal J, Mortimer J. Predictors of depression in caregivers of dementia patients: Boundary ambiguity and mastery. Family Process. 1990;29:245–254. doi: 10.1111/j.1545-5300.1990.00245.x. [DOI] [PubMed] [Google Scholar]
- Boss P, Greenberg J. Family boundary ambiguity: A new variable in family stress theory. Family Process. 1984;23:535–546. doi: 10.1111/j.1545-5300.1984.00535.x. [DOI] [PubMed] [Google Scholar]
- Caron W, Boss P, Mortimer J. Family boundary ambiguity predicts Alzheimer’s outcomes. Psychiatry. 1999;62:347–356. doi: 10.1080/00332747.1999.11024882. [DOI] [PubMed] [Google Scholar]
- Carroll JS, Olson CD, Buckmiller N. Family boundary ambiguity: A 30-year review of theory, research, and measurement. Family Relations. 2007;56:210–230. [Google Scholar]
- Casiday R. Uncertainty, decision-making and trust: Lessons from the MMR controversy. Community Practice. 2006;79:354–357. [PubMed] [Google Scholar]
- Chesler MA, Parry C. Gender roles and/or styles in crisis: An integrative analysis of the experiences of fathers of children with cancer. Qualitative Health Research. 2001;11:363–384. doi: 10.1177/104973230101100307. [DOI] [PubMed] [Google Scholar]
- Davidoff AJ. Identifying children with special health care needs in the National Health Interview Study: A new resource for policy analysis. Health Services Research. 2004;39:53–71. doi: 10.1111/j.1475-6773.2004.00215.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodgson JE, Garwick A, Blozis SA, Patterson JM, Bennett FC, Blum RW. Uncertainty in childhood chronic conditions and family distress in families of young children. Journal of Family Nursing. 2000;6:252–266. [Google Scholar]
- Gartstein MA, Short AD, Vannatta K, Noll RB. Psychosocial adjustment of children with chronic illness: An evaluation of three models. Journal of Developmental and Behavioral Pediatrics. 1999;20:157–163. doi: 10.1097/00004703-199906000-00004. [DOI] [PubMed] [Google Scholar]
- Garwick AW, Patterson JM, Meschke LL, Bennett FC, Blum RW. The uncertainty of preadolescents’ chronic health conditions and family distress. Journal of Family Nursing. 2002;8:11–31. [Google Scholar]
- Goble LA. The impact of a child’s chronic illness on fathers. Issues in Comprehensive Pediatric Nursing. 2004;27:153–162. doi: 10.1080/01460860490497787. [DOI] [PubMed] [Google Scholar]
- Grootenhuis MA, Last BF. Predictors of parental emotional adjustment to childhood cancer. Psycho-Oncology. 1997;6:115–128. doi: 10.1002/(SICI)1099-1611(199706)6:2<115::AID-PON252>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- Hoff AL, Mullins LL, Gillaspy SR, Page MC, Van Pelt JC, Cheney JM. An intervention to decrease uncertainty and distress among parents of children newly diagnosed with diabetes: A pilot study. Families, Systems, & Health. 2005;23:329–342. [Google Scholar]
- Ireys HT, Silver EJ. Perception of the impact of a child’s chronic illness: Does it predict maternal mental health? Developmental and Behavioral Pediatrics. 1996;17:77–83. [PubMed] [Google Scholar]
- Jessop DJ, Stein RE. Uncertainty and its relation to the psychological and social correlates of chronic illness in children. Social Science and Medicine. 1985;20:993–999. doi: 10.1016/0277-9536(85)90255-2. [DOI] [PubMed] [Google Scholar]
- Jöreskog KG, Sörbom D. LISREL 8: User’s reference guide. Scientific Software International; Chicago: 1997. [Google Scholar]
- Kline R. Principles and practice of structural equation modeling. Guilford; New York: 1998. [Google Scholar]
- Mastroyannopoulou K, Stallard P, Lewis M, Lenton S. The impact of childhood non-malignant life-threatening illness on parents: Gender differences and predictors of parental adjustment. Journal of Child Psychology & Psychiatry & Allied Disciplines. 1997;38:823–829. doi: 10.1111/j.1469-7610.1997.tb01600.x. [DOI] [PubMed] [Google Scholar]
- Mishel MH. The measurement of uncertainty in illness. Nursing Research. 1981;30:258–263. [PubMed] [Google Scholar]
- Mishel MH. Parents’ perception of uncertainty concerning their hospitalized child. Nursing Research. 1983;32:324–330. [PubMed] [Google Scholar]
- Mishel MH. Perceived uncertainty and stress in illness. Research in Nursing and Health. 1984;7:163–171. doi: 10.1002/nur.4770070304. [DOI] [PubMed] [Google Scholar]
- Mishel MH. Living with chronic illness: Living with uncertainty. In: Funk SG, Tornquist EM, Champagne MT, et al., editors. Key aspects of caring for the chronically ill. Springer; New York: 1993. pp. 46–58. [Google Scholar]
- Mu PF. Paternal reactions to a child with epilepsy: Uncertainty, coping strategies, and depression. Journal of Advanced Nursing. 2005;49:367–376. doi: 10.1111/j.1365-2648.2004.03300.x. [DOI] [PubMed] [Google Scholar]
- Mu P, Kuo H, Chang K. Boundary ambiguity, coping patterns and depression in mothers caring for children with epilepsy in Taiwan. International Journal of Nursing Studies. 2005;42:273–282. doi: 10.1016/j.ijnurstu.2004.07.002. [DOI] [PubMed] [Google Scholar]
- Mu P, Ma FC, Hwang B, Chao YM. Families of children with cancer: The impact on anxiety experienced by fathers. Cancer Nursing. 2002;25:66–73. doi: 10.1097/00002820-200202000-00012. [DOI] [PubMed] [Google Scholar]
- Mu P, Ma F, Ku S, Shu H, Hwang B, Kuo BI. Families of Chinese children with malignancy: The factors impact on mother’s anxiety. Journal of Pediatric Nursing. 2001;16:287–295. doi: 10.1053/jpdn.2000.25325. [DOI] [PubMed] [Google Scholar]
- Mu PF, Wong TT, Chang KP, Kwan SY. Predictors of maternal depression for families having a child with epilepsy. Journal of Nursing Research. 2001;9:116–126. [PubMed] [Google Scholar]
- Nagy S, Ungerer JA. The adaptation of mothers and fathers to children with cystic fibrosis: A comparison. Children’s Health Care. 1990;19:147–154. [Google Scholar]
- Neil-Urban S, Jones JB. Father-to-father support: Fathers of children with cancer share their experience. Journal of Pediatric Oncology Nursing. 2002;19:97–103. doi: 10.1177/104345420201900304. [DOI] [PubMed] [Google Scholar]
- Perrin EC, Newacheck P, Pless B, Drotar D, Gortmaker SL, Leventhal J, Perrin JM, Stein REK, Walker DK, Weitzman M. Issues involved in the definition and classification of chronic health conditions. Pediatrics. 1993;91:787–793. [PubMed] [Google Scholar]
- Silver EJ, Westbrook LE, Stein REK. Relationship of parental psychological distress to consequences of chronic health conditions in children. Journal of Pediatric Psychology. 1998;23(1):5–15. doi: 10.1093/jpepsy/23.1.5. [DOI] [PubMed] [Google Scholar]
- Staab D, Wenninger K, Gebert N, Rupprath K, Bisson S, Trettin M, Paul KD, Keller KM, Wahn U. Quality of life in patients with cystic fibrosis and their parents: What is important besides disease severity? Thorax. 1998;53:727–731. doi: 10.1136/thx.53.9.727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein REK, Bauman LJ, Westbrook LE, Coupley SM, Ireys T. Framework for identifying children who have chronic conditions: The case for a new definition. The Journal of Pediatrics. 1993;122:342–347. doi: 10.1016/s0022-3476(05)83414-6. [DOI] [PubMed] [Google Scholar]
- Stein RE, Jessop D. Functional Status II: A measure of child health status. Medical Care. 1990;28:1041–1055. doi: 10.1097/00005650-199011000-00006. [DOI] [PubMed] [Google Scholar]
- Svavarsdottir EK. Caring for a child with cancer: A longitudinal perspective. Journal of Advanced Nursing. 2005;50:153–161. doi: 10.1111/j.1365-2648.2005.03374.x. [DOI] [PubMed] [Google Scholar]
- Svavarsdottir EK, Rayens MK. Hardiness in families of young children with asthma. Journal of Advanced Nursing. 2005;50:381–390. doi: 10.1111/j.1365-2648.2005.03403.x. [DOI] [PubMed] [Google Scholar]
- Svavarsdottir EK, Rayens MK, McCubbin M. Predictors of adaptation in Icelandic and American families of young children with chronic asthma. Family & Community Health. 2005;28:328–350. doi: 10.1097/00003727-200510000-00006. [DOI] [PubMed] [Google Scholar]
- Tong HC, Kandala G, Haig AJ, Nelson VS, Yamakawa KSJ, Shin KY. Physical functioning in female caregivers of children with physical disabilities compared with female caregivers of children with a chronic medical condition. Archives of Pediatrics & Adolescent Medicine. 2002;156:1138–1142. doi: 10.1001/archpedi.156.11.1138. [DOI] [PubMed] [Google Scholar]
- Van Dyck PC, Kogan MD, McPherson MG, Weissman GR, Newacheck PW. Prevalence and characteristics of children with special health care needs. Archives of Pediatrics & Adolescent Medicine. 2004;158:884–890. doi: 10.1001/archpedi.158.9.884. [DOI] [PubMed] [Google Scholar]
- Ware JE, Sherbourne CD. The MOS 36-item short-form survey (SF-36): I. Conceptual framework and item selection. Medical Care. 1992;30:473–483. [PubMed] [Google Scholar]