Abstract
Purpose
Laparoscopic simple prostatectomy was recently developed to treat voluminous benign prostatic hyperplasia (BPH). We describe the surgical technique and assess the feasibility of laparoscopic simple prostatectomy through our early experience.
Materials and Methods
The medical records of 11 patients who underwent laparoscopic simple prostatectomy between March 2008 and January 2010 were retrospectively analyzed. The subjects were limited to the patients who satisfied the following conditions: prostate volume was at least 75 g, acute urinary retention repeatedly occurred or maximal flow rate (Qmax) was at most 10 ml/s, and International Prostate Symptom Score (IPSS) was at least 12. The surgery was performed by the laparoscopic extraperitoneal approach with a transcapsular route. Feasibility was assessed by objective operative parameters (reconversion, operating time, and blood loss) and perioperative complications. Data on short-term follow-up were also available.
Results
The mean age of the patients was 70.6 years. Mean preoperative prostate-specific antigen and prostate volume were 6.1 ng/ml and 109.3 cc, respectively. Mean operation time was 191.9 minutes and estimated blood loss was 390.9 cc. The resected adenoma weighed on average 72.4 g. No conversion to open surgery was required. Mean preoperative IPSS and quality of life (QoL) scores were 26.86 and 4.86. Mean Qmax, measured before the surgery, was 4.5 ml/s and residual urine was 106 ml. Mean postoperative IPSS and QoL scores were 4.2 and 1.5. After the surgery, mean Qmax was 15.5 ml/s and residual urine was 24.1 ml.
Conclusions
In the case of voluminous BPH, laparoscopic retropubic simple prostatectomy is expected to be a useful treatment on the condition that the learning curve can be overcome with clinical experience.
Keywords: Laparoscopy, Prostate, Prostatectomy, Prostatic hyperplasia
INTRODUCTION
Benign prostatic hyperplasia (BPH) is one of the most common diseases in middle-aged and senescent males, and the incidence and importance of BPH have increased as the aged population has increased. As a result, treatments have been diversified and continuously advanced. Among them, transurethral resection of the prostate (TURP) has been recognized as the standard of surgical treatments and has been effective for patients with BPH. In rare cases, TURP is performed on patients whose prostates are voluminous, but in most cases, it is applied to small to moderate-sized BPH. In the case of an excessively voluminous prostate, open simple prostatectomy is performed because complications, such as transurethral resection syndrome or hemorrhage, can occur with TURP and postoperative symptoms may not easily improve [1]. Despite the increasing popularity of holmium laser enucleation of the prostate (HoLEP) and evidence that the technique may be superior to conventional treatment modalities [2], open simple prostatectomy remains the procedure of choice for prostate adenomas too large for safe endoscopic resection. Recently, however, laparoscopic surgeries have been technically advanced and laparoscopic simple prostatectomy has been performed by many operators [2-5].
In this report, we describe the surgical technique and assess the feasibility of laparoscopic retropubic simple prostatectomy though our initial experience.
MATERIALS AND METHODS
1. Materials and methods
This study was conducted on 11 consecutive patients with BPH who underwent laparoscopic retropubic simple prostatectomy between March 2008 and January 2010 in our hospital. All operations were performed by a single surgeon. The subjects were limited to the patients who satisfied the following conditions: the prostate volume was at least 75 g, acute urinary retention repeatedly occurred or the maximal urine flow rate (Qmax) was at most 10 ml/s, and the International Prostate Symptom Score (IPSS) was at least 12.
Before the surgery, history taking, physical examination, digital rectal examination (DRE), routine lab tests, IPSS, transrectal ultrasonography (TRUS), prostate-specific antigen (PSA) measurement, and uroflowmetry were performed. IPSS and uroflowmetry were performed again 1 month after the surgery for comparison with the preoperative data.
For the patients whose PSA values were 4 and over or who had any other risk factor (nodule on the DRE or hypoechoic lesion on TRUS), prostate biopsy was performed before the surgery to rule out cancer. The histopathologic analysis of the specimens demonstrated BPH in all cases.
Statistical data were analyzed by use of SPSS (Statistical Package for the Social Sciences; ver. 12.0) with Spearman's rank correlation analysis and the paired t-test. p-values of <0.05 were considered to be statistically significant.
2. Surgical technique
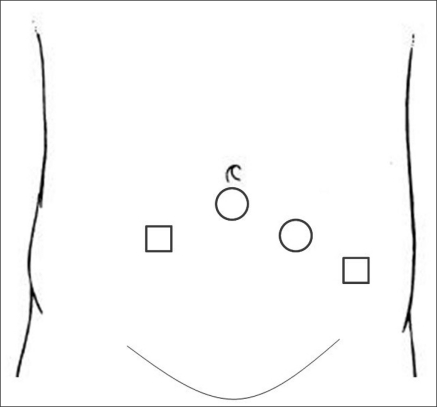
Laparoscopic retropubic simple prostatectomy was performed with the patients under general anesthesia in the Trendelenburg position with bilateral arms at each side. The surgery was performed as follows. A 20 French 3-way Foley catheter was introduced into the bladder, and the skin was incised 1 to 1.5 cm along the fold beneath the umbilicus. Then, the anterior sheath of the rectus abdominis muscle was transversely incised. After incision, the rectus muscle was exposed and spread bilaterally to expose the posterior sheath. Digital dissection of the preperitoneal space was performed. A balloon dilatator with a 10 mm-trocar (Space Maker™ Plus Dissector System, Tyco Healthcare Group LP, USA) was inserted between the rectus abdominis muscle and the posterior sheath, and the balloon was inflated with air to get enough extraperitoneal space under the direct vision. In this process, four trocars were used in all. The 10 mm-trocar was used as the camera port, after being separated from the dilatator. The other 10 mm port was set up on the border of the left rectus abdominis muscle, and a 5 mm port was located medially 2 fingers from the left anterior superior iliac. The other 5 mm port was placed on the border of the right rectus abdominis muscle (Fig. 1).
FIG. 1.
Port placement for extraperitoneal laparoscopic prostatectomy. ○: 10 mm port, □: 5 mm port.
Extraperitoneal dissection of the space of Retzius was performed and the endopelvic fascia was not opened. After the Retzius space and the fat covering the prostatic capsule were completely dissected, the boundary between the bladder and the prostate was clearly identified by moving the Foley catheter.
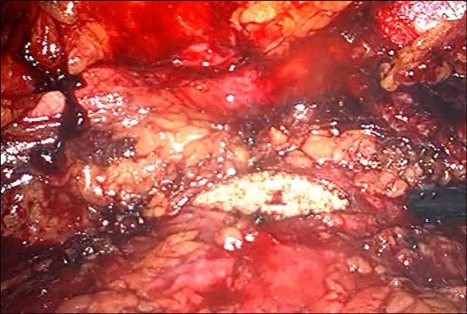
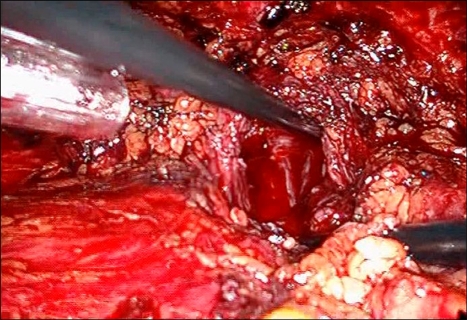
The superficial venous complex that runs the anterior surface of the prostate was carefully coagulated with bipolar electrocautery cranially and far away from the puboprostatic ligaments. Then a 2 or 3 cm incision was made on the anterior part of the prostatic capsule. The capsular incision was deepened with the aid of J-hook electrocautery and bipolar electrocautery until the plane between the surgical prostate capsule and the adenomatous tissue was exposed (Fig. 2). The adenoma was dissected along the surgical capsular plane in the same fashion as the open procedure using the endoscopic scissors and the suction irrigation cannula. Once the catheter was identified, the dissection proceeded until the whole adenomatous tissue had been freed. We divided the adenomatous tissue into two parts corresponding to the lobes (right and left) to ease its dissection and posterior excision (Fig. 3). After excision of the adenoma, the specimens were placed outside the capsule in the lateral iliac space. The bleeding of the prostatic capsule and prostatic fossa was controlled by the use of bipolar electrocautery (Fig. 4). The anterior prostatic capsule was closed by two Vicryl 3-0 running sutures each initiated at the external edges of the capsular incision and ligated at the midpoint.
FIG. 2.
Transverse incision of the anterior prostatic capsule.
FIG. 3.
Enucleation of the adenoma by laparoscopic dissection.
FIG. 4.
After removal of the adenoma, the prostatic fossa is exposed.
Saline solution was irrigated through the Foley catheter, and the bladder was filled with the saline solution to check whether the sutured region leaked. A Jackson-Pratt drain was inserted, and the detached adenoma was placed in the endobag sac. The specimen was finally removed through the 10 mm port site beneath the umbilicus. As for a large adenoma, a wider dissection was applied to allow for an intact retrieval.
RESULTS
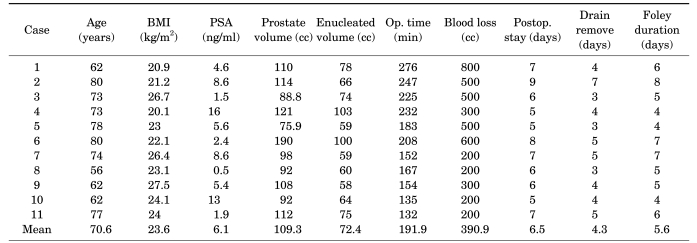
All of the laparoscopic procedures were successfully performed without any open conversion. The mean age of the patients was 70.6 years (range, 56-80 years) and their mean BMI was 23.6 kg/m2. The mean preoperative PSA was 6.1 ng/ml (range, 0.5-15.6 ng/ml) and the mean prostate volume, measured by TRUS, was 109.3 cc (range, 75.9-190 cc). It took on average 191.9 minutes (range, 132-276 minutes) to complete the surgery, and the mean blood loss was 390.9 ml (range, 200-800 ml). Two patients received a blood transfusion (Table 1). The period of postoperative hospitalization was 6.5 days (range, 5-9 days), and the Foley catheter and the drain were indwelled for 5.6 days (range, 4-8 days) and 4.3 days (range, 3-7 days), respectively. The mean weight of the resected adenomas was 72.4 g (range, 58-103 g). The mean enucleation weight of the prostate was 72.4 g, which was 66.2% of the preoperative TRUS-measured mean prostate volume of 109.3 cc.
TABLE 1.
Patient characteristics and operative results
BMI: body mass index, PSA: prostate-specific antigen, Postop. stay: postoperative hospital stay
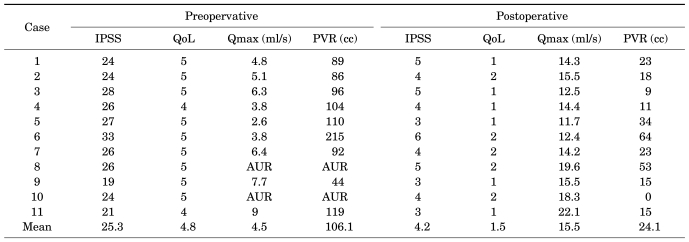
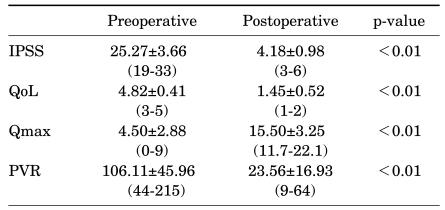
The mean maximal flow rate, measured before the surgery, was 4.5 ml/s (range, 2.6-7.7 ml/s). The mean post-void residual urine was 106 ml (range, 44-215 ml) and the mean IPSS and quality of life (QoL) scores were 25.3 and 4.8, respectively. At 1 month after surgery, the mean maximal flow rate was 15.5 ml/s (range, 11.7-22.1 ml/s), and the mean post-void residual urine was 24.1 ml (range, 0-64 ml). The mean IPSS and QoL scores were 4.2 and 1.5, respectively (Table 2).
TABLE 2.
Comparison of preoperative and postoperative data
IPSS: International Prostate Symptom Score, QoL: quality of life, Qmax: maximal urine flow rate, PVR: post-void residual urine, AUR: acute urinary retention
There were no major intraoperative or anesthetic complications. Subcutaneous emphysema and incontinence occurred in 2 cases and 3 cases, respectively. Subcutaneous emphysema was altered for the better by conservative treatments, and incontinence turned out to be better at the follow-up performed 1 month after the surgery. In a patient who had taken an anticoagulant because of heart disease, hematuria occurred 3 weeks after the surgery, which was treated by transurethral resection (TUR) coagulation. IPSS and QoL were markedly improved after the surgery, and the results were statistically significant. Also, statistically significant changes occurred in the maximal flow rate and the postvoid residual urine after the surgery, excluding 2 cases in which acute urinary retention occurred without data (Table 2, 3).
TABLE 3.
Preoperative and postoperative data as mean and standard deviation (Mean±SD)
IPSS: International Prostate Symptom Score, QoL: quality of life, Qmax: maximal urine flow rate, PVR: post-void residual urine
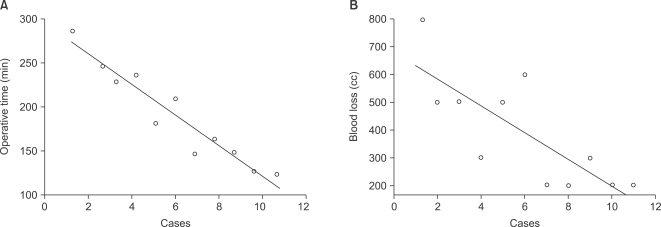
The operation time (Spearman's rho correlation coefficient=-0.955, p<0.001) and the estimated blood loss (Spearman's rho correlation coefficient=-0.786, p=0.004) were significantly shortened and reduced as operators have gained experience (Fig. 5).
FIG. 5.
Operative time and estimated blood loss for each patient. (A) Operative time (Spearman's rho correlation coefficient=-0.955, p<0.001), (B) Estimated blood loss (Spearman's rho correlation coefficient=-0.786, p=0.004).
DISCUSSION
When selecting the appropriate surgical approach in an individual with symptomatic BPH, prostate gland size is an important consideration. For large-sized BPH, open simple prostatectomy has conventionally been performed, but bipolar TURP and photoselective vaporization of the prostate (PVP) have each been applied to prostates weighing 80 g and above [1].
There was a report that bipolar TURP was effective for patients whose prostates weighed 80 g and over [1]. On the other hand, it was also reported that TURP increased morbidity in cases where the prostate weighed 45 g and over, where the surgery took 90 minutes and over, where the patient was aged 80 years and over, and where the patient had a history of acute urinary retention [3,6,7]. In prostates weighing 30 to 80 g, TURP has been recognized as the gold standard [8]. However, the problem is that TURP is apt to cause complications such as transurethral resection syndrome and bleeding, and the procedure takes more time as the prostate size increases. Given the fact that open simple prostatectomy is superior to TURP in recurrence rate and can remove the prostatic adenoma perfectly and is free from the transurethral resection syndrome, the open simple prostatectomy procedure is still more effective for patients whose prostates weigh 75 g and over [9].
Although it was reported that PVP was effective for treating prostates weighing 60 g [10,11], it is usually effective for small or moderate prostates. It has the disadvantage that the tissue cannot be taken after the surgery, and it also causes complications in large BPH [12].
More recently, HoLEP has been used for giant prostatomegaly, even in prostates in excess of 100 g. Nevertheless, at many centers, open simple prostatectomy currently remains the technique of choice in most patients with hugely enlarged BPH [3,13-15]. Open simple prostatectomy accounts for 14% to 32% of the total invasive procedures for BPH in Europe [5,16-18]. However, open simple prostatectomy has disadvantages; it causes considerable bleeding during the surgery, it takes the patient a long time to recover, and it leaves a big scar.
As laparoscopic surgery has been technically advanced, it has been applied to simple prostatectomy in place of open simple prostatectomy. Laparoscopic simple prostatectomy causes less intraoperative bleeding than does open simple prostatectomy, thanks in part to the wide eyeshot and high-pressure CO2 [19]. In addition, it has the merits of minor surgical scars, shorter hospital stay, less analgesic utilization, and more rapid return to physical activities [9].
Laparoscopic simple prostatectomy can be useful in cases in which the prostate is too voluminous to be removed by TURP in a short time, in which the BPH is accompanied by bladder diverticula or bladder stones, in which it is difficult to insert the urethroscope because of a serious urethral stricture, and in which the patient has difficulty in assuming the lithotomy position.
The surgical approach is divided into extraperitoneal and intraperitoneal approaches, and the surgical method is divided according to internal incision, transcapsular route (Millin procedure), and transvesical-prostatic route [2-4].
We adopted the extraperitoneal approach because of the expectation of rapid postoperative recovery and the rare possibility of bowel complications. We used the Millin procedure (transversely incised the prostatic capsule). An important technical caution is that subcapsular dissection should proceed in close contact with the whitish surface of the prostate adenoma bluntly [3].
In 2002, Mariano et al performed the first laparoscopic simple prostatectomy on a patient with BPH whose prostate weighed 173 g on TRUS. The prostatic capsule and the bladder neck were vertically incised through the transperitoneal approach, and the resected adenoma was 120 g. The estimated blood loss and the operation time were 800 ml and 225 minutes, respectively [20].
In 2004, van Velthoven et al performed a laparoscopic extraperitoneal adenomectomy (Millin's procedure) on 18 patients [5]. The surgery was to transversely incise the prostatic capsule. The operation time and the estimated blood loss were 145 minutes and 192 ml, respectively. They reported that the method was effective at reducing blood loss and shortening the time taken for the catheter to indwell.
Nadler et al performed a preperitoneal laparoscopic simple prostatectomy, making a transverse incision on the bladder neck just proximal to the prostatic capsule [21]. The operation time and the blood loss were 350 minutes and 300 ml, respectively.
In 2005, Sotelo et al performed prostatectomy on 17 patients through the laparoscopic extraperitoneal or intraperitoneal approach [3]. In particular, in the last 12 cases, they applied incisions to the bladder neck just proximal to the prostatovesical junction, which was helpful in reducing blood loss.
Mariano et al reported their 6-year experience in laparoscopic simple prostatectomy for BPH and concluded that it significantly improved IPSS, Qmax, and QoL after the surgery [9].
In 2006, Baumert et al compared 30 cases of laparoscopic prostatectomy with 30 cases of open prostatectomy [2]. They reported that the laparoscopic surgery was statistically superior to the open surgery in operation time, blood loss, specimen weight, irrigation time, catheterization time, and hospital stay.
In Korea, Kim et al applied a transverse incision to the bladder anterior walls of 10 patients and applied 360-degree incisions to the bladder necks [22]. Adenomas were resected through the transvesical approach. The maximal flow rate and IPSS were improved after the surgery, and serious complications such as incontinence did not occur.
Baumert et al reported that in the case of the Millin procedure, it was difficult to perform a capsular incision on the large glands or large prostatic lobe, and thus the transvesical-prostatic approach tended to be preferred. But at the same time, they reported that the two methods did not show significant differences in operation time, blood loss, catheterization time, or hospital stay [2].
In this study, a transcapsular incision (Millin procedure) was applied, which was performed even on patients who had large glands or large median prostatic lobes, without particular difficulties. In the surgeries performed by us, mean operation time was longer than reported in other papers, and also mean blood loss was greater. However, operation time and blood loss have been remarkably shortened and reduced as the number of cases has increased. Actually, the first surgery took 276 minutes and blood loss was 800 cc, but in the last surgery, these variables were 132 minutes and 200 cc, respectively. These improvements imply that with time, better results may be achieved. Although it was too difficult to compare our data with open simple prostatectomy because of the small number of our laparoscopic experiences, laparoscopic surgeries tend to produce better results for recovery time, blood loss, and catheterization time over the results of open simple prostatectomy.
Recently, HoLEP has produced good results in large-sized BPH. Particularly in terms of hospital stay, catheterization time, and blood loss, it has shown better results than open simple prostatectomy and TURP [13]. However, it is not easy for operators to overcome the learning curve until they can shorten the operation time, and a given time should be spent on morcellation after enucleation. Moreover, not all centers can afford to be equipped with the HoLEP instrument because of its high cost. Meanwhile, laparoscopic surgeries have been used widely at the urologic part. Accordingly, it may be possible for operators who have a lot of experience in laparoscopic surgery to substitute this for open surgery.
The limitations of this study are the small number of cases and the short follow-up period. More cases and long-term data are needed to clarify the usefulness of laparoscopic retropubic simple prostatectomy.
CONCLUSIONS
Laparoscopic retropubic simple prostatectomy is expected to achieve the merits of both open surgery and laparoscopic surgery, including perfect removal of the adenoma, short recovery time, and wide eyeshot. However, the operators' overcoming the learning curve is a prerequisite for shortening the operation time and reducing the perioperative morbidities. Although long-term data and further comparative studies are needed, we believe that laparoscopic retropubic simple prostatectomy may be a useful treatment option for patients with voluminous BPH, on the condition that the operators overcome the learning curve by gaining a lot of clinical experience.
Footnotes
See Editorial on page 329.
The authors have nothing to disclose.
References
- 1.Baek M, Paick SH, Lee BK, Kang MB, Lho YS, Jung SI, et al. The efficacy of bipolar transurethral resection of the prostate in patients with large prostates (>80 g) and analysis of the postoperative results based on the resection ratio. Korean J Urol. 2008;49:1087–1093. [Google Scholar]
- 2.Baumert H, Ballaro A, Dugardin F, Kaisary AV. Laparoscopic versus open simple prostatectomy: a comparative study. J Urol. 2006;175:1691–1694. doi: 10.1016/S0022-5347(05)00986-9. [DOI] [PubMed] [Google Scholar]
- 3.Sotelo R, Spaliviero M, Garcia-Segui A, Hasan W, Novoa J, Desai MM, et al. Laparoscopic retropubic simple prostatectomy. J Urol. 2005;173:757–760. doi: 10.1097/01.ju.0000152651.27143.b0. [DOI] [PubMed] [Google Scholar]
- 4.Han M, Partin AW. Retropubic and suprapubic open prostatectomy. In: Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh urology. 9th ed. Philadelphia: Saunders; 2007. pp. 2845–2853. [Google Scholar]
- 5.van Velthoven R, Peltier A, Laguna MP, Piechaud T. Laparoscopic extraperitoneal adenomectomy (Millin): pilot study on feasibility. Eur Urol. 2004;45:103–109. doi: 10.1016/j.eururo.2003.07.002. [DOI] [PubMed] [Google Scholar]
- 6.Tubaro A, Vicentini R, Renzetti R, Miano L. Invasive and minimally invasive treatment modalities for lower urinary tract symptoms: what are the relevant differences in randomised controlled trials? Eur Urol. 2000;7(Suppl):38. doi: 10.1159/000052397. [DOI] [PubMed] [Google Scholar]
- 7.Mebust WK, Holtgrewe HL, Cockett AT, Peters PC. Transurethral prostatectomy: immediate and postoperative complications. A cooperative study of 13 participating institutions evaluating 3,885 patients. 1989. J Urol. 2002;167:999–1002. [PubMed] [Google Scholar]
- 8.Madersbacher S, Alivizatos G, Nordling J, Sanz CR, Emberton M, de la Rosette JJ. EAU 2004 guidelines on assessment, therapy and follow-up of men with lower urinary tract symptoms suggestive of benign prostatic obstruction (BPH guidelines) Eur Urol. 2004;46:547–554. doi: 10.1016/j.eururo.2004.07.016. [DOI] [PubMed] [Google Scholar]
- 9.Mariano MB, Tefilli MV, Graziottin TM, Morales CM, Goldraich IH. Laparoscopic prostatectomy for benign prostatic hyperplasia--a six-year experience. Eur Urol. 2006;49:127–131. doi: 10.1016/j.eururo.2005.09.018. [DOI] [PubMed] [Google Scholar]
- 10.Alivizatos G, Skolarikos A, Chalikopoulos D, Papachristou C, Sopilidis O, Dellis A, et al. Transurethral photoselective vaporization versus transvesical open enucleation of prostatic adenomas >80 ml: 12-mo results of a randomized prospective study. Eur Urol. 2008;54:427–437. doi: 10.1016/j.eururo.2007.11.044. [DOI] [PubMed] [Google Scholar]
- 11.Park JH, Son H, Paick JS. Comparative analysis of the efficacy and safety of photoselective vaporization of the prostate for treatment of benign prostatic hyperplasia according to prostate size. Korean J Urol. 2010;51:115–121. doi: 10.4111/kju.2010.51.2.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hwang CH, Cho CK, Lee YK, Hong SJ. Comparative analysis of short-term efficacy and complication of photoselective vaporization for benign prostatic hyperplasia which was classified by prostate size. Korean J Urol. 2007;48:826–831. [Google Scholar]
- 13.Kuntz RM, Lehrich K, Ahyai SA. Holmium laser enucleation of the prostate versus open prostatectomy for prostates greater than 100 grams: 5-year follow-up results of a randomised clinical trial. Eur Urol. 2008;53:160–166. doi: 10.1016/j.eururo.2007.08.036. [DOI] [PubMed] [Google Scholar]
- 14.Moody JA, Lingeman JE. Holmium laser enucleation for prostate adenoma greater than 100 gm.: comparison to open prostatectomy. J Urol. 2001;165:459–462. doi: 10.1097/00005392-200102000-00025. [DOI] [PubMed] [Google Scholar]
- 15.AUA Practive Guidelines Committee. AUA guideline on management of benign prostatic hyperplasia (2003). Chapter 1: diagnosis and treatment recommendations. J Urol. 2003;170:530–547. doi: 10.1097/01.ju.0000078083.38675.79. [DOI] [PubMed] [Google Scholar]
- 16.Serretta V, Morgia G, Fondacaro L, Curto G, Lo bianco A, Pirritano D, et al. Open prostatectomy for benign prostatic enlargement in southern Europe in the late 1990s: a contemporary series of 1800 interventions. Urology. 2002;60:623–627. doi: 10.1016/s0090-4295(02)01860-5. [DOI] [PubMed] [Google Scholar]
- 17.Tubaro A, Montanari E. Management of symptomatic BPH in Italy: who is treated and how? Eur Urol. 1999;36(Suppl 3):28–32. doi: 10.1159/000052346. [DOI] [PubMed] [Google Scholar]
- 18.Lukacs B. Management of symptomatic BPH in France: who is treated and how? Eur Urol. 1999;36(Suppl 3):14–20. doi: 10.1159/000052344. [DOI] [PubMed] [Google Scholar]
- 19.Rey D, Ducarme G, Hoepffner JL, Staerman F. Laparoscopic adenectomy: a novel technique for managing benign prostatic hyperplasia. BJU Int. 2005;95:676–678. doi: 10.1111/j.1464-410X.2005.05361.x. [DOI] [PubMed] [Google Scholar]
- 20.Mariano MB, Graziottin TM, Tefilli MV. Laparoscopic prostatectomy with vascular control for benign prostatic hyperplasia. J Urol. 2002;167:2528–2529. [PubMed] [Google Scholar]
- 21.Nadler RB, Blunt LW, Jr, User HM, Vallancien G. Preperitoneal laparoscopic simple prostatectomy. Urology. 2004;63:778–779. doi: 10.1016/j.urology.2003.12.021. [DOI] [PubMed] [Google Scholar]
- 22.Kim BH, Ryu DS, Oh TH. Initial experience of laparoscopic simple prostatectomy in patients with large benign prostatic hyperplasia. Korean J Urol. 2008;49:418–423. [Google Scholar]