Abstract
Purpose
We investigated the effects of obesity on prostate volume (PV) and lower urinary tract symptoms (LUTS) in Korean men.
Materials and Methods
From December 2007 to 2009, a total of 10,383 ostensibly healthy Korean men aged ≥50 years visited our health promotion center for a routine check-up. Among them, 872 men who wanted a prostate evaluation were enrolled in this study. All men underwent detailed clinical evaluations with the International Prostate Symptom Score (IPSS) questionnaire. Anthropometric measurements, including height, weight, and waist and hip circumferences, were determined. A blood sample was obtained for serum prostate-specific antigen (PSA) measurement. Thereafter, a digital rectal examination and transrectal ultrasound were performed.
Results
In total, 465 men with moderate to severe LUTS (IPSS≥8 points) were included in this prospective study. The participants' mean age was 57.2 years. Multivariate analysis demonstrated that only waist circumference was a significant factor in predicting PV besides age and serum PSA. The univariate analysis showed no statistically significant relations between any of the obesity-related parameters and LUTS. The PV was also not correlated with LUTS.
Conclusions
Central obesity is the more important predictor of PV than overall obesity. There are no significant relations between obesity-related parameters and LUTS.
Keywords: Abdominal obesity, Prostate, Prostatic hyperplasia
INTRODUCTION
Lower urinary tract symptoms (LUTS), often the result of benign prostatic hyperplasia (BPH), are common among older men and have a negative impact on their quality of life [1]. Multiple studies have reported that obese men have a larger prostate volume (PV) than do nonobese men [2-6], and recently some studies have revealed that a relationship exists between obesity and LUTS [2,4,7,8]. The suggested pathophysiology was hyperinsulinemia [9-11], caused by tissue insulin resistance, which stimulates the autonomic nervous system, particularly the sympathetic nervous system [12]. The overactivity of the sympathetic nervous system results in bladder outlet obstruction and LUTS.
The Korean National Health and Nutrition Surveys reported an increase in the prevalence of obesity from 1995 to 2001 [13]. The prevalence of clinical BPH was reported to be from 10.6% to 31% in men over 50 years of age, with an age-related increase seen in South Korea [14,15]. However, there are insufficient data on the effect of obesity on LUTS in Korean men. Therefore, in this cross-sectional study, we investigated the effects of obesity on PV and LUTS in Korean men.
MATERIALS AND METHODS
From December 2007 to 2009, a total of 10,383 ostensibly healthy Korean men aged ≥50 years visited our health promotion center for a routine check-up. Among them, 872 men who wanted a prostate evaluation were enrolled in this study.
All men underwent detailed clinical evaluations with the International Prostate Symptom Score (IPSS) questionnaire. Anthropometric measurements, including height, weight, and waist and hip circumferences, were determined. A blood sample was obtained for serum prostatespecific antigen (PSA) measurement (AxSYM, Abbott Laboratories, Abbott Park, IL, USA). Thereafter, a digital rectal examination (DRE) and transrectal ultrasound was performed. Body mass index (BMI) was calculated as the weight divided by square of the height, and waist-to-hip ratio (WHR) was determined as the waist circumference divided by the hip circumference.
The exclusion criteria of this study were mild LUTS (IPSS<8); the use of medications affecting prostate growth, such as antiandrogens and 5-α-reductase inhibitors; a high serum PSA level of >4.0 ng/ml; abnormal findings on the DRE; pyuria (white blood cells >5 on urinalysis), the presence of neurogenic bladder dysfunction; confirmed prostate cancer; acute or chronic urinary retention status; acute or chronic prostatitis within the previous 3 months; a history of recurrent urinary tract infection or bladder stones; and previous surgical intervention related to BPH.
Univariate analysis by Pearson's correlation coefficient was used to test the linearity of the relationships among the variables. Multiple linear regression analysis was used to test the linear effect of variables in predicting PV. All statistical analysis was performed by using commercially available software (SPSS, version 14.0 KO, Chicago, IL, USA). A p-value of <0.05 was considered statistically significant.
RESULTS
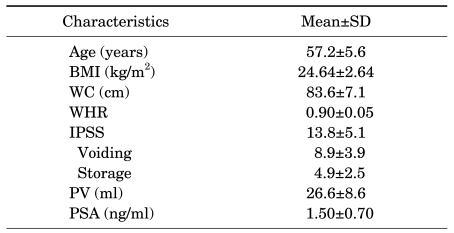
In total, 465 men with LUTS (IPSS≥8 points) and aged ≥50 years were included in this prospective study. The participants' mean age was 57.2 years (Table 1).
TABLE 1.
Characteristics of the study population
BMI: body mass index, WC: waist circumference, WHR: waist to hip ratio, IPSS: International Prostate Symptom Score, PV: prostate volume, PSA: prostate-specific antigen
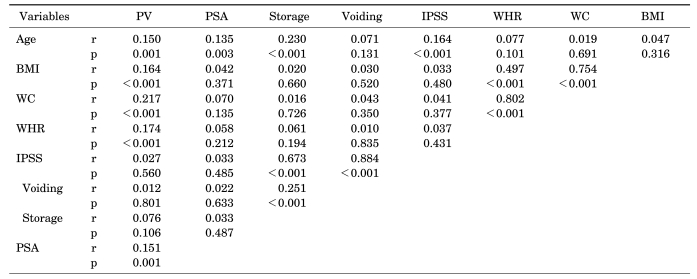
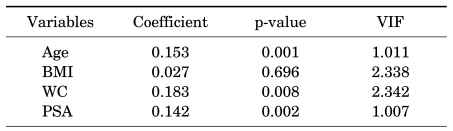
The univariate analysis showed that the PV was positively correlated with all obesity-related parameters: BMI, waist circumference, and WHR (Table 2). However, multiple linear regression analysis demonstrated that, among the obesity-related parameters, only waist circumference was a significant factor in predicting PV (Table 3).
TABLE 2.
Univariate correlation analysis between various parameters
PV: prostate volume, PSA: prostate-specific antigen, IPSS: International Prostate Symptom Score, WHR: waist to hip ratio, WC: waist circumference, BMI: body mass index, r: correlation coefficient, p: as determined by Pearson's correlation coefficient
TABLE 3.
Multiple linear regression analysis to determine independent predictors of PV
PV: prostate volume, VIF: variation inflation factor, BMI: body mass index, WC: waist circumference, PSA: prostate-specific antigen
We then examined the correlation between obesity parameters and LUTS represented by IPSS. The univariate analysis showed that there were no statistically significant relationships between obesity-related parameters and LUTS (Table 2). Voiding and storage symptoms also revealed no correlation with any obesity-related parameters. PV was not correlated with any type of LUTS.
DISCUSSION
LUTS comprise a spectrum of voiding and storage symptoms, which in men are generally considered a sign of clinically significant BPH [16]. A review of the available data appears to support a strong independent relationship between obesity and BPH or LUTS.
Over the past two decades, many different groups have investigated the influence of obesity on the development of BPH and LUTS with conflicting results [1,17-22]. Most of these groups have concluded that overall obesity, abdominal obesity, and/or WHR can increase the risk of BPH and LUTS, at least to some degree.
The Veterans Administration Normative Aging Study reported that increased BMI was a significant predictor of a clinical diagnosis of BPH [17]. Rohrmann et al examined the association between obesity and LUTS in the National Health and Nutrition Examination Survey (NHANES) III cohort [1]. They found that an increase in BMI after age 25 was positively associated with LUTS. They also noted that men with a larger waist circumference (>102 cm) were more likely to have LUTS than were men with a smaller waist circumference. Kristal et al examined several modifiable lifestyle factors related to the development of symptomatic BPH in 5,600 men enrolled in the placebo arm of the Prostate Cancer Prevention Trial who were followed for 7 years [18]. They reported significant increases in symptomatic BPH (IPSS>14), with abdominal obesity as measured by WHR. Laven et al examined a cohort of 27,858 Swedish men and found that low birth weight and abdominal obesity, but not BMI, were associated with an increased risk of LUTS [19]. Together, these results suggested that weight gain and central adiposity in adulthood were associated with a higher prevalence of LUTS.
However, these results may not be universally applicable. Joseph et al looked at modifiable risk factors for LUTS specifically in black men and found no greater risk with increasing BMI [10]. Gupta et al followed 1206 Vietnam veterans from the Air Force Health Study for an average period of 15 years and showed no increased risk of BPH or LUTS in men with metabolic syndrome compared with that in men without it [3].
To our knowledge, only three studies have assessed the relationship between obesity and LUTS in Korean men [20-22], and all were done in a cross-sectional manner. One was a community-based study performed in 348 elderly men whose age was over 65 years, in which no relationship between obesity and LUTS was shown [20]. The second study also showed that there was no association between metabolic syndrome and voiding dysfunction in men older than in their 60 s [21]. The third study by Lee et al involving 602 patients (aged ≥40 years) with BPH or LUTS who were attending a urology clinic, provided evidence that central obesity is the predictor of LUTS correlated with BPH [22]. That study reported that Korean men with a waist circumference of >90 cm experienced a 1.36-fold increased risk of severe LUTS compared with those with a waist circumference of ≤90 cm. They also observed that storage symptoms, such as nocturia and urgency, increased with increasing PV in men with a waist circumference of >90 cm [22].
Our study of 465 men recruited through the health promotion center showed that PV was positively correlated with central obesity, as represented by waist circumference, but not with BMI, which represented overall obesity. There was no significant relationship between obesity-related parameters and LUTS. Our study might have been affected by selection bias due to the heterogeneous eligibility of the study population. This may be why our study population showed a relatively small PV (mean: 26.6 ml) compared with the PV values reported in the three studies mentioned above [20-22].
Recent studies concerning the pathophysiology of BPH have suggested that in addition to the conventional risk factors, such as age, family history, and androgen activity, newly identified risk factors, such as diet and obesity, may have a major role in the development of BPH [23]. However, most of theses studies were performed in Western persons. We think it may be difficult to directly adopt the results of those studies to Korean persons, because differences in the incidence of BPH, LUTS, and obesity exist among different ethnic groups. Moreover, obesity defined by the Adult Treatment Panel III is much more rigid for Western men (>102 cm of waist circumference) than for Orientals (>90 cm of waist circumference).
We need another large, longitudinal, prospective, community-based study to fully reveal the relationship between obesity and BPH or LUTS in Korean men.
CONCLUSIONS
Our data showed that PV was positively correlated with central obesity, as represented by waist circumference, but not with BMI, which represented overall obesity. There was no significant relationship between obesity-related parameters and LUTS.
Footnotes
The authors have nothing to disclose.
References
- 1.Rohrmann S, Smit E, Giovannucci E, Platz EA. Associations of obesity with lower urinary tract symptoms and noncancer prostate surgery in the Third National Health and Nutrition Examination Survey. Am J Epidemiol. 2004;159:390–397. doi: 10.1093/aje/kwh060. [DOI] [PubMed] [Google Scholar]
- 2.Hammarsten J, Högstedt B, Holthuis N, Mellström D. Components of the metabolic syndrome-risk factors for the development of benign prostatic hyperplasia. Prostate Cancer Prostatic Dis. 1998;1:157–162. doi: 10.1038/sj.pcan.4500221. [DOI] [PubMed] [Google Scholar]
- 3.Gupta A, Gupta S, Pavuk M, Roehrborn CG. Anthropometric and metabolic factors and risk of benign prostatic hyperplasia: a prospective cohort study of Air Force veterans. Urology. 2006;68:1198–1205. doi: 10.1016/j.urology.2006.09.034. [DOI] [PubMed] [Google Scholar]
- 4.Ozden C, Ozdal OL, Urgancioglu G, Koyuncu H, Gokkaya S, Memis A. The correlation between metabolic syndrome and prostatic growth in patients with benign prostatic hyperplasia. Eur Urol. 2007;51:199–203. doi: 10.1016/j.eururo.2006.05.040. [DOI] [PubMed] [Google Scholar]
- 5.Xie LP, Bai Y, Zhang XZ, Zheng XY, Yao KS, Xu L, et al. Obesity and benign prostatic enlargement: a large observational study in China. Urology. 2007;69:680–684. doi: 10.1016/j.urology.2006.12.030. [DOI] [PubMed] [Google Scholar]
- 6.Putnam SD, Cerhan JR, Parker AS, Bianchi GD, Wallace RB, Cantor KP, et al. Lifestyle and anthropometric risk factors for prostate cancer in a cohort of Iowa men. Ann Epidemiol. 2000;10:361–369. doi: 10.1016/s1047-2797(00)00057-0. [DOI] [PubMed] [Google Scholar]
- 7.Rohrmann S, Smit E, Giovannucci E, Platz EA. Association between markers of the metabolic syndrome and lower urinary tract symptoms in the Third National Health and Nutrition Examination Survey (NHANES III) Int J Obes. 2005;29:310–316. doi: 10.1038/sj.ijo.0802881. [DOI] [PubMed] [Google Scholar]
- 8.Joseph MA, Harlow SD, Wei JT, Sarma AV, Dunn RL, Taylor JM, et al. Risk factors for lower urinary tract symptoms in a population-based sample of African-American men. Am J Epidemiol. 2003;157:906–914. doi: 10.1093/aje/kwg051. [DOI] [PubMed] [Google Scholar]
- 9.Reaven GM. Banting lecture 1988. Role of insulin resistance in human disease. Diabetes. 1988;37:1595–1607. doi: 10.2337/diab.37.12.1595. [DOI] [PubMed] [Google Scholar]
- 10.DeFronzo RA, Ferrannini E. Insulin resistance. A multifaceted syndrome responsible for NIDDM, obesity, hypertension, dyslipidemia, and atherosclerotic cardiovascular disease. Diabetes Care. 1991;14:173–194. doi: 10.2337/diacare.14.3.173. [DOI] [PubMed] [Google Scholar]
- 11.Rett K, Wicklmayr M, Mehnert H. New aspects of insulin resistance in hypertension. Eur Heart J. 1994;15(Suppl C):78–81. doi: 10.1093/eurheartj/15.suppl_c.78. [DOI] [PubMed] [Google Scholar]
- 12.Berne C, Fagius J, Pollare T, Hjemdahl P. The sympathetic response to euglycaemic hyperinsulinaemia. Evidence from microelectrode nerve recordings in healthy subjects. Diabetologia. 1992;35:873–879. doi: 10.1007/BF00399935. [DOI] [PubMed] [Google Scholar]
- 13.Kim DM, Ahn CW, Nam SY. Prevalence of obesity in Korea. Obes Rev. 2005;6:117–121. doi: 10.1111/j.1467-789X.2005.00173.x. [DOI] [PubMed] [Google Scholar]
- 14.Park YH, Chung MK. The prevalence of clinical benign prostatic hyperplasia and lower urinary tract symptoms in South-East Korea: a community-based study. J Pusan Natl Univ Hosp. 2001;9:141–157. [Google Scholar]
- 15.Lee MW, Lee KS. The prevalence of benign prostatic hyperplasia in self-referral populations over aged 50. Korean J Urol. 1996;37:263–267. [Google Scholar]
- 16.Guess HA, Arrighi HM, Metter FJ, Fozard JL. Cumulative prevalence of prostatism matches the autopsy prevalence of benign prostatic hyperplasia. Prostate. 1990;17:241–246. doi: 10.1002/pros.2990170308. [DOI] [PubMed] [Google Scholar]
- 17.Glynn RJ, Campion FW, Bouchard GR, Silbert JE. The development of benign prostatic hyperplasia among volunteers in the Normative Aging Study. Am J Epidemiol. 1985;121:78–90. [PubMed] [Google Scholar]
- 18.Kristal AR, Arnold KB, Schenk JM, Neuhouser ML, Weiss N, Goodman P, et al. Race/ethnicity, obesity, health related behaviors and the risk of symptomatic benign prostatic hyperplasia: results from the prostate cancer prevention trial. J Urol. 2007;177:1395–1400. doi: 10.1016/j.juro.2006.11.065. [DOI] [PubMed] [Google Scholar]
- 19.Laven BA, Orsini N, Andersson SO, Johansson JE, Gerber GS, Wolk A. Birth weight, abdominal obesity and the risk of lower urinary tract symptoms in a population based study of Swedish men. J Urol. 2008;179:1891–1895. doi: 10.1016/j.juro.2008.01.029. [DOI] [PubMed] [Google Scholar]
- 20.Park HK, Lee HW, Lee KS, Byun SS, Jeong SJ, Hong SK, et al. Relationship between lower urinary tract symptoms and metabolic syndrome in a community-based elderly population. Urology. 2008;72:556–560. doi: 10.1016/j.urology.2008.03.043. [DOI] [PubMed] [Google Scholar]
- 21.Koo KC, Cho KS, Kang EM, Kwon SW, Hong SJ. The relationship between metabolic syndrome and prostate volume in men over sixties who underwent prostate health check-up. Korean J Urol. 2008;49:813–817. [Google Scholar]
- 22.Lee SH, Kim JC, Lee JY, Kim JH, Oh CY, Lee SW, et al. Effects of obesity on lower urinary tract symptoms in Korean BPH patients. Asian J Androl. 2009;11:663–668. doi: 10.1038/aja.2009.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nandeesha H. Benign prostatic hyperplasia: dietary and metabolic risk factors. Int Urol Nephrol. 2008;40:649–656. doi: 10.1007/s11255-008-9333-z. [DOI] [PubMed] [Google Scholar]