Abstract
Objective:
The objective was to report our experience on the implantation of the Prolift system since 2005.
Methods:
Fifty-six patients were operated on between July 2005 and August 2008 by 1 surgeon. The patients were implanted with the transvaginal mesh, the Prolift system, for the treatment of recurrent or high-grade (Baden-Walker stage III or IV) multiple compartment pelvic organ prolapse (POP) associated with symptoms. A concomitant anti-incontinence surgery was performed in 38 patients (68%).
Results:
The population had a mean age of 68 (range 46–88), a body mass index of 27 (range 21–40) and a parity average of 3 (range 1–16). Previous POP repair had been performed in 17 patients (30%) and a hysterectomy in 43 (77%). The operating room time was on average 98 minutes (range 70–135), blood loss 81 mL (range 50–300) and hospital stay 3 days (range 1–10). With a median follow-up of 21 months, we found that the cure rate for POP was 91% (48/53) and the reoperation rate was 8% (4/53). Perioperative complications included 1 rectal laceration and 1 prolonged bleeding. Short-term postoperative complications included 10 episodes of transient urinary retention that required immediate tape release in 4 patients. Long-term complications included 5 POP recurrences, 2 low grade and 3 high grade.
Conclusion:
The Prolift system appears to be a relatively safe and effective alternative to conventional surgeries for the treatment of recurrent or high-grade multiple compartment POP, because of a high mid-term cure rate and a satisfactory complication profile. However, long-term follow-up is still needed to confirm these results.
Résumé
Objectif :
Notre objectif ici est de parler de notre expérience avec l’implantation du système Prolift depuis 2005.
Méthodologie :
Entre juillet 2005 et août 2008, 56 patientes ont été opérées par le même chirurgien. Les patientes ont subi une implantation du système de bandelette transvaginale Prolift, pour le traitement d’un prolapsus pelvien pluricompartimental récurrent ou de grade élevé (stade III ou IV de Baden-Walker) associé à des symptômes. Une chirurgie anti-incontinence concomitante a été réalisée chez 38 patientes (68 %).
Résultats :
L’âge moyen de la population de l’étude était de 68 ans (entre 46 et 88 ans), l’indice de masse corporelle moyen était de 27 (entre 21 et 40), et en moyenne, la parité était de 3 (entre 1 et 16). Une intervention antérieure de correction d’un prolapsus pelvien avait été effectuée chez 17 patientes (30 %), et une hystérectomie, chez 43 patientes (77 %). En moyenne, la durée de l’intervention était de 98 minutes (de 70 à 135), la perte sanguine, de 81 mL (de 50 à 300) et la durée du séjour à l’hôpital, de 3 jours (de 1 à 10). Après un suivi médian de 21 mois, le taux de guérison observé pour le prolapsus pelvien était de 91 % (48/53) et le taux de répétition de l’opération était de 8 % (4/53). (Trois patientes perdues au suivi ne sont pas incluses dans le taux de guérison.) Les complications périopératoires incluent une lacération rectale et un épisode de saignement prolongé. Les complications postopératoires à court terme incluent 10 épisodes de rétention urinaire transitoire néces-sitant un retrait immédiat de la bandelette chez 4 patientes. Les complications à long terme incluent 5 récidives du prolapsus pelvien, 2 de faible grade et 3 de grade élevé.
Conclusion:
Le système Prolift semble être une solution de rechange relativement sûre et efficace aux interventions traditionnelles pour le traitement du prolapsus pelvien pluricompartimental récurrent ou de grade élevé, en raison d’un taux élevé de guérison à moyen terme et d’un profil de complications acceptable. Cependant, un suivi à long terme est toujours requis pour valider ces résultats.
Introduction
Pelvic organ prolapse (POP) is a common problem in the aging female. Treatment options for symptomatic POP include observation, pessary use and surgery. Conventional treatment strategies for POP repair have a recurrence rate of 20% to 30%.1–3 A new surgical technique of pelvic reconstruction using a transvaginal mesh, the Prolift system (Gynecare, Johnson and Johnson, Somerville, NJ), attempts to improve these results by providing mechanical support to the weakened pelvic floor.
With regard to the implantation of the Prolift system, a transvaginal approach is used with percutaneous insertion of implant straps. For the anterior compartment repair, 2 implant straps on each side are placed via the obturator foramen in the arcus tendinus fasciae pelvis. For the posterior compartment repair, 1 implant strap on each side is placed via the sacrospinous ligament.
The objective of this retrospective study was to report our experience on the implantation of the Prolift system since 2005.
Methods
The population of the study included 56 patients who were operated on between July 29, 2005 and August 29, 2008, by 1 surgeon (LMT). Formal review and approval by the ethics committee of our institution was obtained.
Preoperative evaluation included a history, a cystoscopy with a detailed gynecological examination comprising a cough stress test, with full bladder and prolapse reduced, as well as a urodynamics study, with and without pessary and a quality-of-life questionnaire. All the patients were implanted with the transvaginal mesh (TVM), the Prolift system, for the treatment of recurrent or high-grade (Baden-Walker stage III or IV) multiple compartment POP associated with symptoms. The technique used is in accordance with the technique described by the TVM group, led by Dr. Philipe Debodinance, in 2004.4 A concomitant anti-incontinence surgery was performed in 38 patients (68%). The transobturator vaginal tape was implanted in 34 patients, Aris (Coloplast, Minneapolis, MS) in 3 and TVT-SECUR (Gynecare, Johnson and Johnson, Somerville, NJ), in 1 for clinical stress urinary incontinence (SUI) or unmasked SUI, either with a cough stress test with prolapse reduced or a urodynamics study with pessary.
Follow-up after surgery was done at 2 months, 6 months, 12 months and then yearly for 3 years, with a history and physical exam, including a gynecological examinations. The cure rate was evaluated based on the results of these visits. The patients who were lost in follow-up were contacted via telephone. All the patients we contacted said they were cured (27/27). Only 3 patients were not included in the cure rate calculation: 2 could not be contacted via telephone, and 1 had the mesh removed during the surgery. Cure rate was defined as the functional cure of the POP.
Results
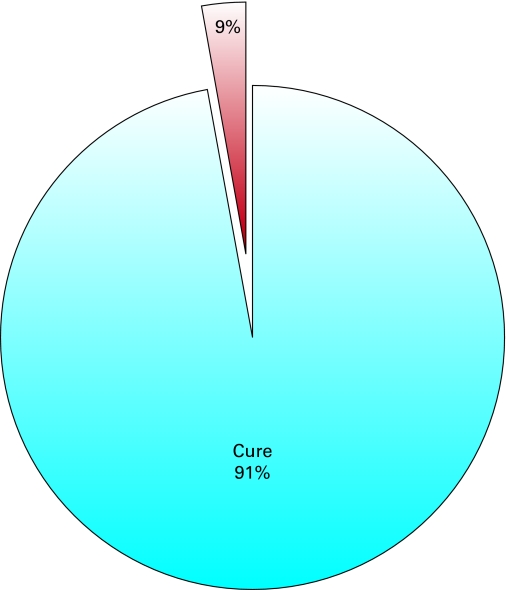
The population of the study had a mean age of 68 (range 46–88), a body mass index of 27 (range 21–40), a parity average of 3 (range 1–16) (Table 1). Previous POP repair had been performed in 17 patients (30%) and a hysterectomy in 43 (77%). High-grade genital prolapse was present in the anterior vaginal wall in 71% (40/56), apical wall in 45% (25/56) and posterior wall in 48% (27/56) (Table 2). Regarding operative data, a total mesh was used in 44 cases (79%), an anterior mesh alone in 5 (9%) and a posterior mesh alone in 7 (13%) (Table 3). General anesthesia was used in 31 patients (55%) and spinal anesthesia in 25 (45%). The operating room time was on average 98 minutes (range 70–135), blood loss 81 mL (range 50–300) and hospital stay 3 days (range 1–10). With a median follow-up of 21 months, we found that the cure rate for POP was 91% (48/53) and the reoperation rate was 8% (4/53) (Fig. 1). Perioperative complications included 1 anterior rectal wall laceration, that required primary repair and removal of the entire mesh, as well as 1 prolonged bleeding, which required embolization of the left internal iliac artery (Table 4). Short-term postoperative complications comprised 10 episodes of transient urinary retention that required immediate tape release in 4 patients, 2 cases of postoperative pain that lasted a maximum of 2 weeks and 1 episode of transient fever. Long-term complications included 5 organ prolapse recurrences, 2 low-grade POP, as well as 3 high-grade POP. One of the 2 low-grade recurrences required reoperation. The high-grade recurrences included 1 low rectocele grade III treated with another mesh, the Avaulta Plus (Bard Medical, Covington, GA), 1 colpocele grade III treated with an abdominal colposacropexy as well as 1 very low rectocele grade IV also treated with the Avaulta Plus. Also, long-term complications included 3 cases of de novo urinary incontinence. No case of vaginal erosion occurred in our series.
Table 1.
Characteristics of the patients
| Characteristics | Patients |
|---|---|
| No. patients | 56 |
| Age, yr (range) | 68.1 (46–88) |
| BMI (range) | 27 (21–40) |
| Parity, no. (range) | 3,3 (1–16) |
| Menopausal status, no. (%) | 53 (95%) |
| HRT, no. (%) | 15 (27%) |
| Preoperative UI, no. (%) | |
| – SUI | 30 (54%) |
| – Unmasked SUI | 8 (14%) |
| Prior vaginal surgery, no. (%) | |
| – Anti-incontinence surgery | 6 (11%) |
| – Pelvic prolapse repair | 17 (30%) |
| – Hysterectomy | 43 (77%) |
BMI = body mass index; HRT = hormone replacement therapy; UI = urinary incontinence; SUI = stress urinary incontinence.
Table 2.
Pelvic organ prolapse characteristics
| Prolapse | No. (%) | No. of stages 3 and 4 (%) |
|---|---|---|
| Cystocele | ||
| – Stage 0–1 | 11 (19.6%) | 40 (71.4%) |
| – Stage 2 | 5 (8.9%) | |
| – Stage 3 | 29 (51.8%) | |
| – Stage 4 | 11 (19.6%) | |
| Uterine prolapse/colpocele | ||
| – Stage 0–1 | 12 (21.4%) | 25 (44.6%) |
| – Stage 2 | 19 (33.9%) | |
| – Stage 3 | 11 (19.6%) | |
| – Stage 4 | 14 (25%) | |
| Enterocele | ||
| – Absent | 33 (58.7%) | N/A |
| – Present | 23 (41.3%) | |
| Rectocele | ||
| – Stage 0–1 | 11 (19.6%) | 27 (48.2%) |
| – Stage 2 | 18 (32.1%) | |
| – Stage 3 | 13 (23.2%) | |
| – Stage 4 | 14 (25%) | |
Table 3.
Operative characteristics
| Technique used, no. (%) | |
| – Total | 44 (79%) |
| – Anterior alone | 5 (9%) |
| – Posterior alone | 7 (13%) |
| Associated anti-incontinence surgery, no. (%) | 38 (68%) |
| Operating room time, minutes (range) | 98 (70–135) |
| Blood loss, mL (range) | 81 (50–300) |
| Type of anesthesia, no. (%) | |
| – General | 31 (55%) |
| – Spinal | 25 (45%) |
| Hospital stay, days (range) | 2.9 (1–10) |
Fig. 1.
Cure rate for pelvic organ prolapse.
Table 4.
Complications
| Perioperative, no. (%) | |
| – Prolonged bleeding | 1 (2%) |
| – Rectal laceration | 1 (2%) |
| – Bladder laceration | 0 |
| Postoperative, no. (%) | |
| Short term | |
| – Urinary retention | 10 (18%) |
| – Prolonged postoperative pain | 2 (4%) |
| – Febrile morbidity | 1 (2%) |
| Long term | |
| – Organ prolapse recurrence | 5 (9%) |
| – De novo urinary incontinence | 3 (6%) |
| – Vaginal erosion | 0 |
Discussion
In this study, the Prolift system demonstrated a high mid-term cure rate, with a cure rate of 91% and only 5 POP recurrences. The 4 cases of POP recurrence that needed reoperation included one rectocele grade II and 1 low rectocele grade III that occurred following an anterior mesh implant only. The colpocele grade III occurred after a separated total mesh implant, because it was impossible during the initial surgery to develop a bridge at the vaginal cuff for the mesh to pass. The case of the very low rectocele grade IV following a total mesh implant may be explained by the fact that the Prolift system does not seem to provide good support of the posterior wall’s lowest portion. In fact, the mesh does not cover the lowest 2 cm of the posterior wall. In that regard, the mesh Avaulta Plus gave better results.
Furthermore, the Prolift system had few major perioperative complications as well as few postoperative complications. In the perioperative period, only 1 prolonged bleeding and 1 rectal laceration occurred. In the postoperative period, no case of vaginal erosion was experienced because of the routine use of premarin cream before and after the surgery, which has now become the standard for most surgeons. The main concern was the 10 cases of transient urinary retention. However, only 4 of them required immediate tape release, the 6 others resolved naturally. The high rate of urinary retention coincided with a change in the time of the catheter removal from postoperative day 1 to postoperative day 2. Since we reverted to removing the catheter on postoperative day 1, the rate of urinary retention has decreased significantly.
The results of this study are in accordance with results from the largest series published so far on the use of a TVM for the treatment of POP. In 2005, Cosson and colleagues reported the results of a multicentric study involving 687 patients with 4 months of follow-up (M. Cosson, International Continence Society meeting, August 2005). The authors of that study were part of the TVM group, which developed the technique back in 2004.4 The cure rate was 95%, with organ prolapse recurrence in the range of 0% to 11%, depending on the centre. Vaginal erosions occurred in 0% to 13%. At the 2008 American Urological Association (AUA) meeting in Orlando, Lukban and colleagues reported a multicentric prospective trial with 168 patients using a similar mesh, the Apogee system (American Medical Systems, Minnetonka, MN) (J.C. Lukban, AUA meeting, May 2008). At 6 months, the cure rate for posterior and apical wall defects were 92% and 94%, respectively. No intraoperative complication was experienced, but vaginal erosions occurred in 9% of the patients. In January 2009, Elmer and colleagues published a paper on 261 patients with a follow-up of 1 year.5 The anatomical cure rate was 79% to 86%. Bladder and rectal lacerations were seen in 3% and postoperative vaginal erosions in 11%. In the same month, Feiner and colleagues published a review of 8 studies and 1295 patients in which the Prolift system was used to treat apical prolapse.6 With a mean follow-up of 30 weeks, the mean objective success rate was 87% (range 75 to 94) and the mean complication rate was 16%. Vaginal erosions occurred in 7%.
Looking back on the results of this present study and a review of literature, the Prolift system showed a high short and mid-term cure rate, as well as a satisfactory complication profile. Therefore, it appears to be a safe and effective alternative to conventional surgeries for the treatment of recurrent or high-grade multiple compartment POP.
The limitations of this study are the retrospective method and the single-surgeon single-centre experience. Also, a high number of patients were lost in follow-up. However, it is worth noting that they did not go to their follow-up visit because they reported that they were all cured.
The strengths of this study are the relatively high number of patients for 1 surgeon and the long follow-up of 21 months compared to similar studies. In fact, we did not find a single report in which the follow-up time was so extensive.
Conclusion
Considering the results of this study and a review of literature, the Prolift system appears to be a relatively safe and effective alternative to conventional surgeries for the treatment of recurrent or high-grade multiple compartment POP, because of a high mid-term cure rate and a satisfactory complication profile. However, long-term follow-up is still needed to confirm these results.
Footnotes
Competing interests: None declared.
This paper has been peer-reviewed.
References
- 1.Julian TM. The efficacy of Marlex mesh in the repair of severe, recurent vaginal prolapse of the anterior midvaginal wall. Am J Obstet Gynecol. 1996;175:1472–5. doi: 10.1016/s0002-9378(96)70092-3. [DOI] [PubMed] [Google Scholar]
- 2.Morley GW, DeLancey JOL. Sacrospinous ligament fixation for eversion of the vagina. Am J Obstet Gynecol. 1988;158:872–81. doi: 10.1016/0002-9378(88)90088-9. [DOI] [PubMed] [Google Scholar]
- 3.Sze EHM, Micklos JR, Partoll L, et al. Sacro-spinous ligament fixation with transvaginal needle suspension for advenced pelvic organ prolapse and stress incontinence. Obstet Gynecol. 1997;89:94–6. doi: 10.1016/s0029-7844(96)00357-2. [DOI] [PubMed] [Google Scholar]
- 4.Debodinance P, Berrocal J, Clavé H, et al. Évolution des idées sur le traitement chirurgical des prolapsus génitaux: naissance de la technique TVM. J Gynecol Obstet Biol Reprod. 2004;33:577–88. doi: 10.1016/s0368-2315(04)96598-2. [DOI] [PubMed] [Google Scholar]
- 5.Elmér C, Altman D, Engh ME, et al. Trocar-guided transvaginal mesh repair of pelvic organ prolapse. Obstet Gynecol. 2009;113:117–26. doi: 10.1097/AOG.0b013e3181922164. [DOI] [PubMed] [Google Scholar]
- 6.Feiner B, Jelovsek JE, Maher C. Efficacy and safety of transvaginal mesh kits in the treatment of prolapse of the vaginal apex: a systematic review. BJOG. 2009;116:15–24. doi: 10.1111/j.1471-0528.2008.02023.x. [DOI] [PubMed] [Google Scholar]