Abstract
OBJECTIVE
The 5-5 homozygous CNDP1 (carnosinase) genotype is associated with a reduced risk of diabetic nephropathy. We investigated whether this association is sex specific and independent of susceptibility for type 2 diabetes.
RESEARCH DESIGN AND METHODS
Three separate groups of 114, 90, and 66 patients with type 2 diabetes and diabetic nephropathy were included in this study and compared with 93 patients with type 2 diabetes for >15 years without diabetic nephropathy and 472 population control subjects. The diabetes control group was used to determine an association in the three patient groups separately, and the population control group was used to estimate the genotype risk [odds ratio (CI)] for the population in a pooled analysis. The population control subjects were also compared with 562 patients with type 2 diabetes without diabetic nephropathy to determine whether the association was independent of type 2 diabetes. The CNDP1 genotype was determined by fragment analysis after PCR amplification.
RESULTS
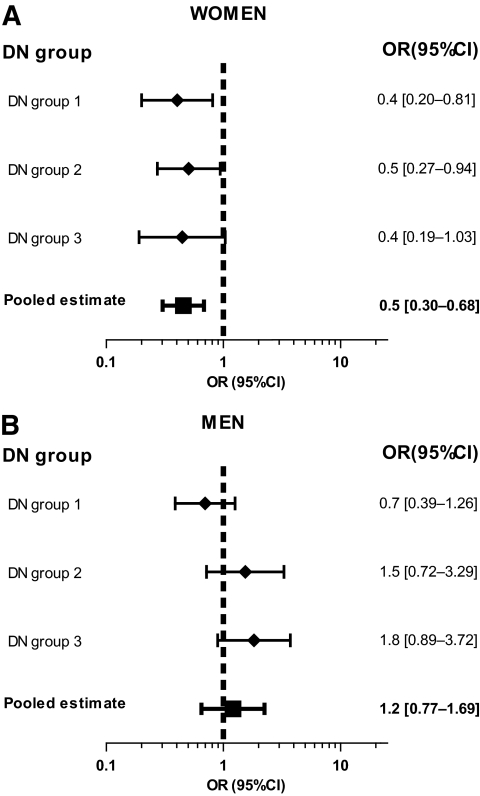
The frequency of the 5-5 homozygous genotype was 28, 36, and 41% in the three diabetic nephropathy patient groups and 43 and 42% in the diabetic and population control subjects, respectively. The 5-5 homozygous genotype occurred significantly less frequently in women in all three patient groups compared with diabetic control subjects. The genotype risk for the population was estimated to be 0.5 (0.30–0.68) in women and 1.2 (0.77–1.69) in men. The 562 patients with type 2 diabetes without diabetic nephropathy did not differ from the general population (P = 0.23).
CONCLUSIONS
This study suggests that the association between the CNDP1 gene and diabetic nephropathy is sex specific and independent of susceptibility for type 2 diabetes.
Only 20–40% of patients with type 1 or type 2 diabetes will develop diabetic nephropathy, and if no signs of nephropathy are present in the first 15 years after diagnosis of diabetes, the chance of ever developing nephropathy is small (1). Furthermore, sibling studies show a strong familial component for development of diabetic nephropathy (2,3), and certain ethnic groups seem to be at a greater risk of developing nephropathy (2,4). These findings suggest that there is a genetic susceptibility component for diabetic nephropathy.
Many genes are thought to be involved in diabetic nephropathy (rev. in 5). One of the genes associated with nephropathy in both patients with type 1 and type 2 diabetes is the CNDP1 gene, which encodes serum carnosinase (6). This was confirmed in European Americans with end-stage diabetic nephropathy due to type 2 diabetes (7), but the association between diabetic nephropathy and the CNDP1 gene could not be confirmed in patients with diabetic nephropathy due to type 1 diabetes (8,9) nor in African Americans (7).
Patients with type 2 diabetes of Caucasian origin with homozygosity for five leucine repeats in exon 2 demonstrated a reduced susceptibility for developing diabetic nephropathy compared with individuals with six to eight repeats (6,7,10). With increasing numbers of leucine repeats, the secretion of serum carnosinase has been shown to increase (11) and to lead to higher serum carnosinase activity (4,6). Serum carnosinase degrades carnosines and other histidine-containing dipeptides. Carnosines and related dipeptides are known for their reactive oxygen scavenging effects (12), for degrading advanced glycation end products (13), and for reducing the transforming growth factor (TGF)-β–induced synthesis of extracellular matrix components (6).
Some genes involved in diabetic nephropathy have been shown to have sex specific effects (14,15). For example, the RANTES receptor gene (CCR5) is only associated with diabetic nephropathy in men (14), and two single nucleotide polymorphisms in the podocyte slit diaphragm gene (ACTN4) were only associated with diabetic nephropathy in women (15).
Therefore, we investigated whether the association between the CNDP1 gene and diabetic nephropathy due to type 2 diabetes is sex specific. Furthermore, we studied whether the association between diabetic nephropathy and the CNDP1 gene is independent of the susceptibility for type 2 diabetes itself.
RESEARCH DESIGN AND METHODS
The institutional medical ethics committees of the participating hospitals approved of the studies described below.
Case groups.
For the first case group, female and male Caucasian diabetic patients with diabetic nephropathy from the case-control study of Janssen et al. (6) were reassessed separately. Diabetic nephropathy was defined as diabetes with retinopathy with either macroalbuminuria or as being on dialysis (because of diabetic nephropathy). The details of the recruitment of this cohort are described elsewhere (6). In the present analysis, only 114 diabetic nephropathy patients with type 2 diabetes were included, and this group will be referred to as diabetic nephropathy group 1.
For the second case group, diabetic nephropathy patients were selected from the ZODIAC (Zwolle Outpatient Diabetes Project Integrating Available Care) study (16). Diabetic nephropathy was defined as having either an estimated glomerular filtration rate <60 ml/min/1.73 m2 (17) in combination with an albumin excretion >30 mg/l (18) or macroalbuminuria (>300 mg/l) in combination with retinopathy (19). ZODIAC was a cross-sectional single-center study investigating only patients with type 2 diabetes, selected from a population of >95% Caucasian origin. Patients were recruited from 61 general practitioners from 1998 to 2000. In this study, 90 diabetic nephropathy patients were identified, and these will be referred to as diabetic nephropathy group 2.
For the third group, diabetic nephropathy patients were selected out of a total of 875 patients from the NECOSAD (Netherlands Cooperative Study on the Adequacy of Dialysis) study (20). NECOSAD is a multicenter prospective follow-up study of patients with end-stage renal disease who were included at the start of dialysis, between 1997 and 2005. For the present analysis, only patients with type 2 diabetes of Caucasian origin and end-stage renal disease due to diabetic nephropathy were selected; 66 diabetic nephropathy patients were included and are referred to as diabetic nephropathy group 3.
Control groups.
The first control group is a diabetic group, consisting of Caucasian patients with type 2 diabetes without microalbuminuria for at least 15 years, in the absence of ACE inhibitor treatment (6,16). This control group is referred to as diabetic non-nephropathy control subjects.
The second control group is a population control group selected from the SUNSET (Surinamese in the Netherlands: Study on health and Ethnicity) study, a population-based cross-sectional survey (21). In brief, between 2001 and 2003, a random sample of noninstitutionalized adults aged 35–60 years was selected. In the present study, only the 472 white Dutch participants, of whom the genotypic distribution was described in a previous report (4), are used and referred to as population control subjects.
To investigate whether the association between diabetic nephropathy and the CNDP1 gene is not due to susceptibility for type 2 diabetes, we additionally studied 562 patients with type 2 diabetes without diabetic nephropathy (defined as any of the criteria above) selected from the ZODIAC study participants, referred to as the type 2 diabetes population, to compare with the general population.
Genotyping.
Genotyping was performed as described previously (4). In brief, after PCR amplification, fragment analysis was performed on the ABI-3130 analyzer to determine the number of leucine repeats in each allele. The success rate was on average 95%, and no errors were detected. Genotyping was performed partially in Leiden and in Mannheim. Some of the samples were measured in both institutes, and there was a 100% concordance.
Statistical analysis.
The baseline characteristics of the groups are presented as means and SDs or percentages. Continuous variables were tested using the Student t test and numeric variables using χ2. All groups were tested for Hardy-Weinberg equilibrium, using a χ2 test.
First, the frequency of the 5-5 homozygous genotype in the respective diabetic nephropathy groups was compared with the 93 diabetic non-nephropathy control subjects stratified by sex, to investigate the relevance of the genotype to disease etiology.
Second, the genotype risk for the population was estimated through comparison of the diabetic nephropathy groups with population control subjects. Odds ratios with CIs were calculated. A pooled analysis was performed to determine the total effect for females and males separately, combining the three case groups when compared with sex-matched population control subjects. The fixed-effects model (inverse variance method) was used when heterogeneity was P > 0.1 (χ2) and the random-effects model when heterogeneity was P < 0.1.
Finally, to assess whether the susceptibility for diabetic nephropathy is independent of susceptibility for type 2 diabetes, we compared the type 2 diabetes population with population control subjects.
The statistical analyses were all performed using SPSS 16.0 and R version 2.9.0.
RESULTS
The baseline characteristics of the three diabetic nephropathy groups are described in Table 1, and comparisons are made with diabetic non-nephropathy control subjects. Baseline characteristics did not differ between diabetic non-nephropathy control subjects and the type 2 diabetes population, except for diabetes duration (data not shown). There was no significant difference in 5-5 homozygous genotype frequency between the diabetic non-nephropathy control subjects and the population control subjects consisting of all patients (P = 0.8), all women (P = 0.07), or all men (P = 0.13). All cohorts were in the Hardy-Weinberg equilibrium (found in the online appendix, available at http://diabetes.diabetesjournals.org/cgi/content/full/db09-1377/DC1).
TABLE 1.
Baseline characteristics
| Diabetic nephropathy groups |
Type 2 diabetes >15 years without diabetic nephropathy | |||
|---|---|---|---|---|
| 1 | 2 | 3 | ||
| Total (n) | 114 | 90 | 66 | 93 |
| Age (years) | 64.0 ± 11.07 | 73.4 ± 8.40†‡ | 66.2 ± 8.97 | 65.8 ± 11.30 |
| Sex (n (%) male) | 64 (56.1) | 30 (33.3)†‡ | 35 (53.0) | 47 (50.5) |
| Diabetes duration (years) | 14.3 ± 8.38† | 9.7 ± 9.51†‡ | 15.2 ± 10.99† | 22.2 ± 6.78 |
| A1C (%) | 7.5 ± 1.71 | 7.5 ± 1.2 | — | 7.3 ± 1.51 |
| Women | ||||
| Age (years) | 64.2 ± 11.64 | 72.2 ± 9.09†‡ | 67.2 ± 7.57 | 65.1 ± 12.07 |
| Diabetes duration (years) | 14.8 ± 9.24† | 9.2 ± 7.77†‡ | 15.9 ± 11.83† | 22.9 ± 6.50 |
| A1C (%) | 8.0 ± 2.08 | 7.4 ± 1.12 | — | 7.5 ± 1.65 |
| Men | ||||
| Age (years) | 63.7 ± 10.68 | 75.9 ± 6.22†‡ | 65.3 ± 10.07 | 66.4 ± 10.60 |
| Diabetes duration (years) | 13.9 ± 7.81† | 10.7 ± 12.4† | 14.7 ± 10.39† | 21.6 ± 7.05 |
| A1C (%) | 7.2 ± 1.32 | 7.6 ± 1.38 | — | 7.6 ± 1.38 |
†P < 0.05 compared with type 2 diabetes >15 years without diabetic nephropathy.
‡P < 0.05 compared with either diabetic nephropathy group 1 or 3. No significant differences were seen between group 1 and 3 or between women and men in each of the groups.
Relevance of the 5-5 homozygous genotype to disease etiology.
Overall, the 5-5 homozygous genotype frequency of the diabetic nephropathy groups did not differ from the diabetic non-nephropathy control subjects or between the diabetic nephropathy groups (P = 0.2). Women in all three diabetic nephropathy groups had a significantly lower frequency of the 5-5 homozygous genotype than female diabetic non-nephropathy control subjects (Table 2), also after Bonferroni adjustment for multiple testing. In contrast, men in all three diabetic nephropathy groups had a higher frequency of the 5-5 homozygous genotype than male diabetic non-nephropathy control subjects.
TABLE 2.
The relation between 5-5 homozygous genotype and diabetic nephropathy
| Diabetic nephropathy groups |
Type 2 diabetes >15 years without diabetic nephropathy | |||
|---|---|---|---|---|
| 1 | 2 | 3 | ||
| Total | ||||
| n | 114 | 90 | 66 | 93 |
| Frequency 5-5 (%) | 28.1 | 35.6 | 40.9 | 43.0 |
| P* | 0.03 | 0.30 | 0.80 | |
| Women | ||||
| n | 50 | 60 | 31 | 46 |
| Frequency 5-5 (%) | 24.0 | 28.3 | 25.8 | 58.7 |
| P* | 0.001 | 0.002 | 0.006 | |
| Men | ||||
| n | 64 | 30 | 35 | 47 |
| Frequency 5-5 (%) | 31.2 | 50.0 | 53.4 | 27.7 |
| P* | 0.62 | 0.05 | 0.02 | |
*Compared with type 2 diabetes >15 years without diabetic nephropathy.
Genotype risk for the population.
No heterogeneity was detected in women (P = 0.64), but heterogeneity was detected in men (P = 0.09). The three diabetic nephropathy groups were pooled for women and men separately, resulting in a genotype risk of 0.5 (0.30–0.68) in women and 1.2 (0.77–1.69) in men (Fig. 1).
FIG. 1.
The relationship between the 5-5 homozygous CNDP1 genotype and diabetic nephropathy (DN) in women (A) and men (B) in the three independent diabetic nephropathy groups and a pooled analysis (total) compared with population control subjects. The filled diamonds represent the odds ratios of the independent diabetic nephropathy groups and the filled square represents the pooled odds ratio.
Specificity of 5-5 homozygous genotype for diabetic nephropathy, not type 2 diabetes.
The 5-5 homozygous genotype frequency of both the 562 type 2 diabetic individuals and the 472 population control subjects are shown in Table 3, showing similar frequency of the 5-5 homozygous genotype.
TABLE 3.
Comparison between type 2 diabetes population and population control subjects
| Type 2 diabetes population | Population control subjects | P | |
|---|---|---|---|
| Total (n) | 562 | 472 | |
| Frequency 5-5 (%) | 38.1 | 41.7 | 0.23 |
| Women (n) | 319 | 239 | |
| Frequency 5-5 (%) | 39.5 | 43.9 | 0.23 |
| Men (n) | 243 | 233 | |
| Frequency 5-5 (%) | 36.7 | 39.5 | 0.58 |
DISCUSSION
Our results show a sex specific effect of the CNDP1 genotype in relation to diabetic nephropathy, suggesting that the 5-5 homozygous genotype is only protective in women. The frequency of the 5-5 homozygous genotype was determined in three independent diabetic nephropathy groups. These groups were compared with two control groups: patients with type 2 diabetes and a low risk of ever developing diabetic nephropathy and a sample from the general population. Compared with the diabetic control group, the 5-5 homozygous genotype frequency was significantly lower in women with diabetic nephropathy in all three cohorts, but not in men. The population control group serves to estimate the genotype risk for the population, showing that women with the 5-5 homozygous genotype have a twofold reduced risk of ever developing diabetic nephropathy. Furthermore, this study shows similar frequencies of the 5-5 homozygous genotype in a large type 2 diabetes population and the general population, underlining that the association with diabetic nephropathy is independent of a genetic susceptibility for type 2 diabetes.
The 5-5 homozygous genotype leads to lower carnosinase activity compared with the other genotypes (4,6), leaving more carnosine free to protect the kidney from oxidative stress. Since men have higher carnosine levels in their muscle tissue and women have slightly higher serum carnosinase levels (22), differences in carnosinase activity due to the different CNDP1 polymorphism may have a stronger impact in women. Carnosine content in the muscles of female mice was shown to increase after testosterone administration, and the increase was 268% (23). This might be because carnosine synthetase, the enzyme that synthesizes carnosine, is upregulated by testosterone. It is possible that this phenomenon plays a role in diabetic nephropathy, because both carnosine synthetase (preliminary results) and androgen receptors are expressed in human kidney (24).
Another explanation for the sex specific effect found in this study is that the association between the CNDP1 gene and diabetic nephropathy is lost in men due to selective survival by cardiovascular disease. As carnosine has shown to be protective against oxidative stress and hemodynamic damage (6,12,13), this might also explain its role in cardiovascular death in diabetic nephropathy patients. Men with diabetic nephropathy due to type 2 diabetes have a higher risk for cardiovascular disease than women (25). Therefore, this might be more prominent in men. Further support for this theory comes from the ZODIAC study. Men with a diabetes duration <10 years and the 5-5 homozygous genotype have a significantly lower mortality risk due to cardiovascular disease than patients with >10 leucine repeats in the CNDP1 genotype (data not shown). We found no difference in cardiovascular death between the different genotypes in women. These findings need to be replicated in an independent study.
The relatively older age of diabetic nephropathy group 2 might influence the number of subjects with an estimated glomerular filtration rate <60 ml/min/1.73 m2. Therefore, a sensitivity analysis was performed, adopting increasingly stringent definitions of diabetic nephropathy. The results of this analysis support the conclusion that the 5-5 homozygous genotype is protective in women (see the online appendix).
The statistical power to detect a similar association in men as that seen in women ranged from 97 to 100% within the three diabetic nephropathy groups. Insufficient statistical power therefore does not explain the sex specific effect found in this study.
Limitations of this study are that ethnic origin is not defined by ethnic markers in these Caucasian populations and that sample sizes are relatively small. We performed a sensitivity analysis to exclude population stratification and a permutation analysis to rule out that our results are due to random fluctuation. These analyses support that population stratification or chance are unlikely to explain the sex specific effect found in this study (online appendix).
Another limitation is that the three diabetic nephropathy groups are compared with the same control group.
In conclusion, this study suggests a sex specific effect of the association between the CNDP1 gene and diabetic nephropathy in three independent patient groups with diabetic nephropathy due to type 2 diabetes, with women being protected by the 5-5 homozygous genotype.
Supplementary Material
ACKNOWLEDGMENTS
This study was financially supported by the Leiden University Medical Center. Part of this study was supported by the EU-funded specifically targeted project, PREDICTIONS, to identify risk factors for developing diabetic nephropathy (FP6-018733). NECOSAD was supported by grants from the Dutch Kidney Foundation (E.018) and the Dutch National Health Insurance Board (OG97/005).
No potential conflicts of interest relevant to this article were reported.
We would like to express our gratitude to the Dutch Diabetes Research Foundation for supporting the Hindinef study and the Health Research and Development Council of the Netherlands (ZonMw) for supporting the SUNSET study. We would also like to thank the members of the NECOSAD study group and the ZODIAC study group.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
REFERENCES
- 1.Krolewski AS, Warram JH, Rand LI, Kahn CR: Epidemiologic approach to the etiology of type I diabetes mellitus and its complications. N Engl J Med 1987; 317: 1390–1398 [DOI] [PubMed] [Google Scholar]
- 2.Pettitt DJ, Saad MF, Bennett PH, Nelson RG, Knowler WC: Familial predisposition to renal disease in two generations of Pima Indians with type 2 (non-insulin-dependent) diabetes mellitus. Diabetologia 1990; 33: 438–443 [DOI] [PubMed] [Google Scholar]
- 3.Seaquist ER, Goetz FC, Rich S, Barbosa J: Familial clustering of diabetic kidney disease: evidence for genetic susceptibility to diabetic nephropathy. N Engl J Med 1989; 320: 1161–1165 [DOI] [PubMed] [Google Scholar]
- 4.Mooyaart AL, van Valkengoed IG, Shaw PK, Peters V, Baelde HJ, Rabelink TJ, Bruijn JA, Stronks K, de Heer E: Lower frequency of the 5/5 homozygous CNDP1 genotype in South Asian Surinamese. Diabetes Res Clin Pract 2009; 85: 272–278 [DOI] [PubMed] [Google Scholar]
- 5.Maeda S: Genetics of diabetic nephropathy. Ther Adv Cardiovasc Dis 2008; 2: 363–371 [DOI] [PubMed] [Google Scholar]
- 6.Janssen B, Hohenadel D, Brinkkoetter P, Peters V, Rind N, Fischer C, Rychlik I, Cerna M, Romzova M, de Heer E, Baelde H, Bakker SJ, Zirie M, Rondeau E, Mathieson P, Saleem MA, Meyer J, Köppel H, Sauerhoefer S, Bartram CR, Nawroth P, Hammes HP, Yard BA, Zschocke J, van der Woude FJ: Carnosine as a protective factor in diabetic nephropathy: association with a leucine repeat of the carnosinase gene CNDP1. Diabetes 2005; 54: 2320–2327 [DOI] [PubMed] [Google Scholar]
- 7.Freedman BI, Hicks PJ, Sale MM, Pierson ED, Langefeld CD, Rich SS, Xu J, McDonough C, Janssen B, Yard BA, van der Woude FJ, Bowden DW: A leucine repeat in the carnosinase gene CNDP1 is associated with diabetic end-stage renal disease in European Americans. Nephrol Dial Transplant 2007; 22: 1131–1135 [DOI] [PubMed] [Google Scholar]
- 8.Wanic K, Placha G, Dunn J, Smiles A, Warram JH, Krolewski AS: Exclusion of polymorphisms in carnosinase genes (CNDP1 and CNDP2) as a cause of diabetic nephropathy in type 1 diabetes: results of large case-control and follow-up studies. Diabetes 2008; 57: 2547–2551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Trégouet DA, Groop PH, McGinn S, Forsblom C, Hadjadj S, Marre M, Parving HH, Tarnow L, Telgmann R, Godefroy T, Nicaud V, Rousseau R, Parkkonen M, Hoverfält A, Gut I, Heath S, Matsuda F, Cox R, Kazeem G, Farrall M, Gauguier D, Brand-Herrmann SM, Cambien F, Lathrop M, Vionnet N: EURAGEDIC Consortium G/T substitution in intron 1 of the UNC13B gene is associated with increased risk of nephropathy in patients with type 1 diabetes. Diabetes 2008; 57: 2843–2850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McDonough CW, Hicks PJ, Lu L, Langefeld CD, Freedman BI, Bowden DW: The influence of carnosinase gene polymorphisms on diabetic nephropathy risk in African-Americans. Hum Genet 2009; 126: 265–275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Riedl E, Koeppel H, Brinkkoetter P, Sternik P, Steinbeisser H, Sauerhoefer S, Janssen B, van der Woude FJ, Yard BA: A CTG polymorphism in the CNDP1 gene determines the secretion of serum carnosinase in Cos-7 transfected cells. Diabetes 2007; 56: 2410–2413 [DOI] [PubMed] [Google Scholar]
- 12.Hipkiss AR, Brownson C, Carrier MJ: Carnosine, the anti-ageing, anti-oxidant dipeptide, may react with protein carbonyl groups. Mech Ageing Dev 2001; 122: 1431–1445 [DOI] [PubMed] [Google Scholar]
- 13.Hobart LJ, Seibel I, Yeargans GS, Seidler NW: Anti-crosslinking properties of carnosine: significance of histidine. Life Sci 2004; 75: 1379–1389 [DOI] [PubMed] [Google Scholar]
- 14.Mlynarski WM, Placha GP, Wolkow PP, Bochenski JP, Warram JH, Krolewski AS: Risk of diabetic nephropathy in type 1 diabetes is associated with functional polymorphisms in RANTES receptor gene (CCR5): a sex-specific effect. Diabetes 2005; 54: 3331–3335 [DOI] [PubMed] [Google Scholar]
- 15.Ihalmo P, Wessman M, Kaunisto MA, Kilpikari R, Parkkonen M, Forsblom C, Holthöfer H, Groop PH: FinnDiane Study Group Association analysis of podocyte slit diaphragm genes as candidates for diabetic nephropathy. Diabetologia 2008; 51: 86–90 [DOI] [PubMed] [Google Scholar]
- 16.Ubink-Veltmaat LJ, Bilo HJ, Groenier KH, Houweling ST, Rischen RO, Meyboom-de Jong B: Prevalence, incidence and mortality of type 2 diabetes mellitus revisited: a prospective population-based study in The Netherlands (ZODIAC-1). Eur J Epidemiol 2003; 18: 793–800 [DOI] [PubMed] [Google Scholar]
- 17.Levey AS, Gassman JJ, Hall PM, Walker WG: Assessing the progression of renal disease in clinical studies: effects of duration of follow-up and regression to the mean. Modification of Diet in Renal Disease (MDRD) Study Group. J Am Soc Nephrol 1991; 1: 1087–1094 [DOI] [PubMed] [Google Scholar]
- 18.Ninomiya T, Perkovic V, de Galan BE, Zoungas S, Pillai A, Jardine M, Patel A, Cass A, Neal B, Poulter N, Mogensen CE, Cooper M, Marre M, Williams B, Hamet P, Mancia G, Woodward M, Macmahon S, Chalmers J: ADVANCE Collaborative Group Albuminuria and kidney function independently predict cardiovascular and renal outcomes in diabetes. J Am Soc Nephrol 2009; 20: 1813–1821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Parving HH, Gall MA, Skøtt P, Jørgensen HE, Løkkegaard H, Jørgensen F, Nielsen B, Larsen S: Prevalence and causes of albuminuria in non-insulin-dependent diabetic patients. Kidney Int 1992; 41: 758–762 [DOI] [PubMed] [Google Scholar]
- 20.Muntinghe FL, Verduijn M, Zuurman MW, Grootendorst DC, Carrero JJ, Qureshi AR, Luttropp K, Nordfors L, Lindholm B, Brandenburg V, Schalling M, Stenvinkel P, Boeschoten EW, Krediet RT, Navis G, Dekker FW: CCR5 deletion protects against inflammation-associated mortality in dialysis patients. J Am Soc Nephrol 2009; 20: 1641–1649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Agyemang C, Bindraban N, Mairuhu G, Montfrans G, Koopmans R, Stronks K: SUNSET (Surinamese in The Netherlands: Study on Ethnicity and Health) Study Group Prevalence, awareness, treatment, and control of hypertension among Black Surinamese, South Asian Surinamese and White Dutch in Amsterdam, The Netherlands: the SUNSET study. J Hypertens 2005; 23: 1971–1977 [DOI] [PubMed] [Google Scholar]
- 22.Bando K, Shimotsuji T, Toyoshima H, Hayashi C, Miyai K: Fluorometric assay of human serum carnosinase activity in normal children, adults and patients with myopathy. Ann Clin Biochem 1984; 21: 510–514 [DOI] [PubMed] [Google Scholar]
- 23.Peñafiel R, Ruzafa C, Monserrat F, Cremades A: Gender-related differences in carnosine, anserine and lysine content of murine skeletal muscle. Amino Acids 2004; 26: 53–58 [DOI] [PubMed] [Google Scholar]
- 24.Kimura N, Mizokami A, Oonuma T, Sasano H, Nagura H: Immunocytochemical localization of androgen receptor with polyclonal antibody in paraffin-embedded human tissues. J Histochem Cytochem 1993; 41: 671–678 [DOI] [PubMed] [Google Scholar]
- 25.Avogaro A, Giorda C, Maggini M, Mannucci E, Raschetti R, Lombardo F, Spila-Alegiani S, Turco S, Velussi M, Ferrannini E: Diabetes and Informatics Study Group, Association of Clinical Diabetologists, Istituto Superiore di Sanità Incidence of coronary heart disease in type 2 diabetic men and women: impact of microvascular complications, treatment, and geographic location. Diabetes Care 2007; 30: 1241–1247 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.