Abstract
We analyze the influence of body weight in early adulthood, and changes in weight over time, on self rated health (SRH) as people age into mid-adulthood. While prior research focused on cross-sectional samples of older adults, we use longitudinal data from the NHANES I Epidemiologic Follow-up Study (NHEFS) and double-trajectory latent growth models to study the association between body mass index (BMI) and SRH trajectories over twenty years. Results indicate that high BMI in early adulthood and gaining more weight over time are both associated with a faster decline in health ratings. Among white women only, those with a higher BMI at the baseline also report lower initial SRH. A small part of the weight-health associations is due to sociodemographic factors, but not baseline health behaviors or medical conditions. The findings provide new support for the cumulative disadvantage perspective, documenting the increasing health inequalities in a cohort of young adults.
Sociological research aims to document and explain life chances and outcomes of people with different levels of resources. Many sociologists interested in patterns of inequalities over the life course have grounded their analyses within the cumulative disadvantage framework, which posits that risk factors accumulate over time based on early life advantages or disadvantages of particular social groups. As cohorts age, this leads to increasing disparities in various outcomes (Dannefer 1987; DiPrete and Eirich 2006; O’Rand 1996). The cumulative disadvantage framework has been employed to study health inequalities over the lifecourse because many health outcomes are a product of accumulated exposures and behavioral patterns initiated early in life and further shaped by social context (Ross and Wu 1996; Willson, Shuey and Elder 2007).
The association of excess body weight with higher morbidity and mortality has been well documented (brief review is below). Little is known, however, about the cumulative impact of excess body weight on health as people age (Ferraro and Kelley-Moore 2003). In this analysis, we conceptualize healthy body weight as a resource that may limit natural health decline as young adults age over a 20-year time period. We posit that excess body weight in early adulthood may act as one of mechanisms that produce cumulative disadvantage in the form of increasing health inequalities as a cohort ages. We further explore how sex and race, ascribed status factors that have a strong and persistent influence on life chances, are associated with the increasing inequalities in body weight and health in adulthood. Specifically, we ask whether the effect of weight on health change over time differs for men versus women, and for black versus white adults.
The cumulative disadvantage framework provides a sound theoretical foundation for studies that consider changes in body weight over time. Body weight early in life strongly influences weight at older ages; people who are overweight when they are young are more likely to be obese at older ages (Serdula et al. 1993), potentially leading to diverging weight trajectories consistent with the cumulative disadvantage pattern. Moreover, excess body weight may exert effects on health that are minimal in the short term but accumulate the over the long term, through a process of “wear and tear” on body and organ systems. Shaefer and Ferraro (2007), for instance, found that the more time people lived obese, the more health services they used in later life. Studying early-adulthood body weight patterns could thus help us better understand the negative health consequences of obesity at older ages (Scharoun-Lee et al. 2009).
Body weight is both a consequence and a cause of social stratification. The prevalence of obesity has been increasing steadily in the U.S. for several decades, but not equally for all social groups (Flegal et al. 1998; Freedman et al. 2002). Obesity rates vary greatly by major ascribed and achieved social status characteristics, including sex, race/ethnicity, and education (Mokdad et al. 2003; Ogden et al. 2006). Excess body weight in turn predicts key socioeconomic outcomes including labor market location and wages (Cawley 2007; Finkelstein, Ruhm and Kosa 2005). Obesity impacts people’s social well-being too, as the obese are stigmatized and discriminated against (Carr and Friedman 2005). These factors make social disparities in excess body weight a critical sociological and public health problem, as well as a fruitful area to better understand processes of cumulative disadvantage that may underlie health disparities.
Prior Research
About two thirds of U.S. adults are overweight or obese (Hedley et al. 2004; Ogden et al. 2006). This high prevalence of excess weight has motivated extensive social epidemiological research into its effects on health outcomes, especially mortality (Bender et al. 1998). Most researchers agree that a body mass index (BMI) in the obesity range is associated with an increased risk of death (Allison et al. 1999; Mokdad et al. 2003). Excess body weight also is associated with higher health care costs (Finkelstein, Ruhm and Kosa 2005; Wolf and Colditz 1998). The increased costs are in part due to a higher prevalence of chronic conditions including diabetes, cardiovascular disease, and cancer among obese adults (Calle et al. 2003; Mokdad et al. 2003; Wannamethee, Shaper and Walker 2005), as well as functional limitations and disabilities (Alley and Chang 2007; Ferraro and Booth 1999; Ferraro et al. 2002).
Relatively few studies have examined the effect of excess body weight on self-rated health (SRH) (Ferraro and Booth 1999; Ford et al. 2001). This is a crucial gap in the literature because SRH is an excellent comprehensive indicator of individual and population health status (Idler and Benyamini 1997). Reports of SRH are thought to reflect underlying health changes that occur before a diagnosis of an illness or disability. They may thus capture an individual’s actual health status more closely than clinical measures (Ferraro, Farmer and Wybraniec 1997; Goldman 2001), especially for young people who have not yet developed major health problems. Strong support for the validity of the SRH measure comes from studies that show it to be an excellent predictor of mortality (Idler and Benyamini 1997; Idler, Russell and Davis 2000) and other health outcomes (Bailis, Segall and Chipperfield 2003; Ferraro, Farmer and Wybraniec 1997).
Ferraro and Yu (1995) published a widely cited study that focused on the association between body weight and SRH among adults and elderly. They found a significant relationship, although attributable largely to poor health of the most obese individuals. Several additional studies have corroborated the weight-SRH association. Okosun (2001), for instance, found that obese adults and elderly were 1.5-2.4 times as likely to rate their health poorly than normal-weight adults. The existing studies, however, have several important limitations. The first is the nature of their data: some were based on non-representative samples such as older Southern women (Ramsey and Glenn 2002), urban chronic-disease patients (Katz, McHorney and Atkinson 2000), or the Appalachian elderly (Goins, Spencer and Krummel 2003). Other studies used samples representative of the US population, but included a wide age range, from young adults to elderly (Ford et al. 2001; Heo et al. 2003a; Okosun et al. 2001). While a broad age range allows for generalization to the population, it complicates drawing inferences about the lifecourse patterns of the relationship and the mechanisms through which weight impacts health.
Another limitation for understanding the process by which excess body weight impacts health over time is that the previous studies relied on cross-sectional data. An assessment of the association between weight and health at a single time point provides only a circumscribed picture of the relationship for several reasons. First, both BMI and SRH are dynamic constructs that vary systematically over the lifecourse. The trajectory of BMI follows an inverse-U shape pattern as people age (Heo et al. 2003b), while health ratings generally decline as people grow older (Lynch 2003; McDonough and Berglund 2003). Taking into account the interplay of these two trajectories across the lifecourse is important and possible only with longitudinal data and an adequate analytic approach. Second, excess body weight may take time to affect health. The impact of obesity may not be obvious at a young age, but over time the cumulative burden of excess weight may result in a faster health decline. Only with longitudinal data is it possible to examine whether heavier young adults experience a faster decline in health as they get older, relative to those who have lower body weights early in life, as the cumulative disadvantage framework would predict.
A final limitation of prior studies is that few have examined the association between excess weight and health separately by sex and/or race, although there are many reasons to expect group differences. The distributions of both BMI and SRH vary considerably by sex and race. Black adults are more likely to be obese than white adults, with the difference particularly large for women (Boardman et al. 2005; Ogden et al. 2006). Self rated health tends to be lower among women than men (Gorman and Read 2006; Ross and Bird 1994) and lower among black adults than white adults (Cagney, Browning and Wen 2005; Farmer and Ferraro 2005). The association between BMI and health outcomes may also vary by sex and race. In studies of mortality, excess weight seems less detrimental for women than for men (Bender et al. 1999; Idler, Russell and Davis 2000), and also less detrimental for black adults than white adults (Durazo-Arvizu et al. 1997; Kumanyika 1993). In contrast, studies show excess weight more strongly related to SRH for women than for men (Katz, McHorney and Atkinson 2000; Okosun et al. 2001). The BMI-SRH association may also differ by race, although the literature is inconsistent: Okosun (2001) found a stronger association for white adults than for black adults, while others found the opposite pattern (Katz, McHorney and Atkinson 2000), or no significant race differences (Ferraro and Yu 1995). Relative to men and to white adults, women and Black adults face systematic disadvantage throughout the lifecourse with respect to many resources, including income, occupational prestige, or power. These disadvantages might multiply the detrimental effects of excess body weight, producing a stronger association between BMI and health changes with age for disadvantaged groups.
Contributions
Building on past findings, our study makes several contributions to the research linking body weight to health over the life course. First, this study is the first to use multi-wave data covering 20 years to examine the weight-health relationship as people age. This long period is essential to detect gradual changes in a relatively stable construct like self rated health. Second, our latent growth modeling approach is optimal for exploring the cumulative disadvantage model of health change within cohorts. The approach is also ideal in terms of the subjective nature of health reports. It is likely that people incorporate the awareness of health risks associated with excess body weight into their judgments about their overall health (Goldman, Glei and Chang 2004; Krause and Jay 1994), beyond any direct health effects they may experience. Following a trajectory of self-reported health over time may filter out individual variation in how people include excess body weight into their health evaluation, isolating the consequences of the gradual wear and tear on the physical health condition.
Third, while many studies focused on the elderly, we examine a relatively young sample, following them through mid-adulthood to observe how early life differences may contribute to diverging lifecourse trajectories within and across social groups over time. The young sample also means that our findings are less likely to be biased by selective mortality prior to and during the study, compared to research focused on older adults. Moreover, findings among younger adults are less vulnerable to reverse causality. Serious illnesses such as cancer often cause weight loss, so studies of older adults, where these diseases are more prevalent, may show an association between weight and health because poor health causes low body weight (Ferraro and Kelley-Moore 2003). Understanding how excess body weight contributes to the widening of health inequalities as people age allows the opportunity for medical and lifestyle interventions in earlier life that could result in better health for vulnerable groups at older ages, and provides a way to interrupt processes of cumulative disadvantage. A final contribution is the examination of the BMI-SRH association by sex and race. Disaggregating the sample allows us to consider how the multiple disadvantages of women and black adults, relative to men and whites, may intersect with the cumulative effects of body weight to generate gradually widening health inequalities across these groups as they age. Doing so will contribute to understanding social differentiation in health over the life course.
METHODS
Data
Data for this analysis are from the NHANES I Epidemiologic Follow-up Study (NHEFS), a nationally-representative longitudinal survey designed to investigate health and nutritional status among U.S. adults. The NHEFS survey included all adults age 25-74 who completed a medical examination at the baseline NHANES I study, and followed them over the course of 20 years. The NHANES I interviews were conducted in 1971-75 and follow-up data were collected in 1982-84, 1987, and 1992-93. The NHANES I was administered in several modules. About half the respondents received a detailed module with a battery of questions that included a self-rated health item. Our analyses are based on NHEFS cohort from this detailed-module group who were 25-39 years old at the baseline, excluding 38 respondents who reported their race as other than black or white and an additional 89 who were underweight (BMI<18.5) at the baseline. The analysis sample thus comprises 2,044 respondents. Compared to same-age adults who did not answer the self-rated health item, this analytic sample includes more males and black adults but is comparable on other sociodemographic variables such as marital status and region of residence.
The baseline NHANES I interviews were completed with 99% of sampled individuals. Of those, about 74% also completed the medical examination and thus were included in the NHEFS followup. Tracing and re-interview rates were high at all follow-up waves. Over the course of the study, 89 respondents from baseline analytic sample (4.3%) were known to have died. In the first follow-up wave in 1982, 93% of the baseline respondents were traced successfully, 93% of the baseline respondents were traced in 1987, and 86% in 1992. Of those traced alive at each wave, interviews were conducted with 88% individuals in 1982-84, 90% in 1987, and 94% in 1992. Respondents who were older, male, less educated, and who reported a higher BMI and lower SRH were more likely to die during the course of the study; respondents who were younger, black, and less educated were more likely to be lost to follow-up.1
Measures
Self-rated health (SRH) and body-mass index (BMI) are included in the models as time-varying outcomes, measured at all four waves of the survey. All other variables are entered as time-invariant predictors measured at the baseline. SRH was collected identically at each wave: respondents were asked “Would you say your health in general is excellent, very good, good, fair, or poor?” It is coded as on a 5-point scale, with 5 representing excellent health and 1 poor health. BMI is calculated as weight in kilograms divided by height in meters squared. Normal weight is defined as BMI between 18.5 and 24.9, overweight corresponds to BMI between 25 and 29.9, and obesity is BMI above 30kg/m2 (NHLBI 1998). Height and weight were measured by physicians during the baseline medical examination. Weight was also measured at the first follow-up and was self-reported in the remaining two waves.
Sociodemographic variables include sex, race, marital status, region of residence, education, and age. Sex, race, marital status, and region are dichotomized, with female, black, south, and unmarried people coded as 1 and others coded as 0, respectively. Education is measured as completed years of schooling. Age, ranging from 25 to 39 years at baseline, is also measured in single years. Health behaviors include smoking, drinking and exercise. Controlling for smoking is essential since smoking status is strongly related to both weight and health (Flegal et al. 1995). Smoking status, which includes cigarette, cigar, or pipe use, is trichotomized: respondents who never smoked (reference category), past smokers, and current smokers. Alcohol use is a dichotomous covariate constructed from frequency and amount of consumption. Respondents who reported drinking 3 or more drinks “every day” or “just about every day” were coded as heavy drinkers. Exercise is also dichotomized; respondents who indicated that they get “much” exercise were coded as exercisers, and those who indicated none to moderate exercise were coded as non-exercisers. Health conditions indicate the number of medical diagnoses at baseline: in the baseline interview, physicians examined the survey participants and reported their findings using the ICD-9 classification. We examined a number of alternative coding schemes for the health behaviors and medical conditions, but the variations did not have any impact on our findings.
Analysis Plan
We employ latent growth modeling, a class of structural equation models (Meredith and Tisak 1990). These models estimate the mean trajectory of a latent (unobserved) variable over time as a function of an underlying growth process; assess individual heterogeneity around this trajectory; and relate this heterogeneity to individual characteristics (Bollen and Curran 2005). Latent growth models are similar to hierarchical random-coefficient models, in that the repeated measures of a variable such as SRH are nested within individuals (level 1), and the individual growth parameters are modeled as a function of individual-level predictors (level 2).
The analysis proceeds in two stages. First, we fit separate trajectories of BMI and SRH, to determine the functional form of the weight and health growth processes. All models are adjusted for age. The measures collected at the four survey waves are conceptualized as imperfect indicators (indicators measured with error) of a general latent growth process (such as health decline over time). The growth process is described by two factors, an intercept and a slope. The intercept represents the starting point of the trajectory. The slope coefficient represents change per unit of time (in our analysis, a 5-year period as a function of the spacing of survey waves); and can be specified as linear or may have an alternative functional form. The models also estimate the intercept and slope variances, which capture individual variability (heterogeneity) around the sample means.
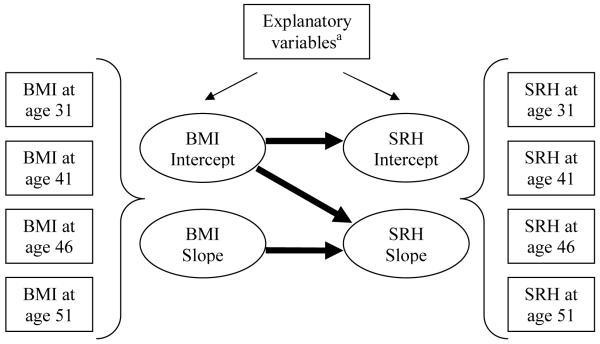
In the next stage of the analysis, the intercept and slope of the SRH trajectory become dependent variables modeled as a function of the BMI intercept and slope, as well as other predictors: demographic characteristics, health behaviors, and health conditions. The parameter estimates indicate how much these predictors affect baseline SRH and the change in SRH over time.2 A simplified model is shown in Figure 1.
Figure 1.
Double-Trajectory Latent Growth Models Estimating the Effect of BMI on SRH
Note: Rectangles indicate observed variables; ovals indicate latent (unobserved) variables. After estimating the BMI and SRH trajectories separately, we analyze their relationship -- the three thick arrows indicate the main coefficients of interest.
aThe explanatory variables include age, sociodemographic predictors, health behaviors, and medical conditions.
We fit models for the full sample, as well as for the four sex/race groups separately. The sex/race stratified models allow for a comparison of the weight-health relationships across groups. The comparison is formalized using a multiple-group analysis, which tests whether the association between weight and health differs significantly among the four groups. This is done by comparing a pair of models: (1) a model where the effect of the BMI intercept and slope on the SRH trajectory is constrained to be equal across a pair of groups, and (2) another model where the effects are estimated freely for each group. A significant improvement in the chi squared statistic from the restricted to the unrestricted model indicates that the BMI-SRH association differs across the groups.
To evaluate the fit of the models to the data, we use multiple indices. Chi-square serves at a formal statistical method for evaluating models: a non-significant result indicates a good fit to the data. This test is, however, sensitive to sample size, and chi-square value for samples over 200 are inflated toward significance. Additional indices are therefore used; the comparative fit index (CFI) indicates a good fit to the data at values above 0.95, while the root mean square error of approximation (RMSEA) should be less than 0.05 (see Hu and Bentler 1998).
Descriptive statistics are conducted with Stata 10.1. Multivariate analyses are conducted with Mplus 5.1, using a full-information maximum likelihood estimator (FIML). This approach accommodates missing data by calculating each model statistic using all available data for that particular statistic (Muthén and Muthén 2006). Unlike listwise deletion, FIML thus preserves information on individuals who drop out during the course of the study. Under the missing at random (MAR) assumption (see Little and Rubin 1987), FIML produces unbiased parameter estimates (Wothke 2000). Most of the attrition was due to loss to follow-up and not to mortality, and was not related to baseline health, providing support for the MAR assumption, and by extension, for the unbiasedness of the findings.
RESULTS
Descriptive statistics
Table 1 presents the characteristics of the sample at baseline.
Table 1.
Characteristics of the Sample at Baseline, Overall and by Sex and Race
| Overall | White men | White women |
Black men | Black women |
Group differencec |
|
|---|---|---|---|---|---|---|
| Weight (BMI, mean)a | 25.1 | 25.6 | 24.1 | 27.2 | 26.9 | *** |
| Normal weight | 57.3% | 48.9% | 69.4% | 33.9% | 46.7% | |
| Overweight | 30.8% | 40.6% | 20.0% | 48.1% | 26.5% | |
| Obese | 11.9% | 10.5% | 10.6% | 18.2% | 26.8% | |
| Health (SRH, mean) | 3.9 | 4.0 | 3.9 | 3.6 | 3.0 | *** |
| Excellent/very good | 63.4% | 69.4% | 63.1% | 53.2% | 30.2% | |
| Good | 28.0% | 25.6% | 28.5% | 35.2% | 35.7% | |
| Fair/poor | 8.6% | 4.9% | 8.4% | 11.6% | 34.0% | |
| Age (mean) | 31.5 | 31.3 | 31.6 | 31.8 | 31.1 | n.s. |
| Education (mean) | 12.4 | 12.9 | 12.1 | 11.6 | 11.1 | *** |
| Married | 80.9% | 84.0% | 82.7% | 77.5% | 48.2% | *** |
| Region = South | 23.0% | 18.8% | 23.5% | 36.8% | 38.8% | *** |
| Smoking | *** | |||||
| Current | 50.2% | 58.1% | 38.3% | 73.7% | 62.8% | |
| Past | 15.7% | 17.7% | 15.9% | 9.5% | 4.9% | |
| Never | 34.1% | 24.3% | 45.8% | 16.8% | 32.3% | |
| Heavy drinking | 11.1% | 20.0% | 3.7% | 6.7% | 5.7% | *** |
| Exercise | 24.2% | 32.2% | 19.0% | 24.3% | 4.9% | *** |
| Medical conditionsb | n.s. | |||||
| 0 | 62.1% | 61.5% | 64.2% | 52.9% | 58.1% | |
| 1 | 25.3% | 26.7% | 22.7% | 38.2% | 24.9% | |
| 2+ | 12.6% | 11.8% | 13.1% | 9.0% | 17.0% | |
|
|
||||||
| N | 2,044 | 799 | 1,000 | 97 | 148 | |
p<.001, two-tailed
Note: Adjusted for sampling design.
The sample excludes adults who were underweight (BMI<18.5) at the baseline.
Indicates the number of conditions diagnosed by physicians at the baseline examination.
Indicates p-value of a design-adjusted F test for the association between sex/race groups and categorical predictors and an adjusted Wald test for group differences in continuous variables.
The mean sample BMI was 25.1, just above the overweight threshold. White men and women had lower mean BMI than their black counterparts. White women were most likely to have a normal body weight, while black women were most likely to be obese, compared to the other groups. In the full sample, the mean health rating was 3.9, just below “very good.” Almost two thirds of the sample reported excellent or very good health; fewer than 9% reported fair or poor health. There were stark differences in health ratings among the four groups: black adults, particularly women, reported considerably worse health than white respondents. These differences are notable since there were no significant differences in diagnosed medical conditions among the four groups. Less than one third of black women reported excellent or very good health; more than a third reported fair/poor health.
Age-adjusted latent growth models for BMI and SRH
Table 2 shows results from the first part of the multivariate analyses, estimating age-adjusted latent growth models for BMI and SRH.3
Table 2.
Single-Trajectory Latent Growth Models of BMI and SRH, for Full Sample and by Sex and Race
| Model 1: BMI |
Model 2: SRH |
|||
|---|---|---|---|---|
| Full sample model | Intercept | Slope | Intercept | Slope |
| Mean | 25.01*** | .60*** | 3.91*** | −.06*** |
| Variance | 23.78*** | .59*** | .58*** | .02*** |
| Effect of age (standardized) | .09*** | −.05 | −.11*** | −.00 |
| Covariance (Int.& Slope) | −.70*** | −.03* | ||
| Indicator reliabilities | ||||
| Wave 1 | .97 | .55 | ||
| Wave 2 | .85 | .55 | ||
| Wave 3 | .88 | .59 | ||
| Wave 4 | .93 | .65 | ||
| Fit indices | ||||
| Chi square (d.f.) | 40*** (6) | 32*** (6) | ||
| CFI | .995 | .988 | ||
| RMSEA | .052 | .046 | ||
|
|
||||
| Sex/Race-specific modelsa | Model 1: BMI |
Model 2: SRH |
||
|---|---|---|---|---|
| Intercept | Slope | Intercept | Slope | |
| White men (mean) | 25.54*** | .56*** | 4.05*** | −.07*** |
| White women (mean) | 24.11*** | .61*** | 3.96*** | −.06*** |
| Black men (mean) | 27.01** | .74*** | 3.60*** | −.11** |
| Black women (mean) | 26.93** | .67*** | 3.10*** | −.05 |
p<.05
p<.01
p<.001, two-tailed
Note: The BMI and SRH trajectories are estimated separately in this table.
The sex/race-specific models, specified the same way as the all-sample model above, show only the intercept and slope of each trajectory; additional results are omitted for parsimony. Across the race/sex groups, the fit indices suggest an adequate to excellent model fit for all eight models. The CFI, for instance, ranges from .980 for black men to .998 for white men in the BMI models, and from .923 for black women to .994 for white women in the SRH models.
The left columns in Table 2 show results for the BMI trajectory. The initial BMI (intercept) for the full sample was 25.0; the slope, which indicates change in BMI per 5-year period, was 0.6. This means that during the 20-year follow-up, the average adult saw their BMI increase to 27.4, in the middle of the overweight range. The variances in the intercept and slope, 23.8 and 0.6 respectively, were highly significant, implying a substantial degree of heterogeneity in the weight pattern over time. The indicator reliabilities for all waves were high, ranging from 0.85 to 0.97. These values indicate the proportion of total variance in the BMI measures at each wave explained by the growth trajectory; they suggest that the linear growth pattern fit the data very well. The fit indices also suggested a good fit, with CFI > 0.99 and RMSEA just above 0.05.
The right columns in Table 2 show results for the SRH trajectory model. The initial SRH was 3.9 and declined by 0.06 per 5-year period, so at the end of follow-up the average health rating was 3.67. This rate of decline is slightly lower than some previous estimates (McDonough and Berglund 2003; Umberson et al. 2006), likely because the decline may accelerate with age and our sample was relatively young. The variances of health intercept and slope showed a significant amount of individual variability around the mean estimates. The indicator reliabilities were moderately high (0.55 to 0.65), indicating that the linear shape of the health trajectory captured the variation in the wave-specific health ratings adequately. The chi square was significant (p < .05) but CFI (0.988) and RMSEA (0.046) both suggested a good fit to the data.
Findings from sex- and race-specific BMI models are shown in the bottom panel of Table 2. They indicate that white women started with the lowest body weight (their BMI intercept was 24.1), while black men experienced the steepest increases in BMI over time (BMI slope = 0.74). The average black man in the sample started with a BMI of 27, which increased to 30 over the follow-up, just at the overweight/obese threshold value. Comparable models for SRH show white men and women to have similar health trajectories, starting around 4 (corresponding to very good health) and declining at similar rates over time. Black men started with a lower SRH of 3.6, which declined at a much steeper rate. Black women began the survey with an average SRH of only 3 (good health), although their decline was slightly slower than for white adults. Due to the small number of black men and women, however, the results for these groups should be viewed as tentative until confirmed with a larger sample from a different data source.
Double-trajectory models – does body weight affect health changes over time?
In the second part of the analysis, the health trajectory was modeled as a function of the BMI intercept and slope. The results, which gradually adjust for all baseline covariates, are presented in Table 3 for the full sample and separately by sex and race groups.
Table 3.
Double-Trajectory Latent Growth Models Estimating the Effect of BMI on SRH, for Full Sample and by Sex and Race
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Full sample (N=2,044) | ||||
| Effect of BMI int. on health int. | −.20*** | −.14*** | −.13*** | −.12*** |
| Effect of BMI int. on health slope | −.22*** | −.23*** | −.23*** | −.24*** |
| Effect of BMI slope on health slope | −.20*** | −.16*** | −.16*** | −.16*** |
| Chi squared | 94***(25) | 96***(37) | 113***(53) | 115***(57) |
| CFI | .993 | .994 | .994 | .994 |
| RMSEA | .037 | .028 | .023 | .022 |
| White men (N=799) | ||||
| Effect of BMI int. on health int. | −.07 | −.06 | −.06 | −.04 |
| Effect of BMI int. on health slope | −.20** | −.20** | −.20** | −.21** |
| Effect of BMI slope on health slope | −.26*** | −.19** | −.18** | −.19** |
| Chi squared | 40*** (25) | 48*** (37) | 63*** (53) | 64*** (57) |
| CFI | .996 | .997 | .997 | .998 |
| RMSEA | .027 | .019 | .016 | .012 |
| White women (N=1,000) | ||||
| Effect of BMI int. on health int. | −.25*** | −.17*** | −.16*** | −.14*** |
| Effect of BMI int. on health slope | −.21** | −.24** | −.25*** | −.26*** |
| Effect of BMI slope on health slope | −.19** | −.18** | −.20** | −.20** |
| Chi squared | 71*** (25) | 85*** (37) | 91*** (53) | 93*** (57) |
| CFI | .991 | .990 | .992 | .993 |
| RMSEA | .043 | .036 | .027 | .025 |
| Black men (N=97) | ||||
| Effect of BMI int. on health int. | −.01 | −.02 | −.01 | −.01 |
| Effect of BMI int. on health slope | −.30 | −.35 | −.32 | −.25 |
| Effect of BMI slope on health slope | .10 | .43 | .49 | .31 |
| Chi squared | 36 (28) | 49 (40) | 60 (56) | 65 (60) |
| CFI | .976 | .973 | .987 | .987 |
| RMSEA | .054 | .049 | .029 | .028 |
| Black women (N=148) | ||||
| Effect of BMI int. on health int. | −.19 | −.10 | −.08 | −.08 |
| Effect of BMI int. on health slope | −.40 | −.40 | −.37 | −.34 |
| Effect of BMI slope on health slope | .60 | .45 | .41 | .34 |
| Chi squared | 36 (28) | 48 (40) | 65 (56) | 72 (61) |
| CFI | .984 | .984 | .983 | .980 |
| RMSEA | .044 | .037 | .033 | .035 |
p<.05
p<.01
p<.001, two-tailed
Note: Shown are standardized coefficients and model fit indices for all 20 models. See note 3 for model specification details. Model 1 adjusts for age, Model 2 also adjusts for sociodemographic factors, Model 3 adds health behaviors, and Model 4 adds for medical conditions.
Model 1 shows the age-adjusted BMI-SRH association. For the full sample, BMI had a strong effect on SRH. A high initial BMI predicted both a lower initial SRH (−0.20), as well as a steeper decline in SRH over time (−0.22). A larger increase in BMI over time also predicted a steeper decline in health over time (−0.20). The coefficients are standardized: they measure the effects in standard deviation units. For instance, the effect of initial BMI on initial SRH (−0.2) means that for every standard deviation increase in BMI, SRH declined by 0.2 standard deviations. The chi squared statistic for Model 1 was significant (94, d.f. = 25) but the CFI (0.993) and RMSEA (0.037) both indicated a good fit to the data.
The four sets of results below summarize sex/race group-specific findings. White men and women evidenced relatively similar and significant effects of weight on health changes over time: higher starting BMI and more weight gain were both associated with a steeper health decline. White men and women differed in whether initial BMI was related to initial SRH: there was no association for men while the association was negative and highly significant for women. None of the associations for black adults were significant, but these null findings may be due to the small samples for these groups and underpowered models (Muthén and Muthén 2002). We can, however, look at the size and direction of the effects cautiously. It appears that the effect of high initial BMI on steeper health declines over time was large for Black adults. Curiously, gaining more weight over time appeared to be associated with a slower health decline, in contrast to the findings for white adults. A larger sample will be needed to validate these findings.
To present the results in a more intuitive form, we plotted the predicted health trajectories by sex and race at different levels of initial BMI in Figure 2.
Figure 2.
Predicted Trajectories of SRH at Different Initial BMI levels
Note: The plots are based on data from age-adjusted double-trajectory models as shown in Table 3. The initial BMI is 20, 25, or 35; BMI change over time is assumed to be equal to the group-specific mean change.
The figure shows that white respondents started the study with a considerably higher SRH than their black counterparts. Additionally, the decline in SRH over time was steeper in black adults, a pattern that corroborates previous findings of increasing racial health disparities through adulthood (House et al. 1994; Ross and Wu 1996). The effect of initial BMI on initial health was larger among women (especially white women) than among men.
Explaining the BMI-SRH association
Models 2 through 4 in Table 3 add blocks of predictors to assess whether they explain the association between BMI and SRH trajectories. These predictors were measured at baseline so they are likely to impact the initial BMI-SRH association more than health changes over time. Model 2 for the full sample, in the top panel of Table 3, shows that sociodemographic factors --- marital status, education, and region of residence--- explained 30% of the initial BMI-SRH association ((−0.20+0.14)/−0.20 = 0.30) but little of the effect of initial weight on health slope. Interestingly, these controls also accounted for 20% of the effect of BMI slope on SRH slope. Adding health behaviors (Model 3) and medical conditions (Model 4) explained little of the remaining BMI-SRH association.
Sex/race-specific models in subsequent panels show that among white women, sociodemographic factors explained almost a third of the association between baseline weight and health. Additional analyses (not shown) indicated that the reduction was mainly attributable to education: less educated white women had a higher BMI and lower SRH. The models for black women suggested a similar pattern, with sociodemographic factors accounting for almost half of the baseline BMI-SRH association. However, we need to keep in mind that the baseline BMI-SRH association was not significant for black women in the age-adjusted model. As in the full-sample models, the additions of the baseline controls explained little of the BMI slope effects in the group-specific models.
Sex/race differences in the BMI-SRH association
In order to evaluate whether the group differences in the BMI-SRH association suggested in Table 3 were statistically significant, we tested six multiple-group models. Table 4 shows the results.
Table 4.
Comparison of the BMI-SRH Association across Sex/Race Groups
| White men | White women | Black men | Black women | |
|---|---|---|---|---|
| White men | --- | |||
| White women | 8.64* | --- | ||
| Black men | 1.57 | 4.72 | --- | |
| Black women | 7.61 | 6.44 | 1.75 | --- |
p<.05, two-tailed
Note: The table shows the difference in the chi squared statistics between restricted and unrestricted models (degrees of freedom = 3).
The differences among the four groups were not found to be statistically significant, except for a significant finding between white men and white women. Additional analyses (not shown) showed that this difference was due to the baseline association: the effect of initial weight on initial health was significantly stronger among white women than white men. Whether the null result for the other comparisons was due to the low power of the black-respondent models or because the groups were indeed similar remains to be verified in the future with a larger sample.
Additional sensitivity analyses
We explored several modeling issues crucial to the validity of our findings. First, we needed to ascertain that the observed weight-health relationship was not biased by high-leverage cases at the tails of the BMI distribution. We estimated two series of sex/race-stratified models in which we restricted the initial BMI range to 20 to 35; these results showed no substantive changes from those presented. Second, we addressed the possibility of reverse causation, whereby health would affect body weight rather than vice versa. We estimated a series of parallel-process models where the changes in SRH were a function of initial BMI, and the changes in BMI were a function of initial SRH. The results from these models, in Table 5, showed that while health changes over time depended on initial BMI, initial health did not influence the BMI trajectory in any demographic group (although there was a small but significant effect for the full sample).
Table 5.
Effect of Initial BMI on SRH Slope and Initial SRH on BMI Slope, for Full Sample and by Sex/Race Groups
| Overall | White men |
White women |
Black men |
Black women |
|
|---|---|---|---|---|---|
| Effect of | |||||
| BMI Intercept on SRH Slope | −.19*** | −.13* | −.19** | −.25 | −.78** |
| SRH Intercept on BMI Slope | −.07* | −.08 | −.06 | .07 | .05 |
p<.05
p<.01
p<.001, two-tailed
Note: The models also include a correlation between the intercepts of the BMI and the SRH trajectories.
A third issue to explore was the complex sampling design of NHANES I. The nature of our models combined with the modest sample sizes meant that the sampling-design-adjusted models for black groups did not converge. To test whether our unadjusted results were comparable to the adjusted results, we estimated a series of cross-sectional models predicting baseline SRH as a function of baseline BMI, comparing survey-adjusted and unadjusted models. We found the coefficients and their standard errors to be essentially identical. Finally, we explored the specification of the health variable: SRH was modeled as a continuous indicator due to sample size constraints, rather than as an ordinal indicator. We estimated full-sample models (for which we had a sufficiently large sample) using an ordinal specification for SRH and found the results comparable to those presented here.
DISCUSSION
In this study, we examined how body weight affects health over time as people age from early to mid-adulthood. Our results fill a large gap in the sociological literature on health stratification, focusing on health consequences of excess body weight. While it is known that excess body weight tends to be associated with worse health outcomes, much of the prior research focused on older adults and relied on a cross-sectional snapshot of the association. In contrast, we considered the weight-health association within the cumulative advantage perspective. Our aim was to understand whether excess body weight contributed to gradual increases in health inequalities in early adulthood.
We found that as people aged from their early thirties to early fifties, their body weight increased and their health ratings declined gradually. The rate of health change was dependent on body weight: on average, adults with a higher initial BMI experienced a significantly steeper health decline with age, compared to their leaner counterparts. This finding offers support for the cumulative disadvantage processes by documenting how initial body weight plays a role in the expected “fanning out” pattern in health. For the cohort, this process would manifest as increasing health inequalities as a function of early-adulthood body weight.
Additionally, we found that adults who gained more weight during the course of the study also saw their health ratings decrease faster, consistent with additional accumulation of wear and tear on the body as implied by cumulative disadvantage processes. These findings generally corroborate previous studies about the negative health consequences of excess body weight on health outcomes (i.e., Calle et al. 2003; Ferraro et al. 2002; Mokdad et al. 2003). Our findings further document the faster health deterioration among heavier people that is evident already in early adulthood.
The overall patterns varied somewhat across demographic groups. Focusing on white men and women, we found that the cumulative weight-health relationship that developed over the 20-year follow-up was strong and similar in both groups: starting heavier and gaining more weight were both associated with a faster health decline. In other words, we found no pronounced modifying effect of sex on the cumulative patterns in early to mid-adulthood: the growth of health inequalities occurred at comparable rates. The men and women differed, however, in where they started. In their early thirties, white men’s health ratings were unrelated to their body weight. Heavier white women, however, rated their health significantly lower in this age group. This difference supports previous research that also found women’s health ratings more affected by their body weight than men’s ratings (Okosun et al. 2001). To the extent that the initial association observed in the data may be a function of prior cumulative processes in adolescence and transition to adulthood that impacted women’s health more than men’s, this pattern may be consistent the cumulative disadvantage perspective.
The initial weight-health association observed only for white women was partially explained by –educational attainment; less educated women tended to both be heavier and to report poorer health—but not health behaviors and medical conditions. Perhaps the findings are due to differences between men and women in the health evaluation process, in particular how excess weight is incorporated into the health rating (Idler, Russell and Davis 2000). Overweight adults, aware of the health risks associated with high BMI, may adjust their health rating accordingly (Ferraro and Yu 1995; Goldman, Glei and Chang 2004). Excess body weight is stigmatized in the US society (Crosnoe and Muller 2004); more among white women than among other groups (Ross 1994; Sobal and Stunkard 1989). Consequently, white women may consider excess body weight as more detrimental and lower their health ratings accordingly.
The number of black men and women available in the NHEFS sample was too small to draw conclusions about the weight-health association these groups. Parts of the analysis, however, produced valuable results: we documented that black men and women not only start with a higher body weight than white adults but also gain more as they age into mid-adulthood. The health ratings of black men and women also differed from their white counterparts: black women reported a particularly low health in their early 30s, on average assessing their health as only “good,” and black men evidenced the most rapid health declines over the follow-up period. These patterns are generally consistent with prior reports (Ferraro and Farmer 1996). Other data sources will be needed to conclusively document the gradual and cumulative impact of excess body weight on health ratings of black young adults, and the ways these may contribute to racial disparities in health.
The NHEFS survey offered a unique opportunity to study health changes in a heterogeneous population within the cumulative disadvantage framework. This dataset is older but remains a widely used and highly regarded source of nationally representative data with excellent follow-up quality, well-measured covariates, and a large enough sample to consider a race-stratified inquiry. Nonetheless, a number of methodological issues in this study limit the strength of conclusions we can draw. Although the data covered a long follow-up period, the results describe only a small section of the life course, from the early thirties to the fifties. It would be desirable to follow a cohort of people across the entire lifecourse, in order to better understand the cumulative processes underlying divergence in health status. Not only may the effect of excess weight on health vary at different ages, but other factors, such as medical conditions, could begin to account for more of the association as they accumulate at older ages. Another limitation is that body weight was self-reported in the latter two waves. Self-reported weight may be underreported, leading to a flatter BMI trajectory and thus to conservative estimates of the effects of weight on health changes over time. Finally, we did not account for the time-dependent nature of some predictors, such as new medical conditions that were diagnosed during the follow-up. Doing so would make the models prohibitively complex – it could, however, help explain the mechanisms through which excess weight affects health over time.
This study generated a number of questions for further research. We suggest two lines of inquiry that could help extend and explain our findings. Researchers should examine alternative measures of health, such as physical limitations or chronic conditions like diabetes, within the cumulative disadvantage framework to clarify the mechanisms through which excess body weight affects health in adulthood. Another line of research, ideally using qualitative studies, should investigate the impact of excess weight on the health evaluation process of young adults, focusing particularly on differences between men and women. How does excess body weight affect the health attribution process among adults in different social and demographic groups?
BIOSKETCHES
Anna Zajacova is a National Institute on Aging postdoctoral researcher at the Population Studies Center at University of Michigan. Her research interests center on socio-economic determinants of health among adults across the lifecourse. She has recently published papers on the association between education and mortality among men and women, on mortality selection, and on socioeconomic correlates of infection and inflammation.
Sarah A. Burgard is Assistant Professor of Sociology, Assistant Research Scientist at the Population Studies Center, and Joint Assistant Professor of Epidemiology at the University of Michigan. Her work examines the consequences of social stratification for population health and health disparities. She studies the links between working conditions and adult health over the career as well as the multilevel social determinants of the health of children and adolescents in multiple international contexts.
Footnotes
Not only is the attrition low for a survey of this duration, but also our analytic approach includes attriters. The full-information maximum likelihood estimator uses all available data points on all individuals, whether they attritted or not. Auxiliary analyses suggested that the exclusion of attriters would result in somewhat stronger findings, so our analytic approach provides somewhat conservative estimates, as compared to estimates that would be obtained under the more common (and more bias-inducing) casewise deletion approach.
The model thus assumes a linear association between BMI and SRH. While the association between BMI and health is known to be curvilinear (with worse health among the lightest and heaviest individuals), the nonlinearity is accounted for mainly by underweight individuals, and we excluded underweight adults from the analytic sample. Additional analyses, available on request, show that the baseline association of BMI and SRH for the sample is reasonably linear.
We also examined alternative trajectory specifications for both BMI and SRH: a quadratic trajectory, as well as a fully latent specification where the last two slope indicators are freely estimated. The linear models were the best fit for both variables although SRH shows some acceleration in decline over time, which a quadratic trajectory would also capture well. We selected the most parsimonious linear model for both BMI and SRH, but allowed a correlation between the 1982 and 1987 measurements of both weight and health in the full sample and white samples. These correlations were always positive and likely captured the minor curvature in the trajectories. All models for black men and women constrain the covariance between the SRH intercept and SRH slope to zero in order to achieve a positive latent variable covariance matrix, due to the small sample sizes available for these groups. Model 4 in Table 3 for black women also constrains the variance of the SRH slope to zero because of convergence issues.
We thank Brady West, Scott M. Lynch, Elizabeth M. Armstrong, and the editor and reviewers for insightful comments and suggestions on earlier versions of this paper. Both authors were supported by core funding from the Eunice Kennedy Shriver National Institute of Child Health & Human Development (R24 HD041028) and the National Institute on Aging (P30 AG012846-14) to the Population Studies Center, University of Michigan.
Contributor Information
Anna Zajacova, University of Michigan.
Sarah A. Burgard, University of Michigan
REFERENCES
- Alley Dawn E., Chang Virginia W. The Changing Relationship of Obesity and Disability, 1988-2004. JAMA. 2007;298:2020–2027. doi: 10.1001/jama.298.17.2020. [DOI] [PubMed] [Google Scholar]
- Allison David B., Fontaine Kevin R., Manson JoAnn E., Stevens June, VanItallie Theodore B. Annual Deaths Attributable to Obesity in the United States. JAMA. 1999;282:1530–38. doi: 10.1001/jama.282.16.1530. [DOI] [PubMed] [Google Scholar]
- Allison David B., Zhu Shankuan, Plankey Michael, Faith Myles S., Heo Moonseong. Differential Associations of Body Mass Index and Adiposity with All-Cause Mortality among Men in the First and Second National Health and Nutrition Examination Surveys (NHANES I and NHANES II) Follow-up Studies. International Journal of Obesity. 2002;26:410–6. doi: 10.1038/sj.ijo.0801925. [DOI] [PubMed] [Google Scholar]
- Bailis Daniel S., Segall Alexander, Chipperfield Judith G. Two Views of Self-Rated General Health Status. Social Science and Medicine. 2003;56:203–17. doi: 10.1016/s0277-9536(02)00020-5. [DOI] [PubMed] [Google Scholar]
- Bender Ralf, Jockel Karl H., Trautner Christoph, Spraul Maximilian, Berger Michael. Effect of Age on Excess Mortality in Obesity. JAMA. 1999;281:1498–504. doi: 10.1001/jama.281.16.1498. [DOI] [PubMed] [Google Scholar]
- Bender Ralf, Trautner Christoph, Spraul Maximilian, Berger Michael. Assessment of Excess Mortality in Obesity. American Journal of Epidemiology. 1998;147:42–8. doi: 10.1093/oxfordjournals.aje.a009365. [DOI] [PubMed] [Google Scholar]
- Boardman Jason D., Saint Onge Jarron M., Rogers Richard G., Denney Justin T. Race Differentials in Obesity: The Impact of Place. Journal of Health and Social Behavior. 2005;46:229–243. doi: 10.1177/002214650504600302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bollen Kenneth A., Curran Patrick J. Latent Curve Models: A Structural Equation Perspective. Wiley; Hoboken NJ: 2005. [Google Scholar]
- Cagney Kathleen A., Browning Christopher R., Wen Ming. Racial Disparities in Self-Rated Health at Older Ages: What Difference Does the Neighborhood Make? Journal of Gerontology: Social Sciences. 2005;60:S181–90. doi: 10.1093/geronb/60.4.s181. [DOI] [PubMed] [Google Scholar]
- Calle Eugenia E., Rodriguez Carmen, Walker-Thurmond Kimberly, Thun Michael J. Overweight, Obesity, and Mortality from Cancer in a Prospectively Studied Cohort of U.S. Adults. New England Journal of Medicine. 2003;348:1625–1638. doi: 10.1056/NEJMoa021423. [DOI] [PubMed] [Google Scholar]
- Carr Deborah, Friedman Michael A. Is Obesity Stigmatizing? Body Weight, Perceived Discrimination, and Psychological Well-Being in the United States. Journal of Health and Social Behavior. 2005;46:244–59. doi: 10.1177/002214650504600303. [DOI] [PubMed] [Google Scholar]
- Cawley John H. The Labor Market Impact of Obesity. In: Acs Zoltan J., Lyles Alan., editors. Obesity, Business and Public Policy. Edward Elgar; Northampton, MA: 2007. pp. 76–88. [Google Scholar]
- Crosnoe Robert, Muller Chandra. Body Mass Index, Academic Achievement, and School Context: Examining the Educational Experiences of Adolescents at Risk of Obesity. Journal of Health and Social Behavior. 2004;45:393–407. doi: 10.1177/002214650404500403. [DOI] [PubMed] [Google Scholar]
- Dannefer Dale. Aging as Intracohort Differentiation: Accentuation, the Matthew Effect, and the Life Course. Sociological Forum. 1987;2:211–236. [Google Scholar]
- DiPrete Thomas A., Eirich Gregory M. Cumulative Advantage as a Mechanism for Inequality: A Review of Theoretical and Empirical Developments. Annual Review of Sociology. 2006;32:271–297. [Google Scholar]
- Durazo-Arvizu Ramon, McGee Daniel, Li Zhaohai, Cooper Richard. Establishing the Nadir of the Body Mass Index-Mortality Relationship: a Case Study. Journal of American Statistical Association. 1997;92:312–9. [PubMed] [Google Scholar]
- Farmer Melissa M., Ferraro Kenneth F. Are Racial Disparities in Health Conditional on Socioeconomic Status? Social Science and Medicine. 2005;60:191–204. doi: 10.1016/j.socscimed.2004.04.026. [DOI] [PubMed] [Google Scholar]
- Ferraro Kenneth F., Booth Tara L. Age, Body Mass Index, and Functional Illness. Journal of Gerontology: Social Sciences. 1999;54:S339–48. doi: 10.1093/geronb/54b.6.s339. [DOI] [PubMed] [Google Scholar]
- Ferraro Kenneth F., Farmer Melissa M. Double Jeopardy, Aging as Leveler, or Persistent Health Inequality? A Longitudinal Analysis of White and Black Americans. Journal of Gerontology: Social Sciences. 1996;51B:S319–328. doi: 10.1093/geronb/51b.6.s319. [DOI] [PubMed] [Google Scholar]
- Ferraro Kenneth F., Farmer Melissa M., Wybraniec John A. Health Trajectories: Long-Term Dynamics among Black and White Adults. Journal of Health and Social Behavior. 1997;38:38–54. [PubMed] [Google Scholar]
- Ferraro Kenneth F., Kelley-Moore Jessica A. Cumulative Disadvantage and Health: Long-Term Consequences of Obesity? American Sociological Review. 2003;68:707–729. [PMC free article] [PubMed] [Google Scholar]
- Ferraro Kenneth F., Su Ya-Ping, Gretebeck Randall J., Black David R., Badylak Stephen F. Body Mass Index and Disability in Adulthood: a 20-Year Panel Study. American Journal of Public Health. 2002;92:834–40. doi: 10.2105/ajph.92.5.834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferraro Kenneth F., Yu Yan. Body Weight and Self-Ratings of Health. Journal of Health and Social Behavior. 1995;36:274–84. [PubMed] [Google Scholar]
- Finkelstein Eric A., Ruhm Christopher J., Kosa Katherine M. Economic Causes and Consequences of Obesity. Annual Review of Public Health. 2005;26:239–57. doi: 10.1146/annurev.publhealth.26.021304.144628. [DOI] [PubMed] [Google Scholar]
- Flegal Katherine M., Carroll Margaret D., Kuczmarski Robert J., Johnson Clifford L. Overweight and Obesity in the United States: Prevalence and Trends, 1960-1994. International Journal of Obesity. 1998;22:39–47. doi: 10.1038/sj.ijo.0800541. [DOI] [PubMed] [Google Scholar]
- Flegal Katherine M., Troiano Richard P., Pamuk Elsie R., Kuczmarski Robert J., Campbell Stephen M. The Influence of Smoking Cessation on the Prevalence of Overweight in the United States. New England Journal of Medicine. 1995;333:1165–70. doi: 10.1056/NEJM199511023331801. [DOI] [PubMed] [Google Scholar]
- Ford Earl S., Moriarty David G., Zack Matthew M., Mokdad Ali H., Chapman Daniel P. Self-Reported Body Mass Index and Health-Related Quality of Life: Findings from the Behavioral Risk Factor Surveillance System. Obesity Research. 2001;9:21–31. doi: 10.1038/oby.2001.4. [DOI] [PubMed] [Google Scholar]
- Freedman David S., Khan Laura K., Serdula Mary K., Galuska Deborah A., Dietz William H. Trends and Correlates of Class 3 Obesity in the United States from 1990 through 2000. JAMA. 2002;288:1758–61. doi: 10.1001/jama.288.14.1758. [DOI] [PubMed] [Google Scholar]
- Goins Turner R., Spencer Melinda S., Krummel Debra A. Effect of Obesity on Health-Related Quality of Life among Appalachian Elderly. Southern Medical Journal. 2003;96:552–7. doi: 10.1097/01.SMJ.0000056663.21073.AF. [DOI] [PubMed] [Google Scholar]
- Goldman Noreen. Social Inequalities in Health: Disentangling the Underlying Mechanisms. Annals of the New York Academy of Sciences. 2001;954:118–139. [PubMed] [Google Scholar]
- Goldman Noreen, Glei Dana A., Chang Ming-Cheng. The Role of Clinical Risk Factors in Understanding Self-Rated Health. Annals of Epidemiology. 2004;14:49–57. doi: 10.1016/s1047-2797(03)00077-2. [DOI] [PubMed] [Google Scholar]
- Gorman Bridget K., Read Jen’nan G. Gender Disparities in Adult Health: An Examination of Three Measures of Morbidity. Journal of Health and Social Behavior. 2006;47:95–110. doi: 10.1177/002214650604700201. [DOI] [PubMed] [Google Scholar]
- Hedley Allison A., Ogden Cynthia L., Johnson Clifford L., Carroll Margaret D., Curtin Lester R., Flegal Katherine M. Prevalence of Overweight and Obesity Among US Children, Adolescents, and Adults, 1999-2002. JAMA. 2004;291:2847–50. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- Heo Moonseong, Allison David B., Faith Myles S., Zhu Shankuan, Fontaine Kevin R. Obesity and Quality of Life: Mediating Effects of Pain and Comorbidities. Obesity Research. 2003a;11:209–16. doi: 10.1038/oby.2003.33. [DOI] [PubMed] [Google Scholar]
- Heo Moonseong, Faith Myles S., Mott John W., Gorman Bernard S., Redded David T., Allison David B. Hierarchical Linear Models for the Development of Growth Curves: An Example with Body Mass Index in Overweight/Obese Adults. Statistics in Medicine. 2003b;22:1911–42. doi: 10.1002/sim.1218. [DOI] [PubMed] [Google Scholar]
- House James S., Lepkowski James M., Kinney Ann M., Mero Richard P., Kessler Ronald C., Herzog A. Regula. The Social Stratification of Aging and Health. Journal of Health and Social Behavior. 1994;35:213–234. [PubMed] [Google Scholar]
- Hu Li-tze, Bentler Peter M. Fit Indices in Covariance Structure Modeling: Sensitivity to Underparameterized Model Misspecification. Psychological Methods. 1998;3:424–453. [Google Scholar]
- Idler Ellen L, Benyamini Yael. Self-Rated Health and Mortality: a Review of Twenty-Seven Community Studies. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- Idler Ellen L, Russell Louise B., Davis Diane. Survival, Functional Limitations, and Self-Rated Health in the NHANES I Epidemiologic Follow-up Study, 1992. First National Health and Nutrition Examination Survey. American Journal of Epidemiology. 2000;152:874–83. doi: 10.1093/aje/152.9.874. [DOI] [PubMed] [Google Scholar]
- Katz David A., McHorney Colleen A., Atkinson Richard L. Impact of Obesity on Health-Related Quality of Life in Patients with Chronic Illness. Journal of General Internal Medicine. 2000;15:789–96. doi: 10.1046/j.1525-1497.2000.90906.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krause Neal M., Jay Gina M. What Do Self-Rated Health Items Measure? Medical Care. 1994;32:930–42. doi: 10.1097/00005650-199409000-00004. [DOI] [PubMed] [Google Scholar]
- Kumanyika Shiriki K. Special Issues Regarding Obesity in Minority Populations. Annals of Internal Medicine. 1993;119:650–4. doi: 10.7326/0003-4819-119-7_part_2-199310011-00005. [DOI] [PubMed] [Google Scholar]
- Little Roderick J.A., Rubin Donald B. Statistical Analysis with Missing Data. John Wiley; New York: 1987. [Google Scholar]
- Lynch Scott M. Cohort and Life-Course Patterns in the Relationship between Education and Health: A Hierarchical Approach. Demography. 2003;40:309–331. doi: 10.1353/dem.2003.0016. [DOI] [PubMed] [Google Scholar]
- McDonough Peggy, Berglund Pat. Histories of Poverty and Self-Rated Health Trajectories. Journal of Health and Social Behavior. 2003;44:198–214. [PubMed] [Google Scholar]
- Meredith William, Tisak John. Latent Curve Analysis. Psychometrika. 1990;55:107–122. [Google Scholar]
- Mokdad Ali H., Ford Earl S., Bowman Barbara A., Dietz William H., Vinicor Frank, Bales Virginia S., Marks James S. Prevalence of Obesity, Diabetes, and Obesity-Related Health Risk Factors, 2001. JAMA. 2003;289:76–9. doi: 10.1001/jama.289.1.76. [DOI] [PubMed] [Google Scholar]
- Muthén Bengt, Muthén Linda K. Mplus User’s Guide. Muthén & Muthén; Los Angeles, CA: 2006. [Google Scholar]
- Muthén Linda K., Muthén Bengt O. How to Use a Monte Carlo Study to Decide on Sample Size and Determine Power. Structural Equation Modeling. 2002;9:599–620. [Google Scholar]
- NHLBI. Obesity Initiative Expert Panel Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults -- The Evidence Report. Obesity Research. 1998;6(suppl.):51s–209s. [PubMed] [Google Scholar]
- O’Rand Angela M. The Precious and the Precocious: Understanding Cumulative Disadvantage and Cumulative Advantage over the Life Course. The Gerontologist. 1996;36:239–239. doi: 10.1093/geront/36.2.230. [DOI] [PubMed] [Google Scholar]
- Ogden Cynthia L., Carroll Margaret D., Curtin Lester R., McDowell Margaret A., Tabak Carolyn J., Flegal Katherine M. Prevalence of Overweight and Obesity in the United States, 1999-2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- Okosun Ike S., Choi Simon, Matamoros Tara, Dever Alan G. Obesity is Associated with Reduced Self-Rated General Health Status: Evidence from a Representative Sample of White, Black, and Hispanic Americans. Preventive Medicine. 2001;32:429–36. doi: 10.1006/pmed.2001.0840. [DOI] [PubMed] [Google Scholar]
- Ramsey Priscilla W., Lee Glenn L. Obesity and Health Status in Rural, Urban, and Suburban Southern Women. Southern Medical Journal. 2002;95:666–671. [PubMed] [Google Scholar]
- Ross Catherine E. Overweight and Depression. Journal of Health and Social Behavior. 1994;35:63–79. [PubMed] [Google Scholar]
- Ross Catherine E., Bird Chloe E. Sex Stratification and Health Lifestyle: Consequences for Men’s and Women’s Perceived Health. Journal of Health and Social Behavior. 1994;35:161–178. [PubMed] [Google Scholar]
- Ross Catherine E., Ling Wu Chia. Education, Age, and the Cumulative Advantage in Health. Journal of Health and Social Behavior. 1996;37:104–120. [PubMed] [Google Scholar]
- Schafer Markus H., Ferraro Kenneth F. Obesity and Hospitalization over the Adult Life Course: Does Duration of Exposure Increase Use? Journal of Health and Social Behavior. 2007;48:434–449. doi: 10.1177/002214650704800407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scharoun-Lee Melissa, Adair Linda S., Kaufman Jay S., Gordon-Larsen Penny. Obesity, Race/Ethnicity and the Multiple Dimensions of Socioeconomic Status During the Transition to Adulthood: A Factor Analysis Approach. Social Science and Medicine. 2009;68:708–716. doi: 10.1016/j.socscimed.2008.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serdula Mary K., Ivery Donna, Coates Ralph J., Freedman David S., Williamson David F., Byers Tim. Do Obese Children Become Obese Adults? A Review of the Literature. Preventive Medicine. 1993;22:167–177. doi: 10.1006/pmed.1993.1014. [DOI] [PubMed] [Google Scholar]
- Sobal Jeffery, Stunkard Albert J. Socioeconomic Status and Obesity: A Review of the Literature. Psychological Bulletin. 1989;105:260–275. doi: 10.1037/0033-2909.105.2.260. [DOI] [PubMed] [Google Scholar]
- Umberson Debra, Williams Kristi, Powers Daniel A., Liu Hui, Needham Belinda. You Make Me Sick: Marital Quality and Health Over the Life Course. Journal of Health and Social Behavior. 2006;47:1–16. doi: 10.1177/002214650604700101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wannamethee S. Goya, Shaper A. Gerald, Walker Mary. Overweight and Obesity and Weight Change in Middle Aged Men: Impact on Cardiovascular Disease and Diabetes. Journal of Epidemiology and Community Health. 2005;59:134–139. doi: 10.1136/jech.2003.015651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willson Andrea E., Shuey Kim M., Elder Glen H. Cumulative Advantage Processes as Mechanisms of Inequality in Life Course Health. American Journal of Sociology. 2007;112:1886–1924. [Google Scholar]
- Wolf Anne M., Colditz Graham A. Current Estimates of the Economic Cost of Obesity in the United States. Obesity Research. 1998;6:173–5. doi: 10.1002/j.1550-8528.1998.tb00322.x. [DOI] [PubMed] [Google Scholar]
- Wothke Werner. Longitudinal and Multi-Group Modeling with Missing Data. In: Little Todd D., Schnabel Kai U., Baumert Jurgen., editors. Modeling Longitudinal and Multiple Group Data: Practical Issues, Applied Approaches and Specific Examples. Lawrence Erlbaum Publishers; Mahwah, NJ: 2000. pp. 219–240. [Google Scholar]