Abstract
Hypoxia contributes to the aggressive and treatment-resistant phenotype of pancreatic ductal adenocarcinoma (PDAC). Oncolytic vaccinia virus has potential as an anti-tumour agent but the ability to lyse hypoxic tumour cells is vital for clinical efficacy. We hypothesised that unique aspects of the poxvirus lifecycle would protect it from attenuation in hypoxic conditions. We characterised and compared the viral protein production, viral replication, cytotoxicity and transgene expression of Lister strain vaccinia virus in a panel of pancreatic cancer cell lines after exposure to normoxic or hypoxic conditions. Viral protein production was not affected by hypoxia, and high viral titres were produced in both normoxic and hypoxic conditions. Interestingly there was a five-fold (P<0.001) and 10-fold (P<0.0001) increase in viral cytotoxicity for CFPac1 and MiaPaca2 cell lines respectively in hypoxic conditions. Cytotoxicity was equivalent in the remaining cell lines. Levels of transgene expression (luciferase reporter gene) from the vaccinia viral vector were comparable regardless of the ambient oxygen concentration. The present study suggests that vaccinia virus is a promising vector for targeting pancreatic cancer and potentially other hypoxic tumour types.
Keywords: human pancreatic cancer, vaccinia virus, hypoxia
Introduction
Solid tumours are characterized by regions of hypoxia that are inherently resistant to both radiotherapy and chemotherapy1. Many studies have shown that a wide variety of tumour types exhibit hypoxia-related resistance mechanisms resulting in a worse prognosis2,3. Pancreatic ductal adenocarcinoma (PDAC) remains a disease with a dismal prognosis. The majority of patients present with metastatic disease and attempts to alter the natural history with conventional chemotherapy have shown limited benefit. Response rates of only 5-20% are seen and median survival for those with advanced disease remains less than 6 months4. PDACs contain significant areas of hypoxia that have been measured intraoperatively in a clinical setting5. In addition, hypoxia is associated with a poor prognosis in PDAC6 and is implicated in the resistance to gemcitabine, the current standard of care7. Therefore, development of novel therapeutics to conquer this obstacle is pivotal to improving the survival of this lethal disease.
Replicating oncolytic viruses have a natural tropism for tumour cells. Further modification of viruses enables selective tumour targeting and offers the possibility of treating cancers that are resistant to conventional therapies. The oncolytic viruses are not subject to the same resistance mechanisms as conventional cytotoxic therapies and are effective even if apoptosis is blocked8. Despite encouraging laboratory data, clinical trials using oncolytic viral therapy for pancreatic cancer have demonstrated safety but limited efficacy. A replication-selective oncolytic adenovirus, Onyx 015 (dl1520), has been administered by intratumoral (IT) injection into patients with locally advanced pancreatic tumors in phase I/II trials. Although treatments were well tolerated, no objective responses were seen in patients after virus alone, and only two of 21 patients showed objective responses when gemcitabine was used in combination9,10.
One major hurdle affecting oncolytic adenovirus potency is the tumour environment which can affect different stages of the viral life cycle. Recent studies show that replication of Adenovirus serotype 5 (Ad5), the most commonly used oncolytic viral vector, is attenuated in hypoxic conditions. Expression of cell surface receptors for adenovirus, Coxsackie/Adenovirus receptor (CAR) and αv integrins, is unaffected by hypoxia as is the mRNA expression of critical viral genes such as E1A and Hexon. However, translation of viral mRNA to protein is reduced, resulting in a 10-100 fold reduction in the yield of infectious virus particles 11,12. In addition, the group B adenoviruses, serotype 3 and 11, are attenuated in hypoxia with both reduced lytic potential and production of virus particles independent of viral receptor status or viral gene expression13. Consequently adenoviruses may not be the ideal vectors for tumours with significant hypoxic fractions such as PDAC.
Vaccinia virus is an alternative oncolytic virus and has some potential advantages over other viral vectors. Vaccinia is a DNA virus with an extensive safety profile in humans as the virus has been used in millions of people for the World Health Organisation smallpox eradication programme14. In comparison to adenoviral vectors the virion particle size and DNA organisation of vaccinia virus allows insertion of multiple transgenes with less deleterious effects on subsequent viral DNA replication, virion packaging and dissemination 15. As an Orthopoxvirus the life cycle of vaccinia virus is entirely located in the cytoplasm of infected host cells, in contrast to other viral vectors which replicate in the nucleus and rely on host transcription factors for DNA replication16. In addition the infectious virion is packaged with pre-transcribed early viral gene mRNA and ATP so consequently viral replication is initiated early after infection and the life cycle of vaccinia is shorter than other oncolytic viruses 17.
We hypothesised that, unlike adenovirus, the unique features of vaccinia virus would mean that its inherent oncolytic potential would not be deleteriously affected under hypoxic conditions. This hypothesis was further supported by two recent reports. First, it was demonstrated that the entry of mature vaccinia virions to host cells is accelerated by brief low-pH via an endosomal pathway18. Second, the tumour microenviroment is known to be hypoxic and genes involved in regulating intracellular pH are upregulated by hypoxia inducible factor (Hif-1α)19. Given that pancreatic cancer has been shown to be one of the most hypoxic tumours5, we therefore investigated the effect of hypoxia on the life cycle of vaccinia virus using pancreatic cancer as a model and characterised vaccinia virus as an alternative vector targeting hypoxic tumour cells.
Materials and Methods
Cells and tissue culture conditions
All cell lines were obtained from Cancer Research UK Central Cell Services and maintained in DMEM containing 0.06μg/l penicillin and 0.1μg/l streptomycin with 10% foetal calf serum (FCS). Cell lines were cultured at 37°C with 5% CO2 unless otherwise specified. Similarly low passage numbers were used for each experiment.
Viral Stocks and Viral Infection
The Lister vaccine strain of vaccinia virus (VVLister) and the recombinant luciferase-expressing vaccinia viruses (VVL15) were constructed and kindly provided by Professor Istvan Fodor (Loma Linda University Campus, CA, USA). VVL15 was constructed by the insertion of the firefly luciferase and the lacZ reporter genes into the thymidine kinase (TK) region of VVLister downstream of the early–late vaccinia p7.5 promoter20. Cells were trypsinised, replated and exposed to either normoxia or hypoxia for 16 hours prior to any viral infection. Infections were performed using a multiplicity of infection (MOI) = 1 plaque forming unit (pfu) per cell unless otherwise specified.
Hypoxia
For this study, hypoxia is defined as 1% oxygen, which is an oxygen concentration of approximately 7mmHg. This was achieved using a hypoxic incubator maintained at 94% nitrogen, 5% CO2 and 1% oxygen (Heto-Holten Cell Chamber 170, Surrey, United Kingdom).
Immunoblotting
Nuclear extracts were isolated using the NE-PER Nuclear and Cytoplasmic Extraction Reagents (Pierce, Rockford, IL, USA) according to the manufacturer’s instructions. Whole cell lysates were prepared by removing adherent cells using a cell scraper, washing cells in 1ml of PBS at 4°C and centrifuging at 2000rpm for 5 mins at 4°C. Following the removal of PBS, cells were resuspended in 50μl of NP40 cell lysis buffer (50mM Tris pH7.4, 150mM NaCl, 10mM Ca2+, protease inhibitor cocktail (Roche Applied Science, Mannheim, Germany) and 1% Nonidet P40 (Sigma Chemicals Co., Poole, UK)) prior to storage at −80°C. Total protein concentration was determined using the BCA protein assay (Pierce, Rockford, IL, USA), and equal amounts of protein were electrophoresed on a denaturing 10% polyacrylamide gel. Proteins were transferred by electroblotting to a PVDF membrane (Immobilon-P, Millipore, Bedford, MA, USA). Non-specific binding was blocked in 5% bovine serum albumin (BSA) in PBS-t (0.1% Tween-20). Antibodies were incubated in 3% BSA in PBS-t. The murine monoclonal Hif-1α antibody (AbCam Plc, Cambridge, UK) was used at a dilution of 1:750. The rabbit polyclonal Vaccinia virus coat protein antibody (MorphoSys UK Ltd, Bath, UK) was used at a dilution of 1:1000. The PCNA antibody (Santa Cruz Biotech Inc, California, USA) was used at a dilution of 1:1000. The β actin antibody was used at a dilution of 1:3000 (AbCam Plc, Cambridge, UK). The appropriate anti-mouse or anti-rabbit secondary antibody (Santa Cruz Biotech Inc, California, USA) was used at a dilution of 1:1000. Chemiluminescent detection was performed using ECL Detection reagent (GE Healthcare, Buckinghamshire, UK) according to the manufacturer’s instructions.
Vaccinia Virus replication Assay
Cells were seeded in triplicate at a density of 2×105 cells. All plates were incubated overnight in normoxia or hypoxia. Plates were infected 16 hours later with VVLister at a MOI= 1 pfu/cell. Cells and supernatant were harvested using a cell scraper. Samples were freeze-thawed three times then centrifuged. The viral titre in each sample was determined by measuring the 50% tissue culture infective dose (TCID50) on indicator CV1 green monkey kidney cells. The cytopathic effect (CPE) on CV1 was determined by light microscopy 10 days after infection. The Reed-Meunch accumulate method was used to calculate the TCID50 value for each sample21. Triplicates were used for each time point and each replicate had CPE assayed twice. Viral burst titres were converted to PFU/cell based on the number of cells present at viral infection.
MTS Assay
Cells were seeded in medium supplemented with 5% FCS in 96- well plates, and maintained under hypoxic or normoxic conditions for 16 h prior to infection. On the day of infection medium containing serial dilutions of vaccinia virus was added to each well. Cell viability was measured at 6 days by the MTS (3-(4,5-dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium) assay to assess vaccinia virus cytotoxicity. The MTS assays were carried out by adding 20 μl of the CellTiter96 Aqueous Nonradioactive cell proliferation assay kit (Promega, Madison, WI, USA) to each well and the plates were incubated at 37°C with 5% CO2 for 2–3 h. Hypoxic plates were always incubated in the hypoxic chamber for the duration of the experiment. Cell viability was determined by measuring the absorbance or optical density (OD) at 490nm using an Opsys MR 96-well plate absorbance reader (Dynex, VA, USA), and a dose-response curve created by non-linear regression using Prism® (GraphPad Software, CA, USA) allowing calculation of the concentration of virus required to kill 50% of cells (EC50) for each cell line and oxygen condition. The cell viability was measured as a percentage of viable cells remaining in the infected wells against viable cells remaining in the non-infected wells. Each assay contained six replicates and each assay was repeated four times.
Reporter gene expression detected by IVIS camera in vitro
Cells were infected with VVL15 for 24, 48 or 72 hours and the luciferase activity measured using an IVIS camera (In Vivo Imaging System; Xenogen Corp., CA, USA). Between 5×104 cells were seeded in 0.5ml of media with 10% FCS in 24-well plates. Cells were incubated in normoxia or hypoxia as indicated for 16 hours. Cells were harvested from control plates and the mean number of cells per well used to calculate the amount of virus required for infection. Cells were infected with a multiplicity of infection (MOI) of 1 PFU/cell of VVL15 in DMEM with 5% FCS. At 24, 48 and 72 hours after infection, luciferase expression was determined as per the manufacturer’s instructions. Media was replaced with 150μg/ml D-Luciferin (Xenogen Corp., CA, USA) in serum-free medium at 37°C and luminescence measured after two minutes. Light emission was quantified as the sum of all detected photon counts within uniform-sized regions of interest (ROI) with each well manually defined during post-data acquisition image analysis. This was measured in photons per second per cm2 (p/s/cm2) using Living Image software (Xenogen Corp., CA, USA). The mean light emission per cell (p/sec/cm2/cell) was calculated using the number of cells infected at time 0 and compared for each MOI at 24,48 and 72 hours.
Statistical Analysis
The unpaired students T-test was used for all statistical analysis unless otherwise specified.
Results
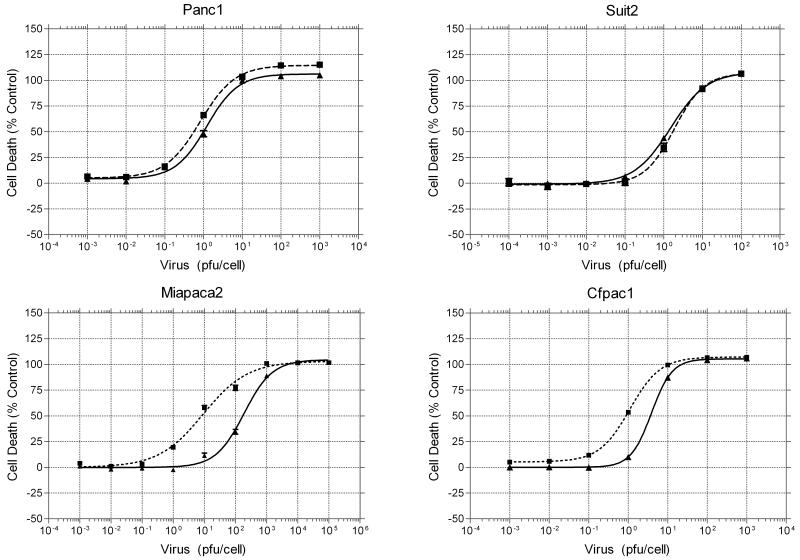
Hypoxia stabilises Hif-1α and induces nuclear translocation
Hif-1α is the key protein mediating the response of cells to a hypoxic microenvironment. In the presence of oxygen Hif-1α is hydroxylated at specific proline residues which results in its interaction with the Von Hippel–Lindau gene product and subsequent ubiquitination and degradation22. In the absence of ambient oxygen this degradation does not occur and subsequent nuclear localisation results in the transcription of Hif-1α target genes and cellular adaptation to hypoxia. Vaccinia Virus is becoming an increasingly common vector for viral gene and oncolytic therapy. However, its ability to replicate in hypoxia has not been reported to date. In the present study hypoxic conditions were simulated with the use of a hypoxic incubator maintaining the ambient oxygen concentration at 1% pO2. Immunoblotting for Hif-1α in nuclear extracts of three pancreatic cancer cell lines, shown in Fig.1, demonstrated that nuclear localisation of this protein was observed only when cells were exposed to 1% pO2 and validates the use of this equipment in subsequent experiments. This suggests the environment used in the present study is suitably hypoxic.
Figure 1.
Stabilisation and nuclear translocation of Hif-1α under hypoxia. Cell lines were incubated in normoxia (20% pO2) (lanes 1, 3, 5) or hypoxia (1% pO2) (lanes 2, 4, 6) for 16 hours before harvesting of nuclear extracts for immunoblotting. Lysates were probed for Hif-1α and proliferating cell nuclear antigen (PCNA) expression.
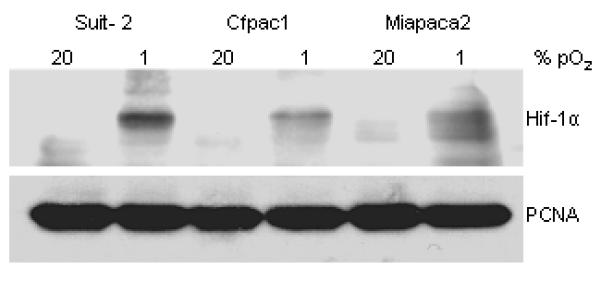
Vaccinia Virus Protein Expression is not affected by hypoxic conditions
Given the fact that viral protein expression is the direct indicator of initiation of the viral life cycle and hypoxia has been shown to limit the total amount of protein synthesis23, we first investigated if production of viral proteins in pancreatic cancer cell lines exposed to hypoxia would be altered. CFPac1 and Miapaca2 cell lines were infected with VVLister at an MOI=1 and cell lysates were harvested at 24h, 48h and 72h post-infection. Similar levels of vaccinia virus protein were present at 72 hours when exposed to normoxia or hypoxia as shown in lanes 6 & 7 of Fig. 2 A. Immunoblotting for stabalisation and nuclear translocation of Hif-1α from MiaPaca2 lysates was performed to confirm that exposure to hypoxia had been adequate during the experiment (Fig. 2 B). This result confirms that critical viral proteins are translated efficiently in hypoxic conditions. This also implies that the steps of the vaccinia virus life cycle before viral gene expression such as attachment and internalisation etc may be not affected by hypoxia.
Figure 2.
Viral gene expression of vaccinia virus in human pancreatic cancer after viral infection, and Hif-1α stabilisation and nuclear translocation in normoxia or hypoxia. A, Hypoxia does not affect viral gene expression of vaccinia virus. Cells were maintained in normoxia or hypoxia prior to and after viral infection. Cells were infected with VVLister at an MOI=1. Vaccinia virus protein was measured using an anti-vaccinia polyclonal antibody. Human PCNA was used as a loading control; B, Hif-1α stabilisation and nuclear translocation was demonstrated on nuclear lysates from MiaPaca2 cells in normoxia (20% pO2) or hypoxia (1% pO2) over a time course. β-actin was used as a loading control.
Vaccinia Virus replication under hypoxic conditions
The ability of replication-competent viruses to infect, multiply, lyse and then subsequently infect neighbouring cells is crucial in order for them to spread throughout a tumour. There has been concern that hypoxia may present a barrier to this24. We investigated the replication of VVLister in pancreatic cancer cell lines Suit-2, MiaPaca2 and CFPac1 when exposed to normoxia or hypoxia prior to and post-viral infection. Cells and supernatant were collected at 24, 48, 72 and 96 hours post-infection. The number of pfu/cell produced for each cell line in different conditions was determined using a TCID50 assay as described in the Materials and Methods section. The levels of viral replication in MiaPaca-2 and CFPac1 cells are unaffected at any point by hypoxic conditions (Fig. 3). Suit2 cells show a similar pattern at 24h and 48h, producing a high titre of infectious viral particles in both hypoxia and normoxia. At later time points, even higher titres are achieved when replication occurs in ambient oxygen concentrations, however, there was no significant difference compared to those in hypoxia. In summary, high viral titres of VVLister (approximately more than 100pfu/cell) were achievable in all pancreatic cancer cell lines tested in both normoxia and hypoxia.
Figure 3.
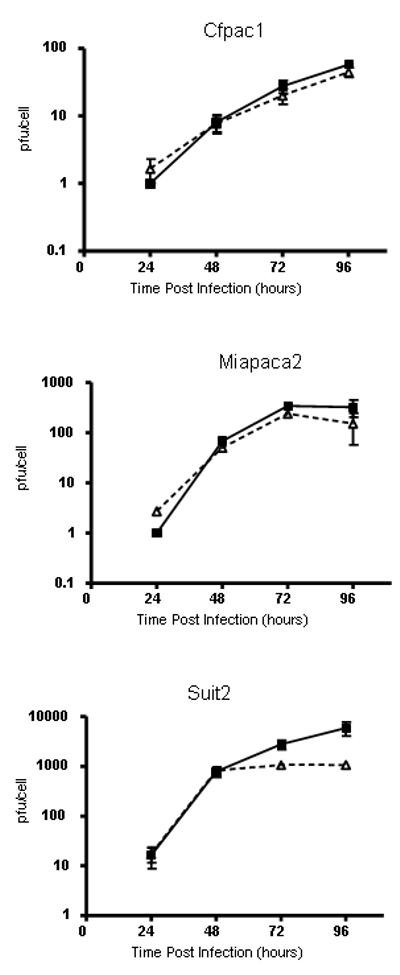
Viral replication of VVLister in normoxia (solid line) and hypoxia (dashed line) measured by TCID50 assay of viral burst assays. Cell lines were exposed to normoxia or hypoxia prior to and post infection with an MOI=1 of VVLister. Burst assay samples were collected at 24, 48, 72 and 96 hours post infection. TCID50 assays were performed on CV1 green monkey kidney cells. Experiments were performed in triplicate for each cell line, time point and condition. Results are presented as mean +/− standard deviation.
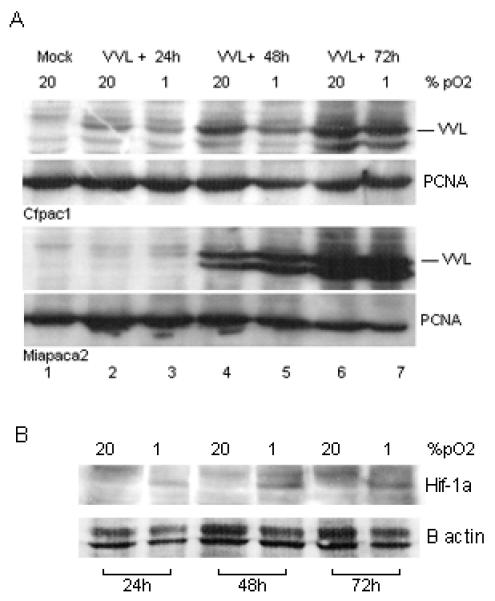
Enhanced Cytotoxicity of Vaccinia Virus in Hypoxia
Effective lysis of infected tumour cells is the ultimate aim of oncolytic therapy. We used the MTS assay to determine the EC50 (dose of virus required to kill 50% of cells) for four pancreatic cancer cell lines. Cells were infected and maintained in the indicated oxygen conditions for the duration of the experiment and cell viability was analysed at 6 days post-infection. Dose response curves and EC50 values were calculated and the results were shown in Fig.4 and Table 1. Cytotoxicity of vaccinia virus in Suit-2 and Panc1 cell lines was maintained irrespective of a reduction in ambient oxygen concentration. Interestingly, for MiaPaca2 and CFPac1 cell lines there were a statistically significant increase in vaccinia virus cytotoxicity in hypoxia with an approximately 10-fold (P < 0.001) and 5-fold (P < 0.01) reduction in EC50 respectively. These data suggest that Lister strain Vaccinia Virus is a potential agent for oncolytic virotherapy where hypoxia occurs in the tumour microenvironment.
Figure 4.
Effect of hypoxia on cytotoxicity of Vaccinia Virus Lister Strain. Pancreatic cancer cell lines were pre-treated with hypoxia or normoxia for at least 16 h, then infected with serial dilutions of VVLister and maintained under the same oxygen tension. The infected cells were assayed with MTS reagents at days 6 post infection in 37°C with 5% CO2 for 2 h. Viable cells were determined as a percentage of the non-infected controls and non linear regression analysis was used to draw dose response curves. Each assay contained six replicates and results are presented as mean +/− standard deviation of four independent experiments.
Table 1.
Comparison of cytotoxicity of vaccinia virus in normoxia and hypoxia
| Cell Lines | EC50 (95% CI) |
P Value | Hill Slope |
||||
|---|---|---|---|---|---|---|---|
| 20% Oxygen | 1% Oxygen | 20% Oxygen |
1% Oxygen |
||||
| Panc1 | 1.21 | (1.03 to 1.41) | 0.82 | (0.71 to 0.95) | = 0.07 | 1.075 | 0.9662 |
| Suit2 | 1.50 | (1.24 to 1.81) | 1.88 | (1.37 to 2.59) | = 0.48 | 0.924 | 1.12 |
| MiaPaca2 | 187.00 |
(154.39 to
226.37) |
9.15 |
(7.24 to
11.58) |
<
0.00004 |
0.9555 | 0.6065 |
| CFPac1 | 3.89 | (3.59 to 4.20) | 1.10 | (1.04 to 1.16) | <0.002 | 1.66 | 1.122 |
The EC50 values of Vaccinia Virus in the four different pancreatic cancer cell lines is presented with 95% confidence intervals and P values represent any significant difference between infection in normoxia versus hypoxia. Hill slope values for the dose response curves are also presented.
Transgene expression in vaccinia virus vector is not affected by hypoxic conditions
Many replicating viruses used for oncolytic therapy have additional therapeutic transgenes inserted into the viral genome to increase their therapeutic effect. Examples include pro-apoptotic proteins, prodrug-converting enzymes and cytokines 25. One of the attractions of vaccinia virus over alternative viral vectors is its large capacity for transgene insertion17. Hypoxia will modulate the gene expression of any host cell so verifying the effect of hypoxia on transgene expression from replication-competent vaccinia virus is important if this vector is to be of clinical use23. We used VVL15 (a recombinant vaccinia virus derived from the Lister vaccine strain) in which the firefly luciferase reporter gene was inserted into the thymidine kinase (TK) region downstream of the early–late vaccinia p7.5 promoter to assess transgene expression. The levels of luciferase activity after infection of four pancreatic cancer cell lines were detected by the Live Imaging System IVS200 (Xenogen, USA) at multiple time points as opposed to isolated readings or early time points as used in other studies to produce more representative data on gene expression26,27. As shown in Fig. 5, luciferase expression was largely unaffected by hypoxia. Only two of the four cell lines tested showed a significant difference between normoxia and hypoxia at two isolated time points. There was a decrease at 24 hours and increase at 48 hours in luciferase expression for CFPac1 and Panc1 respectively. However, this difference was not sustained at later time points. This result suggests that hypoxia does not compromise transgene expression from replication-competent vaccinia virus.
Figure 5.
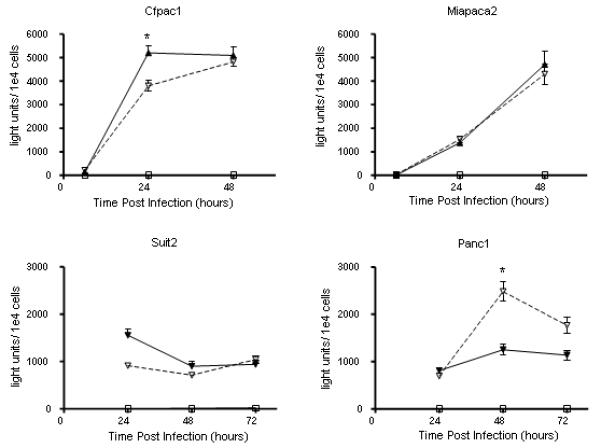
The effect of hypoxia on transgene expression from VVL15. Cells were infected with 1pfu/cell of VVL15 and luciferase activity measured at the time points indicated. All experiments were performed in triplicate and results represent the data from three separate experiments. Results are presented as mean +/− s.d. (Solid line & triangle = 20% pO2, Dashed line & triangle = 1% pO2, Solid line and square & mock infection. Light units = photons/second/cm2. * = P<0.05).
Discussion
Wild-type vaccinia virus has been well characterized and much data on the molecular biology, genome sequence, viral life cycle and immunology have been reported. Vaccinia virus is an appealing candidate agent for oncolytic virotherapy because of these inherent properties. Besides several other attractive qualities (such as fast and efficient replication with rapid cell-to-cell spread; natural tropism for tumours; strong lytic ability; large cloning capacity; well-defined molecular biology; safety in human beings and good stability28-31), a defining feature that we demonstrated from the present study, is that hypoxia does not significantly affect viral gene expression, viral replication, cytotoxicity and even enhances the tumour-killing activity in some tumour cell lines.
We have demonstrated here that Lister strain vaccinia virus shows comparable efficacy in infection, replication and transgene expression regardless of the ambient oxygen concentration. It is important to highlight that hypoxic cells used in these experiments had been exposed to reduced oxygen concentration for at least 16 hours prior to infection which is more likely to reflect cellular adaptation to hypoxia and model clinical vaccinia virus infection than shorter exposure times that have been used for the study of other oncolytic viruses12,26. In addition, we found that effective tumour cell lysis was maintained after infection of hypoxic PDAC cell lines and in half of the cell lines tested there was a statistically significant improvement in viral cytotoxicty. This is an important result given that tumour lysis is the ultimate goal of oncolytic therapy.
Many groups have tried to target hypoxic fractions of tumours using hypoxia-specific promoters often containing hypoxia-response elements (HRE) that facilitate HIF-1α binding and downstream gene transcription. Unfortunately, such promoters are invariably less powerful drivers of gene expression than constitutive viral promoters and result in lower levels of gene expression and viral replication relative to wild-type viruses32,33. Our results show that vaccinia virus has the capacity to infect and replicate in hypoxic tumour cells without the need for such approaches. A recent report from Conner et al. showed that Oncolytic Vesicular Stomatitis Virus (VSV) has comparable viral replication in normoxic HeLa cells versus those exposed to 1% O2 for 2 hours prior to infection and only a slight reduction of viral induced CPE on semi-quantitative analysis26. The availability of other oncolytic viruses that are not significantly attenuated in hypoxia in comparison to adenoviral strains is a welcome finding. However, our results suggest a several-fold, statistically significant improvement in the oncolytic potential of vaccinia virus in some pancreatic cell lines exposed to hypoxic conditions. The underlying mechanisms are not clear, which warrants further investigation. Conner et al conclude that their results suggest an advantage of RNA viruses over DNA viruses in targeting hypoxic tumour cells because of a greater reduction of DNA synthesis in hypoxic cells26. Vaccinia virus is a double-stranded DNA virus and like VSV replicates in the cytoplasm, encodes its own polymerases and is consequently less dependent on host gene and protein expression. Our alternative conclusion is that it is a cytoplasmic life cycle, with a reduced dependence on host gene and protein expression, rather the nucleic acid construction of the viral genome that dictates the efficacy of oncolytic viruses in hypoxia.
In summary we report the comparable efficacy of oncolytic vaccinia virus (including direct cancer cell killing and transgene expression) in both normoxic and hypoxic pancreatic tumour cells. These results suggest that vaccinia virus may be a potent therapeutic vector for targeting pancreatic cancer and potentially other hypoxic tumour types.
Acknowledgement
This project is supported by Cancer Research UK (C633-A6253/A6251), and Barts and The London Research Advisory Board. We are very grateful to Professor Istvan Fodor of Loma Linda University, Loma Linda, CA, USA, for providing the viruses.
Financial disclosures: None of the authors have any financial arrangement nor involvement with commercial organizations producing competing products.
References
- 1.Harris AL. Hypoxia--a key regulatory factor in tumour growth. Nat Rev Cancer. 2002;2:38–47. doi: 10.1038/nrc704. [DOI] [PubMed] [Google Scholar]
- 2.Hiley CT, Green MML, Shanks JH, Bottomley IC, West CML, Cowan RA, et al. Expression of vascular endothelial growth factor (VEGF) in locally invasive prostate cancer is prognostic for radiotherapy outcome. International journal of radiation oncology, biology, physics. 2007;67:84–90. doi: 10.1016/j.ijrobp.2006.08.077. [DOI] [PubMed] [Google Scholar]
- 3.Hutchison GJ, Valentine HR, Loncaster JA, Davidson SE, Hunter RD, Roberts SA, et al. Hypoxia-inducible factor 1alpha expression as an intrinsic marker of hypoxia: correlation with tumor oxygen, pimonidazole measurements, and outcome in locally advanced carcinoma of the cervix. Clinical cancer research : an official journal of the American Association for Cancer Research. 2004;10:8405–8412. doi: 10.1158/1078-0432.CCR-03-0135. [DOI] [PubMed] [Google Scholar]
- 4.Ghaneh P, Costello E, Neoptolemos JP. Biology and management of pancreatic cancer. Postgrad Med J. 2008;84:478–497. doi: 10.1136/gut.2006.103333. [DOI] [PubMed] [Google Scholar]
- 5.Koong AC, Mehta VK, Le QT, Fisher GA, Terris DJ, Brown JM, et al. Pancreatic tumors show high levels of hypoxia. International journal of radiation oncology, biology, physics. 2000;48:919–922. doi: 10.1016/s0360-3016(00)00803-8. [DOI] [PubMed] [Google Scholar]
- 6.Sun HC, Qiu ZJ, Liu J, Sun J, Jiang T, Huang KJ, et al. Expression of hypoxia-inducible factor-1 alpha and associated proteins in pancreatic ductal adenocarcinoma and their impact on prognosis. Int J Oncol. 2007;30:1359–1367. [PubMed] [Google Scholar]
- 7.Yokoi K, Fidler IJ. Hypoxia increases resistance of human pancreatic cancer cells to apoptosis induced by gemcitabine. Clin Cancer Res. 2004;10:2299–2306. doi: 10.1158/1078-0432.ccr-03-0488. [DOI] [PubMed] [Google Scholar]
- 8.Hawkins LK, Lemoine NR, Kirn D. Oncolytic biotherapy: a novel therapeutic platform. Lancet Oncol. 2002;3:17–26. doi: 10.1016/s1470-2045(01)00618-0. [DOI] [PubMed] [Google Scholar]
- 9.Mulvihill S, Warren R, Venook A, Adler A, Randlev B, Heise C, et al. Safety and feasibility of injection with an E1B-55 kDa gene-deleted, replication-selective adenovirus (ONYX-015) into primary carcinomas of the pancreas: a phase I trial. Gene therapy. 2001;8:308–315. doi: 10.1038/sj.gt.3301398. [DOI] [PubMed] [Google Scholar]
- 10.Hecht JR, Bedford R, Abbruzzese JL, Lahoti S, Reid TR, Soetikno RM, et al. A phase I/II trial of intratumoral endoscopic ultrasound injection of ONYX-015 with intravenous gemcitabine in unresectable pancreatic carcinoma. Clinical cancer research : an official journal of the American Association for Cancer Research. 2003;9:555–561. [PubMed] [Google Scholar]
- 11.Pipiya T, Sauthoff H, Huang YQ, Chang B, Cheng J, Heitner S, et al. Hypoxia reduces adenoviral replication in cancer cells by downregulation of viral protein expression. Gene Ther. 2005;12:911–917. doi: 10.1038/sj.gt.3302459. [DOI] [PubMed] [Google Scholar]
- 12.Shen B, Hermiston T. Effect of hypoxia on Ad5 infection, transgene expression and replication. Gene Ther. 2005;12:902–910. doi: 10.1038/sj.gt.3302448. [DOI] [PubMed] [Google Scholar]
- 13.Shen BH, Bauzon M, Hermiston TW. The effect of hypoxia on the uptake, replication and lytic potential of group B adenovirus type 3 (Ad3) and type 11p (Ad11p) Gene therapy. 2006;13:986–990. doi: 10.1038/sj.gt.3302736. [DOI] [PubMed] [Google Scholar]
- 14.Fenner F. Smallpox and Its Eradication (History of International Public Health, No. 6) World Health Organization; Geneva: 1988. [Google Scholar]
- 15.Smith GL, Moss B. Infectious poxvirus vectors have capacity for at least 25 000 base pairs of foreign DNA. Gene. 1983;25:21–28. doi: 10.1016/0378-1119(83)90163-4. [DOI] [PubMed] [Google Scholar]
- 16.Schramm B, Locker J. Cytoplasmic organization of POXvirus DNA replication. Traffic (Copenhagen, Denmark) 2005;6:839–846. doi: 10.1111/j.1600-0854.2005.00324.x. [DOI] [PubMed] [Google Scholar]
- 17.Thorne SH. Oncolytic vaccinia virus: from bedside to benchtop and back. Curr Opin Mol Ther. 2008;10:387–392. [PubMed] [Google Scholar]
- 18.Townsley A, Weisberg A, Wagenaar T, Moss B. Vaccinia Virus Entry into Cells via a Low-pH-Dependent Endosomal Pathway. The Journal of Virology. 2006;80:8899–8908. doi: 10.1128/JVI.01053-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Swietach P, Vaughan-Jones RD, Harris AL. Regulation of tumor pH and the role of carbonic anhydrase 9. Cancer metastasis reviews. 2007;26:299–310. doi: 10.1007/s10555-007-9064-0. [DOI] [PubMed] [Google Scholar]
- 20.Hung CF, Tsai YC, He L, Coukos G, Fodor I, Qin L, et al. Vaccinia virus preferentially infects and controls human and murine ovarian tumors in mice. Gene Ther. 2007;14:20–29. doi: 10.1038/sj.gt.3302840. [DOI] [PubMed] [Google Scholar]
- 21.Reed LJ, Muench H. A simple method of estimating fifty percent endpoints. The American Journal of Hygiene. 1938;27:493–497. [Google Scholar]
- 22.Masson N, Ratcliffe PJ. HIF prolyl and asparaginyl hydroxylases in the biological response to intracellular O(2) levels. J Cell Sci. 2003;116:3041–3049. doi: 10.1242/jcs.00655. [DOI] [PubMed] [Google Scholar]
- 23.Kraggerud SM, Sandvik JA, Pettersen EO. Regulation of protein synthesis in human cells exposed to extreme hypoxia. Anticancer Res. 1995;15:683–686. [PubMed] [Google Scholar]
- 24.Hay JG. The potential impact of hypoxia on the success of oncolytic virotherapy. Curr Opin Mol Ther. 2005;7:353–358. [PubMed] [Google Scholar]
- 25.Bhattacharyya M, Lemoine NR. Gene therapy developments for pancreatic cancer. Best practice & research Clinical gastroenterology. 2006;20:285–298. doi: 10.1016/j.bpg.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 26.Connor JH, Naczki C, Koumenis C, Lyles DS. Replication and cytopathic effect of oncolytic vesicular stomatitis virus in hypoxic tumor cells in vitro and in vivo. J Virol. 2004;78:8960–8970. doi: 10.1128/JVI.78.17.8960-8970.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shen B, Bauzon M, Hermiston T. The effect of hypoxia on the uptake, replication and lytic potential of group B adenovirus type 3 (Ad3) and type 11p (Ad11p) Gene Ther. 2006;13:986–990. doi: 10.1038/sj.gt.3302736. [DOI] [PubMed] [Google Scholar]
- 28.Poland GA, Grabenstein JD, Neff JM. The US smallpox vaccination program: a review of a large modern era smallpox vaccination implementation program. Vaccine. 2005;23:2078–2081. doi: 10.1016/j.vaccine.2005.01.012. [DOI] [PubMed] [Google Scholar]
- 29.Roenigk HH, Jr., Deodhar S, Jacques R, Burdick K. Immunotherapy of malignant melanoma with vaccinia virus. Arch Dermatol. 1974;109:668–673. [PubMed] [Google Scholar]
- 30.Kim JH, Oh JY, Park BH, Lee DE, Kim JS, Park HE, et al. Systemic armed oncolytic and immunologic therapy for cancer with JX-594, a targeted poxvirus expressing GM-CSF. Mol Ther. 2006;14:361–370. doi: 10.1016/j.ymthe.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 31.Park BH, Hwang T, Liu TC, Sze DY, Kim JS, Kwon HC, et al. Use of a targeted oncolytic poxvirus, JX-594, in patients with refractory primary or metastatic liver cancer: a phase I trial. Lancet Oncol. 2008;9:533–542. doi: 10.1016/S1470-2045(08)70107-4. [DOI] [PubMed] [Google Scholar]
- 32.Binley K, Iqball S, Kingsman A, Kingsman S, Naylor S. An adenoviral vector regulated by hypoxia for the treatment of ischaemic disease and cancer. Gene therapy. 1999;6:1721–1727. doi: 10.1038/sj.gt.3301001. [DOI] [PubMed] [Google Scholar]
- 33.Binley K, Askham Z, Martin L, Spearman H, Day D, Kingsman S, et al. Hypoxia-mediated tumour targeting. Gene therapy. 2003;10:540–549. doi: 10.1038/sj.gt.3301944. [DOI] [PubMed] [Google Scholar]