Abstract
OBJECTIVE
National Heart, Lung, and Blood Institute clinical practice guidelines strongly recommend that health professionals educate children with asthma and their caregivers about self-management. We conducted a meta-analysis to estimate the effects of pediatric asthma education on hospitalizations, emergency department visits, and urgent physician visits for asthma.
PATIENTS AND METHODS
Inclusion criteria included enrollment of children aged 2 to 17 years with a clinical diagnosis of asthma who resided in the United States. Pooled standardized mean differences and pooled odds ratios were calculated. Random-effects models were estimated for all outcomes assessed.
RESULTS
Of the 208 studies identified and screened, 37 met the inclusion criteria. Twenty-seven compared educational interventions to usual care, and 10 compared different interventions. Among studies that compared asthma education to usual care, education was associated with statistically significant decreases in mean hospitalizations and mean emergency department visits and a trend toward lower odds of an emergency department visit. Education did not affect the odds of hospitalization or the mean number of urgent physician visits. Findings from studies that compared different types of asthma education interventions suggest that providing more sessions and more opportunities for interactive learning may produce better outcomes.
CONCLUSIONS
Providing pediatric asthma education reduces mean number of hospitalizations and emergency department visits and the odds of an emergency department visit for asthma, but not the odds of hospitalization or mean number of urgent physician visits. Health plans should invest in pediatric asthma education or provide health professionals with incentives to furnish such education. Additional research is needed to determine the most important components of interventions and compare the cost-effectiveness of different interventions.
Keywords: asthma, asthma education, children, patient education, self-management
The national heart, Lung, and Blood Institute (NHLBI) guideline for treatment of asthma strongly recommends that health professionals provide asthma education to children with asthma and their caregivers.1 A wide variety of asthma education programs for children have been implemented and evaluated. However, results have been mixed, and the ability to draw inferences from many of these studies has been limited by small sample sizes.
In this article we present findings from a meta-analysis of the impact of pediatric asthma education on hospitalizations, emergency department (ED) visits, and urgent physician visits for asthma. These outcomes were chosen because asthma is one of the major reasons that children use acute care services. In 2004, children in the United States had ~198 000 hospitalizations for asthma, 754 000 ED visits, and 7 million outpatient visits.2 Although several meta-analyses on pediatric asthma education have been published,3-6 they only incorporated studies that were published before 1999. Many additional studies have been published since then that evaluated novel types of educational programs that were not assessed in earlier literature.
PATIENTS AND METHODS
Data Sources and Study Selection
Inclusion criteria included enrollment of children aged 2 to 17 years who had a clinical diagnosis of asthma. Children were considered to have a clinical diagnosis of asthma if they were diagnosed by a physician or had at least 1 previous urgent physician visit, ED visit, or hospitalization for asthma. Studies in which most enrollees were under the age of 2 were excluded, because it is difficult to diagnose asthma in children in this age group.1 The analysis was limited to studies conducted in the United States and published in English, because utilization of acute care services may vary across countries with different types of health care systems.
Studies with the following research designs were included: randomized, controlled trials (RCTs), cluster RCTs, controlled clinical trials, and observational studies with contemporaneous comparison groups. Four major databases on medical literature were searched: PubMed, the Cochrane Database of Systematic Reviews, the Cochrane Central Register of Controlled Trials, and the Cumulative Index to Nursing and Allied Health Literature. The search terms included “asthma (education or educational),” “asthma (education or educational) intervention*,” “asthma (educational or education) plan,” “asthma (education or educational) program*,” “clinical trial*,” “counsel*,” health education,” “patient education,” “program evaluation,” and “self-care.”
The literature search was performed by a medical librarian at the University of California, San Francisco. Dr Coffman screened titles and abstracts for all articles, retrieved the full text of potentially eligible studies, and read the full text of these studies to confirm that they met the inclusion criteria. As questions arose with regard to inclusion or interpretation of articles, Drs Cabana, Halpin, and Yelin were consulted, and the topic was discussed until consensus was reached. For each eligible study, we extracted information regarding the research design, sample size, characteristics of the educational intervention, and characteristics of the study population. When articles did not report the data needed to calculate pooled estimates, we attempted to obtain this information from the authors.
Analysis
We analyzed the effects of pediatric asthma education on mean number of hospitalizations, ED visits, and urgent physician visits for asthma and on the odds of receiving 1 or more units of each of these services. Asthma education was hypothesized to increase children's and care-givers' ability to manage asthma and, thus, reduce the frequency and severity of asthma symptoms, which in turn was hypothesized to decrease the need for acute care.
If not reported in the articles, SDs of mean differences in utilization were calculated by using methods recommended by the Cochrane Collaboration.7 Mean differences were transformed into standardized mean differences (SMDs) by using the Hedges (adjusted) g method, because studies differed in the time intervals over which mean differences were reported.8 We used DerSimion and Laird's random-effects model to generate all pooled estimates, because we wanted to control for variation in the time intervals over which outcomes were measured, the populations studied, and the educational content of the interventions.9 Q statistics were calculated to determine if the results of the studies pooled were heterogeneous (ie, whether the variance was greater than might occur by chance).7,8,10,11 All analyses were performed in Stata 9.0 (Stata Corp, College Station, TX).
We also developed a rubric to assess the comprehensiveness of asthma education interventions based on the NHLBI guideline for asthma education. This guideline recommends that providers educate patients and their caregivers about 4 major topics: basic facts about the pathophysiology of asthma, correct usage of medications, techniques for monitoring symptoms, and the importance of avoiding triggers.1 Asthma education programs that incorporated all 4 topics were rated as the most comprehensive. Ratings were assigned on the basis of information reported in the articles.
RESULTS
Study Characteristics
A total of 208 abstracts were reviewed, and 37 articles12-48 met the selection criteria. Twenty-seven of the articles were published recently and were not part of previously published meta-analyses. Articles were excluded for the following reasons: not original research (eg, an editorial); not conducted in the United States; adults were enrolled; children who were not diagnosed with asthma were included; intervention was directed toward health professionals rather than children and/or caregivers; lack of data on outcomes of interest; and absence of a comparison group.
Table 1 lists the 37 studies12-48 we reviewed and describes their research designs and sample sizes, as well as the characteristics of the asthma education interventions and populations they assessed. A table that provides additional details about individual studies is available from Dr Coffman on request. Twenty-seven studies compared asthma education interventions to “usual care” for asthma.† Most studies did not define “usual care,” which likely means asthma care that the children routinely received from their usual health care provider. Ten studies compared different types of asthma education interventions.‡
TABLE 1.
Characteristics of Studies of Pediatric Asthma Education Included in Meta-analysis
| Authors | Type of Study | Sample Sizea |
Type of Comparison | Type of Education | No. of Sessions (Contact Time) |
Topics Addressed | Severity | Socioeconomic Status |
|---|---|---|---|---|---|---|---|---|
| Alexander et al12 (1988) | RCT | 21 | Education vs usual care | Individual education | Not stated | Basic facts, medication usage, symptom monitoring, avoiding triggers | Not stated, but all had at least 1 ED visit in the previous 12 mo | 100% enrolled in Medicaid and had no usual source of care |
| Anderson et al13 (2004) | Controlled observational study | 54 | Education vs usual care | Not stated | Not stated | Not stated | Not stated | Family income = $0–36 335, 78% Medicaid, 11% State Children's Health Insurance Program, 11% indigent |
| Bartholomew et al14 (2000) | RCT | 133 | Education vs usual care | Educational computer game | Not stated | Medication usage, symptom monitoring, avoiding triggers | 33% mild, 36% moderate, 31% severe | 48% Medicaid, 31% no insurance, 7% health maintenance organization, 7% Medicare, 7% self-pay |
| Brown et al15 (2002) | RCT | 95 | Education vs usual care | Individual education | 8 sessions (12 h) | Not stated | 19% mild intermittent, 56% mild persistent, 21% moderate persistent, 4% severe persistent | 82% enrolled in Medicaid |
| Butz et al16 (2005) | Cluster RCT | 201 | Education vs usual care | Group education | 3 sessions (5 h) | Basic facts, medication usage, symptom monitoring, avoiding triggers | 39% mild intermittent, 39% mild persistent, 12% moderate persistent, 11% severe persistent | Parent income: 6% less than $10 000, 23% $10 000–29 999, 34% $30 000–39 999, 35% $40 000 + |
| Butz et al17 (2006) | RCT | 181 | 2 different asthma education interventions | Individual education, focused on nebulizer use vs focused on use of asthma action plan | 6 sessions (6 h) vs 3 sessions (3 h) | Medication usage, symptom monitoring | 5% mild intermittent, 61% mild persistent, 21% moderate persistent, 14% severe persistent | 80% enrolled in Medicaid; 100% lived in inner-city areas |
| Chan et al18 (2007) | RCT | 120 | 2 different asthma education interventions | Internet-based education plus individual, in-person education vs individual in-person education | Not stated | Medication usage, symptom monitoring | 18% mild persistent, 68% moderate persistent, 14% severe persistent | Dependents of active-duty or retired military personnel |
| Christiansen et al19 (1997) | Controlled observational study | 52 | Education vs usual care | Group education | 5 sessions (1 h, 40 min) | Basic facts, medication usage, symptom monitoring, avoiding triggers | Not stated | Lived in inner city |
| Clark et al20 (1986) | RCT | 310 | Education vs usual care | Group education | 6 sessions (6 h) | Medication usage, symptom monitoring, avoiding triggers | Not stated, but all had ≥1 visit to allergy clinic in the previous 12 mo | Low income and lived in inner city |
| Evans et al21 (1987) | Cluster RCT | 239 | Education vs usual care | Group education | 6 sessions (6 h) | Basic facts, medication usage, symptom monitoring, avoiding triggers | Not stated | 71% received Medicaid or other public assistance |
| Evans et al22 (1999)b | RCT | 1033 | Education vs usual care | Individual education and group education | 13 sessions (not stated) | Basic facts, medication usage, avoiding triggers | Most mild | Lived in inner-city census tracts in which at least 20% of the population was below 100% of the federal poverty level |
| Farber and Oliveria23 (2004) | RCT | 56 | Education vs usual care | Individual education | 1 session (not stated) | Basic facts, medication usage, symptom monitoring, avoiding triggers | Not stated, but recruited during ED visit | 100% Medicaid; 82% had family income less than $15 000 |
| Fireman et al24 (1981) | Controlled clinical trial | 26 | Education vs usual care | Individual education and group classes | 6 sessions (8 h) | Basic facts, medication usage, symptom monitoring, avoiding triggers | 50% intermittent, 50% persistent | Most had moderate family incomes |
| Gerald et al25 (2006) | Cluster RCT | 736 | Education vs usual care | Group education | 6 sessions (3 h) | Basic facts, medication usage, symptom monitoring, avoiding triggers | Not stated | Lived in an inner-city school district |
| Greineder et al26 (1999) | RCT | 57 | 2 different asthma education interventions | Individual, in-person education vs individual, in-person education plus telephone calls | ≥1 sessions (not stated) | Basic facts, medication usage, symptom monitoring, avoiding triggers | Not stated | 100% commercial health maintenance organization |
| Guendelman et al27 (2002) | RCT | 122 | Education vs usual care | Educational Internet device | ~90 sessions (not stated) | Basic facts, medication usage, symptom monitoring, avoiding triggers | 26% mild, 62% moderate, 11% severe | 93% public insurance |
| Harish et al28 (2001)b | Controlled clinical trial | 129 | Education vs usual care | Individual education | 3 sessions (at least 3 h) | Basic facts, medication usage, symptom monitoring, avoiding triggers | Not stated, but recruited during an ED visit | Lived in low-income, inner-city area |
| Homer et al29 (2000) | RCT | 137 | 2 different asthma education interventions | Educational computer game and individual, in-person education vs individual, in-person education | 3 sessions (not stated) | Basic facts, medication usage, symptom monitoring, avoiding triggers | Mean = moderate | 13% private health insurance |
| Joseph et al30 (2005) | Cluster RCT | 510 | Education vs usual care | Group education | Not stated | Not stated | 48% mild intermittent, 29% mild persistent, 17% moderate persistent, 6% severe persistent | 52% lived in families with incomes of less than $15 000 |
| Karnick et al31 (2007) | RCT | 212 | 3 different asthma education interventions | Individual education: in-person education vs in-person education plus telephone calls vs in-person education, telephone calls, and case management | Not stated | Basic facts, medication usage, avoiding triggers | 80% experienced symptoms ≥2 times per week | 89% Medicaid |
| Kelly et al32 (2000) | Controlled clinical trial | 78 | Education vs usual care | Individual education | 3 sessions (not stated) | Basic facts, medication usage, symptom monitoring, avoiding triggers | Not stated, but had at least 2 ED visits or 1 hospitalization for asthma in the previous 12 mo | 100% Medicaid |
| Krieger et al33 (2005)b | RCT | 214 | Asthma education interventions of differing intensities | Individual education: 7 home visits vs 1 home visit | 7 sessions vs 1 session (not stated) | Avoiding triggers | 24% mild intermittent, 14% mild persistent, 34% moderate persistent, 28% severe persistent | Enrolled in Medicaid and/or lived in households with incomes below 200% of the federal poverty level |
| Krishna et al34 (2003) | RCT | 86 | 2 different asthma education interventions | Educational computer game and individual, in-person education vs individual, in-person education | At least 3 sessions (hours varied) | Basic facts, medication usage, symptom monitoring, avoiding triggers | Not stated, but all were receiving treatment from an allergy and pulmonology clinic | Among children's parents: 9% less than high school education, 54% high school graduates, 37% some college |
| La Roche et al35 (2006) | Controlled observational study | 22 | Education vs usual care | Group education | 3 sessions (3 h) | Basic facts, medication usage, symptom monitoring, avoiding triggers | Not stated | 100% low socioeconomic status |
| Levy et al36 (2006) | Cluster RCT | 243 | Education vs usual care | Group education and individual education | ~32 sessions (not stated) | Basic facts, medication usage, symptom monitoring, avoiding triggers | Not stated | >80% enrolled in Medicaid |
| Lewis et al37 (1984) | RCT | 76 | 2 different asthma education interventions | Group education: interactive, small-group education vs lectures to large groups | 5 sessions (5 h) vs 3 sessions (4.5 h) | Basic facts, medication usage, symptom monitoring, avoiding triggers | Not stated, but used medication at least 25% of days per month | 100% enrolled in Kaiser Permanente |
| Lukacs et al38 (2002) | Controlled observational study | 298 | Education vs usual care | Individual education | Not stated | Not stated | Moderate or severe | 100% enrolled in Kaiser Permanente |
| McNabb et al39 (1985) | RCT | 14 | Education vs usual care | Individual education | 4 sessions (3 h) | Symptom monitoring | Not stated, but at least 1 ED visit in previous year | 100% enrolled in Kaiser Permanente |
| Morgan et al40 (2004)b | RCT | 821 | Education vs usual care | Individual education | Median of 5 sessions (not stated) | Basic facts, avoiding triggers | Not stated, but at least 1 hospitalization or 2 ED or urgent care visits in previous 6 mo and positive test for allergen | Lived in census tracts in which at least 20% of households had incomes below 100% of the federal poverty level |
| Persaud et al41 (1996) | RCT | 36 | Education vs usual care | Individual education | 8 sessions (2 h, 40 min) | Medication usage, symptom monitoring | 44% mild, 50% moderate, 6% severe | 69% Medicaid |
| Rubin et al42 (1986) | RCT | 54 | 2 different asthma education interventions | Educational computer game vs brief, verbal instructions | 6 sessions (4.5 h) | Medication usage, symptom monitoring, avoiding triggers | Moderately severe | Most high socioeconomic status |
| Shames et al43 (2004) | RCT | 119 | Education vs usual care | Individual education and an educational computer game | At least 3 sessions (not stated) | Basic facts, medication usage, symptom monitoring, avoiding triggers | Moderate-to-severe | 72% Medicaid; 69% had family income less than $15 000 |
| Shields et al44 (1990) | RCT | 253 | Education vs usual care | Group education; individual education | 8 sessions (8 h) | Medication usage, symptom monitoring, avoiding triggers | Not stated, but all had at least 1 ED visit or hospitalization for asthma in the previous 4 y | Most low income |
| Sockrider et al45 (2006) | RCT | 218 | Education vs usual care | Individual education | 2 sessions (not stated) | Medication usage, symptom monitoring, avoiding triggers | 46% intermittent, 54% persistent | 85% insured, 15% uninsured |
| Teach et al46 (2006)b | RCT | 437 | Education vs usual care | Individual education | 1 session (1–1.5 h) | Basic facts, medication usage, symptom monitoring, avoiding triggers | 41% mild intermittent, 29% mild persistent, 14% moderate persistent, 16% severe persistent | 68% public insurance, 28% commercial insurance, 4% uninsured |
| Velsor-Friedrich et al47 (2004) | Cluster RCT | 102 | Education vs usual care | Group education | 6 sessions (4.5 h) | Basic facts, medication usage, symptom monitoring, avoiding triggers | Not stated | 100% Temporary Assistance for Needy Families; 100% resided in inner-city neighborhoods |
| Walders et al48 (2006) | RCT | 175 | 2 different asthma education interventions | Individual education: comprehensive education plus a 24-h advice line vs education about metered-dose inhalers | 2 sessions vs 1 session (not stated) | Basic facts, medication usage, symptom monitoring, avoiding triggers | 15% mild intermittent, 40% mild persistent, 33% moderate persistent, 12% severe persistent | Lived in inner-city area |
In all cases, the sample size refers to the number of children for whom data were collected for the outcomes of interest to this meta-analysis. In some cases, these sample sizes are smaller than the total number of children enrolled in the study as a result of attrition or missing data.
In addition to education, included ≥1 environmental control intervention such as providing bedding encasements, air purifiers, low-emission vacuums, and pest-control products and services and referring family members for smoking-cessation counseling.
Over 80% of the studies were RCTs§ or cluster RCTs,16,21,25,30,36,47 and the remainder were controlled clinical trials or observational studies with comparison groups.13,19,24,28,32,35,38 Sample sizes ranged from 14 children39 to 1033 children.22 In 22 studies, asthma education was provided to children with asthma and their parents or other caregivers.∥ Twelve studies evaluated educational interventions that were furnished only to children,¶ and 3 assessed interventions that were delivered solely to caregivers.17,33,40
Several different types of educational interventions were examined, including provision of individualized education to children and/or their caregivers,# group classes,†† and educational computer games.14,29,34,42 Outpatient clinics and physician offices were the most common settings in which asthma education was provided.‡‡ Other settings included schools,§§ homes,15,17,18,27,28,33,40 and EDs.23,45,46 The intervention period ranged from a few weeks to > 12 months. The number of sessions ranged from 123,45,46 to 90.27 Just over half of the studies reported providing comprehensive education that addressed all 4 major topics recommended in the NHLBI guideline.∥∥ Five studies did not describe the educational content of the intervention.13,15,30,33,38
The majority of participants in 70% of the studies received Medicaid, were uninsured, and/or lived in low-income families or low-income neighborhoods.¶¶ Most studies enrolled children with a wide range of ages. Mean age at enrollment ranged from 4 years15 to 12 years.27 Boys outnumbered girls in all studies that reported gender. In two thirds of the studies, two thirds or more of the children enrolled were black or Latino.## We could not ascertain the proportion of interventions that offered Latino children and caregivers instruction in Spanish, because two thirds of the studies did not discuss the language(s) in which education was provided. Only 7 studies reported providing some or all components of the intervention in both Spanish and English.19,20,33,35,43,45,46 Some studies only enrolled children or caregivers who spoke English.14,15,27,37,42,48
Asthma Education Versus Usual Care
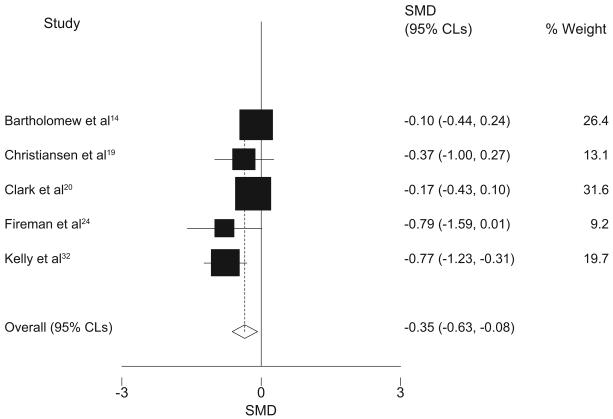
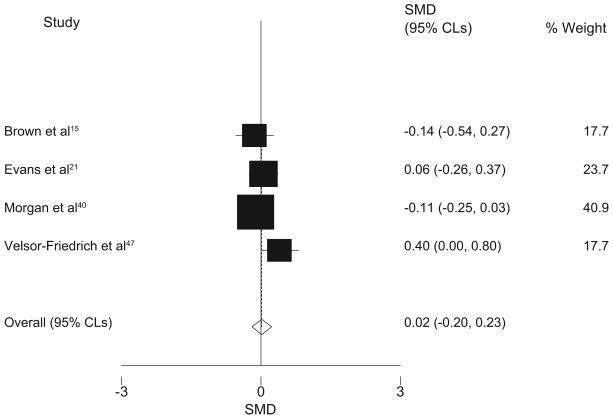
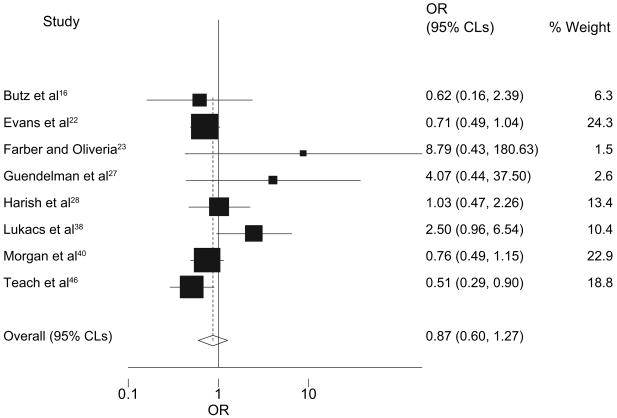
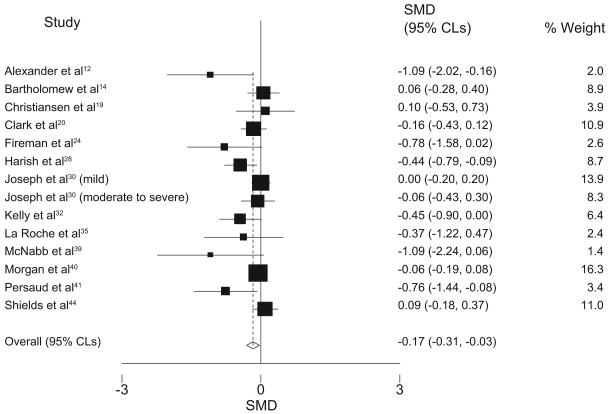
Table 2 and Figs 1-5 display pooled estimates of the effects of pediatric asthma education relative to usual care. The number of studies pooled ranged from 4 to 13. A pooled estimate could not be calculated for odds of an urgent physician visit, because only 1 of the 3 studies that examined this outcome reported sufficient data to generate a pooled estimate. The results of 2 studies that compared asthma education to usual care could not be pooled with other studies, because the authors combined data on use of 2 types of acute care services.36,43 One study could not be pooled because the authors reported median differences instead of mean differences.25 A fourth study13 was excluded because the intervention was much more intensive than those assessed in other studies. In that study, the children in the intervention group were enrolled in a special school for children with chronic illness, at which they received individualized education and case management to ensure compliance with medication regimens.
TABLE 2.
Meta-analysis Results
| Outcome | Total No. of Observations |
Pooled Effect (95% CLs) |
Test of Statistical Significance of Effect |
Test of Heterogeneity |
||
|---|---|---|---|---|---|---|
| z | P | χ2 (df) | P | |||
| Mean No. of hospitalizations | 535 | SMD: −0.35 (−0.63, −0.08) | 2.53 | .01 | 7.68 (4) | .10 |
| Odds of hospitalization | 3087 | OR: 0.87 (0.60, 1.27) | 0.70 | .48 | 13.31 (7) | .07 |
| Mean No. of ED visits | 2269 | SMD: −0.17 (−0.31, −0.03) | 2.40 | .02 | 24.48 (13) | .03 |
| Odds of an ED visit | 2202 | OR: 0.78 (0.61, 1.01) | 1.86 | .06 | 14.59 (10) | .15 |
| Mean No. of urgent physician visits | 1386 | SMD: 0.02 (−0.20, 0.23) | 0.14 | .89 | 6.28 (3) | .10 |
df indicates degrees of freedom.
FIGURE 1.
Mean number of hospitalizations for asthma: asthma education versus usual care.
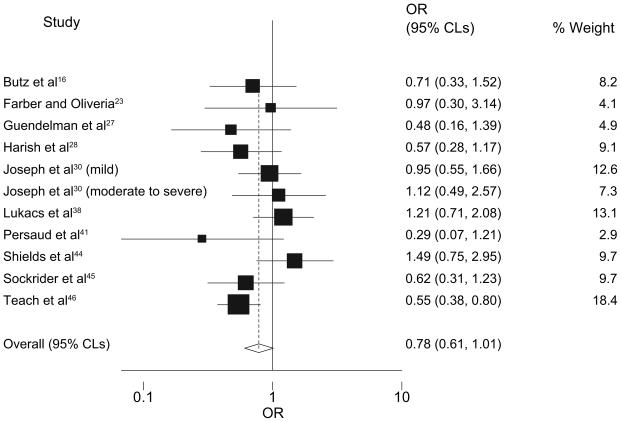
FIGURE 5.
Mean number of urgent physician visits for asthma: asthma education versus usual care.
The pooled estimates indicate that pediatric asthma education reduces both mean number of hospitalizations (n = 5 studies; SMD: −0.35; 95% confidence limits [CLs]: −0.63, −0.08) and mean number of ED visits (n = 13 studies; SMD: −0.17; 95% CLs: −0.31, −0.03) but had a greater affect on mean number of hospitalizations. Pediatric asthma education was also associated with a trend toward lower odds of having an ED visit (n = 10 studies; odds ratio [OR]: 0.78; 95% CLs: 0.61, 1.01). Education had no effect on the odds of hospitalization (n = 8 studies; OR: 0.87; 95% CLs: 0.60, 1.27) or mean number of urgent physician visits (n = 4 studies; SMD: 0.02; 95% CLs: −0.20, 0.23). Findings from the 3 studies that assessed the effect on odds of an urgent physician visit were inconsistent. One study46 found that education reduced the risk of having an urgent physician visit, but the other 2 studies reported no effect.38,45 The relative risks of an ED visit and hospitalization were similar to the ORs for these services (results not shown). For all outcomes except the odds of an ED visit, the P values for the Q statistics were ≤0.1, which indicates that the results of the studies pooled were heterogeneous.
Comparisons of 2 Asthma Education Interventions
Six studies compared the effects of 2 or 3 different asthma education interventions on mean ED visits for asthma. One study found that children whose caregivers participated in 5 interactive, small-group classes had lower mean numbers of ED visits than children whose caregivers attended 3 lectures given to large groups (P < .05).37 Studies of the impact of combining in-person education and telephone calls were equivocal. One study reported that adding follow-up telephone calls and additional in-person educational sessions to a single in-person educational session yielded a greater reduction in mean number of ED visits (P < .05).26 However, another study revealed no statistically significant difference in mean number of ED visits by children who only received 1 in-person education session and those who also received follow-up telephone calls or telephone calls plus case management services.31 One study examined the effects of different interventions on odds of an ED visit and reported that an intervention that consisted of 6 home visits focused on proper use of nebulizers was more effective than a 3-visit intervention that emphasized use of peak flow meters and asthma action plans (P = .05).17
Findings from 2 studies that compared in-person education to in-person education plus an asthma education computer game were inconsistent. One study reported a reduction in mean number of ED visits34; the other study found no statistically significant difference.29 Another study found no statistically significant difference in mean number of ED visits between children who received 6 in-person, individual education sessions in conjunction with clinical care and children who received 3 in-person sessions plus Internet-based education.18
The findings of these studies regarding mean number of hospitalizations and odds of hospitalization were similar to the findings for ED visits.17,18,26,31,34,37 Findings for the mean number of urgent physician visits were also similar.18,29,34 No studies of the odds of urgent physician visits compared 2 different interventions.
Three studies assessed the effects of different asthma education interventions on use of 2 or more types of acute care services. One study reported that children whose caregivers received 7 educational sessions in their homes had fewer urgent physician visits, ED visits, and hospitalizations combined than children whose caregivers received only 1 session (P = .03).33 Another study revealed that supplementing instruction regarding proper use of metered-dose inhalers with education on additional topics and access to a 24-hour advice line was associated with fewer ED visits and hospitalizations combined (P = .05).48 However, a study that compared the effects of an asthma education computer game to brief verbal education reported no statistically significant difference in urgent physician visits and ED visits combined.42
DISCUSSION
The findings from this meta-analysis suggest that, relative to usual care, pediatric asthma education is associated with reductions in mean number of hospitalizations and ED visits and a trend toward decreased odds of an ED visit for asthma but does not affect odds of hospitalization or mean number of urgent physician visits. Findings from studies that compared 2 or more asthma education interventions suggest that interventions that involve more sessions and provide more opportunities for interaction between educators and children or care-givers may be more effective.
Why might asthma education affect the numbers of hospitalizations and ED visits but not the numbers of urgent physician visits? We believe this paradoxical finding may reflect the impact of asthma education on care-seeking behavior. In the studies we reviewed, children and caregivers who received asthma education may have been more aware of the importance of monitoring symptoms closely and may have promptly sought treatment from children's office-based providers if children experienced symptoms. Obtaining office-based urgent care before symptoms became severe may have obviated the need for ED visits and hospitalizations.
Changes in care-seeking behavior may also explain why asthma education had a greater effect on mean number of hospitalizations than on mean number of ED visits. Asthma education may have reduced the severity of exacerbations or prompted parents to bring children to the ED before their symptoms became very severe, which may have reduced the number of children who presented to the ED and required hospitalization. Alternately, some ED visits may have been unavoidable. Some visits may have been made on nights and weekends when children's office-based providers were not available. In other cases, children may not have had a usual source of asthma care and relied on EDs for treatment.
The presence of heterogeneity suggests that pooling results across studies may obscure important, systematic differences among the interventions and populations studied. Several explanations seem plausible. Educational interventions that address all 4 topics recommended in the NHLBI guideline might be more effective, because they are more comprehensive. Interventions composed of more or longer sessions may have greater impact, because educators have more opportunities to reiterate their messages. Individual education might be more effective than group education, because individual sessions can be tailored to the needs of individual children and caregivers. Similarly, educators in clinical settings may have access to medical charts that can enable them to customize content on the basis of a child's medical history, medication regimen, and/or allergy-test results. Differences in results might also reflect variation in rates of hospitalization and ED visits for asthma across regions, health systems, and types of health insurance. Unfortunately, the numbers of studies that evaluated each outcome were too small to permit quantitative analysis of subgroups of studies. We could only make qualitative comparisons. Those comparisons suggested that the interventions with the most favorable results tended to furnish comprehensive education to individual children or families in clinical settings.12,22,24,28,32,41,46
Previous meta-analyses of the effects of pediatric asthma education on ED visits and hospitalizations have reached different conclusions. These meta-analyses found that asthma education was associated with a statistically significant reduction in mean number of ED visits but had no effect on mean number of hospitalizations.3-6 However, our findings are not directly comparable because of differences in inclusion criteria. Whereas our meta-analysis was limited to studies conducted in the United States, the previous meta-analyses also included studies conducted in other developed countries. In addition, previous meta-analyses combined studies that compared asthma education to usual care with studies that compared 2 different asthma education interventions.
STUDY LIMITATIONS
The most important limitation of this study was the lack of specificity regarding the definition of “usual care.” Most studies did not define the term precisely. Their authors assumed that children in the intervention groups received more asthma education than children in the control group.
Inability to discern which children benefit most from asthma education was another important limitation. We could not examine whether findings differed by severity and persistence of asthma symptoms, because the studies did not measure symptoms consistently. The 2 studies that assessed whether effects varied with asthma severity reported conflicting findings. One study found education was associated with a reduction in the odds of having an ED visit for children with intermittent asthma but found no difference for children with persistent asthma45; the other study reported that ED visits were similar for children with mild asthma and moderate/severe asthma.30
The heterogeneity of the results of the studies we assessed also limited the strength of our conclusions. We would have more confidence in our pooled estimates if results had been more consistent across studies. As indicated previously, we could not determine if effectiveness varied systematically with the characteristics of educational interventions or study populations.
The generalizability of our findings may be limited to low-income children in the United States. Three quarters of the studies we reviewed primarily enrolled low-income children. Asthma education may have greater effects on acute care utilization for low-income children than for middle- and upper-income children, because low-income parents may have less formal education and may have less access to information about asthma outside the educational programs. To assess the generalizability of our findings to children in other nations, we obtained studies conducted in other developed countries and generated additional pooled estimates for hospitalizations and ED visits that incorporated these studies. The pooled estimates were similar regardless of whether studies from other developed countries were included. However, the degree of heterogeneity increased dramatically, suggesting that adding these studies increased the variability in the estimates from individual studies above the already high levels observed for US studies. (Results are available from Dr Coffman on request.)
Finally, our findings may overstate the effect of asthma education if there is bias in the publication of studies. We created funnel plots to assess the potential for publication bias (available from Dr Coffman on request). For all outcomes, the funnel plots were asymmetrical, which suggests that small studies of asthma education that yielded nonsignificant or unfavorable results may have been conducted but not published. However, asymmetrical funnel plots do not provide conclusive evidence of publication bias, especially when the number of studies is small.7
CONCLUSIONS
Providing pediatric asthma education reduces the mean number of hospitalizations and both the mean number and odds of ED visits for asthma. These achievements are important, because hospitalizations and ED visits are expensive and can often be prevented if asthma is managed appropriately by a child's caregivers and office-based asthma care providers. Our findings suggest that health plans and medical groups should develop asthma education programs or give clinicians incentives for providing such education.
Additional research is needed to assist clinicians, medical groups, and health plans in determining the amounts and types of asthma education to offer and who should receive it. Previous meta-analyses of the effects of asthma education on other important outcomes, such as self-efficacy, days and nights with symptoms, quality of life, and school absences, should be updated. Researchers can also help identify the most important components of educational interventions (eg, instruction in proper medication usage). Additional study should be undertaken to determine which children with asthma benefit most from asthma education, because it is not clear whether the effectiveness of education varies by age or severity of symptoms. More studies of the cost/benefit of asthma education are needed. Health plans and medical groups are unlikely to invest greater resources in asthma education unless there is compelling evidence that such investments will be cost saving or at least cost neutral. In particular, there is a need for large randomized trials that compare the effects of asthma education interventions of varying intensity and cost. Such studies would provide clinicians and others concerned about pediatric asthma with a stronger evidence base on which they can draw to better integrate asthma education and clinical practice.
FIGURE 2.
Odds of hospitalization for asthma: asthma education versus usual care.
FIGURE 3.
Mean number of ED visits for asthma: asthma education versus usual care.
FIGURE 4.
Odds of ED visits for asthma: asthma education versus usual care.
ACKNOWLEDGMENTS
Funding for this project was provided by the California Health Benefits Review Program and National Institutes of Health grant HL70771.
We acknowledge Min-Lin Fang, MLIS (University of California-San Francisco Library) for completing the literature search for this review. We also thank the members of the California Health Benefits Review Program faculty task force and participants in the University of California-San Francisco Institute for Health Policy Studies Writing Seminar for comments on previous versions of the manuscript.
Abbreviations
- NHLBI
National Heart, Lung, and Blood Institute
- ED
emergency department
- RCT
randomized, controlled trial
- SMD
standardized mean difference
- CLs
confidence limits
- OR
odds ratio
Footnotes
The authors have indicated they have no financial relationships relevant to this article to disclose.
REFERENCES
- 1.National Heart, Lung, and Blood Institute . Guidelines for the Diagnosis and Management of Asthma: Expert Panel Report 2. US Department of Health and Human Services; Washington, DC: 1997. [Google Scholar]
- 2.Akinbami L. Asthma prevalence, health care use and mortality, 2003–05. Available at: www.cdc.gov/nchs/products/pubs/pubd/hestats/asthma03-05/asthma03-05.htm. Accessed December 20, 2006.
- 3.Bernard-Bonnin AC, Stachenk S, Bonin D, Charette C, Rousseau E. Self-management teaching programs and morbidity of pediatric asthma: a meta analysis. J Allergy Clin Immunol. 1995;95(1 pt 1):34–41. doi: 10.1016/s0091-6749(95)70150-8. [DOI] [PubMed] [Google Scholar]
- 4.Guevara JP, Wolf FM, Grum CM, Clark NM. Effects of educational interventions for self management of asthma in children and adolescents: systematic review and meta-analysis. BMJ. 2003;326(7402):1308–1313. doi: 10.1136/bmj.326.7402.1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haby MM, Waters E, Robertson CF, Gibson PG, Ducharme FM. Interventions for educating children who have attended the emergency room for asthma. Cochrane Database Syst Rev. 2001;(1):CD001290. doi: 10.1002/14651858.CD001290. [DOI] [PubMed] [Google Scholar]
- 6.Wolf FM, Guevara JP, Grum CM, Clark NM, Cates CJ. Educational interventions for asthma in children. Cochrane Database Syst Rev. 2002;(1):CD000326. doi: 10.1002/14651858.CD000326. [DOI] [PubMed] [Google Scholar]
- 7.Higgins JPT, Green S, editors. Cochrane handbook for systematic reviews of interventions 4.2.5. Available at: www.cochrane.org/resources/handbook/hbook.htm. Accessed December 20, 2006.
- 8.Deeks JJ, Altman DG, Bradburn MJ. Statistical methods for examining heterogeneity and combining results from several studies in meta-analysis. In: Egger M, Davey-Smith GD, Altman DG, editors. Systematic Reviews in Health Care: Meta-analysis in Context. 2nd ed. BMJ Publishing Group; London, United Kingdom: 2001. pp. 285–312. [Google Scholar]
- 9.Guevara JP, Berlin JA, Wolf FM. Meta-analytic methods for pooling rates when follow-up duration varies: a case study. BMC Med Res Methodol. 2004;4:17–23. doi: 10.1186/1471-2288-4-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sutton AJ, Abrams KR, Jones DR, Sheldon TA, Song F. Methods for Meta-analysis in Medical Research. John Wiley & Sons, LTD; Chichester, United Kingdom: 2000. [Google Scholar]
- 11.Huedo-Medina TB, Sánchez-Meca, Marín-Martínez F, Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods. 2006;11(2):193–206. doi: 10.1037/1082-989X.11.2.193. [DOI] [PubMed] [Google Scholar]
- 12.Alexander JS, Younger RE, Cohen RM, Crawford LV. Effectiveness of a nurse-managed program for children with chronic asthma. J Pediatr Nurs. 1988;3(5):312–317. [PubMed] [Google Scholar]
- 13.Anderson ME, Freas MR, Wallace AS, Kempe A, Gelfand EW, Liu AH. Successful school-based intervention for inner-city children with persistent asthma. J Asthma. 2004;41(4):445–453. doi: 10.1081/jas-120033987. [DOI] [PubMed] [Google Scholar]
- 14.Bartholomew LK, Gold RS, Parcel GS, et al. Watch, Discover, Think, and Act: evaluation of computer-assisted instruction to improve asthma self-management in inner-city children. Patient Educ Couns. 2000;39(2–3):269–280. doi: 10.1016/s0738-3991(99)00046-4. [DOI] [PubMed] [Google Scholar]
- 15.Brown JV, Bakeman R, Celano MP, Demi AS, Kobrynski L, Wilson SR. Home-based asthma education of young low-income children and their families. J Pediatr Psychol. 2002;27(8):677–688. doi: 10.1093/jpepsy/27.8.677. [DOI] [PubMed] [Google Scholar]
- 16.Butz AM, Pham L, Lewis L, et al. Rural children with asthma: impact of a parent and child asthma education program. J Asthma. 2005;42(10):813–821. doi: 10.1080/02770900500369850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Butz AM, Tsoukleris MG, Donithan M, et al. Effectiveness of nebulizer use-targeted asthma education on underserved children with asthma. Arch Pediatr Adolesc Med. 2006;160(6):622–628. doi: 10.1001/archpedi.160.6.622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chan DS, Callahan CW, Hatch-Pigott VB, et al. Internet-based home monitoring and education of children with asthma is comparable to ideal office-based care: results of a 1-year asthma in-home monitoring trial. Pediatrics. 2007;119(3):569–578. doi: 10.1542/peds.2006-1884. [DOI] [PubMed] [Google Scholar]
- 19.Christiansen SC, Martin SB, Schleicher NC, Koziol JA, Mathews KP, Zuraw BL. Evaluation of a school-based asthma education program for inner-city children. J Allergy Clin Immunol. 1997;100(5):613–617. doi: 10.1016/s0091-6749(97)70164-7. [DOI] [PubMed] [Google Scholar]
- 20.Clark NM, Feldman CH, Evans D, Levison MJ, Wasilewski Y, Mellins RB. The impact of health education on frequency and cost of health care use by low income children with asthma. J Allergy Clin Immunol. 1986;78(1 pt 1):108–115. doi: 10.1016/0091-6749(86)90122-3. [DOI] [PubMed] [Google Scholar]
- 21.Evans D, Clark N, Feldman C, et al. A school health education program for children with asthma aged 8–11 years. Health Educ Q. 1987;14(3):267–279. doi: 10.1177/109019818701400302. [DOI] [PubMed] [Google Scholar]
- 22.Evans R, 3rd, Gergen PJ, Mitchell H, et al. A randomized clinical trial to reduce asthma morbidity among inner-city children: results of the National Cooperative Inner-City Asthma Study. J Pediatr. 1999;135(3):332–338. doi: 10.1016/s0022-3476(99)70130-7. [DOI] [PubMed] [Google Scholar]
- 23.Farber HJ, Oliveria L. Trial of an asthma education program in an inner-city pediatric emergency department. Pediatr Asthma Allergy Immunol. 2004;17(2):107–115. [Google Scholar]
- 24.Fireman P, Friday GA, Gira C, Vierthaler WA, Michaels L. Teaching self-management skills to asthmatic children and their parents in an ambulatory care setting. Pediatrics. 1981;68(3):341–348. [PubMed] [Google Scholar]
- 25.Gerald LB, Redden D, Wittich AR, et al. Outcomes for a comprehensive school-based asthma management program. J Sch Health. 2006;76(6):291–296. doi: 10.1111/j.1746-1561.2006.00114.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Greineder DK, Loane KC, Parks P. A randomized controlled trial of a pediatric asthma outreach program. J Allergy Clin Immunol. 1999;103(3 pt 1):436–440. doi: 10.1016/s0091-6749(99)70468-9. [DOI] [PubMed] [Google Scholar]
- 27.Guendelman S, Meade K, Benson M, Chen YQ, Samuels S. Improving asthma outcomes and self-management behaviors of inner-city children: a randomized trial of the Health Buddy interactive device and an asthma diary. Arch Pediatr Adolesc Med. 2002;156(2):114–120. doi: 10.1001/archpedi.156.2.114. [DOI] [PubMed] [Google Scholar]
- 28.Harish Z, Bregante AC, Morgan C, et al. A comprehensive inner-city asthma program reduces hospital and emergency room utilization. Ann Allergy Asthma Immunol. 2001;86(2):185–189. doi: 10.1016/S1081-1206(10)62689-0. [DOI] [PubMed] [Google Scholar]
- 29.Homer C, Susskind O, Alpert HR, et al. An evaluation of an innovative multimedia educational software program for asthma management: report of a randomized, controlled trial. Pediatrics. 2000;106(1 pt 2):210–215. [PubMed] [Google Scholar]
- 30.Joseph CL, Havstad S, Anderson EW, Brown R, Johnson CC, Clark NM. Effect of asthma intervention on children with undiagnosed asthma. J Pediatr. 2005;146(1):96–104. doi: 10.1016/j.jpeds.2004.09.001. [DOI] [PubMed] [Google Scholar]
- 31.Karnick P, Margellos-Anast H, Seals G, Whitmann S, Aljadeff G, Johnson D. The Pediatric Asthma Intervention: a comprehensive cost-effective approach to asthma management in a disadvantaged inner-city community. J Asthma. 2007;44(1):39–44. doi: 10.1080/02770900601125391. [DOI] [PubMed] [Google Scholar]
- 32.Kelly CS, Morrow AL, Shults J, Nakas N, Strope GL, Adelman RD. Outcomes evaluation of a comprehensive intervention program for asthmatic children enrolled in Medicaid. Pediatrics. 2000;105(5):1029–1035. doi: 10.1542/peds.105.5.1029. [DOI] [PubMed] [Google Scholar]
- 33.Krieger JW, Takaro TK, Song L, Weaver M. The Seattle-King County Healthy Homes Project: a randomized controlled trial of a community health worker intervention to decrease exposure to indoor asthma triggers. Am J Public Health. 2005;95(4):652–659. doi: 10.2105/AJPH.2004.042994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Krishna S, Francisco BD, Balas EA, König P, Graff GR, Madsen RW. Internet-enabled interactive multimedia asthma education program: a randomized trial. Pediatrics. 2003;111(3):503–510. doi: 10.1542/peds.111.3.503. [DOI] [PubMed] [Google Scholar]
- 35.La Roche MJ, Koinis-Mitchell D, Gualdron L. A culturally competent asthma management intervention: a randomized controlled pilot study. Ann Allergy Asthma Immunol. 2006;96(1):80–85. doi: 10.1016/S1081-1206(10)61044-7. [DOI] [PubMed] [Google Scholar]
- 36.Levy M, Heffner B, Stewart T, Beeman G. The efficacy of asthma case management in an urban school district in reducing school absences and hospitalizations for asthma. J Sch Health. 2006;76(6):320–324. doi: 10.1111/j.1746-1561.2006.00120.x. [DOI] [PubMed] [Google Scholar]
- 37.Lewis CE, Rachelefsky G, Lewis MA, de la Sota A, Kaplan M. A randomized trial of A.C.T. (Asthma Care Training) for kids. Pediatrics. 1984;74(4):478–486. [PubMed] [Google Scholar]
- 38.Lukacs SL, France EK, Baron AE, Crane LA. Effectiveness of an asthma management program for pediatric members of a large health maintenance organization. Arch Pediatr Adolesc Med. 2002;156(9):872–876. doi: 10.1001/archpedi.156.9.872. [DOI] [PubMed] [Google Scholar]
- 39.McNabb WL, Wilson-Pessano SR, Hughes GW, Scamagas P. Self-management education of children with asthma: Air Wise. Am J Public Health. 1985;75(10):1219–1220. doi: 10.2105/ajph.75.10.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Morgan WJ, Crain EF, Gruchalla RS, et al. Results of a home-based environmental intervention among urban children with asthma. N Engl J Med. 2004;351(11):1068–1080. doi: 10.1056/NEJMoa032097. [DOI] [PubMed] [Google Scholar]
- 41.Persaud DI, Barnett SE, Weller SC, Baldwin CD, Niebuhr V, McCormick DP. An asthma self-management program for children, including instruction in peak flow monitoring by school nurses. J Asthma. 1996;33(1):37–43. doi: 10.3109/02770909609077761. [DOI] [PubMed] [Google Scholar]
- 42.Rubin DH, Leventhal JM, Sadock RT, et al. Educational intervention by computer in childhood asthma: a randomized controlled trial testing the use of a new teaching intervention in childhood asthma. Pediatrics. 1986;77(1):1–10. [PubMed] [Google Scholar]
- 43.Shames RS, Sharek P, Mayer M, et al. Effectiveness of a multicomponent self-management program in at-risk, school-aged children with asthma. Ann Allergy Asthma Immunol. 2004;92(6):611–618. doi: 10.1016/S1081-1206(10)61426-3. [DOI] [PubMed] [Google Scholar]
- 44.Shields MC, Griffin KW, McNabb WL. The effect of a patient education program on emergency room use for inner-city children with asthma. Am J Public Health. 1990;80(1):36–38. doi: 10.2105/ajph.80.1.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sockrider MM, Abramson S, Brooks E, Caviness AC, Pilney S, Koerner C, Macias CG. Delivering tailored asthma family education in a pediatric emergency department setting: a pilot study. Pediatrics. 2006;117(4 pt 2):S135–S144. doi: 10.1542/peds.2005-2000K. [DOI] [PubMed] [Google Scholar]
- 46.Teach SJ, Crain EF, Quint DM, Hylan ML, Joseph JG. Improved asthma outcomes in a high-morbidity pediatric population. Arch Pediatr Adolesc Med. 2006;160(5):535–541. doi: 10.1001/archpedi.160.5.535. [DOI] [PubMed] [Google Scholar]
- 47.Velsor-Friedrich B, Pigott TD, Louloudes A. The effects of a school-based intervention on the self-care and health of African-American inner-city children with asthma. J Pediatr Nurs. 2004;19(4):247–256. doi: 10.1016/j.pedn.2004.05.007. [DOI] [PubMed] [Google Scholar]
- 48.Walders N, Kercsmar C, Schluchter M, Redline S, Kirchner HL, Drotar D. An interdisciplinary intervention for undertreated pediatric asthma. Chest. 2006;129(2):292–299. doi: 10.1378/chest.129.2.292. [DOI] [PubMed] [Google Scholar]