Abstract
Objective
To estimate the national prevalence of arthritis-attributable work limitation (AAWL) among persons ages 18–64 with doctor-diagnosed arthritis and examine correlates of AAWL.
Methods
Using the 2002 National Health Interview Survey, we estimated the prevalence of AAWL (limited in whether individuals work, the type of work they do, or the amount of work they do) and correlates of AAWL in univariable and multivariable-adjusted logistic regression analyses. Survey data were analyzed in SAS and SUDAAN to account for the complex sample design.
Results
A total of 5.3% of all US adults ages 18–64 reported AAWL; in this age group, AAWL is reported by ~30% of those who report arthritis. The prevalence of AAWL was highest among people ages 45–64 years (10.2%), women (6.3%), non-Hispanic blacks (7.7%), people with less than a high school education (8.6%), and those with an annual household income <$20,000 (12.6%). AAWL was substantially increased among people with arthritis-attributable activity limitations (multivariable-adjusted odds ratio [OR] 9.1, 95% confidence interval [95% CI] 7.1–11.6). The multivariable-adjusted likelihood of AAWL was moderately higher among non-Hispanic blacks (OR 1.6, 95% CI 1.2–2.3), Hispanics (OR 1.8, 95% CI 1.2–2.6), and people with high levels of functional/social/leisure limitations (OR 1.8, 95% CI 1.4–2.3) and was decreased among those with a college education (OR 0.6, 95% CI 0.4–0.8).
Conclusion
AAWL is highly prevalent, affecting millions of Americans and one-third of adults with doctor-diagnosed arthritis. Findings suggest the need for more targeted research to better understand the natural history, success of interventions, and effects of policy on AAWL. Public health interventions, including self-management education programs, may be effective in countering AAWL.
Keywords: Epidemiology, Disability, Work
INTRODUCTION
As the leading cause of disability among US adults (1), affecting ~43 million people, arthritis can have serious impact on the physical, social, and functional aspects of one’s life (2). Arthritis-attributable work limitation (AAWL) is an important component of the larger picture of arthritis disability, reflecting social and economic impacts such as absenteeism, reduced productivity, work loss, and lower income (3,4). Because effective, but underused, interventions exist for arthritis management, characterizing AAWL in the working-age population offers great potential for developing targeted interventions that can benefit affected individuals and society as a whole.
Some studies have examined work limitation among people with specific rheumatic conditions. For example, work limitation/disability among individuals with rheumatoid arthritis (RA) has been estimated between 51–60% (5) and as high as 90% in one longitudinal study (6). Rates of work withdrawal among those with ankylosing spondylitis have been estimated to be 3.1 times higher than in the general population (7). However, although condition-specific estimates are useful, a more complete picture of work limitation across the entire spectrum of arthritis in the general population is necessary for an appropriate and more complete public health perspective. This perspective is reflected in Healthy People 2010 objective 2-5b, which aims to “reduce the proportion of people with doctor-diagnosed arthritis who are limited in their ability to work for pay due to arthritis” (8).
To address this objective, the 2002 National Health Interview Survey (NHIS) introduced a question attributing work limitation specifically to arthritis or joint symptoms among people self reporting doctor-diagnosed arthritis (hereafter called arthritis). Preliminary analyses of these data found differences in the prevalence and impact of arthritis by racial/ethnic groups, including AAWL (2). The purpose of the present study was to further elaborate on these initial findings by estimating the US prevalence and examining correlates of AAWL among adults ages 18–64 with arthritis.
PATIENTS AND METHODS
Data source
Data were obtained from the 2002 NHIS, an ongoing, multistage probability survey conducted annually by personal standardized interview in English or Spanish and administered to a nationally representative sample of the US civilian, noninstitutionalized population (9). The 2002 NHIS Sample Adult Core questionnaire (10), from which our sample was drawn, was administered to 31,044 individuals ages ≥18 years; the survey response rate for this component was 74.3% (10).
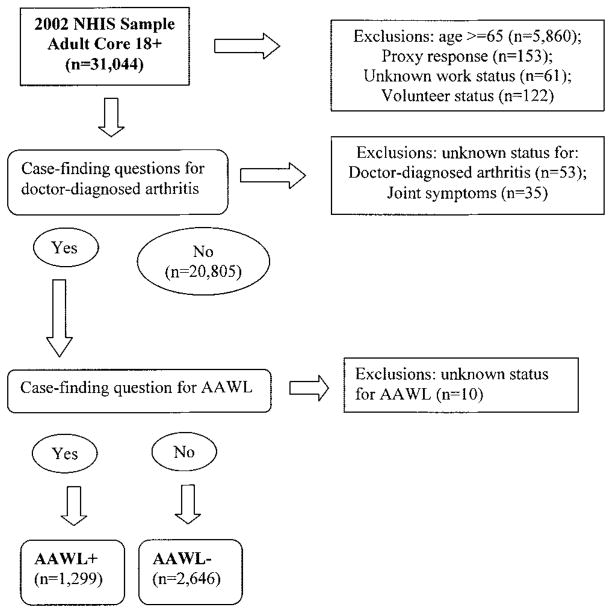
To be included in the analysis, respondents had to be between the ages of 18 and 64 years, the traditional working lifespan. Individuals were excluded if their responses were given by proxy or if status was unknown or missing for the following variables: arthritis status, joint symptoms, work status, or AAWL. Respondents were also excluded if they reported their work status as working, but not for pay, at a job or business; these individuals were considered to be volunteers and, therefore, not appropriate for the AAWL question, which sought information on work for pay (Figure 1).
Figure 1.
Selection of study population for Table 2 (complete case analysis unweighted n = 3,586). NHIS = National Health Interview Survey; AAWL = arthritis-attributable work limitation.
Variables examined in the analysis are described below. Potential factors associated with AAWL were identified by reviewing the arthritis work limitation literature to determine factors that have been observed, or conceptualized, to be associated with AAWL.
Definition of variables
Arthritis and arthritis-attributable work limitation
The preamble to the NHIS arthritis questions section states: “The next questions refer to your joints. Please do NOT include the back or neck.” Respondents were considered to have arthritis if they answered yes to the question: “Have you EVER been told by a doctor or other health professional that you have some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia?” This question was developed through consultation with arthritis epidemiology experts and cognitive testing by the Centers for Disease Control and Prevention to measure the burden of arthritis and related conditions in population-based surveys. Currently, the question is used in the NHIS and Behavioral Risk Factor Surveillance System and for the Healthy People 2010 arthritis objectives (11,12). Among those with arthritis, respondents were considered to have AAWL if they answered yes to the following question: “In this next question we are referring to work for pay. Do arthritis or joint symptoms now affect whether you work, the type of work you do, or the amount of work you do?”
Demographics
Demographic variables examined included age (18–24, 25–44, and 45–64 years), sex, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, and non-Hispanic other/multiple race), annual household income (<$20,000, ≥$20,000, and unknown), body mass index (BMI; calculated from self-reported weight and height [weight in kg/height in m2], categorized as underweight [<18.5], normal [18.5–24.9], overweight [25.0–29.9], and obese [≥30]), and education (high school or less, high school graduate, some college, and at least college [college graduate or higher]).
Physical activity
To determine levels of self-reported leisure-time physical activity, respondents were asked to describe how often they participate in vigorous activities for at least 10 minutes and light or moderate activities for at least 10 minutes. Responses were classified into 3 standard categories: inactive (no leisure-time activity), insufficient (some activity but not meeting recommendations), and recommended (≥3 days of vigorous activity for ≥20 minutes per session or ≥5 days of moderate activity for≥30 minutes per session) levels of activity per federal guidelines for the general population (13,14).
Comorbid conditions
Respondents were queried regarding the presence of 26 discrete chronic co-conditions (angina, asthma, cancer, cataracts, chronic bronchitis, congestive heart failure, diabetes, diabetic retinopathy, emphysema, glaucoma, hearing difficulties, heart attack, heart disease [not otherwise listed], high cholesterol, hypertension, hyper- and hypothyroidism, irritable bowel syndrome, kidney problems [not including kidney stones], macular degeneration, multiple sclerosis, neuropathy, Parkinson’s disease, stroke, ulcers, and vision problems), which were coded dichotomously and summed to create a continuous summary variable representing none to ≥6 conditions. Back pain or neck pain (within the past 3 months) and both recurring pain (in the past 12 months) and anxiety/depression (self-reported frequent anxiety/depression in the past 12 months) were examined as independent comorbidities and were not included in the summary variable.
Nonwork limitations
Nonwork limitations were assessed in 3 separate domains: arthritis-attributable activity limitation, specific functional limitations, and social/leisure limitation. People were categorized as having arthritis-attributable activity limitation if they had arthritis and indicated that arthritis or joint symptoms caused any limitation in any usual activities. The 9 specific functional activities assessed were grasp or handle small objects, lift or carry something as heavy as 10 pounds, push or pull large objects, walk one-quarter of a mile, walk up 10 steps, stand for 2 hours, sit for 2 hours, stoop/bend/kneel, or reach over one’s head. Individuals reporting any task as “very difficult” or “can’t do” were classified as having a functional limitation. Similarly, social/leisure limitation was determined by any “very difficult” or “can’t do at all” response to questions regarding 1) going out to events, movies, or shopping; 2) visiting friends, attending meetings, parties, going to clubs; and 3) relaxing at home or for leisure. A composite variable, functional/social/leisure limitation, was created to represent limitation in any of the functional or social/leisure activities. These functional/social/leisure limitations were not specifically attributable to arthritis.
Arthritis-related variables
Respondents with arthritis who reported joint symptoms in the past 30 days were asked to rate the average severity of their joint pain during that time on a scale from 0 to 10, where 0 is no pain or aching and 10 is pain or aching as bad as it can be, and to identify which joints were affected. Severe pain was defined as a pain level ≥7. Affected joints were collapsed into 5 categories: none, lower extremity, upper extremity, unspecified, or more than 1 site. People reporting no joint symptoms were assigned to the “none” category for each of these 2 variables.
Work status and disability payments
Information on work status and disability payments, available in the NHIS Person File, was linked to the records in the Sample Adult Core. Work status was determined by asking respondents whether, in the past week, they had 1) worked for pay at a job or business, 2) been employed with a job or business but not at work (e.g., on scheduled leave), 3) worked but not for pay at a job or business (e.g., volunteered), 4) looked for work, or 5) did not work and did not look for work. Based on exploratory analysis, work status was categorized as either working (response categories 1 or 2) or not working (response categories 4 or 5); category 3 (volunteers) was excluded. Respondents were considered to have received disability payments if they answered yes to receiving social security, railroad retirement, or Supplemental Security Income as a disability benefit or to receiving any other disability pension in the past year.
Health care access and utilization
Variables representing health care access were constructed from questions linked from the NHIS Person File. Individuals responding no to a dichotomous question on the presence or absence of health insurance were classified as not covered, including those with only Indian Health Service (as classified in Health, United States) (10,15). Individuals responding yes were categorized as having public, private, or a combination of any public and any private insurance. Number of office visits, a measure of health service utilization, was determined from responses to a question regarding the number of visits with health care professionals concerning one’s own health in the past year (excluding hospitalizations, emergency room or home visits, and telephone calls). Responses were collapsed into 2 categories: 0–7 visits and ≥8 visits.
Statistical analysis
The sampling weights created by the NHIS for the Sample Adult Core were applied in all analyses to generate nationally representative population estimates. Analyses were conducted using SAS software, version 9 (which includes complex survey design procedures) (16) and SUDAAN (17). Age-adjusted prevalences were generated in SUDAAN and the remaining analyses were conducted in SAS; all standard error estimates were adjusted for the complex survey design of the NHIS. Estimates considered unstable (i.e., having a relative standard error [RSE] >30%) do not meet minimum reliability criteria and are not reported in the tables. Estimates considered potentially unreliable (RSE between 20% and 30%) are reported and have been flagged as such in tables and footnotes.
Construct validity
Because this analysis examined a newly developed question on work limitations attributable to arthritis, the construct validity (known groups validity method) of the question was examined among an a priori selection of variables that were expected to reflect greater limitations, less employment, and generally less favorable findings among people with AAWL compared with those without AAWL. Study findings supported a priori hypotheses regarding the relationship of AAWL status with physical and demographic variables, providing evidence for construct validity for AAWL in this study. For example, 80.3% of people reporting AAWL also responded yes to arthritis-attributable activity limitation, whereas only 18.4% of those without AAWL indicated arthritis-attributable activity limitation. Among other features, individuals with AAWL also reported greater median joint pain (8.0 versus 5.4 on a 0–10 scale), more affected joints on average (5.0 versus 2.2), and consistently more limitations in both the social/leisure domain (19.6% versus 2.8%) and the functional domain (67.0% versus 20.7%). In addition, individuals with AAWL had much lower workforce participation compared with those without AAWL (42.3% versus 73.7%). A higher percentage of respondents with AAWL reported not working all of the previous year (44.0% versus 18.1%) and self identified as not working due to generic disability (62.8% versus 25.6%) compared with those without AAWL.
Descriptive analyses
Once construct validity was satisfied, the descriptive analysis served 2 purposes: to estimate the prevalence of AAWL and to characterize the sample. Population prevalence of AAWL was estimated and age adjusted using the projected 2000 standard population (18). All respondents were included in the denominator for population prevalence estimates, including individuals with chronic joint symptoms (joint symptoms that began at least 3 months ago in the absence of arthritis). To determine what characteristics were associated with AAWL, we first stratified adults with arthritis by reported AAWL status. The prevalence of additional demographic, physical, health-related, and employment characteristics was then estimated by AAWL status with proportions and 95% confidence intervals (95% CIs).
Regression analyses
To identify potential correlates of AAWL, the relationship between selected variables and AAWL was estimated in age-adjusted logistic regression models with odds ratios (ORs) and 95% CIs. A complete case analysis method, in which all respondents had complete information for all variables of interest, was used for modeling. We tested for interactions between arthritis-attributable activity limitations and both functional/social/leisure limitations and employment status in association with AAWL, using a significance criteria of P = 0.05.
Forward stepwise logistic regression was then conducted to identify variables to be included in the multivariable model, with all variables analyzed in the univariable analyses considered for inclusion. Variables were determined to be significantly associated with AAWL at P ≤ 0.20. Highest educational attainment, marital status, and anxiety/depression did not meet the minimum significance criterion; however, they were included in the final multivariable model because each has been previously reported to be a significant risk factor for AAWL. Multivariable ORs and 95% CIs were estimated in a model that included the variables that were significant in the stepwise forward regression procedure and the 3 variables that were significant in previous reports. The multivariable analysis was limited to people for whom there was complete information for all variables of interest.
RESULTS
Population prevalence estimates (Table 1) show that 5.3%, or 6.9 million US adults between the ages of 18 and 64 years report AAWL. AAWL was more common in older age groups and age-adjusted AAWL prevalence was higher among women, non-Hispanic blacks, and individuals with lower education and income. Among those with arthritis, AAWL was reported by 29.5%, or nearly 1 in 3.
Table 1.
National US population prevalence (weighted) and 95% confidence intervals (95% CIs) of arthritis-attributable work limitation, crude and age adjusted*
| No. in 1,000s | Crude prevalence (95% CI) | Age-adjusted prevalence (95% CI) | |
|---|---|---|---|
| Total (age 18–64) | 6,884 | 5.3 (5.0–5.7) | 5.3 (5.0–5.7) |
| Age, years | |||
| 18–24 | 210 | 1.0 (0.6–1.5)† | — |
| 25–44 | 1,910 | 3.1 (2.8–3.5) | — |
| 45–64 | 4,765 | 10.2 (9.4–11.0) | — |
| Sex | |||
| Male | 2,739 | 4.3 (3.9–4.9) | 4.3 (3.9–4.9) |
| Female | 4,146 | 6.3 (5.8–6.9) | 6.3 (5.8–6.8) |
| Race/ethnicity | |||
| Non-Hispanic white | 4,955 | 5.4 (5.0–5.9) | 5.2 (4.7–5.6) |
| Non-Hispanic black | 1,057 | 6.9 (6.0–8.0) | 7.7 (6.8–8.8) |
| Hispanic | 567 | 3.7 (3.0–4.5) | 4.7 (3.9–5.7) |
| Non-Hispanic other | 306 | 4.3 (3.2–6.0) | 5.0 (3.6–6.8) |
| Education | |||
| High school or less | 1,504 | 8.4 (7.3–9.6) | 8.6 (7.5–9.8) |
| High school graduate | 2,332 | 6.4 (5.7–7.2) | 6.2 (5.5–7.0) |
| Some college | 1,467 | 5.4 (4.6–6.2) | 6.3 (5.4–7.2) |
| At least college | 1,582 | 3.3 (2.9–3.8) | 3.2 (2.9–3.7) |
| Annual household income | |||
| <$20,000 | 2,108 | 10.6 (9.5–11.8) | 12.6 (11.4–13.9) |
| ≥$20,000 | 4,423 | 4.3 (3.9–4.7) | 4.2 (3.8–4.6) |
| Unknown | 353 | 6.3 (4.6–8.4) | 5.9 (4.3–8.1) |
Based on projected US Bureau of the Census 2000 population (18) and stratified by 4 age groups: 18–34, 35–44, 45–54, and 55–64.
Potentially unreliable, based on an estimate with relative standard error of 20–30%.
The distributions of potentially associated characteristics are shown in Table 2 (unweighted n = 3,586); variables relevant to construct validity have been flagged here. In univariable models (Table 2), all characteristics were associated with AAWL except age, sex, insurance status, BMI (overweight), and marital status (married). In the multivariable analysis, there was a strong and highly significant association between arthritis-attributable activity limitations and AAWL (OR 9.1, 95% CI 7.1–11.6). AAWL was moderately higher (and statistically significant) among non-Hispanic blacks (OR 1.6), Hispanics (OR 1.8), those with an unknown income (OR 2.1), and those with functional/social/leisure limitations (OR 1.8) or recurring pain (OR 1.7). Four groups were significantly less likely to report AAWL: people with at least a college education (OR 0.6), those with an annual household income ≥$20,000 (OR 0.7), those rating their health as good to excellent (OR 0.7), and women (OR 0.8).
Table 2.
Prevalence of arthritis-attributable work limitation (AAWL) and univariable and multivariable-adjusted odds ratios (ORs) and 95% confidence intervals (95% CIs) of associations with AAWL status, by selected characteristics, among persons with doctor-diagnosed arthritis (complete case analysis, unweighted n = 3,586)
| AAWL, % |
Univariable |
Multivariable adjusted* |
||||
|---|---|---|---|---|---|---|
| No | Yes | OR | 95% CI | OR | 95% CI | |
| Demographics | ||||||
| Age, years | ||||||
| 18–24 | 4.0 | 2.9 | 1.0 | 1.0 | ||
| 25–44 | 28.3 | 27.2 | 1.3 | (0.8–2.3) | 1.5 | (0.7–3.2) |
| 45–64 | 67.7 | 69.9 | 1.4 | (0.9–2.4) | 1.0 | (0.5–2.1) |
| Sex | ||||||
| Male | 42.3 | 39.6 | 1.0 | 1.0 | ||
| Female | 57.7 | 60.4 | 1.1 | (0.9–1.3) | 0.8 | (0.6–1.0) |
| Race/ethnicity | ||||||
| Non-Hispanic white | 81.7 | 71.5 | 1.0 | 1.0 | ||
| Non-Hispanic black | 9.5 | 15.6 | 1.9 | (1.5–2.4) | 1.6 | (1.2–2.3) |
| Hispanic | 5.6 | 8.2 | 1.7 | (1.3–2.2) | 1.8 | (1.2–2.6) |
| Non-Hispanic other | 3.2 | 4.8 | 1.7 | (1.1–2.8) | 1.4 | (0.8–2.4) |
| Education | ||||||
| High school or less | 11.0 | 21.9 | 1.0 | 1.0 | ||
| High school graduate | 29.5 | 34.8 | 0.6 | (0.5–0.8) | 0.9 | (0.6–1.3) |
| Some college | 21.8 | 21.2 | 0.5 | (0.4–0.6) | 0.8 | (0.6–1.1) |
| At least college | 37.8 | 22.1 | 0.3 | (0.2–0.4) | 0.6 | (0.4–0.8) |
| Annual household income | ||||||
| >$20,000 | 11.1 | 31.1 | 1.0 | 1.0 | ||
| ≥$20,000 | 85.9 | 63.3 | 0.3 | (0.2–0.3) | 0.7 | (0.5–1.0) |
| Unknown | 3.0 | 5.6 | 0.7 | (0.5–1.0) | 2.1 | (1.2–3.7) |
| Marital/cohabitating status | ||||||
| Never married | 11.1 | 10.9 | 1.0 | 1.0 | ||
| Married/common law | 70.0 | 62.0 | 0.9 | (0.7–1.1) | 1.1 | (0.8–1.5) |
| Divorced/separated/widowed | 18.9 | 27.0 | 1.4 | (1.1–1.9) | 1.1 | (0.8–1.6) |
| Body mass index | ||||||
| <18.5 | 1.0 | 2.1 | 3.0 | (1.6–5.9) | 2.1 | (1.1–4.2) |
| 18.5–24.9 | 28.4 | 21.1 | 1.0 | 1.0 | ||
| 25.0–29.9 | 35.8 | 28.8 | 1.1 | (0.9–1.3) | 1.1 | (0.8–1.5) |
| ≥30 | 35.0 | 48.1 | 1.9 | (1.5–2.3) | 1.3 | (1.0–1.8) |
| Physical activity | ||||||
| Recommended | 35.0 | 20.7 | 1.0 | 1.0 | ||
| Insufficient | 35.1 | 52.3 | 1.3 | (1.1–1.6) | 0.9 | (0.7–1.2) |
| Inactive | 30.0 | 27.0 | 3.0 | (2.4–3.7) | 1.2 | (0.9–1.6) |
| Arthritis characteristics | ||||||
| Site of joint pain | ||||||
| None | 33.9 | 13.3 | 1.0 | |||
| Upper extremity | 14.5 | 12.1 | 2.1 | (1.6–2.9) | 1.3 | (0.9–1.9) |
| Lower extremity | 25.2 | 22.0 | 2.2 | (1.7–2.9) | 1.1 | (0.8–1.6) |
| Unspecified | 1.5 | 1.3 | 2.1 | (1.0–4.7) | 1.0 | (0.4–2.2) |
| More than 1 | 24.9 | 51.3 | 5.3 | (4.2–6.6) | 1.5 | (1.1–2.0) |
| Arthritis-attributable activity limitation† | ||||||
| No | 81.6 | 19.7 | 1.0 | 1.0 | ||
| Yes | 18.4 | 80.3 | 18.2 | (14.8–22.3) | 9.1 | (7.1–11.6) |
| Physical characteristics | ||||||
| Functional/social/leisure limitations† | ||||||
| No | 79.2 | 32.7 | 1.0 | 1.0 | ||
| Yes | 20.8 | 67.3 | 7.8 | (6.5–9.4) | 1.8 | (1.4–2.3) |
| Chronic conditions, no. | ||||||
| 0 | 24.8 | 11.9 | 1.0 | 1.0 | ||
| 1 | 24.9 | 16.9 | 1.4 | (1.1–1.8) | 1.2 | (0.9–1.7) |
| 2 | 19.0 | 18.6 | 2.0 | (1.5–2.8) | 1.1 | (0.8–1.7) |
| 3 | 12.8 | 14.9 | 2.4 | (1.8–3.3) | 1.1 | (0.7–1.7) |
| 4 | 7.5 | 9.6 | 2.7 | (1.9–3.9) | 1.0 | (0.6–1.7) |
| 5 | 4.9 | 10.5 | 4.4 | (3.1–6.3) | 0.9 | (0.5–1.6) |
| ≥6 | 6.1 | 17.7 | 6.1 | (4.5–8.3) | 0.8 | (0.5–1.3) |
| Specific conditions | ||||||
| Neck or back pain | ||||||
| No | 50.6 | 24.0 | 1.0 | 1.0 | ||
| Yes | 49.4 | 76.0 | 3.2 | (2.7–3.9) | 1.5 | (1.2–1.9) |
| Anxiety/depression | ||||||
| No | 21.5 | 45.1 | 1.0 | 1.0 | ||
| Yes | 78.5 | 54.9 | 3.0 | (2.5–3.6) | 1.1 | (0.8–1.4) |
| Recurring pain | ||||||
| No | 35.9 | 74.2 | 1.0 | 1.0 | ||
| Yes | 64.1 | 25.8 | 5.2 | (4.3–6.1) | 1.7 | (1.3–2.2) |
| Self-rated health in general† | ||||||
| Fair/poor | 15.0 | 50.4 | 1.0 | 1.0 | ||
| Good/very good/excellent | 85.0 | 49.7 | 0.2 | (0.2–0.2) | 0.7 | (0.5–0.9) |
| Health care access and utilization | ||||||
| Health insurance | ||||||
| Not covered‡ | 10.4 | 14.4 | 1.0 | 1.0 | ||
| Public | 9.5 | 29.6 | 2.3 | (1.7–2.9) | 0.7 | (0.5–1.1) |
| Private | 77.2 | 50.7 | 0.5 | (0.4–0.6) | 0.9 | (0.7–1.3) |
| Public and private | 2.8 | 5.4 | 1.4 | (0.9–2.1) | 0.7 | (0.3–1.3) |
| No. office visits to any doctor in past year | ||||||
| 0–7 | 74.4 | 49.4 | 1.0 | 1.0 | ||
| ≥8 | 25.6 | 50.6 | 3.0 | (2.5–3.5) | 1.4 | (1.1–1.8) |
| Generic work characteristics§ | ||||||
| Work status† | ||||||
| Not working | 73.7 | 42.3 | 1.0 | 1.0 | ||
| Working | 26.3 | 57.7 | 3.8 | (3.2–4.6) | 1.3 | (1.0–1.7) |
| Received disability benefits in last year† | ||||||
| No | 92.9 | 68.7 | 1.0 | 1.0 | ||
| Yes | 7.1 | 31.3 | 6.0 | (4.8–7.5) | 1.4 | (1.0–2.0) |
Multivariable-adjusted model included all variables listed in the table.
A priori variables of interest for construct validity.
Uninsured/not covered consistent with definition in Health, United States (10,15). Respondents reporting both private insurance and no insurance coverage were classified as uninsured, consistent with National Center for Health Statistics (10).
Generic work characteristics are not arthritis attributable.
DISCUSSION
Arthritis affects ~21% of all US adults ≥18 years of age and roughly 18% of adults, or 23.4 million, between the ages of 18 and 64. Of those with arthritis in this age group, almost 30% report AAWL, corresponding to 5.3% of the adult population (almost 6.9 million people). Overall, people with AAWL had multiple indicators of poor physical health and function (e.g., high BMI, joint and other pains, physical limitations in multiple domains, and frequent doctor’s office visits), demonstrating considerable burden in those with AAWL. Notably, this burden seems to fall disproportionately on nonwhite minority groups. Jordan states that racial and ethnic differences in health status may reflect complex relationships between socioeconomic status, ethnicity, and biologic and lifestyle factors (19). While the reasons for these differences are not understood, language barriers and use of health care services may contribute (20). Differences in impact may also reflect racial/ethnic differences in type of work activity (2).
AAWL status was independent of site of joint pain (e.g., upper versus lower extremity). This finding may be surprising to readers; however, a recent study by Allaire et al examining occupational hand use among a cohort of employed people with rheumatoid arthritis (RA) found that 83% of the sample reported extensive occupational hand use and that extensive hand use was required across all types of jobs (21). These authors note that occupational hand use is increasing due to increased computer work. The results of our study may reflect the potential problem for people with arthritis in the hand(s) (e.g., RA, osteoarthritis of the hand) across job sectors.
Research has demonstrated several consistent risk factors for work disability among individuals with musculoskeletal conditions. Among correlates of AAWL examined here, educational attainment (except having at least a college degree) was not found to be significant in the multivariable model, a contrast to some previous findings (22–24) but not surprising given the mixed importance of education in a recent overview of studies examining work disability in patients with RA (6). The lack of significance of health insurance status also contradicts previous results (22) whereas the importance of higher levels of joint pain is consistent with other studies (23,24). The association of functional limitations (23,25,26) and the receipt of disability payments (27) with AAWL in this study was also consistent with previous results.
Differences observed between results of this and previous studies may be explained in part by differences in sample (e.g., nationally representative versus clinic patients, and condition-specific estimates versus our wider arthritis definition). Our case-finding question derives from the original definition of arthritis and other rheumatic conditions as defined by the National Arthritis Data Workgroup with the intent to separate the major musculoskeletal conditions into more manageable categories and to avoid “orphaning” rheumatic conditions (e.g., lupus, fibromyalgia) that would otherwise be omitted as not clinical arthritis (2).
The findings of this study are subject to at least 4 limitations. First, data were from self reports of survey participants and may be subject to recall bias. Also, the presence of arthritis was not confirmed by a health care provider; however, this case-finding question appears valid for public health surveillance purposes (28,29). We adjusted for the presence of depression, pain, and other conditions in the multivariable analysis with dichotomous variables derived from self report (rather than from standardized, diagnostically oriented instruments) because the purpose of including these variables was to statistically control for these conditions, and not to identify them as clinical cases. Second, particularly for individuals with comorbid conditions, it may be difficult to attribute one’s work limitation to one specific condition accurately. Third, the work limitation case-finding question asks if arthritis or joint symptoms affect whether a person works, as well as the amount or type of work a person does. The wording of this question does not allow us to separate respondents with AAWL who could not work from those who continued to work but with modifications to the amount or type. In addition, we could not determine whether the factors associated with AAWL may be different for each of these groups, and constraints of the survey data did not allow for an examination of employment type. Finally, cross-sectional data cannot be used to infer causation, and therefore we cannot determine the temporal sequencing of arthritis and work limitation.
Strengths of this study include use of a data source sufficiently large enough to allow adjustment for potential confounders and to enable us to develop US national prevalence estimates for AAWL. The 6.9 million prevalence estimate reported in this article differs from an earlier report of 8.2 million (2) because more conservative inclusion criteria were used (Figure 1). Results can therefore be used as a benchmark for future prevalence estimates to monitor progress toward Healthy People 2010 (8) and other public health goals. Also, individuals with chronic joint symptoms may have undiagnosed arthritis; therefore, because those individuals were included in the denominator of our prevalence estimates, our estimates are likely conservative.
Past studies of rheumatic diseases have suggested that primary prevention of work disability may be more effective than interventions after job loss or work disability has occurred (26,30,31), implying a need for ways to identify those at risk of work disability in order to offer timely interventions. Characteristics associated with AAWL in this study suggest places to start. Once individuals have been identified, however, programs exist to address job retention (26,32). In a recent study, a vocational rehabilitation program provided to employed patients with rheumatic diseases who were at risk for job loss was shown both to delay and reduce job loss (33), while other research has explored the success of behavioral coping in relation to employment participation and productivity (7,34).
Concurrently, the role of early diagnosis and appropriate medical and self management remains strong, as does the role of public health in educating individuals with arthritis and AAWL and in promoting appropriate self management. Current evidence-based arthritis self-management programs include the Arthritis Foundation Self-Help Course, the Arthritis Foundation Exercise Program (formerly PACE), and the Arthritis Foundation Aquatics Program. Each of these programs have been shown to be effective in reducing physical and functional limitations, decreasing pain, and delaying disability due to arthritis (35), which may contribute to AAWL. Offering an arthritis-specific self-management program in the corporate disease management setting has been shown to be effective in reducing pain, physician visits, and health care costs per patient with arthritis (36).
In addition, reducing the personal and societal financial impact of AAWL is an important but unstated goal of most discussions. Many individuals who are medically unable to work receive Social Security or other public benefits, and with less than 0.005% of Social Security recipients of working age leaving the program to take a job each year (37) and only 3–4% of all beneficiaries with arthritis-related disability ever leaving the program (25), it is in the best financial interest of the patient and the public to identify and develop appropriate accommodations and interventions for AAWL. Estimates vary, but between 79% and 84% of the disabled population in general express a desire to be working (22,38). Because arthritis and various other disabilities increase with age, the population is aging, and arthritis currently ranks as the most prevalent cause of disability, the work status of people with arthritis has considerable implications for business and the national economy, especially as indirect costs of arthritis have been estimated at $35.1 billion (39). Moreover, protecting workers from disability, injury, and prolonged negative effects of illness makes simple social and economic sense (40).
As stated elsewhere, service provision and policy improvements related to work disability resulting from chronic health conditions will benefit from additional research (21). Possible future research questions relevant to public health and arthritis management include: What work are people with arthritis unable to do? Which groups are more affected and why? How can interventions for these groups be tested, targeted, delivered? There is evidence for the value of interventions that prevent work limitation from occurring (26,30,31) and that rehabilitate workers (33,41), therefore both could be explored in relation to delivery of interventions. A longitudinal study is also called for to distinguish the temporal sequence of AAWL and associated limitations.
The Centers for Disease Control and Prevention and state-based arthritis programs strive to prevent functional limitation and disability among individuals with arthritis, and describing and addressing work limitation are important components of that goal. This initial characterization of AAWL will aid in informing research and the development and evaluation of interventions to decrease work limitation experienced by individuals with arthritis.
Acknowledgments
The findings and conclusions in this article are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Supported by the Centers for Disease Control and Prevention.
Footnotes
AUTHOR CONTRIBUTIONS
Ms Theis had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study design. Theis, Hootman, Helmick, Yelin.
Acquisition of data. Theis, Hootman.
Analysis and interpretation of data. Theis, Murphy, Hootman, Helmick, Yelin.
Manuscript preparation. Theis, Murphy, Hootman, Helmick, Yelin.
Statistical analysis. Theis, Murphy, Hootman.
References
- 1.Centers for Disease Control and Prevention (CDC) Prevalence of disabilities and associated health conditions among adults: United States, 1999 [published erratum appears in MMWR Morb Mortal Wkly Rep 2001;50:149] MMWR Morb Mortal Wkly Rep. 2001;50:120–5. [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) Racial/ethnic differences in the prevalence and impact of doctor-diagnosed arthritis: United States, 2002. MMWR Morb Mortal Wkly Rep. 2005;54:119–23. [PubMed] [Google Scholar]
- 3.Lacaille D, Hogg RS. The effect of arthritis on working life expectancy. J Rheumatol. 2001;28:2315–9. [PubMed] [Google Scholar]
- 4.Allaire S, Wolfe F, Niu J, LaValley M, Michaud K. Work disability and its economic effect on 55–64-year-old adults with rheumatoid arthritis. Arthritis Rheum. 2005;53:603–8. doi: 10.1002/art.21326. [DOI] [PubMed] [Google Scholar]
- 5.Yelin EH. Musculoskeletal conditions and employment. Arthritis Care Res. 1995;8:311–7. doi: 10.1002/art.1790080417. [DOI] [PubMed] [Google Scholar]
- 6.Verstappen SM, Bijlsma JW, Verkleij H, Buskens E, Blaauw AA, ter Borg EJ, et al. Overview of work disability in rheumatoid arthritis patients as observed in cross-sectional and longitudinal surveys. Arthritis Rheum. 2004;51:488–97. doi: 10.1002/art.20419. [DOI] [PubMed] [Google Scholar]
- 7.Boonen A, Chorus A, Miedema H, van der Heijde D, Landewe R, Schouten H, et al. Withdrawal from labour force due to work disability in patients with ankylosing spondylitis. Ann Rheum Dis. 2001;60:1033–9. doi: 10.1136/ard.60.11.1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.US Department of Health and Human Services. Healthy people 2010: understanding and improving health. 2. Washington, DC: US Government Printing Office; 2000. Objectives. [Google Scholar]
- 9.Botman SL, Moore TF, Moriarty CL, Parsons VL. Design and estimation for the National Health Interview Survey, 1995–2004. Vital Health Stat 2. 2000;130:10. [Google Scholar]
- 10.National Center for Health Statistics 2003. Data file documentation, National Health Interview Survey, 2002 (machine readable data file and documentation) Hyattsville (MD): National Center for Health Statistics, Centers for Disease Control and Prevention; 2003. URL: http://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2002/srvydesc.pdf. [Google Scholar]
- 11.National Center for Chronic Disease Prevention and Health Promotion. Arthritis Case Definition for estimating population prevalence. Atlanta: Centers for Disease Control and Prevention; 2006. URL: http://www.cdc.gov/arthritis/data_statistics/case_def.htm. [Google Scholar]
- 12.National Center for Chronic Disease Prevention and Health Promotion. FAQs (data related): self-reported arthritis case definition. Atlanta: Centers for Disease Control and Prevention; 2006. URL: http://www.cdc.gov/arthritis/data_statistics/faqs/case_definition.htm. [Google Scholar]
- 13.US Department of Health and Human Services. Physical activity and health: a report of the Surgeon General. Atlanta (GA): US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion; 1996. [Google Scholar]
- 14.American College of Sports Medicine Position Stand. The recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults [review] Med Sci Sports Exerc. 1998;30:975–91. doi: 10.1097/00005768-199806000-00032. [DOI] [PubMed] [Google Scholar]
- 15.National Center for Health Statistics. Health, United States, 2004, with chartbook on trends in health of Americans. Hyattsville (MD): National Center for Health Statistics; 2004. [PubMed] [Google Scholar]
- 16.SAS Institute. SAS/STAT user’s guide. Version 9. Cary (NC): SAS Institute; 2004. [Google Scholar]
- 17.Research Triangle Institute. SUDAAN language manual. Research Triangle Park (NC): Research Triangle Institute; 2002. [Google Scholar]
- 18.Klein RJ, Schoenborn CA. Healthy People 2010 stat notes. 20. Hyattsville (MD): National Center for Health Statistics; 2001. Age adjustment using the 2002 projected US population; pp. 1–10. [PubMed] [Google Scholar]
- 19.Jordan JM. Effect of race and ethnicity on outcomes in arthritis and rheumatic conditions. Curr Opin Rheumatol. 1999;11:98–103. doi: 10.1097/00002281-199903000-00003. [DOI] [PubMed] [Google Scholar]
- 20.Escalante A, del Rincon I. Epidemiology and impact of rheumatic disorders in the United States Hispanic population [published erratum appears in Curr Opin Rheumatol 2001;13: 244] Curr Opin Rheumatol. 2001;13:104–10. doi: 10.1097/00002281-200103000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Allaire S, Wolfe F, Niu J, Baker N, Michaud K, LaValley M. Extent of occupational hand use among persons with rheumatoid arthritis. Arthritis Rheum. 2006;55:294–9. doi: 10.1002/art.21839. [DOI] [PubMed] [Google Scholar]
- 22.Partridge AJ, Karlson EW, Daltroy LH, Lew RA, Wright EA, Fossel AH, et al. Risk factors for early work disability in systemic lupus erythematosus: results from a multicenter study. Arthritis Rheum. 1997;40:2199–206. doi: 10.1002/art.1780401214. [DOI] [PubMed] [Google Scholar]
- 23.Backman CL. Employment and work disability in rheumatoid arthritis [review] Curr Opin Rheumatol. 2004;16:148–52. doi: 10.1097/00002281-200403000-00014. [DOI] [PubMed] [Google Scholar]
- 24.Reisine S, McQuillan J, Fifield J. Predictors of work disability in rheumatoid arthritis patients: a five-year followup. Arthritis Rheum. 1995;38:1630–7. doi: 10.1002/art.1780381115. [DOI] [PubMed] [Google Scholar]
- 25.Yelin EH, Henke CJ, Epstein WV. Work disability among persons with musculoskeletal conditions. Arthritis Rheum. 1986;29:1322–33. doi: 10.1002/art.1780291104. [DOI] [PubMed] [Google Scholar]
- 26.Allaire SH, Anderson JJ, Meenan RF. Reducing work disability associated with rheumatoid arthritis: identification of additional risk factors and persons likely to benefit from intervention. Arthritis Care Res. 1996;9:349–57. doi: 10.1002/1529-0131(199610)9:5<349::aid-anr1790090503>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 27.Lacaille D, Sheps S, Spinelli JJ, Chalmers A, Esdaile JM. Identification of modifiable work-related factors that influence the risk of work disability in rheumatoid arthritis. Arthritis Rheum. 2004;51:843–52. doi: 10.1002/art.20690. [DOI] [PubMed] [Google Scholar]
- 28.Sacks JJ, Harrold LR, Helmick CG, Gurwitz JH, Emani S, Yood RA. Validation of a surveillance case definition for arthritis. J Rheumatol. 2005;32:340–7. [PubMed] [Google Scholar]
- 29.Bombard JM, Powell KE, Martin LM, Helmick CG, Wilson WH. Validity and reliability of self-reported arthritis: Georgia senior centers, 2000–2001. Am J Prev Med. 2005;28:251–8. doi: 10.1016/j.amepre.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 30.Allaire SH. Update on work disability in rheumatic diseases [review] Curr Opin Rheumatol. 2001;13:93–8. doi: 10.1097/00002281-200103000-00001. [DOI] [PubMed] [Google Scholar]
- 31.Frank AO, Chamberlain MA. Keeping our patients at work: implications for the management of those with rheumatoid arthritis and musculoskeletal conditions [letter] Rheumatology (Oxford) 2001;40:1201–5. doi: 10.1093/rheumatology/40.11.1201. [DOI] [PubMed] [Google Scholar]
- 32.Lerner D, Allaire SH, Reisine ST. Work disability resulting from chronic health conditions [review] J Occup Environ Med. 2005;47:253–64. doi: 10.1097/01.jom.0000150206.04540.e7. [DOI] [PubMed] [Google Scholar]
- 33.Allaire SH, Li W, LaValley MP. Reduction of job loss in persons with rheumatic diseases receiving vocational rehabilitation: a randomized controlled trial. Arthritis Rheum. 2003;48:3212–8. doi: 10.1002/art.11256. [DOI] [PubMed] [Google Scholar]
- 34.Gignac MA. Arthritis and employment: an examination of behavioral coping efforts to manage workplace activity limitations. Arthritis Rheum. 2005;53:328–36. doi: 10.1002/art.21169. [DOI] [PubMed] [Google Scholar]
- 35.Brady TJ, Kruger J, Helmick CG, Callahan LF, Boutaugh ML. Intervention programs for arthritis and other rheumatic diseases [review] Health Educ Behav. 2003;30:44–63. doi: 10.1177/1090198102239258. [DOI] [PubMed] [Google Scholar]
- 36.Musich SA, Schultz AB, Burton WN, Edington DW. Overview of disease management approaches: implications for corporate-sponsored programs. Dis Manag Health Outcomes. 2004;12:299–326. [Google Scholar]
- 37.LaPlante M, Kennedy J, Stephen H, Wenger B. Disability statistics abstract no. 11, disability and employment. Washington (DC): US Department of Education, National Institute on Disability and Rehabilitation Research; 1996. [Google Scholar]
- 38.Stoddard S, Jane L, Ripple J, Kraus L. An InfoUse Report. Washington (DC): US Department of Education; 1998. Chartbook on work and disability in the United States, 1998. [Google Scholar]
- 39.Yelin E, Cisternas MG, Pasta DJ, Trupin L, Murphy L, Helmick CG. Medical care expenditures and earnings losses of persons with arthritis and other rheumatic conditions in the United States in 1997: total and incremental estimates. Arthritis Rheum. 2004;50:2317–26. doi: 10.1002/art.20298. [DOI] [PubMed] [Google Scholar]
- 40.Lerner DJ, Amick BC, 3rd, Malspeis S, Rogers WH. A national survey of health-related work limitations among employed persons in the United States. Disabil Rehabil. 2000;22:225–32. doi: 10.1080/096382800296791. [DOI] [PubMed] [Google Scholar]
- 41.Straaton KV, Maisiak R, Wrigley JM, White MB, Johnson P, Fine PR. Barriers to return to work among persons unemployed due to arthritis and musculoskeletal disorders. Arthritis Rheum. 1996;39:101–9. doi: 10.1002/art.1780390114. [DOI] [PubMed] [Google Scholar]