Abstract
OBJECTIVE
To assess the long-term cost-effectiveness of aspirin use among adults aged ≥40 years with newly diagnosed type 2 diabetes.
RESEARCH DESIGN AND METHODS
We used a validated cost-effectiveness model of type 2 diabetes to assess the lifetime health and cost consequences of use or nonuse of aspirin. The model simulates the progression of diabetes and accompanying complications for a cohort of subjects with type 2 diabetes. The model predicts the outcomes of type 2 diabetes along five disease paths (nephropathy, neuropathy, retinopathy, coronary heart disease, and stroke) from the time of diagnosis until age 94 years or until death.
RESULTS
Over a lifetime, aspirin users gained 0.31 life-years (LY) or 0.19 quality-adjusted LYs (QALYs) over nonaspirin users, at an incremental cost of $1,700; the incremental cost-effectiveness ratio (ICER) of aspirin use was $5,428 per LY gained or $8,801 per QALY gained. In probabilistic sensitivity analyses, the ICER was <$30,000 per QALY in all of 2,000 realizations in two scenarios.
CONCLUSIONS
Regular use of aspirin among people with newly diagnosed diabetes is cost-effective.
Diabetes is a major risk factor for cardiovascular disease (CVD) among people with diabetes. The risk of developing coronary heart disease (CHD) is two to four times higher for people with diabetes than those without diabetes (1). Aspirin decreases CHD incidence in adults at risk for CVD (2,3).
The American Diabetes Association recommends aspirin use for primary prevention of CVD in diabetic patients aged >40 years or in all people aged >30 years if they have risk factors for CVD and no aspirin contraindications (4). However, the cost-effectiveness of aspirin use for primary prevention in a diabetic population has not been evaluated. Previous studies have evaluated the cost-effectiveness of aspirin therapy for primary prevention of CVD in the general population (5,6). These studies concluded that aspirin use was cost saving or cost-effective. It is not known if the same conclusion holds for people with diabetes. The cost-effectiveness of aspirin therapy could differ between people with diabetes and the general population because of the additional cost and health consequences related to diabetes and its complications. Our study evaluates the lifetime cost-effectiveness of aspirin use in adults aged ≥40 years who have newly diagnosed type 2 diabetes.
RESEARCH DESIGN AND METHODS
We assessed the cost-effectiveness of aspirin use by comparing the long-term health and cost consequences of aspirin use and no aspirin use among people with newly diagnosed type 2 diabetes under different scenarios, using a diabetes cost-effectiveness model developed by the Centers for Disease Control and Prevention (CDC) and the Research Triangle Institute (RTI).
The model
Details of the CDC-RTI diabetes cost-effectiveness model appear elsewhere (7,8). Briefly, it is a Markov disease progression model of type 2 diabetes. The model starts patients at the time of diagnosis of their diabetes and progresses them until death or until age 94 years. Diabetic patients in the model can develop five complications: neuropathy, nephropathy, retinopathy, CHD (i.e., cardiac arrest [CA]/myocardial infarction [MI] and angina), and stroke. Each complication has its own costs, and the model aggregates costs over a patient's lifetime. Death can result from diabetes complications or from other causes (7). The model also simulates possible side effects of aspirin therapy on gastrointestinal bleeding. The transitional probabilities between modeled disease states and intervention effectiveness parameters were derived from the Framingham Heart Study, the UK Prospective Diabetes Study (UKPDS), and other clinical trials and observational studies (9–11).
The model was validated following procedures of the American Diabetes Association Consensus Panel on Computer Modeling (12). Overall, the diabetes cost-effectiveness model accurately simulates the natural history of the diabetic population. This model has been used to evaluate the cost-effectiveness of many type 2 diabetes interventions (7,8).
We defined the demographics of our simulated population as described below. We calculated incidence rates for cohorts defined through age, sex, and race/ethnicity using data from the 2005 National Health Interview Survey, reported by the CDC. We estimated the prevalence of hypertension, high cholesterol, and smoking using National Health and Nutrition Examination Survey (NHANES) 2001–2006 data. We also obtained the initial prevalence of diabetes complications (nephropathy, neuropathy, retinopathy, CHD, and stroke) using NHANES data from 2001 to 2006. The initial A1C level was assumed to be 6.8% based on UKPDS (9,10).
Baseline analysis
We modeled daily use of 80 mg of aspirin among a cohort of U.S. residents aged 40–94 years who, in 2006, were newly diagnosed with diabetes. We defined standard care for subjects with diabetes: all patients received intensive glucose control with a treatment intensity similar to that of the intensive arm of the UKPDS (A1C 7%); and hypertensive patients were treated to meet the target diastolic blood pressure of 80 mmHg, the target blood pressure rate in the UKPDS intensive arm. We assessed the cost-effectiveness of aspirin use plus standard care compared with standard care alone. We assumed that aspirin was effective for everyone who took it. We also assumed 100% compliance. Table 1 shows the main analytic parameters' values and the sources of these parameters.
Table 1.
Baseline values and sources of data for selected variables used to estimate the cost-effectiveness of aspirin use among people with diabetes (costs in 2006 U.S. dollars)
| Parameter (reference number) | Base-case estimates |
|---|---|
| Relative risk of primary prevention | RR (95% CI) |
| Major coronary events (14) | 0.82 (0.75–0.90) |
| Overall stroke (14) | 0.95 (0.85–1.06) |
| Hemorrhagic (14) | 1.32 (1.00–1.75) |
| Ischemic (14) | 0.86 (0.74–1.00) |
| Relative risk of secondary prevention | |
| Major coronary events (14) | 0.80 (0.73–0.88) |
| Annual risk for side effects | % (95% CI) |
| Gastrointestinal bleeding (14) | 0.0003 (0.0002–0.0005) |
| Death resulting from gastrointestinal bleeding (18) | 0.00001 (0.000001–0.0001) |
| Annual cost* | 0.001 (0.001–0.01) |
| Aspirin† | 24 |
| MI (15) | |
| Year 1 | 7,765 |
| Ongoing annual cost after year 1 | 2,006 |
| Stroke (15) | |
| Year 1 | 67,347 |
| Ongoing annual cost after year 1 | 26,553 |
| Gastrointestinal bleeding (18) | |
| Nonfatal | 7,842 |
| Fatal | 7,842 |
| Utility score (17) | |
| Diabetes without complications | 0.689 |
| MI | 0.637 |
| Stroke | 0.617 |
| Gastrointestinal bleeding | 0.970 |
Data are point estimate (95% CI) unless otherwise indicated.
*Per person with newly diagnosed type 2 diabetes.
†Averaging the price of Bayer low-dose aspirin (i.e., baby aspirin) at several large chain pharmacies in the U.S.
Health benefits of regular aspirin usage
A recently published meta-analysis estimated the effect of aspirin use in primary prevention of CVD in patients with diabetes. The conclusion was that the effect of aspirin use in patients with diabetes remains unproved (13). We are aware of no data that suggest that the effect of aspirin on primary prevention of CVD in the diabetic population differs from that in the general population. Accordingly, we used the effects that were derived from a new meta-analyses of clinical trials for the general population in the base-case scenario. In the base-case analysis, for primary prevention, aspirin use reduced annual risk of coronary events by 18% and stroke by 5%; for secondary prevention, aspirin reduced the risk of major coronary events by 20% (14).
In our base-case scenario, we assumed that CVD-free patients with newly diagnosed diabetes received aspirin for primary CVD prevention. Those with a history of MI (13%) at the time of diagnosis of diabetes received aspirin for secondary CVD prevention. In addition, we assumed that the effects of aspirin use on primary or secondary prevention in the trial lasted throughout the lifetime.
Side effects of aspirin use
Aspirin use increases risk of hemorrhagic stroke and reduces risk of ischemic stroke (14). However, we did not have reliable cost data for hemorrhagic stroke. Thus, we used the overall risk ratio (RR) of 0.95 for all stroke events, whether ischemic or hemorrhagic, in the base-case analysis. We modeled ischemic and hemorrhagic strokes separately in the sensitivity analyses, described later. Aspirin use also increases the risk of gastrointestinal bleeding. For major gastrointestinal bleeding, the RR associated with aspirin use was 1.54. We assumed no gastrointestinal bleeding for patients not using aspirin. We estimated that the gastrointestinal bleeding occurred in patients in the aspirin group at a rate of 0.03 per 100 (14). We assumed that patients who experienced aspirin side effects would stop taking aspirin.
Costs
Our analysis, conducted from a health system perspective, includes only direct medical costs. We considered the following: cost of aspirin treatment, costs of the standard care (intensive glycemic control for all patients and intensive hypertension control for patients with hypertension), costs of treating diabetes complications, and costs of treating aspirin side effects. Costs for standard care and diabetes complications were estimated using a multiplicative cost function. This cost function was based on data from adults with diabetes under different treatment regimes and with different complications and comorbidities (15,16). We obtained the costs of aspirin from Web sites of the large chain pharmacies and gastrointestinal bleeding from the literature and added them to the total costs of treatment for diabetes and its complications (Table 1) (5). We also assumed that gastrointestinal bleeding occurs only once and incurs costs only in the first year after occurrence. All costs were converted to 2006 U.S. dollars by using the Consumer Price Index for medical services.
Outcomes
Measures of primary outcomes for our analysis were the number of life-years (LYs) and the number of quality-adjusted LYs (QALYs), measured from time of clinical diagnosis of diabetes until the cohort reaches 94 years of age or death. We used an additive model for the utility measures (17). In this model, patients with characteristics (e.g., demographic characteristics, risk factors, complications, and BMI) differing from the baseline characteristics had those characteristics' disutility coefficients added to the intercept (17). For example, for a male subjects with BMI <30 kg/m2 and without major complications, the state of having diabetes had a utility value of 0.689. If this subject had a cardiac arrest/MI, his utility score was reduced from the baseline score by 0.052. We also assumed no disutility for taking aspirin and a disutility of 0.030 for gastrointestinal bleeding (18). Costs and QALYs were discounted at 3% annually.
Sensitivity analyses
We conducted both one-way and probabilistic sensitivity analyses. For the former, we considered multiple scenarios. We examined the effectiveness and cost-effectiveness for several age-groups and both sexes. We used the upper and lower 95% confidence bounds of the main parameters and the parameters in diabetes subgroups reported by De Berardis et al. (13). Because the average follow-up times in the primary and secondary prevention trials for aspirin use were 5 and 3 years, respectively, we modeled interventions with benefits limited to the trial follow-up time. We also varied the cost of gastrointestinal bleeding and compliance rate and modeled cost-effectiveness of aspirin use for secondary prevention of CVD only.
Substantial proportions of diabetic patients do not receive intensive glycemic or hypertension control (19). Aspirin use might be more effective in these patients because of their increased CVD risk. We modeled the aspirin cost-effectiveness in patients with less intensive glucose or blood pressure control as the UKPDS control arms.
We also modeled ischemic and hemorrhagic strokes separately. We assumed that all strokes in the nonaspirin group were ischemic and modeled the change in costs and effectiveness of aspirin use as a result of increased risk for hemorrhagic stroke and decreased risk for ischemic stroke. We assumed an excess annual risk of hemorrhagic stroke and decreased risk of ischemic stroke as reported in the Antithrombotic Trialists' (ATT) Study (14). The multiplicative cost model did not provide costs for hemorrhagic stroke. Accordingly, we calculated that cost by adjusting the cost of ischemic stroke, using the ratios of the first year and ongoing costs between hemorrhagic stroke and ischemic stroke reported by Pignone et al. (5), respectively. This is equivalent to assuming that the cost ratios between hemorrhagic and ischemic strokes are constant as reported in the study by Pignone et al.
For our probabilistic sensitivity analysis, we randomly varied the following parameters in the model simultaneously based on distributions of their estimates: relative risk of aspirin use for primary and secondary prevention of CHD, stroke, and gastrointestinal bleeding; utilities for all health states; and cost of MI, stroke, and gastrointestinal bleeding. We assumed that efficacy and the rate of side effects followed a log-normal distribution. We assumed a log-normal distribution for MI and stroke cost, a triangular distribution for the cost of gastrointestinal bleeding, and a normal distribution for utility data with reported means and SDs. Running simulations for all age-groups was computationally prohibitive. However, the baseline effectiveness, cost, and cost-effectiveness ratios for the 55–64 years age-group were similar to those for the entire population. Accordingly, we ran 1,000 realizations using parameters on the efficacy of aspirin use reported in the ATT study (14) and the study by De Berardis et al. (13), limited to the 55–64 years age-group, and reported the results as our probabilistic sensitivity analysis.
Results for base-case analysis
Over the lifetime of people with newly diagnosed diabetes, aspirin use reduced the cumulative incidence of CHD events by 3.91% and the CHD mortality rate by 4.65%; however, aspirin increased the cumulative incidence of stroke by 0.51% and the stroke mortality rate by 0.28%. Overall, a person in the aspirin group gained 0.31 LYs and 0.19 QALYs (discounted at 3% annually) compared with a person who did not take aspirin, at an incremental cost of $1,700. The Incremental cost-effectiveness ratio (ICER) was $5,428 per LY gained or $8,801 per QALY gained (Table 2).
Table 2.
Effectiveness and costs of aspirin treatment
| Outcome* | Aspirin group | Nonaspirin group | Difference |
|---|---|---|---|
| Cumulative risk of history of cardiac arrest/MI (%) | 33.15 | 36.15 | −3.00 |
| Cumulative risk of angina (%) | 10.93 | 12.46 | −1.53 |
| Cumulative risk of CHD (%) | 42.12 | 46.03 | −3.91 |
| Cumulative risk of stroke (%) | 16.96 | 16.45 | 0.51 |
| Cumulative risk of gastrointestinal | |||
| bleeding (%) | 0.44 | 0 (only inputs excess risk of gastrointestinal bleeding in the model) | 0.44 |
| Mortality rate due to CHD (%) | 31.15 | 35.80 | −4.65 |
| Mortality rate due to stroke (%) | 6.93 | 6.65 | 0.28 |
| Remaining life years (LYs) | 8.67 | 8.98 | 0.31 |
| Remaining QALYs | 7.34 | 7.15 | 0.19 |
| Costs† | |||
| Cost of aspirin treatment | 278 | 0 | 278 |
| Cost for intensive diabetes and hypertension treatment | 39,809 | 38,398 | 1,411 |
| Cost for treating complications | 31,021 | 31,010 | −10 |
| Total costs | 71,108 | 69,407 | 1,700 |
*Outcomes on effectiveness of aspirin were rounded to the nearest 100th.
†Unit for cost was 2006 US dollars. Data are point estimates.
Results for sensitivity analyses
The one-way sensitivity analysis showed that the ICERs of aspirin use changed moderately if the extreme values for the effect of aspirin on primary prevention of CHD, different sex, aspirin effect on secondary prevention, and modeling different types of strokes separately hold. The ICERs did not change substantially for other variables (Table 3). Using the upper 95% of confidence limits of the effect of aspirin in primary prevention of CHD increased the ICER from $8,801/QALY at baseline to $11,289/QALY. When men and women were modeled separately using parameters in the ATT study (14) and De Berardis et al. (13) study, women always had higher CERs than men: $13,833/QALY vs. $5,752/QALY using parameters in ATT study and $22,259/QALY vs. $3,633/QALY using parameters in De Berardis et al. study. Only considering aspirin effect in secondary prevention of CVD has an ICER of $18,348/QALY. Modeling hemorrhagic stroke and ischemic stroke separately yielded an ICER of $16,484/QALY, which doubled the baseline results.
Table 3.
Cost-effectiveness of aspirin use in the one-way sensitivity analyses (2006 U.S. dollars)*
| Sensitivity analysis scenario† | Cost-effectiveness ratios |
||||
|---|---|---|---|---|---|
| Life year gained (LYG)‡ | QALY gained‡ | Incremental costs | Cost/LYG ($) | Cost/QALY ($) | |
| Base-case analysis | 0.31 | 0.19 | 1,700 | 5,428 | 8,801 |
| Age-group when diagnosed with diabetes (years) | |||||
| 35–44 | 0.37 | 0.22 | 1,999 | 5,415 | 8,943 |
| 45–54 | 0.38 | 0.24 | 2,033 | 5,283 | 8,619 |
| 55–64 | 0.35 | 0.21 | 1,837 | 5,311 | 8,557 |
| 65–74 | 0.26 | 0.16 | 1,490 | 5,762 | 9,201 |
| ≥75 | 0.13 | 0.08 | 787 | 6,201 | 9,890 |
| Sex | |||||
| Male§ | 0.36 | 0.23 | 1,329 | 3,685 | 5,752 |
| Female§ | 0.27 | 0.16 | 2,237 | 8,239 | 13,833 |
| Effectiveness of aspirin | |||||
| Primary on CHD (RR 0.82) | |||||
| +95% CI (0.90) | 0.25 | 0.15 | 1,700 | 6,894 | 11,289 |
| −95% CI (0.75) | 0.37 | 0.23 | 1,703 | 4,555 | 7,342 |
| Secondary on CHD (RR 0.80) | |||||
| +95% CI (0.88) | 0.37 | 0.23 | 2,243 | 5,998 | 9,796 |
| −95% CI (0.73) | 0.25 | 0.16 | 1,128 | 4,526 | 7,258 |
| Side effect | |||||
| Total stroke (RR 0.95) | |||||
| +95% CI (0.85) | 0.31 | 0.19 | 1,734 | 5,590 | 9,088 |
| −95% CI (1.06) | 0.30 | 0.18 | 1,821 | 6,032 | 9,882 |
| Gastrointestinal bleeding (excess risk 0.03%) | |||||
| +95% CI (0.05%) | 0.31 | 0.19 | 1,714 | 5,481 | 8,890 |
| −95% CI (0.02%) | 0.31 | 0.19 | 1,694 | 5,402 | 8,757 |
| Diabetes subgroup‖ | 0.26 | 0.16 | 1,567 | 6,056 | 9,783 |
| Men with diabetes‖ | 0.55 | 0.35 | 1,282 | 2,344 | 3,633 |
| Women with diabetes‖ | 0.11 | 0.07 | 1,492 | 13,207 | 22,259 |
| Secondary prevention only | 0.16 | 0.10 | 1,754 | 10,841 | 18,348 |
| Cost of gastrointestinal bleeding ($) | |||||
| 7,800 | |||||
| 4,500 | 0.31 | 0.19 | 1,690 | 5,394 | 8,746 |
| 10,200 | 0.31 | 0.19 | 1,708 | 5,452 | 8,840 |
| A1C and blood pressure control goals | |||||
| Intensive glycemic control + intensive hypertension control | |||||
| Standard glycemic control + intensive hypertension control | 0.33 | 0.20 | 1,661 | 5,005 | 8,240 |
| Intensive glycemic control + standard hypertension control | 0.31 | 0.19 | 1,750 | 5,630 | 9,203 |
| Standard glycemic control + standard hypertension control | 0.33 | 0.20 | 1,718 | 5,220 | 8,685 |
| Effectiveness limited in the trial period (aspirin treatment lifetime) | 0.09 | 0.06 | 621 | 6,703 | 10,669 |
| Effectiveness limited to the trial period (aspirin use for 5 years) | 0.09 | 0.06 | 451 | 4,867 | 7,746 |
| Compliance rate (%) | |||||
| 100 | |||||
| 78 | 0.24 | 0.15 | 1,314 | 5,420 | 8,787 |
| 56 | 0.17 | 0.11 | 935 | 5,412 | 8,773 |
| Modeling ischemic and hemorrhagic stroke separately | 0.29 | 0.18 | 2,921 | 9,973 | 16,484 |
*Costs, LYGs, and QALYs are discounted at 3% annually;
†the bolded text and numbers showed the base-case scenario;
‡rounding to the nearest hundredth;
§parameters are from ATT study; RRs: Men: primary prevention of CHD 0.77, ischemic stroke 1.01, secondary prevention of CHD 0.81; women: primary prevention of CHD 0.95, ischemic stroke 0.77, secondary prevention of CHD 0.73.
‖parameters are from the study by De Berardis et al. RRs: overall: primary prevention of CHD 0.90, stroke 0.83, secondary prevention of CHD 0.80, gastrointestinal bleeding (excess risk: 0.03%); men: primary prevention of CHD 0.57, stroke 1.11, secondary prevention of CHD 0.8; women: primary prevention of CHD 1.08, stroke 0.75, secondary prevention of CHD 0.8.
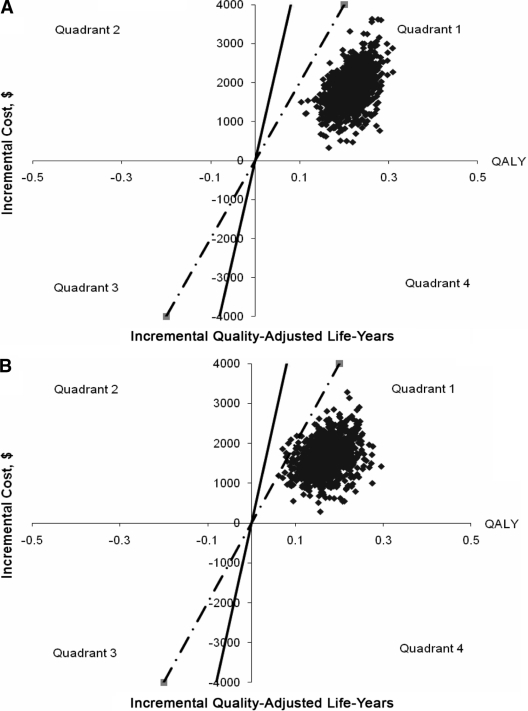
Figure 1A and B show the ICER plot from the probabilistic sensitivity analysis of the cost-effectiveness of aspirin using parameters in the general population as in the ATT study (14) and parameters in diabetes subgroup as in De Berardis et al. (13) study. Using the ATT study parameters, 100% of the realizations yielded an ICER of <$16,000/QALY gained. The 2.5th and 97.5th percentiles were $5,520 and $12,600 per QALY gained, respectively (Fig. 1A). Using parameters in De Berardis et al. (13) study, all of the 1,000 simulations yielded an ICER <$27,000 per QALY gained. The 2.5th and 97.5th percentiles were $4,916 and $16,680 per additional QALY gained, respectively (Fig. 1B).
Figure 1.
Results of the probabilistic sensitivity analyses for the cost-effectiveness of aspirin use in newly diagnosed type 2 diabetes. A: Using parameters for general population in the ATT study. B: Using parameters for diabetes subgroup in the meta-analysis by De Berardis et al. (13). Plot of incremental cost versus incremental QALYs for aspirin use versus no aspirin use. Each dot on the graph represents one ICER from one of the 1,000 iterations. Solid line represents ICER = $50,000/QALY; dotted line represents ICER = $20,000/QALY. Dots on the right of the lines mean that the ICERS are less than the ICER the line represents. Dots in quadrant 1 show that the intervention is more effective and less costly; dots in quadrant 4 show that the intervention is cost saving.
CONCLUSIONS
Our study showed that regular use of aspirin in people with newly diagnosed type 2 diabetes over their lifetime cost $8,801 per QALY gained. Medicare and Medicaid programs cover many drugs and medical technologies with much higher ICERs than our estimated ICERs for aspirin (20). If we use the conventional $50,000/QALY as the threshold for cost-effectiveness, aspirin use is a very cost-effective intervention for people with newly diagnosed diabetes. Both one-way and probabilistic sensitivity analyses showed that the baseline results were robust. All the ICERs in one-way sensitivity analyses were below $25,000/QALY. There is near certainty that the ICER of aspirin use for primary prevention is <$30,000 per QALY, whether parameters come from the ATT study or the De Berardis et al. meta-analysis.
Our study reported higher ICERs of aspirin use for primary prevention of CVD in people with diabetes than in members of the general population who have a similar risk for CHD or stroke. For example, Pignone et al. (5) reported that aspirin use was cost saving in men with a 10-year risk of CHD of 25%; our study reported an ICER of $5,752/QALY for men with slightly higher risk of CHD (28%). For women, Pignone et al. (6) reported an ICER of $2,532/QALY in women with a 10-year stroke risk of 5.5% and predicted an even lower ICER for women with higher risk for stroke. In our study, the ICER was $13,833/QALY for women with an average 10-year risk of 8.7% for stroke.
Some have postulated that aspirin use might be cost saving in people with diabetes (21). Our results did not support this. There are three possible reasons. First, aspirin's effect on gastrointestinal bleeding increased the total medical costs of the group taking aspirin. Second, the aspirin treatment group lived longer and required additional resources for treatment of diabetes and hypertension. Our study results showed that the treatment cost for glycemic and hypertension control was $1,411 higher in the group taking aspirin than the group not taking aspirin (Table 2). Third, aspirin treatment affects diabetes macrovascular complications but not microvascular ones. Those receiving aspirin therapy live longer due to reduced risk of CHD and therefore are more likely to develop diabetic microvascular complications later in life. We found that the cumulative incidence of other diabetes complications (i.e., end-stage renal disease, nephropathy, blindness, and lower-extremity amputations) at year 10 were similar in both the aspirin and nonaspirin groups. However, the lifetime cumulative incidence of these complications was higher in the aspirin group, indicating a total excess risk of 0.87% in men and 0.66% in women. However, our results are consistent with results previously reported by Gaspoz et al. (21) and Kahn et al. (22) on the cost-effectiveness of aspirin use in secondary prevention of CVD.
Our study has several limitations. First, the effectiveness of aspirin use for people with diabetes needs to be further demonstrated by large clinical trials. The difference in the effects of aspirin used as primary prevention of CVD in people with and without diabetes is debated (23). The recently published Prevention of Progression of Arterial Disease and Diabetes Trial in the U.K. and the Japanese Primary Prevention of Atherosclerosis With Aspirin for Diabetes trials (24,25) reported that aspirin did not reduce the risk of cardiovascular events. However, questions about aspirin effectiveness remain, and two additional trials are underway to address the issue of aspirin use for CVD prevention in people with diabetes (14). Our cost-effectiveness analysis of the aspirin therapy is subject to change, pending results from ongoing clinical trials. Second, although our cost-effectiveness model was validated against clinical trials, it, like all models, is based on simplifying assumptions. However, we have tried to make our assumptions transparent and performed sensitivity analyses to show the impact of our assumptions.
Our study shows that regular aspirin use appears to be very cost-effective in people aged ≥40 years with newly diagnosed type 2 diabetes. However, use of aspirin in primary prevention is still controversial. Future clinical trials are needed to better understand if aspirin is efficacious for people with type 2 diabetes. Additional cost-effectiveness analyses, accounting for these studies, might be needed.
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1. Cull CA, Neil HAW, Holman RR: Changing aspirin use in patients with type 2 diabetes in the UKPDS. Diabet Med 2004;21:1368–1371 [DOI] [PubMed] [Google Scholar]
- 2. Antithrombotic Trialists Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. Br J Med 2002;324:71–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. U.S. Preventive Services Task Force. Aspirin for the primary prevention of cardiovascular events: recommendation and rationale. Ann Intern Med 2002;136:157–160 [DOI] [PubMed] [Google Scholar]
- 4. American Diabetes Association. Aspirin therapy in diabetes. Diabetes Care 2000;23(Suppl. 1):S61–S62 [PubMed] [Google Scholar]
- 5. Pignone M, Earnshaw S, Tice JA, Pletcher MJ: Aspirin, statins, or both drugs for the primary prevention of coronary heart disease events in men: a cost-utility analysis. Ann Intern Med 2006;144:326–336 [DOI] [PubMed] [Google Scholar]
- 6. Pignone M, Earnshaw S, Pletcher MJ, Tice JA: Aspirin for the primary prevention of cardiovascular disease in women, a cost-utility analysis. Arch Intern Med 2007;167:290–295 [DOI] [PubMed] [Google Scholar]
- 7. CDC Diabetes Cost-effectiveness Group. Cost-effectiveness of intensive glycemic control, intensified hypertension control, and serum cholesterol level reduction for type 2 diabetes. JAMA 2002;287:2542–2551 [DOI] [PubMed] [Google Scholar]
- 8. Hoerger TJ, Harris R, Hicks KA, Donahue K, Sorensen S, Engelgau M: Screening for type 2 diabetes mellitus: a cost-effectiveness analysis. Ann Intern Med 2004;140:689–699 [see comment] [DOI] [PubMed] [Google Scholar]
- 9. Eastman RC, Javitt JC, Herman WH, Dasbach EJ, Abrozek AS, Dong F, Manninen D, Garfield SA, Copley-Merriman C, Maier W, Eastman JF, Kotsanos J, Cowie CC, Harris M: Model of complications for NIDDM, I: model construction and assumptions. Diabetes Care 1997;20:725–734 [DOI] [PubMed] [Google Scholar]
- 10. Eastman RC, Javitt JC, Herman WH, Dasbach EJ, Zbrozek AS, Dong F, Manninen D, Garfield SA, Copley-Merriman C, Maier W, Eastman JF, Kotsanos J, Cowie CC, Harris M: Model of complications of NIDDM: II. model construction and assumptions. Diabetes Care 1997;20:735–744 [DOI] [PubMed] [Google Scholar]
- 11. Weinstein MC, Coxson PG, Williams LW, Pass TM, Stason WB, Goldman L: Forecasting coronary heart disease incidence, mortality, and cost: the coronary heart disease policy model. Am J Public Health 1987;77:1417–1426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. American Diabetes Association Consensus Panel: Guidelines for computer modeling of diabetes and its complications. Diabetes Care 2004;27:2262–2265 [DOI] [PubMed] [Google Scholar]
- 13. De Berardis G, Sacco M, Strippoli GFM, Pellegrini F, Graziano G, Tognoni G, Nicolucci A: Aspirin for primary prevention of cardiovascular events in people with diabetes:meta-analysis of randomised controlled trials. Br J Med 2010;339:b4531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Antithrombotic Trialists (ATT) Collaboration. Aspirin in the primary and secondary prevention of vascular disease:collaborative meta-analysis of individual participant data from randomised trials. Lancet 2009;373:1849–1860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Brandle Ml, Zhou H, Smith BR, Marriott D, Burke R, Tabaei BP, Brown MB, Herman WH: The direct medical cost of type 2 diabetes. Diabetes Care 2003;26:2300–2304 [DOI] [PubMed] [Google Scholar]
- 16. Hoerger TJ: Using costs in cost-effectiveness models for chronic diseases. Med Care 2009;47(Suppl. 1):S21–S27 [DOI] [PubMed] [Google Scholar]
- 17. Coffey JT, Zhou H, Burke MR, Tabaei BP, Engelgau MM, Kaplan RM, Herman WH: Valuing health-related quality of life in diabetes. Diabetes Care 2002;25:2238–2243 [DOI] [PubMed] [Google Scholar]
- 18. Augustovski FA, Cantor SB, Thach CT, Spann SJ: Aspirin for primary prevention of cardiovascular events. J Gen Intern Med 1998;13:824–835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Saaddine JB, Cadwell B, Gregg EW, Engelgau MM, Vinicor F, Imperatore G, Narayan KM: Improvements in diabetes processes of care and intermediate outcomes: United States, 1988–2002. Ann Intern Med 2006;144:465–474 [DOI] [PubMed] [Google Scholar]
- 20. Laupacis A, Deeny D, Detsky AS, Tugwell PX: How attractive does a new technology have to be to warrant adoption and utilization? Tentative guidelines for using clinical and economic evaluations. Can Med Assoc J 1992;146:473–481 [PMC free article] [PubMed] [Google Scholar]
- 21. Gaspoz J-M, Goxson PG, Goldman PA, Williams LW, Kuntz KM, Hunink M: Cost effectiveness of aspirin, clopidogrel, or both fro secondary prevention of coronary heart disease. N Engl J Med 2002;346:1800–1806 [DOI] [PubMed] [Google Scholar]
- 22. Kahn R, Robertson RM, Smith R, Eddy D: The impact of prevention on reducing the burden of cardiovascular disease. Circulation 2008;118 [DOI] [PubMed] [Google Scholar]
- 23. Woods RL, Tonkin AM, Nelson MR, Britt HC, Reid CM: Should aspirin be used for the primary prevention of cardiovascular disease in people with diabetes? Med J Australia 2009;190:614–615 [DOI] [PubMed] [Google Scholar]
- 24. Belch J, MacCuish A, Campbell I: The prevention of progression of arterial disease and diabetes (POPADAD) trial: factorial randomised placebo controlled trial of aspirin and antioxidants in patients with diabetes and asymptomatic peripheral arterial disease. Br J Med 2008;337:a1840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ogawa H, Nakayama M, Marimato T, Uemura S, Kanauchi M, Doi N, Jinnonchi H, Sugiyamak S, Saito Y: low-dose aspirin for primary prevention of atherosclerotic events in patients with type 2 diabetes: a randomized controlled trial. JAMA 2008;300:2134–2141 [DOI] [PubMed] [Google Scholar]