Abstract
OBJECTIVE
To evaluate efficacy and safety of switching from twice-daily exenatide to once-daily liraglutide or of 40 weeks of continuous liraglutide therapy.
RESEARCH DESIGN AND METHODS
When added to oral antidiabetes drugs in a 26-week randomized trial (Liraglutide Effect and Action in Diabetes [LEAD]-6), liraglutide more effectively improved A1C, fasting plasma glucose, and the homeostasis model of β-cell function (HOMA-B) than exenatide, with less persistent nausea and hypoglycemia. In this 14-week extension of LEAD-6, patients switched from 10 μg twice-daily exenatide to 1.8 mg once-daily liraglutide or continued liraglutide.
RESULTS
Switching from exenatide to liraglutide further and significantly reduced A1C (0.32%), fasting plasma glucose (0.9 mmol/l), body weight (0.9 kg), and systolic blood pressure (3.8 mmHg) with minimal minor hypoglycemia (1.30 episodes/patient-year) or nausea (3.2%). Among patients continuing liraglutide, further significant decreases in body weight (0.4 kg) and systolic blood pressure (2.2 mmHg) occurred with 0.74 episodes/patient-year of minor hypoglycemia and 1.5% experiencing nausea.
CONCLUSIONS
Conversion from exenatide to liraglutide is well tolerated and provides additional glycemic control and cardiometabolic benefits.
Glucagon-like peptide (GLP)-1 receptor agonists improve glycemic control and reduce weight with minimal risk of hypoglycemia (1,2). The first randomized head-to-head comparison of two GLP-1 receptor agonists added to oral antidiabetes agents (Liraglutide Effect and Action in Diabetes [LEAD]-6) showed that 1.8 mg once-daily liraglutide provided greater improvements in A1C and fasting plasma glucose (FPG) with lower hypoglycemia and less persistent nausea than 10 μg twice-daily exenatide after 26 weeks; similar decreases in weight (∼3 kg) and systolic blood pressure (SBP) (2.0–2.5 mmHg) occurred with both drugs (3). The objectives of this 14-week extension were to assess the safety and efficacy of switching from exenatide to liraglutide, or continuing liraglutide for up to 40 weeks.
RESEARCH DESIGN AND METHODS
The LEAD-6 design has been reported (3). Adults with type 2 diabetes inadequately controlled (A1C 7–11%) with maximally tolerated stable doses of metformin, sulfonylurea, or both for ≥3 months were randomized (1:1) to 1.8 mg liraglutide once daily or 10 μg exenatide twice daily. After 26 weeks, patients continued into a nonrandomized 14-week extension: all exenatide patients were switched to 0.6 mg liraglutide once daily for 1 week, then escalated to 1.2 mg for another week, and then given a final maintenance dose of 1.8 mg. Patients originally randomized to 1.8 mg liraglutide continued. Background oral antidiabetes drugs remained unchanged, although sulfonylurea doses could be decreased by 50% if unacceptable hypoglycemia occurred.
Visits occurred at weeks −2 (screening), 0 (randomization), 4, 8, 12, 20, 26, 34, and 40 for both groups. Efficacy and safety assessments during the extension phase (weeks 26–40) were identical to those previously described (3). Extension intention-to-treat (ITT) (all randomized patients exposed to trial product who entered the extension) and extension safety (all patients exposed to trial product who entered the extension) populations were used for efficacy and safety analyses, respectively. Changes from baseline (last available observation up to 26 weeks) to week 40 within each treatment group were analyzed by paired t tests. Treatment groups were not compared. Post-baseline missing values were imputed using last observation carried forward. Unless noted, mean (±SE) values are presented. Significance was P < 0.05.
RESULTS
All 389 patients completing 26 weeks entered the extension. Three patients who were not formally randomized were excluded from the extension ITT population. Demographics were well matched between groups and similar to those previously reported (3). Overall, 376 of 389 patients (97%) completed the extension: 10 of 187 (5.3%) with exenatide liraglutide and 3 of 202 (1.5%) continuing liraglutide withdrew. Withdrawals (n [%]) in the exenatide
liraglutide and 3 of 202 (1.5%) continuing liraglutide withdrew. Withdrawals (n [%]) in the exenatide liraglutide and liraglutide groups, respectively, were due to either adverse events (6 [3.2%] and 0), ineffective therapy (0 and 2 [1.0%]), protocol noncompliance (0 and 1 [0.5%]), meeting withdrawal criteria (1 [0.5%] and 0), or other reasons (3 [1.6%] and 0). Demographic and screening characteristics were similar between patients who withdrew during the extension and those who completed the extension, with the exception of mean duration of diabetes, which was longer for those withdrawing (12.2 years) than completers (7.9 years).
liraglutide and liraglutide groups, respectively, were due to either adverse events (6 [3.2%] and 0), ineffective therapy (0 and 2 [1.0%]), protocol noncompliance (0 and 1 [0.5%]), meeting withdrawal criteria (1 [0.5%] and 0), or other reasons (3 [1.6%] and 0). Demographic and screening characteristics were similar between patients who withdrew during the extension and those who completed the extension, with the exception of mean duration of diabetes, which was longer for those withdrawing (12.2 years) than completers (7.9 years).
Efficacy
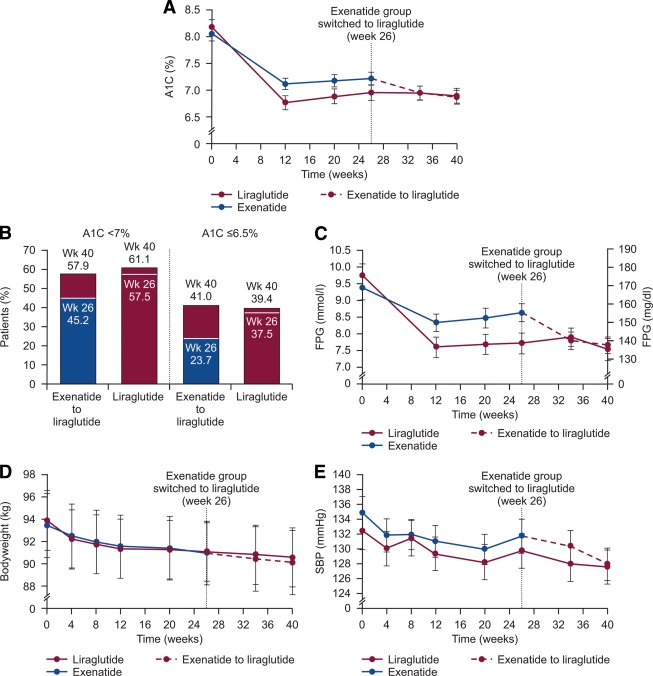
Mean A1C further decreased from 7.2% at week 26 to 6.9% at week 40 (−0.32 ± 0.043%; P < 0.0001) after switching from exenatide to liraglutide, but remained similar with continued liraglutide (7.0 to 6.9%; −0.06 ± 0.041%, P = 0.1222) (Fig. 1A). Additional patients reached A1C targets after switching from exenatide to liraglutide (Fig. 1B).
Figure 1.
Effect of switching from exenatide to liraglutide or continuing liraglutide on various measures of efficacy (extension ITT population). A: A1C over time. B: Percentage of patients reaching A1C targets at week 26 (after the main part of the trial) and week 40 (after the exenatide group switched to liraglutide for 14 weeks). C: FPG over time. D: Body weight over time. E: SBP over time. All patients originally in the exenatide group switched to liraglutide at week 26, whereas the liraglutide group continued liraglutide. Maroon represents liraglutide and blue exenatide. In B, the white line within each bar indicates the percentage of patients reaching A1C targets at week 26 and the top of the bar indicates the percentage reaching A1C targets at week 40. In A and C–E, dotted maroon lines indicate patients who switched from exenatide to liraglutide at week 26. Values are mean (±2 SE). Post-baseline timepoints were imputed using last observation carried forward.
After switching from exenatide to liraglutide, further reductions in FPG (Fig. 1C; −0.9 ± 0.16 mmol/l, P < 0.0001), body weight (Fig. 1D; −0.9 ± 0.15 kg, P < 0.0001), and SBP (Fig. 1E; −3.8 ± 0.84 mmHg, P < 0.0001) occurred while the homeostasis model of β-cell function (HOMA-B) assessment increased (14.5 ± 4.4%, P = 0.001), consistent with the FPG reductions. In patients continuing liraglutide, reductions in FPG (Fig. 1C; −0.2 ± 0.11 mmol/l, P = 0.0973), body weight (Fig. 1D, −0.4 ± 0.15 kg, P = 0.0089), and SBP (Fig. 1E; −2.2 ± 0.88 mmHg, P = 0.0128) occurred. No significant changes in postprandial glucose (except after lunch with exenatide liraglutide [−0.64 ± 0.21 mmol/l, P = 0.0032], diastolic blood pressure, fasting insulin, fasting C-peptide, proinsulin-to-insulin ratio, or homeostasis model assessment–insulin resistance [HOMA-IR]) occurred in either group.
liraglutide [−0.64 ± 0.21 mmol/l, P = 0.0032], diastolic blood pressure, fasting insulin, fasting C-peptide, proinsulin-to-insulin ratio, or homeostasis model assessment–insulin resistance [HOMA-IR]) occurred in either group.
Safety
Similar numbers of patients reported one or more adverse events during the extension (exenatide liraglutide: 70 [37.4%] and liraglutide: 76 [37.6%]). Most adverse events were mild in severity (exenatide
liraglutide: 70 [37.4%] and liraglutide: 76 [37.6%]). Most adverse events were mild in severity (exenatide liraglutide: 79/117 events, liraglutide: 81/120 events); investigators assessed most as unrelated to trial drug (exenatide
liraglutide: 79/117 events, liraglutide: 81/120 events); investigators assessed most as unrelated to trial drug (exenatide liraglutide: 72/117 events, liraglutide: 94/120 events).
liraglutide: 72/117 events, liraglutide: 94/120 events).
Nausea and diarrhea occurred in 3.2% of patients switching from exenatide liraglutide and 1.5% in those continuing liraglutide, whereas vomiting occurred in 0.5% switching from exenatide
liraglutide and 1.5% in those continuing liraglutide, whereas vomiting occurred in 0.5% switching from exenatide liraglutide and 2.0% in those continuing liraglutide.
liraglutide and 2.0% in those continuing liraglutide.
One major hypoglycemic episode occurred in a patient continuing liraglutide, while extension rates (episodes/patient-year) of minor hypoglycemia were 1.30 (exenatide liraglutide), down from 2.60 with exenatide at week 26 (3), and 0.74 (liraglutide). Thirteen adverse events associated with withdrawal from the extension of six patients in the exenatide
liraglutide), down from 2.60 with exenatide at week 26 (3), and 0.74 (liraglutide). Thirteen adverse events associated with withdrawal from the extension of six patients in the exenatide liraglutide group were myocardial infarction, diarrhea (three events), impaired gastric emptying, eructation, nausea, lethargy, paraesthesia, anxiety, depressed mood, depression, and dyspnea. For two of these six patients, the adverse events associated with their withdrawal from the extension (nausea and diarrhea) had been previously reported as separate events during the 26-week exenatide treatment period.
liraglutide group were myocardial infarction, diarrhea (three events), impaired gastric emptying, eructation, nausea, lethargy, paraesthesia, anxiety, depressed mood, depression, and dyspnea. For two of these six patients, the adverse events associated with their withdrawal from the extension (nausea and diarrhea) had been previously reported as separate events during the 26-week exenatide treatment period.
Four patients in the exenatide liraglutide group had seven severe adverse events (cardiac failure, myocardial infarction, cataract, chest discomfort, chronic obstructive pulmonary disease [two events], dyspnea). Five patients continuing liraglutide had eight severe adverse events (cerebral infarction, cerebrovascular accident, transient ischemic attack, acute coronary syndrome, coronary artery occlusion, portal vein thrombosis, rectal cancer, and depression). Two deaths occurred (exenatide
liraglutide group had seven severe adverse events (cardiac failure, myocardial infarction, cataract, chest discomfort, chronic obstructive pulmonary disease [two events], dyspnea). Five patients continuing liraglutide had eight severe adverse events (cerebral infarction, cerebrovascular accident, transient ischemic attack, acute coronary syndrome, coronary artery occlusion, portal vein thrombosis, rectal cancer, and depression). Two deaths occurred (exenatide liraglutide: myocardial infarction after 198 days of treatment; liraglutide: cerebral infarction [patient completed the study but died shortly after]). Investigators assessed all events as “unlikely” to be related to trial product.
liraglutide: myocardial infarction after 198 days of treatment; liraglutide: cerebral infarction [patient completed the study but died shortly after]). Investigators assessed all events as “unlikely” to be related to trial product.
Calcitonin levels remained at the lower level of the normal range (<1 pg/ml) and did not differ between groups. No medullary thyroid carcinoma or pancreatitis cases were reported during the extension.
CONCLUSIONS
This extension shows that patients can be simply and safely switched from twice-daily premeal exenatide to meal-independent once-daily liraglutide using weekly dose escalation from 0.6 to 1.2 to 1.8 mg. Conversion to liraglutide from exenatide was well tolerated and further improved glycemic control. Additional reductions in body weight and SBP occurred in both groups. Over 40 weeks, liraglutide reduced A1C by 1.3%.
The magnitude of these changes and differences between liraglutide and exenatide are consistent with results reported in phase 3 LEAD (liraglutide) (3–8) and exenatide (9–11) trials. The greater efficacy of liraglutide may be due to sustained levels achieved over 24 h by once-daily dosing compared with biphasic levels achieved during the 2.4-h half-life of exenatide after dosing within 1 h of breakfast and dinner (12).
Further studies are required to investigate the durability of these responses. Given the likely preference for once-daily meal-independent dosing, liraglutide appears to be a useful addition to the diabetes treatment armamentarium.
Supplementary Material
Acknowledgments
J.B.B.'s employer, the University of North Carolina, has contracted for his effort as an investigator and consultant with numerous companies, including the following: Amylin, Bristol-Myers Squibb, Eli Lilly, GlaxoSmithKline, Hoffman-La Roche, Merck, Novartis, Novo Nordisk, Pfizer, sanofi-aventis, and Wyeth. G.S. has been a consultant or attended speakers' bureau for Novo-Nordisk, Eli Lilly, Merck, Novartis, Servier, GlaxoSmithKline, and sanofi-aventis. W.E.S. has received research grants from, served on advisory boards for, and/or has been a member of speaker's bureaus for Novo Nordisk, Lilly, Amylin, Roche, Merck Sharp & Dohme, Berlin Chemie, Novartis, Astra Zeneca, Takeda, Bristol-Myers Squibb, and sanofi-aventis. E.M. has attended advisory panels for Merck Sharp & Dohme, Novartis, Novo Nordisk, and sanofi-aventis and has received research support from Novo Nordisk. C.-T.C. and Y.X. are employees of Novo Nordisk. L.B. has acted as an investigator for Amylin Pharmaceuticals, AstraZeneca, Boehringer-Ingelheim Pharmaceutical, Bristol-Myers Squibb, Eli Lilly, MannKind Corporation, Merck, Novo Nordisk, Novartis Corporation, Pfizer, and sanofi-aventis; has been a speaker for Abbott, Amylin Pharmaceuticals, AstraZeneca, Bristol-Myers Squibb, Daiichi Sankyo, Eli Lilly, GlaxoSmithKline, LifeScan, Merck, Novartis, Novo Nordisk, Pfizer, and sanofi-aventis; and has acted as a consultant for Boehringer-Ingelheim Pharmaceutical and Hazlozyme. J.R. has served on advisory boards and received honorarium or consulting fees from Pfizer, Roche, sanofi-aventis, Novo Nordisk, Eli Lilly, MannKind, GlaxoSmithKline, Takeda, Daiichi Sankyo, Forest, Johnson & Johnson, Novartis, Boehringer Ingelheim, and Amylin. He has received research grants from Merck, Pfizer, sanofi-aventis, Novo Nordisk, Roche, Bristol-Myers Squibb, Eli Lilly, Forest, GlaxoSmithKline, Takeda, Novartis, AstraZeneca, Amylin, Johnson & Johnson, Daiichi Sankyo, MannKind, and Boehringer Ingelheim. No other potential conflicts of interest relevant to this article were reported.
This study was presented in poster form at the 69th Scientific Sessions of the American Diabetes Association, New Orleans, Louisiana, 5–9 June 2009.
The authors gratefully acknowledge the LEAD-6 study group, their staff, clinical trial personnel, and the patients for participating in the study. The authors thank Jen Faleska, PhD, and John Smith, PhD, from Novo Nordisk for writing assistance. Artwork and administrative support was provided by Watermeadow Medical, funded by Novo Nordisk.
Footnotes
Clinical trial reg. no. NCT00518882, clinicaltrials.gov.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1. Horton ES: Can newer therapies delay the progression of type 2 diabetes mellitus? Endocr Pract 2008;14:625–638 [DOI] [PubMed] [Google Scholar]
- 2. Pratley RE, Gilbert M: Targeting incretins in type 2 diabetes: role of GLP-1 receptor agonists and DPP-4 inhibitors. Rev Diabet Stud 2008;5:73–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Buse JB, Rosenstock J, Sesti G, Schmidt WE, Montanya E, Brett JH, Zychma M, Blonde L: LEAD-6 Study Group. Liraglutide once a day versus exenatide twice a day for type 2 diabetes: a 26-week randomised, parallel-group, multinational, open-label trial (LEAD-6). Lancet 2009;374:39–47 [DOI] [PubMed] [Google Scholar]
- 4. Garber A, Henry R, Ratner R, Garcia-Hernandez PA, Rodriguez-Pattzi H, Olvera-Alvarez I, Hale PM, Zdravkovic M, Bode B: LEAD-3 (Mono) Study Group. Liraglutide versus glimepiride monotherapy for type 2 diabetes (LEAD-3 Mono): a randomised, 52-week, phase III, double-blind, parallel-treatment trial. Lancet 2009;373:473–481 [DOI] [PubMed] [Google Scholar]
- 5. Marre M, Shaw J, Brändle M, Bebakar WM, Kamaruddin NA, Strand J, Zdravkovic M, Le Thi TD, Colagiuri S: LEAD-1 SU Study Group. Liraglutide, a once-daily human GLP-1 analogue, added to a sulphonylurea over 26 weeks produces greater improvements in glycaemic and weight control compared with adding rosiglitazone or placebo in subjects with type 2 diabetes (LEAD-1 SU). Diabet Med 2009;26:268–278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nauck M, Frid A, Hermansen K, Shah NS, Tankova T, Mitha IH, Zdravkovic M, Düring M, Matthews DR: LEAD-2 Study Group. Efficacy and safety comparison of liraglutide, glimepiride, and placebo, all in combination with metformin, in type 2 diabetes: the LEAD (Liraglutide Effect and Action in Diabetes)-2 study. Diabetes Care 2009;32:84–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zinman B, Gerich J, Buse JB, Lewin A, Schwartz S, Raskin P, Hale PM, Zdravkovic M, Blonde L: LEAD-4 Study Investigators. Efficacy and safety of the human GLP-1 analog liraglutide in combination with metformin and TZD in patients with type 2 diabetes mellitus (LEAD-4 Met+TZD). Diabetes Care 2009;32:1224–1230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Russell-Jones D, Vaag A, Schmitz O, Sethi BK, Lalic N, Antic S, Zdravkovic M, Ravn GM, Simó R: Liraglutide Effect and Action in Diabetes 5 (LEAD-5) met+SU Study Group. Liraglutide vs insulin glargine and placebo in combination with metformin and sulfonylurea therapy in type 2 diabetes mellitus (LEAD-5 met+SU): a randomised controlled trial. Diabetologia 2009;52:2046–2055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Buse JB, Henry RR, Han J, Kim DD, Fineman MS, Baron AD: Exenatide-113 Clinical Study Group. Effects of exenatide (exendin-4) on glycemic control over 30 weeks in sulfonylurea-treated patients with type 2 diabetes. Diabetes Care 2004;27:2628–2635 [DOI] [PubMed] [Google Scholar]
- 10. DeFronzo RA, Ratner RE, Han J, Kim DD, Fineman MS, Baron AD: Effects of exenatide (exendin-4) on glycemic control and weight over 30 weeks in metformin-treated patients with type 2 diabetes. Diabetes Care 2005;28:1092–1100 [DOI] [PubMed] [Google Scholar]
- 11. Kendall DM, Riddle MC, Rosenstock J, Zhuang D, Kim DD, Fineman MS, Baron AD: Effects of exenatide (exendin-4) on glycemic control over 30 weeks in patients with type 2 diabetes treated with metformin and a sulfonylurea. Diabetes Care 2005;28:1083–1091 [DOI] [PubMed] [Google Scholar]
- 12. Rosenstock J, Gumprecht J, Szyprowska E, Bednarczyk-Kaluzny M, Zychma M, During M, Buse J: Pharmacokinetics of liraglutide vs. exenatide in type 2 diabetes: sustained vs. fluctuating concentrations over 24 hours (LEAD-6) (Abstract). Diabetes 2009;58(Suppl. 1):A150 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.