Abstract
OBJECTIVE
We used confirmatory factor analysis to test whether a single factor might explain the clustering of the metabolic syndrome (MS) components in children.
RESEARCH DESIGN AND METHODS
We studied 1,020 children aged 10–13 years from 20 schools in Cuenca, Spain. The single-factor model included: waist circumference (WC), fasting insulin, triglyceride to HDL cholesterol ratio (Triglyl/HDL-C), and mean arterial pressure (MAP). The standardized scores of the four variables in the model were used to develop a continuous MS index.
RESULTS
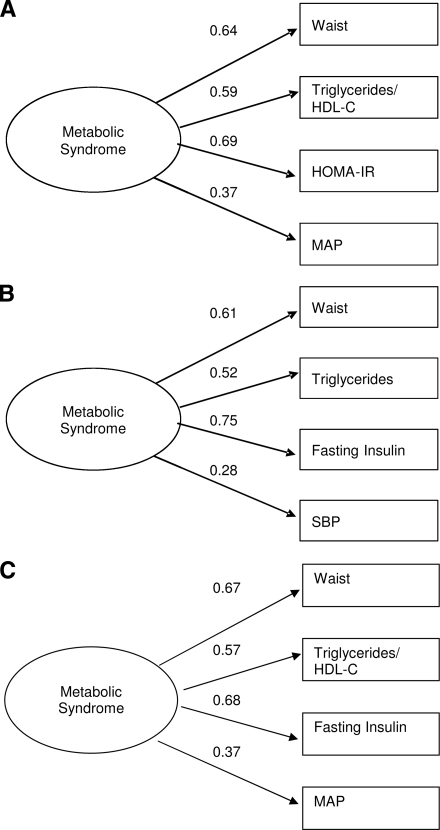
Factor loadings were 0.67 for WC, 0.68 for fasting insulin, 0.57 for Triglyl/HDL-C, and 0.37 for MAP. The single-factor model also showed a good fit to the data. As compared with Adult Treatment Panel III criteria, the MS index showed strong validity in the diagnosis of MS (area under the receiver operating characteristic curve = 0.98, 95% CI 0.96–0.99).
CONCLUSIONS
A single underlying factor has acceptable validity to represent MS in children.
Among children, classic cardiovascular risk factors tend to cluster into metabolic syndrome (MS). Whether the clustering of MS components is attributable to only one or to multiple determinants is a matter of debate (1). In adults, confirmatory factor analysis (CFA) studies have suggested that there are four factors underlying MS (2–4). In contrast, Pladevall et al. in adults (5), and Li and Ford in U.S. adolescents (6), observed that a single-factor model validly represented MS.
A single-factor model with a few clinically relevant variables could facilitate diagnosis of MS in children. Accordingly, we used CFA to test a single-factor model representing MS in children. This model includes a single variable for each of the four core components usually accepted in MS: waist circumference (WC) for abdominal obesity, fasting insulin for insulin resistance, triglyceride/HDL cholesterol ratio (Triglyl/HDL-C) for dyslipemia, and mean arterial pressure (MAP) for hypertension. In contrast to Pladevall et al. (7), who used the homeostasis model assessment of insulin resistance (HOMA-IR), we used fasting insulin because it can be a sensitive indicator of insulin resistance even in children without elevated glycemia. Furthermore, unlike Li and Ford's model (8), which only used triglycerides, ours also incorporates HDL-C because it has antithrombotic and antiplatelet effects, which influence cardiovascular risk within MS.
RESEARCH DESIGN AND METHODS
The study methods have been reported elsewhere (9). We studied 1,020 children aged 10–13 years from 20 schools in Cuenca, Spain. Anthropometry, blood pressure readings, and laboratory determinations were performed with standard procedures. Also, the Child Health and Illness Profile-Child Edition (CHIP-CE) questionnaire was used to assess physical activity (10). The Clinical Research Ethics Committee of the Virgen de la Luz Hospital in Cuenca approved the study protocol.
To examine the construct validity of our model for MS, and those of Pladevall et al. and of Li and Ford, we calculated the factor loadings of the variables in each model with AMOS 16.0 software (11). Factor loadings were required to be >0.3 and statistically significant (P < 0.05) to accept that any variable was part of the MS construct (12).
The χ2 test is prone to show a significant lack of model fit in studies with large sample size, so its results cannot be assessed in isolation. Also, the higher the comparative fit index (CFI) and the lower the root mean square residual (SRMR), the better the fit. A model was deemed to have a good fit when the CFI was >0.96 and the SRMR <0.08 (13).
Because the MS components are continuous variables, we estimated the likelihood of having MS with an MS index calculated as the sum of the standardized scores of the four variables comprising our model. We built a receiver operating characteristic (ROC) curve to obtain the sensitivity and specificity of the different cut-points for the MS index in the diagnosis of MS. As gold standard for MS, we used Adult Treatment Panel III criteria modified for age (14).
RESULTS
Figure 1 depicts the CFA results for the three single-factor MS models in our population. The goodness of fit was fairly good for the model by Pladevall et al. (Fig. 1A) and the model by Li and Ford (Fig. 1B). Yet for the latter, the factor loading of systolic blood pressure was below 0.3, indicating a poor validity. Our model displayed a somewhat better fit than that of Pladevall et al., and the factor loading of all variables was >0.3, indicating acceptable construct validity (Fig. 1C). Similar results were observed when fasting insulin was replaced by R-HOMA (factor loading: 0.67).
Figure 1.
Factor loading and goodness-of-fit indexes of one-factor models for the metabolic syndrome. A: Model proposed by Pladevall et al. (5): χ2 = 17.53, df = 2, P = 0.001; CFI = 0.97; and SRMR = 0.029. B: Model proposed by Li and Ford (9): χ2 = 5.40, df = 2, P = 0.067; CFI = 0.99; and SRMR = 0.018. C: Our model: χ2 = 14.3, df = 2, P = 0.001; CFI = 0.98; and SRMR=0.026. SBP, systolic blood pressure.
Our model also showed a good fit in each sex and physical activity group. The factor loading of the MS components did not differ between boys and girls (P = 0.682) or between active and sedentary children (P = 0.187).
The median of the MS index was −0.3 (range −8.349–9.64). No difference was observed in the mean MS index between boys (mean = −0.019) and girls (mean = −0.019; P = 0.998). In contrast, active children registered a lower MS index (mean = −0.355) than sedentary children (mean = 0.229; P < 0.001), validating the benefit of physical activity on the MS.
The area below the ROC curve was 0.98 (95% CI 0.96–0.99). The best cut point for the MS index was 4.2, with a sensitivity of 94.1% (95% CI 91.11–97.13) and a specificity of 93.5% (95% CI 93.46–93.58).
CONCLUSIONS
Our study may lead to improvements in the understanding and diagnosis of MS. First, it confirms that a single factor may underlie the MS construct in children and suggests that there could be some pattern of common causation for the core components of MS. Second, it provides an MS index that may be useful for identifying MS in children. To assist practicing physicians in obtaining immediate results based on crude patient data, we have developed a software application that gives the value of the child's MS index (15).
Our results must be confirmed in other populations and in children of different ages. In addition, future research should test if inflammatory and procoagulant variables, proposed components of MS, should be incorporated into the single-factor model of MS.
Acknowledgments
This study was funded mainly by La Consejería de Sanidad de Castilla-La Mancha (grant GC03060-00). Additional funding was obtained from the Instituto de Salud Carlos III, Red de Investigación en Actividades Preventivas y de Promoción de Salud (grant RD06/0018/0038).
No potential conflicts of interest relevant to this article were reported.
We thank the schools, families, and children for their enthusiastic participation in the study.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1. Steinberger J, Daniels SR, Eckel RH, Hayman L, Lustig RH, McCrindle B, Mietus-Snyder ML: Progress and challenges in metabolic syndrome in children and adolescents: a scientific statement from the American Heart Association Atherosclerosis, Hypertension, and Obesity in the Young Committee of the Council on Cardiovascular Disease in the Young; Council on Cardiovascular Nursing; and Council on Nutrition, Physical Activity, and Metabolism. Circulation 2009;119:628–647 [DOI] [PubMed] [Google Scholar]
- 2. Shen BJ, Goldberg RB, Llabre MM, Schneiderman N: Is the factor structure of the metabolic syndrome comparable between men and women and across three ethnic groups: the Miami Community Health Study. Ann Epidemiol 2006;16:131–137 [DOI] [PubMed] [Google Scholar]
- 3. Novak S, Stapleton LM, Litaker JR, Lawson KA: A confirmatory factor analysis evaluation of the coronary heart disease risk factors of metabolic syndrome with emphasis on the insulin resistance factor. Diabetes Obes Metab 2003;5:388–396 [DOI] [PubMed] [Google Scholar]
- 4. Shah S, Novak S, Stapleton LM: Evaluation and comparison of models of metabolic syndrome using confirmatory factor analysis. Eur J Epidemiol 2006;21:343–349 [DOI] [PubMed] [Google Scholar]
- 5. Pladevall M, Singal B, Williams LK, Brotons C, Guyer H, Sadurni J, Falces C, Serrano-Rios M, Gabriel R, Shaw JE, Zimmet PZ, Haffner S: A single factor underlies the metabolic syndrome: a confirmatory factor analysis. Diabetes Care 2006;29:113–122 [DOI] [PubMed] [Google Scholar]
- 6. Li C, Ford ES: Is there a single underlying factor for the metabolic syndrome in adolescents? A confirmatory factor analysis. Diabetes Care 2007;30:1556–1561 [DOI] [PubMed] [Google Scholar]
- 7. Oliveira AC, Oliveira AM, Almeida MS, Silva AM, Adan L, Ladeia AM: Alanine aminotransferase and high sensitivity C-reactive protein: correlates of cardiovascular risk factors in youth. J Pediatr 2008;152:337–342 [DOI] [PubMed] [Google Scholar]
- 8. Grundy SM: Metabolic syndrome: a multiplex cardiovascular risk factor. J Clin Endocrinol Metab 2007;92:399–404 [DOI] [PubMed] [Google Scholar]
- 9. Martínez Vizcaíno V, Salcedo Aguilar F, Franquelo Gutiérrez R, Solera Martínez M, Sánchez López M, Serrano Martínez S, López García E, Rodríguez Artalejo F: Assessment of an after-school physical activity program to prevent obesity among 9- to 10-year-old children: a cluster randomized trial. Int J Obes (Lond) 2008;32:12–22 [DOI] [PubMed] [Google Scholar]
- 10. Sánchez López M, Salcedo Aguilar F, Solera Martínez M, Moya Martínez P, Notario Pacheco B, Martínez Vizcaíno V: Physical activity and quality of life in schoolchildren aged 11–13 years of Cuenca, Spain. Scand J Med Sci Sports 2009;19:879–884 [DOI] [PubMed] [Google Scholar]
- 11. Byrne BM: Structural Equation Modeling with AMOS: Basic Concepts, Applications and Programming. 2nd ed. New York, Taylor and Francis Group, 2010. [Google Scholar]
- 12. Hillier TA, Rousseau A, Lange C, Lépinay P, Cailleau M, Novak M, Calliez E, Ducimetière P, Balkau B: Practical way to assess metabolic syndrome using a continuous score obtained from principal components analysis. Diabetologia 2006;49:1528–1535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hu L, Bentler PM: Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Structural Equation Modeling 1999;6:1–55 [Google Scholar]
- 14. Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH: Prevalence of a metabolic syndrome phenotype in adolescents: findings from the third National Health and Nutrition Examination Survey, 1988–1994. Arch Pediatr Adolesc Med 2003;157:821–827 [DOI] [PubMed] [Google Scholar]
- 15. The MOVI program. Social and Health Care Research Center, University of Castilla-La Mancha. Available from http://www.movidavida.org/sm. Accessed 4 January 2010