Abstract
OBJECTIVE
We aimed to establish optimal definitions for abdominal obesity and metabolic syndrome (MetS) among Andean adults.
RESEARCH DESIGN AND METHODS
Among 1,448 Andean adults, we assessed the relationship between waist circumference and subclinical vascular disease assessed by carotid intima-media thickness (cIMT) and manifest cardiovascular disease (M-CVD).
RESULTS
Optimal waist circumference cutoffs to classify individuals with abnormal cIMT or M-CVD were >97 and >87 cm in men and women, respectively. With these cutoffs, there was substantial disagreement between the original American Heart Association/National Heart, Lung and Blood Institute (AHA/NHLBI) and the recently updated MetS definition, particularly among men (κ = 0.85). Subjects with MetS identified by the updated definition but not meeting the original AHA/NHLBI MetS criteria demonstrated significantly increased cIMT (P < 0.001) compared with subjects who did not meet the MetS criteria by either definition.
CONCLUSIONS
Our findings support the use of ethnic-specific waist circumference cutoffs and the updated MetS definition in Andean adults.
In contrast to the third report of the expert panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults and the original American Heart Association/National Heart, Lung and Blood Institute (AHA/NHLBI) criteria for the diagnosis of metabolic syndrome (MetS) (1), the International Diabetes Federation (IDF) established abdominal obesity as a prerequisite for the diagnosis of MetS (2) and suggested ethnic-specific waist circumference cut points. A recent statement by IDF/NHLBI/AHA, World Heart Federation, International Atherosclerosis Society, and International Association for the Study of Obesity established an updated MetS definition (hereby referred to as the “updated definition”) based on ethnic-specific waist circumference cut points but not requiring the presence of abdominal obesity as long as at least three remainder components were present. In the absence of data from South Americans, waist circumference cut-points derived from South Asians were recommended (3), but it is unclear whether these are truly appropriate (3–6).
We aimed to determine: 1) the appropriate waist circumference cut points for defining abdominal obesity in Andean Hispanics; 2) the agreement between the presence of MetS diagnosed by original AHA/NHLBI versus updated criteria and resulting differences in MetS prevalence estimates; and 3) the relationship between both criteria and the presence of subclinical and manifest vascular disease.
RESEARCH DESIGN AND METHODS
The design and methods sections of the PREVENCION study have been previously published (7). The study included a large probabilistic sample of Andean Mestizos aged 20–80 years from Arequipa, Peru. The study was approved by the Santa Maria Catholic University Human Research Committee. Participants gave informed consent. Details regarding the original AHA/NHLBI and updated MetS definitions were previously published (3,8). In the updated MetS definition, abdominal obesity was defined using ethnic-specific waist circumference cut points derived from initial analyses in our study. Carotid intima-media thickness (cIMT) was measured with high-resolution carotid ultrasonography in the 1-cm proximal to the carotid bulb (9).
To define cut points for abnormal cIMT, we selected a reference sample (n = 472; 45.3% male) using the following exclusion criteria: (1) coronary heart disease, heart failure, stroke, peripheral vascular disease, or previous myocardial infarction; (2) systolic blood pressure ≥140 mmHg, diastolic blood pressure ≥90 mmHg, antihypertensive drug treatment; (3) diabetes (fasting blood glucose ≥126 mg/dl or pharmacologic treatment for diabetes); (4) LDL cholesterol >130 mg/dl; (5) lipid-lowering therapy; (6) current smoking; and (7) BMI ≥30 kg/m2.
Age-independent, sex-specific cIMT cut points were defined from the 95th percentiles of all men and women in the reference sample. Sex- and age-specific cIMT cut points for high cIMT were defined using curve-estimation procedures (R2 > 0.95) in reference participants based on 95th percentiles within each decade of life (10). Manifest cardiovascular disease (M-CVD) was defined as coronary heart disease, heart failure, stroke, peripheral vascular disease, previous myocardial infarction, or diabetes (considered a vascular disease risk equivalent) (1).
We constructed receiver operator characteristic (ROC) curves to identify optimal waist circumference cut points as values resulting in the largest sum of sensitivity and specificity for the presence of abnormal cIMT or M-CVD. A final waist circumference cut point value was defined for each sex as the average value weighted for the area under the ROC curve for each end point.
Once optimal waist circumference cut points were defined, we assessed statistical agreement between original AHA/NHLBI and updated MetS definitions using the κ-statistic. We compared cIMT with agreement categories using ANCOVA, adjusting for sex. Analyses are age-standardized to the World Health Organization standard world population (11).
RESULTS
Characteristics of the study population are shown in supplemental Table A1 (available at http://care.diabetesjournals.org/cgi/content/full/dc09-2353/DC1). Areas under the ROC curves for waist circumference as a predictor of abnormal cIMT (supplemental Table A2) ranged between 0.58–0.70. In women, optimal waist circumference cut points to detect an abnormal cIMT based on age-specific cutoffs, an abnormal cIMT based on age-independent cutoff, and M-CVD were 86, 86, and 89 cm, respectively. In men, corresponding optimal waist circumference cut points were 96, 99, and 96 cm. Optimal weighted–average waist circumference cut points were 97 cm for men and 87 cm for women. These cut points correspond to waist-to-height ratios of 0.577 and 0.560 in men and women, respectively.
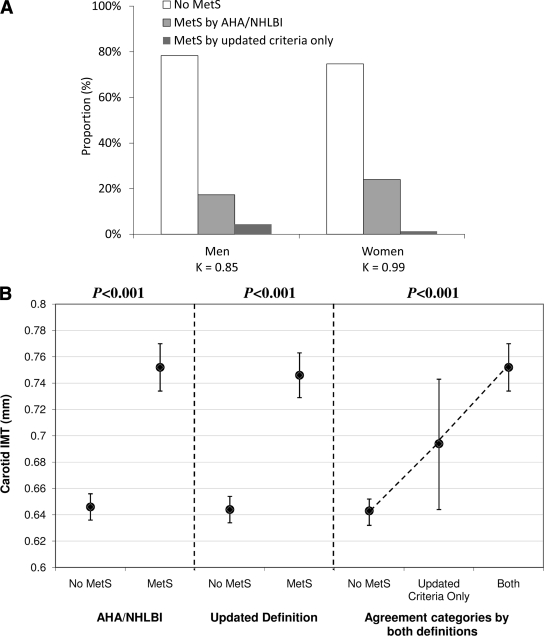
Using these cutoffs, the updated MetS definition generated greater prevalence estimates than the original AHA/NHLBI definition (supplemental Table A3). The original AHA/NHLBI and updated definitions differed in classifying 4.4% of men (κ = 0.85) and 1.3% of women (κ = 0.99) (Figure 1A). Between-sex differences in the prevalence of MetS were less pronounced with the updated definition than the original AHA/NHLBI definition.
Figure 1.
Prevalence of different categories of agreement between updated and AHA/NHLBI MetS definitions in men (n = 723) and women (n = 662) (A) and mean cIMT in subjects with and without MetS according to the original AHA/NHLBI definition and the updated definition (B). B: The left panel shows mean cIMT among subjects with (n = 401) and without (n = 984) MetS according to the original AHA/NHLBI definition. The middle panel shows the mean cIMT among subjects with (n = 444) and without (n = 941) MetS according to the updated MetS definition. The right panel shows mean cIMT among subjects who do not meet the MetS criteria by any definition (“No MetS,” left bar; n = 941), those who meet the updated criteria but not the original AHA/NHLBI criteria (“Updated Criteria Only,” middle bar; n = 43) and those who meet the MetS criteria by both definitions (“Both,” right bar; n = 401). Point estimates and 95% CIs (bars) are shown. All comparisons are adjusted for sex.
Figure 1B shows sex-adjusted mean cIMT among subjects with and without MetS according to the original AHA/NHLBI definition (left panel), and subjects with and without MetS according to the updated definition (center panel). The right panel compares cIMT with subjects meeting the updated but not the original AHA/NHLBI criteria (middle bar) versus those who do not meet the criteria by any definition (left bar), and those who meet the criteria by both definitions (right bar). Either definition identified subjects with increased cIMT. However, compared with those who did not meet the criteria by either definition, cIMT was significantly higher among subjects who met the updated but not the original AHA/NHLBI MetS criteria, but was highest in subjects who met the criteria by both definitions (P < 0.001).
CONCLUSIONS
In Andean Hispanic adults, waist circumference cut points of >97 cm in men and >87 cm in women provide optimal discrimination for cardiovascular risk assessment as judged by the presence of M-CVD or increased cIMT. Using these cut points in the context of the updated MetS definition, we found considerable disagreement between the updated and original AHA/NHLBI definitions among men. The updated criteria identified a larger proportion of subjects. Individuals who met only the updated MetS criteria (and not the original AHA/NHLBI-criteria) demonstrated higher cIMT compared with subjects who did not have MetS by either criteria, indicating that the more sensitive updated classification is not spurious but rather predictive of early vascular disease. These findings are important because they provide preliminary definitions of abdominal obesity for the purpose of atherosclerotic risk assessment and they identify a useful operative MetS definition in Andean adults until more definitive prospective data become available.
The lower waist circumference cut points identified among Andean men may result from a lower body height (resulting in lower waist circumference for any given fat distribution and waist-to-height ratio), from ethnic-related differences in body fat accumulation, or from competing risk factors (unrelated to abdominal obesity) for the development of CVD in this population.
Our study is limited by its cross-sectional nature and because it may not representative of all mixed-Andean populations.
In conclusion, our findings support the use of ethnic-specific cutoff points for abdominal obesity (>97 cm in men and >87 cm in women) and the use of the updated definition for the diagnosis of MetS in Andean Hispanic adults.
Supplementary Material
Acknowledgments
The PREVENCION study was supported by the Santa Maria Research Institute, Arequipa, Peru. C.A.P. is supported by the National Institutes of Health (NIH) Office of the Director, Fogarty International Center, Office of AIDS Research, National Cancer Center, National Eye Institute, NHBLI, National Institute of Dental and Craniofacial Research, National Institute on Drug Abuse, National Institute of Mental Health, National Institute of Allergy and Infectious Diseases, and NIH Office of Research on Women's Health through the International Clinical Research Fellows Program at Vanderbilt University (R24 TW007988). J.A.C. is supported by NIH Grant RO1-HL080076 and American Heart Association National Research Award 0885031N.
No potential conflicts of interest relevant to this article were reported.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001;285:2486–2497 [DOI] [PubMed] [Google Scholar]
- 2. Alberti KG, Zimmet P, Shaw J: IDF Epidemiology Task Force Consensus Group. The metabolic syndrome–a new worldwide definition. Lancet 2005;366:1059–1062 [DOI] [PubMed] [Google Scholar]
- 3. Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC, Jr: International Diabetes Federation Task Force on Epidemiology and Prevention, National Heart, Lung, and Blood Institute, American Heart Association, World Heart Federation, International Atherosclerosis Society, International Association for the Study of Obesity. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009;120:1640–1645 [DOI] [PubMed] [Google Scholar]
- 4. Perez M, Casas JP, Cubillos-Garzón LA, Serrano NC, Silva F, Morillo CA, López-Jaramillo P: Using waist circumference as a screening tool to identify Colombian subjects at cardiovascular risk. Eur J Cardiovasc Prev Rehabil 2003;10:328–335 [DOI] [PubMed] [Google Scholar]
- 5. Garcia RG, Cifuentes AE, Caballero RS, Sanchez L, López-Jaramillo P: A proposal for an appropriate central obesity diagnosis in Latin American population. Int J Cardiol 2006;110:263–264 [DOI] [PubMed] [Google Scholar]
- 6. Herrera VM, Casas JP, Miranda JJ, Perel P, Pichardo R, González A, Sanchez JR, Ferreccio C, Aguilera X, Silva E, Oróstegui M, Gómez LF, Chirinos JA, Medina-Lezama J, Pérez CM, Suárez E, Ortiz AP, Rosero L, Schapochnik N, Ortiz Z, Ferrante D, Diaz M, Bautista LE: Interethnic differences in the accuracy of anthropometric indicators of obesity in screening for high risk of coronary heart disease. Int J Obes 2009;33:568–576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Medina-Lezama J, Chirinos JA, Zea-Díaz H, Morey O, Bolanos JF, Munoz-Atahualpa E, Chirinos-Pacheco J: Design of PREVENCION: a population-based study of cardiovascular disease in Peru. Int J Cardiol 2005;105:198–202 [DOI] [PubMed] [Google Scholar]
- 8. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC, Jr, Spertus JA, Costa F: American Heart Association, National Heart, Lung, and Blood Institute. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005;112:2735–2752 [DOI] [PubMed] [Google Scholar]
- 9. Chirinos JA, David R, Bralley JA, Zea-Díaz H, Muñoz-Atahualpa E, Corrales-Medina F, Cuba-Bustinza C, Chirinos-Pacheco J, Medina-Lezama J: Endogenous nitric oxide synthase inhibitors, arterial hemodynamics, and subclinical vascular disease: the PREVENCION Study. Hypertension 2008;52:1051–1059 [DOI] [PubMed] [Google Scholar]
- 10. Vasan RS: Biomarkers of cardiovascular disease: molecular basis and practical considerations. Circulation 2006;113:2335–2362 [DOI] [PubMed] [Google Scholar]
- 11. Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJL, Lozano R, Inoue M: Age standardization of rates: a new WHO standard. Global Programme on Evidence for Health Policy Discussion Paper Series: No. 31. World Health Organization [article online], http://www.who.int/healthinfo/paper31.pdf. Accessed 1 December 2009
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.