Sir,
Familial idiopathic basal ganglia calcification (FIBGC) is characterized by brain calcium deposition and variable combinations of movement disorders, gait impairment, and neuropsychiatric symptoms [1-3, 5-7]. A locus was mapped on chromosome 14 [2], but it fails to account for disease in some families [7]. Penetrance estimates are hampered by inconsistent clinical-radiological correlation, and few detailed pathological reports are available [4, 7]. Herein, we provide clinical, radiological and pathological studies of a patient with FIBGC. We previously reported this family, including one autopsy study [4, 7]. The patient signed informed consent.
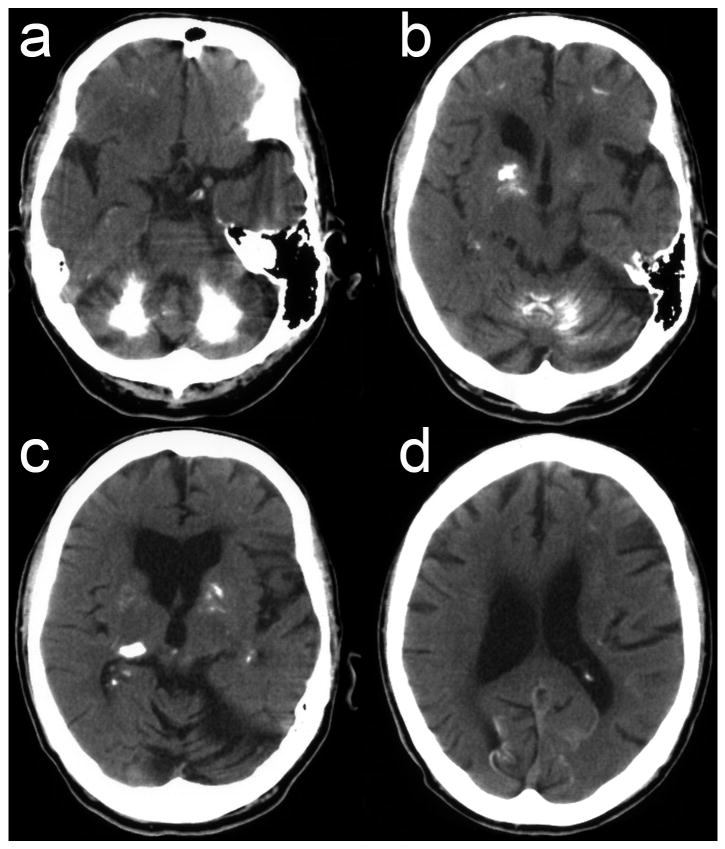
A right-handed male (patient III-3 in [7]) came to our attention at age 76 with a 50-year history of trunk, upper extremities and oral abnormal movements. Motor symptoms began with writing difficulties, followed by right-predominant abnormal movements of both shoulders. At age 50, he developed progressive speech difficulties with mild memory and gait impairment. Six first-degree and three second-degree relatives had similar symptoms including generalized, oromandibular, axial, limb and cervical dystonia, chorea, postural tremor and ataxia (reported in [7]). The patient had mild recall impairment, speech-induced jaw-opening dystonia, trunk and right-predominant upper extremities chorea, right shoulder postural dystonia, and writer's cramp. Genetic testing was negative for Huntington's disease. Brain CT-scan showed calcification of the basal ganglia, subcortical white matter, thalamus, and cerebellum (Figure 1).
Figure 1.
Brain axial CT-scan shows third and lateral ventricles enlargement and severe calcification of the cerebellar hemispheres and vermis (a,b), striatum, globus pallidus and thalamus (b,c), and subcortical white matter and occipital cortex (a-d). Basal ganglia calcification predominates on the right side (b,c), ipsilateral to symptomatic predominance.
Over the next five years, the patient became severely dysarthric and unstable with falls. Upper extremities and trunk chorea and dystonia remained unchanged, whereas jaw-opening dystonia worsened. He scored 21/26 on the Mini Mental Status Examination (unable to write or draw), missing points on attention span and recall. The patient subsequently developed severe cognitive impairment and behavioral troubles with agitation and aggressiveness. He became unable to stand, chew or speak, lost 30kg over two years, and died at age 85.
The fixed left hemibrain weighed 520g. There was mild frontal-predominant atrophy with enlarged lateral ventricles, and cerebellar atrophy. Brain arteries showed severe atherosclerosis. There was gray discoloration and gritty consistency of the posterior periventricular region, globus pallidus, putamen and anterior thalamus, and mild atrophy of the caudate nucleus (Figure 2a). The cerebellum had yellow-red discoloration and gritty consistency of deep white matter and dentate nucleus region.
Figure 2.

Macroscopic view (a) shows brown discoloration of globus pallidus (arrow), which had a gritty consistency at autopsy. On histology, von Kossa calcium staining (b) and hematoxylin-eosin staining (c-l) show widespread calcification of cerebellum deep regions (b,c, large pleomorphic calcification = arrows, dark compact round calcification = arrowheads), cerebellum blood vessels (d, arrows), dentate nucleus (e, dark round calcification = arrowheads), cerebellum cortex (f, large pleomorphic calcification = arrows), visual cortex (g,h, pleomorphic calcification = arrows, dark round calcification = arrowheads), hippocampal dentate fascia (i,j, arrows), and hemisphere white matter (k,l, perivascular calcification = arrows, dark round calcification in the vicinity of a capillary = arrowheads).
There was striking vascular and parenchymal mineralization (Figure 2b-l) that stained positive for calcium (Figure 2b). In the cortex, small vessel calcific vasculopathy was prominent in lower cortical layers and at the grey-white junction in the depths of the sulci. Parenchymal calcification was patchy and multifocal in deep subcortical and posterior periventricular regions, putamen, globus pallidus, anterior thalamus, and in the visual cortex. There was massive cerebellar calcification in the hemispheres (cortex and white matter) and in the dentate nucleus. Even in severely affected areas, there was no significant neuronal loss. Mild Alzheimer pathology and amyloid angiopathy were present. There were ischemic changes in subcortical areas and numerous microinfarcts in the cortex and basal ganglia. Overall, the pathology was similar to that of our previous autopsied patient from the same family [4, 7].
Our observation highlights the difficulties in correlating the clinical, radiological and pathological features in FIBGC. Reasons for this include that: a) many family members have widespread calcification without symptoms [7], b) radiologic asymmetry does not always match that of symptoms, c) ataxia is rare despite common severe cerebellar involvement, and d) there is no significant neuronal loss even in severely affected areas. Although basal ganglia and subcortical/periventricular white matter involvement may explain movement disorders and cognitive impairment, the mechanism of neuronal dysfunction remains elusive. Extensive blood vessel and perivascular calcification may suggest a chronic ischemic mechanism leading to neuronal dysfunction only in susceptible brain regions/individuals. Chronic low-grade inflammation has been suggested to favor calcification, a hypothesis that gained support from the report of reactive astrocytes and microglia overexpressing inflammatory molecules around calcified areas [4]. However, using HLA-DR and GFAP immunostaining in our patient, we were unable to demonstrate activated microglia and reactive astrocytes. Alternatively, calcium deposition may alter glial cells metabolism and secondarily impair neuronal function, or only represent a by-standing phenomenon of a yet undefined patho-mechanism involving genetically-determined age-related neuronal dysfunction.
Acknowledgments
We thank Dr. David Welbourne and Audrey Strongosky for their help in obtaining the autopsy material, and Dr. Rosa Rademakers and Matt Baker for providing us with the DNA sample. C.W. is supported by the Swiss National Science Foundation (PBLAB-115478), Parkinson Switzerland, are the Robert H. and Clarice Smith and the M.L. Simpson Foundation Trust. K.J.S. is supported by the German Research Foundation (DFG). Z.K.W. and D.W.D. are supported by the Morris K. Udall Center of Excellence for Parkinson's Disease Research (P50-NS40256). D.W.D. is supported by the Mayo Clinic ADRC grant P50-AG16574. Z.K.W. and D.W.D. are supported by the Pacific Alzheimer Research Foundation (PARF) grant C06-01. D.F.B. is supported by the Mayo Clinic Jacksonville Research Committee CR10 program grant.
References
- 1.Baba Y, Broderick DF, Uitti RJ, Hutton ML, Wszolek ZK. Heredofamilial brain calcinosis syndrome. Mayo Clin Proc. 2005;80:641–651. doi: 10.4065/80.5.641. [DOI] [PubMed] [Google Scholar]
- 2.Geschwind DH, Loginov M, Stern JM. Identification of a locus on chromosome 14q for idiopathic basal ganglia calcification (Fahr disease) Am J Hum Genet. 1999;65:764–772. doi: 10.1086/302558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Manyam BV, Walters AS, Keller IA, Ghobrial M. Parkinsonism associated with autosomal dominant bilateral striopallidodentate calcinosis. Parkinsonism Relat Disord. 2001;7:289–295. doi: 10.1016/s1353-8020(00)00036-5. [DOI] [PubMed] [Google Scholar]
- 4.Miklossy J, Mackenzie IR, Dorovini-Zis K, Calne DB, Wszolek ZK, Klegeris A, McGeer PL. Severe vascular disturbance in a case of familial brain calcinosis. Acta Neuropathol. 2005;109:643–653. doi: 10.1007/s00401-005-1007-7. [DOI] [PubMed] [Google Scholar]
- 5.Oliveira JR, Spiteri E, Sobrido MJ, Hopfer S, Klepper J, Voit T, Gilbert J, Wszolek ZK, Calne DB, Stoessl AJ, Hutton M, Manyam BV, Boller F, Baquero M, Geschwind DH. Genetic heterogeneity in familial idiopathic basal ganglia calcification (Fahr disease) Neurology. 2004;63:2165–2167. doi: 10.1212/01.wnl.0000145601.88274.88. [DOI] [PubMed] [Google Scholar]
- 6.Warren JD, Mummery CJ, Al-Din AS, Brown P, Wood NW. Corticobasal degeneration syndrome with basal ganglia calcification: Fahr's disease as a corticobasal look-alike? Mov Disord. 2002;17:563–567. doi: 10.1002/mds.10122. [DOI] [PubMed] [Google Scholar]
- 7.Wszolek ZK, Baba Y, Mackenzie IR, Uitti RJ, Strongosky AJ, Broderick DF, Baker MC, Melquist S, Hutton ML, Tsuboi Y, Allanson JE, Carr J, Kumar A, Calne SM, Miklossy J, McGeer PL, Calne DB, Stoessl AJ. Autosomal dominant dystonia-plus with cerebral calcifications. Neurology. 2006;67:620–625. doi: 10.1212/01.wnl.0000230141.40784.09. [DOI] [PubMed] [Google Scholar]