Abstract
To quantify the risk of human papillomavirus (HPV) acquisition associated with a first male sex partner and to identify associated risk factors, we analyzed data from women who were enrolled before or within 3 months of first intercourse with a male partner and were censored at the report of a second partner. The 1-year cumulative incidence of first HPV infection was 28.5% (95% confidence interval, 20.6%–38.6%) and increased to almost 50% by 3 years. The risk was increased when the first male partner was sexually experienced. Our results indicate a high risk of HPV infection in young women who have had just 1 male sex partner.
Rates of genital human papillomavirus (HPV) acquisition are high in sexually active young women, with several longitudinal studies reporting 3-year cumulative incidence estimates of 40% or greater [1–3]. Although previous estimates have indicated a high risk of infection after sexual debut (we previously reported that 30%–37% of women acquired an HPV infection in the year following first vaginal intercourse [2, 4]) and with each new sex partner [5], the risk of infection specifically associated with a first male sex partner has not been quantified. One previous study of newly sexually active young women showed a 3-year cumulative incidence of infection before having a second sex partner of 45% [6]; however, given that participants were recruited up to 1 year after sexual debut, early infections of short duration may have been missed, and 1- and 2-year cumulative incidence estimates were not reported. The primary goal of the present analysis was to quantify the risk of HPV acquisition associated with a first male sex partner. We also sought to identify characteristics of young women and their first male sex partners that were associated with an increased risk of HPV acquisition.
Methods
Between December 2000 and November 2006, 244 female university students 18–22 years old were recruited to participate in a longitudinal study of HPV infection. Recruitment procedures and data collection have been described elsewhere [4]. Women were eligible to enroll if they had never had vaginal intercourse with a male partner or had first had intercourse with 1 male partner within the previous 3 months. Informed consent was obtained from all participants, and the human-experimentation guidelines of the University of Washington Institutional Review Board were followed.
Every 2 weeks, women completed a Web-based diary designed to capture daily sexual behavior information, including detailed information on new partners (e.g., date of first intercourse with a new partner, partner age, and partner's number of previous sex partners). Detailed diary features have been described elsewhere [4, 7]. Every 4 months, women were followed with gynecological examinations. At each visit, self-collected vaginal swabs and clinician-collected cervical and vulvovaginal swabs were collected for HPV DNA testing by polymerase chain reaction (PCR)–based methods [4]. As described elsewhere, specimens testing positive by a generic probe were typed using a reverse line-blot assay (Roche Molecular Systems) for 37 HPV types [8]. PCR results for self-collected vaginal swabs and clinician-collected cervical and vulvovaginal swabs were combined to analyze genital HPV acquisition.
Analyses were restricted to 130 women who reported their first intercourse with a male partner within 3 months of enrollment or during follow-up and had at least 1 clinical visit after first intercourse. Five women testing positive for HPV before their first intercourse were excluded; 4 were positive for a single type (including 6, 51, 53, and 66), and 1 was concurrently positive for types 40, 61, and 66.
The cumulative incidence of first HPV infection associated with a first sex partner was estimated using the Kaplan-Meier method. Time to event was calculated from first intercourse to first HPV detection (any type). Women were censored at the date of first vaginal intercourse with a second male partner or at the last follow-up visit. Cox proportional hazards models were used to determine risk factors for first HPV infection associated with a first sex partner. Female subject and first male partner characteristics (based on the female subject's report) considered as risk factors for HPV acquisition included age at first intercourse, years between menarche and first intercourse, partner age, and partner's number of previous sex partners. Partner's number of previous sex partners was categorized a priori into 5 categories: approximate quartiles (0, 1, 2, and ≥3) and unknown. All other variables were evaluated for linear trends by use of a likelihood ratio test to compare categorical models with approximate quartiles or terciles to corresponding linear models based on the categorical variables. Variables with significant likelihood ratio tests were retained as categorical variables and variables without significant likelihood ratio tests were included as continuous variables. This resulted in the following classifications: age at first intercourse, continuous; years between menarche and first intercourse, 2–5, 6, 7, and 8–14; and partner age, 16–19, 20–21, and 22–42 years. Variables were first tested univariately. Statistically significant (P < .10) variables were entered into a multivariate model. Backward stepwise regression was used to construct the final multivariate model, with P < .05 used as the criterion for removing variables.
Results
The mean age of the 130 women (assessed at the date of first intercourse) was 19.4 years (SD, 1.3 years; range, 18–24 years). Their mean age at menarche was 12.5 years (SD, 1.3 years; range, 10–17 years), and the mean interval between menarche and first intercourse was 6.9 years (SD, 1.8 years; range, 2–14 years). The mean age of their first male sex partner was 21.0 years (SD, 3.3 years; range, 16–42 years). After first intercourse, their mean follow-up time was 28.2 months (SD, 19.4 months), the mean number of visits per woman was 5.8 (SD, 4.5), and the median time between visits was 4.1 months. Of the 130 women, 45 (34.6%) were censored at the date of report of a second sex partner; their mean time between intercourse with a first partner and intercourse with a second partner was 12.5 months (SD, 8.5 months).
The 12-month cumulative incidence of first HPV infection after reporting a first sex partner was 28.5% (95% confidence interval [CI], 20.6%–38.6%) and increased to 39.2% (95% CI, 28.6%–52.0%) at 24 months and to 49.1% (95% CI, 35.8%–64.2%) at 36 months (figure 1). The mean number of types detected at the time of first HPV infection was 1.5 (SD, 0.8; range, 1–4).
Figure 1.
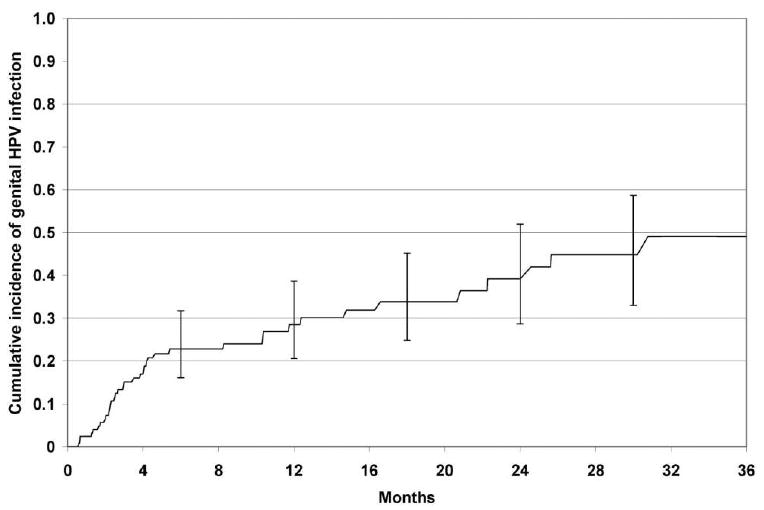
Cumulative incidence of any genital HPV infection associated with a first sex partner. The X-axis shows the no. of months from the time of first reported vaginal intercourse with a male partner (women were censored at the reported date of a second male sex partner).
In univariate analyses, women reporting partners with 2 (hazard ratio [HR], 3.57 [95% CI, 1.04–12.22]), ≥3 (HR, 8.46 [95% CI, 3.13–22.88]), or an unknown (HR, 6.80 [95% CI, 2.15–21.50]) number of previous partners were more likely to acquire HPV than were women reporting partners with no previous partners (table 1). Women reporting menarche 2–5 years before first intercourse were more likely to acquire HPV than were women reporting menarche 8–14 years before first intercourse (HR, 2.57 [95% CI, 1.13–5.82]) (table 1). Women reporting partners who were 22–42 years old were more likely to acquire HPV than were women reporting partners who were 16–19 years old (HR, 2.75 [95% CI, 1.34–5.67]) (table 1). Age at first intercourse was not statistically significantly associated with the risk of HPV acquisition (table 1). When partner's numbers of previous partners, years between menarche and first intercourse, and partner age were entered in the multivariate model, the only variable that remained statistically significant was partner's number of previous partners.
Table 1. Univariate hazard ratios (HRs) for the associations between first incident human papillomavirus (HPV) infection (any type) and characteristics of subjects and their first male sex partners.
| Risk factor | HR (95% CI) | No. of first incident HPV infections/women-years at risk |
|---|---|---|
| Age at first intercourse (continuous) | 1.06 (0.81–1.37) | 39/132.1 |
| Years between menarche and first intercourse | ||
| 8–14 | 1.00 | 10/40.5 |
| 7 | 1.15 (0.46–2.89) | 9/33.4 |
| 6 | 0.57 (0.19–1.70) | 5/38.6 |
| 2–5 | 2.57 (1.13–5.82) | 5/19.6 |
| Partner agea | ||
| 16–19 years | 1.00 | 13/42.2 |
| 20–21 years | 0.50 (0.20–1.21) | 7/55.1 |
| 22–42 years | 2.75 (1.34–5.67) | 18/22.7 |
| Partner's no. of previous partnersa,b | ||
| 0 | 1.00 | 4/41.4 |
| 1 | 0.37 (0.04–3.29) | 1/31.9 |
| 2 | 3.57 (1.04–12.22) | 5/11.5 |
| ≥3 | 8.46 (3.13–22.88) | 16/16.4 |
| Unknown | 6.80 (2.15–21.50) | 12/19.8 |
NOTE. CI, confidence interval.
Based on the female subject's report.
This was the only variable remaining significant in multivariate analysis.
Discussion
We previously reported that the risk of HPV infection is high in the years immediately following a woman's sexual debut [2, 4]. In the present study, we have quantified the risk of infection from a first male sex partner by censoring data from women who acquired a second male sex partner during follow-up. Nearly 30% of the female university students in our cohort tested positive for HPV DNA within 1 year of first intercourse with a first male sex partner, and by 3 years almost half tested positive. These results indicate that women are at high risk of acquiring an HPV infection from just 1 male sex partner. Although our unique study population consisted of women who had delayed first intercourse until at they were at least 18 years of age, our 3-year cumulative incidence estimate is comparable to that reported in a previous study of 15–19-year-old women recruited within 1 year of sexual debut and followed until report of a second male sex partner [6].
Our previous analyses suggest that most new HPV infections will be detectable within 1 year of exposure [2, 4]. Indeed, in the present study, the majority of first HPV infections (30/39 [76.9%]) were first detected within 1 year of first intercourse. The remaining 9 infections were first detected between 12 and 44 months after first intercourse. Infections detected farther from the date of first intercourse could be attributable to incomplete reporting (e.g., failure to report sex with a second male partner), nonpenetrative sexual contact (without vaginal intercourse) with another male partner [2], or sexual contact with female partners [9]. (These are also plausible explanations for why HPV DNA was detected in 5 women who reported no previous vaginal intercourse.) All of these possibilities would result in an overestimate of the cumulative incidence of infection associated with a first male sex partner. In addition, the likelihood of transmission may change during the course of a partnership (e.g., a couple who uses condoms consistently at the beginning of the relationship may cease to do so later in the partnership or a male partner may have concurrent partners and become exposed to new HPV infections during the course of the partnership), thus delaying acquisition.
As in previous studies [2, 4, 6, 10], a woman's estimate of her male partner's lifetime number of sex partners was positively associated with her risk of HPV infection. However, the associations were statistically significant only when women reporting male partners with 2 or more or an unknown number of previous partners were compared with women reporting virginal partners. In previous analyses, we grouped partners with 1 or more previous partners into 1 risk category [2, 4]; in the present analysis, the finer comparisons suggest that the increased risk associated with acquiring sexually experienced partners may be limited to those partners who (are thought to) have had at least 2 other sex partners.
After adjustment for a first male partner's number of previous sex partners, the excess risk associated with partners >21 years old (relative to partners <20 years old) was attenuated. These data suggest that the risk of acquiring an HPV infection from a first male partner is more strongly related to the partner's prior sexual experience than the partner's age.
In this cohort of 18–24-year-old women, years since menarche was not independently associated with the risk of acquiring HPV infection from a first male sex partner after adjustment for the male partner's number of previous sex partners. Previous studies have suggested that the interval between menarche and first intercourse is related to the risk of HPV infection (possibly due to biological factors that increase susceptibility to infection), but the directions of the observed associations have been inconsistent [6, 11, 12]. Given that >95% of participants in this study were at least 5 years past menarche at the time of first intercourse, we were unable to assess whether short intervals between menarche and first intercourse increase the risk of infection from a first partner.
In summary, the percentage of university-aged women who acquired an HPV infection from a first male sex partner was high, and the risk increased when the partner was sexually experienced. Our results indicate a high risk of HPV infection in women who acquire just 1 male sex partner.
Acknowledgments
National Institute of Allergy and Infectious Diseases (grants R01-A138383 and T32AI007140-24).
Footnotes
Potential conflicts of interest: none reported.
Presented in part: 16th Biennial Meeting of the International Society for Sexually Transmitted Diseases Research, Amsterdam, July 2005 (abstract MP-120).
References
- 1.Ho GYF, Bierman R, Beardsley L, Chang CJ, Burk RD. Natural history of cervicovaginal papillomavirus infection in young women. N Engl J Med. 1998;338:423–8. doi: 10.1056/NEJM199802123380703. [DOI] [PubMed] [Google Scholar]
- 2.Winer RL, Lee SK, Hughes JP, Adam DE, Kiviat NB, Koutsky LA. Incident infection with genital human papillomavirus: rates and risk factors among a cohort of female university students. Am J Epidemiol. 2003;157:218–26. doi: 10.1093/aje/kwf180. [DOI] [PubMed] [Google Scholar]
- 3.Woodman CB, Collins S, Winter H, et al. Natural history of cervical human papillomavirus infection in young women: a longitudinal cohort study. Lancet. 2001;357:1831–6. doi: 10.1016/S0140-6736(00)04956-4. [DOI] [PubMed] [Google Scholar]
- 4.Winer RL, Hughes JP, Feng Q, et al. Condom use and the risk of genital human papillomavirus infection in young women. N Engl J Med. 2006;354:2645–54. doi: 10.1056/NEJMoa053284. [DOI] [PubMed] [Google Scholar]
- 5.Burchell AN, Winer RL, de Sanjosé S, Franco EL. Chapter 6: epidemiology and transmission dynamics of genital HPV infection. Vaccine. 2006;24(Suppl 3):S52–61. doi: 10.1016/j.vaccine.2006.05.031. [DOI] [PubMed] [Google Scholar]
- 6.Collins SI, Mazloomzadeh S, Winter H, et al. Proximity of first intercourse to menarche and the risk of human papillomavirus infection: a longitudinal study. Int J Cancer. 2005;114:498–500. doi: 10.1002/ijc.20732. [DOI] [PubMed] [Google Scholar]
- 7.Baer A, Saroiu S, Koutsky LA. Obtaining sensitive data through the Web: an example of design and methods. Epidemiology. 2002;13:640–5. doi: 10.1097/00001648-200211000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Weaver BA, Feng Q, Holmes KK, et al. Evaluation of genital sites and sampling techniques for detection of human papillomavirus DNA in men. J Infect Dis. 2004;189:677–85. doi: 10.1086/381395. [DOI] [PubMed] [Google Scholar]
- 9.Marrazzo JM, Koutsky LA, Stine KL, et al. Genital human papillomavirus infection in women who have sex with women. J Infect Dis. 1998;178:1604–9. doi: 10.1086/314494. [DOI] [PubMed] [Google Scholar]
- 10.Burk RD, Ho GYF, Beardsley L, Lempa M, Peters M, Bierman R. Sexual behavior and partner characteristics are the predominant risk factors for genital human papillomavirus infection in young women. J Infect Dis. 1996;174:679–89. doi: 10.1093/infdis/174.4.679. [DOI] [PubMed] [Google Scholar]
- 11.Kahn JA, Rosenthal SL, Succop PA, Ho GY, Burk RD. The interval between menarche and age of first sexual intercourse as a risk factor for subsequent HPV infection in adolescent and young adult women. J Pediatr. 2002;141:718–23. doi: 10.1067/mpd.2002.128893. [DOI] [PubMed] [Google Scholar]
- 12.Shew ML, Fortenberry JD, Miles P, Amortegui AJ. Interval between menarche and first sexual intercourse, related to risk of human papillomavirus infection. J Pediatr. 1994;125:661–6. doi: 10.1016/s0022-3476(94)70031-1. [DOI] [PubMed] [Google Scholar]


