Abstract
The aim of the study was to investigate a porous nanohydroxyapatite/polyamide 66 (n-HA/PA66) scaffold material that was implanted into muscle and tibiae of 16 New Zealand white rabbits to evaluate the biocompatibility and osteogenesis and osteoinductivity of the materials in vivo. The samples were harvested at 2, 4, 12 and 26 weeks respectively, and subjected to histological analysis. At 2 weeks, the experiment showed that osteogenesis was detected in porous n-HA/PA66 composite and the density of new bone formation was similar to the surrounding host bone at 12 weeks. The study indicated that three-dimensional pore structures could facilitate cell adhesion, differentiation and proliferation, and help with fibrovascular and nerve colonization. In conclusion, porous n-HA/PA66 scaffold material could be a good candidate as a bone substitute material used in clinics due to its excellent histocompatibility, osteoconductivity and osteoinductivity.
Keywords: porous, nano hydroxyapatite, polyamide, interconnected porosity, biocompatibility, osteoconductivity, osteoinductivity
Introduction
In bone tissue engineering, scaffolds serve as the matrices of tissue formation, and play a pivotal role in osseointegration and tissue integration. After dental extractions, periodontal disease or trauma factors, alveolar bone resorption alters both the height and thickness of the remaining alveolar ridge.1 Bone grafting is frequently used to augment bone healing with numerous approaches to reconstructing or replacing skeletal defects. Autologous bone graft remains the most effective grafting material because it provides the three elements required for bone regeneration: osteoconduction, osteoinduction, and osteogenic cells. But there are some problems for allogeneic and autologous bone grafts such as limited availability and increased trauma. Allogeneic bone grafting can sometimes induces immunologic rejection and transmission of potential pathogens such as the human immunodeficiency virus (HIV) and the hepatitis virus. Therefore, the search for an ideal artificial bone substitute material has been a hot issue for bone repair and reconstruction.
Nanohydroxyapatite (n-HA) is an ideal bioactive material whose composition and crystal structure is very close to the natural bone, and can directly bond to bone tissue in vivo. It has been developed in a variety of forms such as substitute and regeneration material because of its excellent osteoconductivity, osteoinductivity, abrasion resistance, corrosion resistance and stable chemical properties. But this is exactly what limits its application, because ideal scaffolds should support cell migration and bone growth, in accordance with the rate of material degradation.2,3 On the other hand, its brittleness and poor performance of mechanical stability limit its use for the regeneration of load bearing bone defects.
Bone is one of the biomineralization materials which are comprised of collagen, apatite and water, one third of which is inorganic and two thirds of which is organic. Polyamide (PA) has good biocompatibility with human tissue, probably due to its similarity to collagen protein in chemical structure. It has been widely used in the biomaterials application of surgical sutures for nearly half a century. Especially important, PA also exhibits excellent mechanical properties.4 But the degradation of it is difficult to control. To overcome these shortages, the novel porous nanohydroxyapatite/polyamide 66 (n-HA/PA66) which is synthesized from hydroxyapatite and polyamide is foamed by thermal pressing and injection molding techniques. High porosity and proper pore size may facilitate cell seeding, survival, growth, differentiation and proliferation. Therefore, the aim of this research is to investigate the tissue reaction to evaluate the histocompatibility and osteogenesis of the materials in vivo.
Materials and methods
Materials and characterization
Porous n-HA/PA66 scaffold materials were synthesized from n-HA and polyamide, foamed by thermal pressing and injection molding techniques. The bending strength, tensile strength and compressive strength of the composite with 64.5 wt% n-HA content were 95, 79, and 117 MPa5 respectively, which was close to the natural bone (80–100, 60–120, 50–140 MPa separately).6 The elastic modulus of the composite was 5.6 GPa which is similar to natural bone (3–25 GPa). Therefore, the composite prepared can match well to human bone.5
Surgery
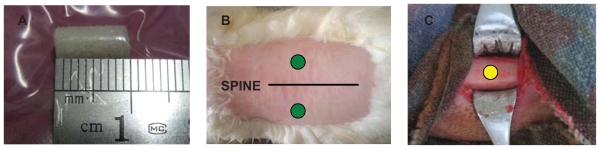
Sixteen New Zealand white rabbits (average weight between 2.0 kg and 2.5 kg) were obtained from State Key Laboratory, Chengdu, China, and were divided by random treatment into four groups of four each. The rabbits were anesthetized by intravenous injection of 3% sodium pentobarbital (1 ml/kg) and operated on under sterile conditions. As seen in Figure 1, middle skin incision was performed on the middle of the back, and two discs of porous n-HA/PA66 samples (5 mm in diameter and 10 mm in length) were inserted into the muscular pocket and sutured wounds. At the same time, the samples (2 mm in diameter and 4 mm in length) were implanted into the bone defect which matched the sample size in the tibiae. The rabbits were sacrificed at 2, 4, 12, and 26 weeks respectively. The specimens were submitted to histological assessment.
Figure 1.
Schematic diagram of material shape and the site of implantation. A) material shape B) the site of intramuscular implantation on the both sides of the spine. C) the site of endosseous implantation in the tibia.
Ethical approval
All animal procedures were carried out according to the guidelines of the Animal Ethics Committee of Sichuan University.
Results
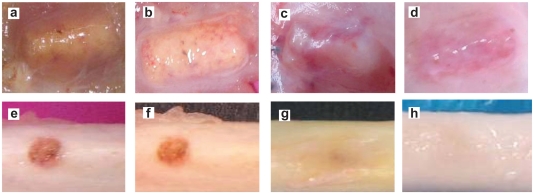
Macroscopic observation
No rabbits died or were infected in any of the groups. Food intake and weight bearing in each animal subject gradually improved. The wounds healed uneventfully with no postoperative infection or material displacement. Macroscopic observation revealed that muscular tissue bundled the samples tightly with no suppuration or necrosis (Figures 2a–d). As time went by, porous material integrated with bony tissue into a whole. There was no infection or immunologic rejection either. (Figures 2e–f).
Figure 2.
Macroscopic observations of intramuscular and endosseous implantation. (a–d: 2, 4, 12, and 26 weeks respectively after implantation in back muscles. e–f: 2, 4, 12, and 26 weeks respectively after implantation in tibia).
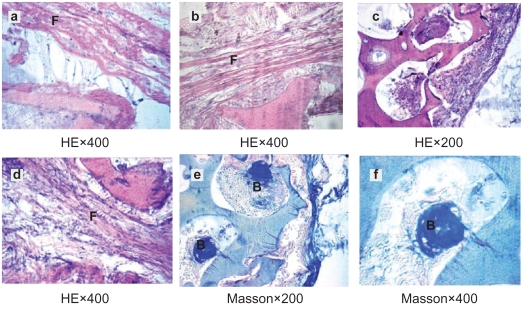
Intramuscular implantation
The host reaction was reflected at the site of implantation by histological assessment.7 At 2 weeks, material was surrounded by fibrous connective tissue which was comprised of approximately 10 layers of loose cells. The main reaction was that the fibroblast bundled the scaffold to form a fibrous capsule, because the organism considered it foreign.8 Small vessels and fibroblasts with a few lymphocytes and neutrophils infiltrated into the pores but no macrophages were detected, indicating the porous material had an excellent histocompatibility (Figure 3a). About 4 weeks later, the fibrous connective tissue gradually became thinner and denser. Collagen fiber formatted and crept into the pores (Figures 3b, c). At 12 weeks, the fibrous capsule wall was comprised of a great number of collagen fibers, and fibrocytes with no inflammatory cells existed (Figure 3d). Finally, reengineered cells were basically stable at 26 weeks (Figures 3e, f). Bone lacuna was clearly observed and new bone formed in the interconnected porosity increased, which indicated the n-HA/PA66 material with porosity and proper pore size facilitated cell adhesion, differentiation, and proliferation. It proved that porous n-HA/PA66 scaffold had excellent tissue compatibility and osteoinduction.
Figure 3.
HE staining and Masson’s staining of material implanted in muscle. a, b–c, d, e–f were the histological reaction at 2, 4, 12 and 26 weeks respectively.
Abbreviations: B, bone lacuna; F, fibrous capsule.
Endosseous implantation
No immunologic rejection was observed throughout the experiment. Pores were filled with loose connective tissue and small vessels at 2 weeks. Osseous tissue gradually crept into the interconnected porosity and connected with the material directly, without fibrous tissue. The amount of osteoid tissue was illustrated in the pore structure (Figure 4a). As we know, fibrous tissue existing at the interface between material and osseous tissue is a primary cause of implantation failure. After 4 weeks, osseous tissue formation augmented and became more mature. Bone trabecula enlarged showed active osteogenesis. Ossein graduated into woven bone and calcific nodules in the interconnected porosity (Figures 4b, c). Osteoclasts adhered to the surface of the pores’ structure which contributed to the bioresorption of the material (Figure 4d). At 12 weeks, needle-like bone trabecula connected with each other. New bone formatted in the pores and gradually linked one to another, and connected with materials directly (Figures 4e, f). At 26 weeks, interconnected porosity filled completely with new bone tissue, which integrated into a whole, and showed good osteoinductivity and osteocompatibility. Marrow cavity was also generated at that time (Figures 4g, h).
Figure 4.
HE staining and Masson’s staining of material implanted in tibiae. a, b–d, e–f, g–h were the histological reaction at 2, 4, 12 and 26 weeks respectively. Arrow points to osteoblast.
Abbreviation: M, marrow cavity.
Discussion
Bone was considered as a nanocomposite material which was comprised of collagen, apatite and water, one third of which was inorganic and two thirds of which was organic. Artificial bone grafting repaired bone defects as substitutes in the implantation, and not only had a good biocompatibility but also combined with natural bone as in osseointegration. It was necessary to provide support, voids and enhance biologic repair of bone defects. Strategies for development of biological substitutes capable of mimicking homeostasis were based on an understanding of the basic events in the healing of bone defects. Artificial bone substitutes had an ideal osteoconduction due to its three-dimensional structure and the related process of growth of capillaries, perivascular tissue and osteoprogenitor cells of the host into the graft. Bone substitutes used in the past (eg, medical metal materials, macromolecule materials, and bio-ceramic materials) could not bond to osseous tissue tightly, mostly due to the mechanical retention of the composites. Porous n-HA/PA66 scaffold material had better biological activity with high specific surface area, since the three-dimensional structure had a large contact region which facilitated cell adhesion, differentiation and proliferation, and benefited the metabolization. Kim indicated that nano-HA particles had better bioactivity and osteoinductivity than micro ones.9 In addition, the implantation environment was beneficial for osteoinduction because there was sufficient blood supply in the muscular tissue where there were some undifferentiated mesenchymal cells around vessels. Therefore, we observed bone lacuna clearly, and bone formed in the interconnected porosity when samples were implanted in muscle.
We evaluated porosity as a main indicator of three-dimensionally porous material, which related to the quantity and rapidity of osteogenesis. The pore size was a critical factor to osseointegration.10 Hulbert proposed 100 μm was the minimum porosity which allowed bone to creep in, and 150 μm was the best.11 Vaz considered that 500 μm was a more suitable diameter for bone cells.12 Scaffold for tissue engineering should possess a three-dimensionally porous structure with porosity no less than 70% and pore size ranging from 50 to 900 μm.13 Pores provide an ideal structure to induce cell adhesion, differentiation and proliferation, which not only benefits nutrient transportation, but also helps with fibrovascular and nerve colonization. However, the degree of porosity and diameter of pore size influenced the mechanical property of the scaffold. Consequently, to provide a lasting stress-absorbent core framework with transplants for bone tissue regeneration, we prepared an innovative n-HA/PA66 scaffold with relatively low porosity but better mechanical properties. Pore size of porous n-HA/PA66 scaffold material used in this study was 300–500 μm, porosity was 65%–75%. Macropores and micropores were captured from scanning electron microscope photographs of the porous scaffold. Mean size of macropores ranged from 300 to 500 μm, and on the wall of them there were micropores whose pore size was less than 50 μm.5 The pore size and inner surface area was important for the growth of bone tissue into the scaffold, the bigger the inner surface area the more the cells planting in it and the faster the tissue and organ formation. Macropores and micropores worked together to facilitate tissue ingrowth. In addition, the pores’ structure was propitious to form mechanical locking within, which was good for enhancing the combination of bone tissue and scaffold materials and creating a reliable retention. Pore structure also reduced the rigidity of the materials that were closed to the elastic modulus of the organization, which ensured the interface was stable. Cambium crept into the pores as time went by, not only reducing the brittleness of the materials, but also improving the bending strength – though the strength of the porous scaffold was low in the early days of planting.
Conclusions
The innovative bone tissue engineering porous n-HA/PA66 scaffold material provided a three-dimensional microstructure to accelerate bone tissue, fibrovascular and nerves colonization. According to the histological experiment results, we indicated that porous n-HA/PA66 scaffold material could be a good candidate as a bone substitute due to its excellent histocompatibility, osteoconductivity and osteoinductivity.
Footnotes
Disclosures
The authors report no conflicts of interest in this work.
References
- 1.Mecall RA, Rosenfeld A. The influence of residual ridge resorption patterns on fixture placement and tooth positon. Int J Periodontics Restorative Dent. 1991;11(1):8–23. [PubMed] [Google Scholar]
- 2.Strocchi R, et al. Bone regeneration with calcium sulfate: evidence for increased angiogenesis in rabbits. J Oral Implantol. 2002;28:273–278. doi: 10.1563/1548-1336(2002)028<0273:BRWCSE>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 3.Couri CJ, Maze GI, Hinkson DW, Byran H, Deborah V. Medical grade calcium sulfate hemihydrate versus expanded polytetrafluoroethylene in the treatment of mandibular class II furcations. J Periodontol. 2002;73(11):1352–1359. doi: 10.1902/jop.2002.73.11.1352. [DOI] [PubMed] [Google Scholar]
- 4.Springer ING, Fleiner B, Jepsen S, Acil Y. Culture of cells gained from temporomandibular joint cartilage on non-absorbable scaffolds. Biomaterials. 2001;22(18):2569–2577. doi: 10.1016/s0142-9612(01)00148-x. [DOI] [PubMed] [Google Scholar]
- 5.Jie W, Yubao L. Tissue engineering scaffold material of nano-apatite crystals and polyamide composite. Eur Polym J. 2004;40:509–515. [Google Scholar]
- 6.Verheyen CCPM, de Wijn JR, van Blitterswijk CA, De Groot K. Evaluation of hydroxylapatite/poly (L-lactide) composites: mechanical behavior. J Biomed Mater Res. 1992;26:1277–1296. doi: 10.1002/jbm.820261003. [DOI] [PubMed] [Google Scholar]
- 7.Ungersbock A, Pohler O, Perren SM. Evaluation of the soft tissue interface at titanium implants with different surface treatments: experiment study on rabbits. Bio-Med Mat Eng. 1994;4(4):317–325. [PubMed] [Google Scholar]
- 8.Behling CA, Spector M. Quantitative characterization of cells at the interface of long-term implants of selected polymers. J Biomed Mater Res. 1986;20(5):653–666. doi: 10.1002/jbm.820200509. [DOI] [PubMed] [Google Scholar]
- 9.Kim HM, Furuya T, Kokubo T, Miyazaki T, Nakamura T. Composition of apatite produced in simulated body fluids. In: Brown S, Clarke I, Williams P, editors. Bioceramics. Vol. 14. Stafa-Zurich, Switzerland: Trans Tech Publications; 2001. pp. 621–624. [Google Scholar]
- 10.Green DW, Walsh D, Mann S, Oreffo ROC. The potential of biomimesis in bone tissue engineering: lessons from the design and synthesis of invertebrate skeletons. Bone. 2002;30(6):810–815. doi: 10.1016/s8756-3282(02)00727-5. [DOI] [PubMed] [Google Scholar]
- 11.Hulbert SF, Morrison SJ, Klawitter JJ. Tissue reaction to three ceramics of porous and non-porous structures. J Biomed Mater Res. 1972;6(5):347–374. doi: 10.1002/jbm.820060505. [DOI] [PubMed] [Google Scholar]
- 12.Vaz L, Lopes AB, Almeida M. Porosity control of hydroxyapatite implants. J Mater Sci Mater Medicine. 1999;10(4):239–242. doi: 10.1023/a:1008910213166. [DOI] [PubMed] [Google Scholar]
- 13.Wang Y, Kim HJ, Vunjak-Novakovic G, Kaplan DL. Stem cellbased tissue engineering with silk biomaterials. Biomaterials. 2006;27(36):6064–6082. doi: 10.1016/j.biomaterials.2006.07.008. [DOI] [PubMed] [Google Scholar]