Abstract
Objective
Examine associations between patient experiences with care and service use across markets.
Data Sources/Study Setting
Medicare fee-for-service (FFS) and managed care (Medicare Advantage [MA]) beneficiaries in 306 markets from the 2003 Consumer Assessments of Healthcare Providers and Systems (CAHPS) surveys. Resource use intensity is measured by the 2003 end-of-life expenditure index.
Study Design
We estimated correlations and linear regressions of eight measures of case-mix-adjusted beneficiary experiences with intensity of service use across markets.
Data Collection/Extraction
We merged CAHPS data with service use data, excluding beneficiaries under 65 years of age or receiving Medicaid.
Principal Findings
Overall, higher intensity use was associated (p<.05) with worse (seven measures) or no better care experiences (two measures). In higher-intensity markets, Medicare FFS and MA beneficiaries reported more problems getting care quickly and less helpful office staff. However, Medicare FFS beneficiaries in higher-intensity markets reported higher overall ratings of their personal physician and main specialist. Medicare MA beneficiaries in higher-intensity markets also reported worse quality of communication with physicians, ability to get needed care, and overall ratings of care.
Conclusions
Medicare beneficiaries in markets characterized by high service use did not report better experiences with care. This trend was strongest for those in managed care.
Keywords: Patient experiences with care, Medicare, small area variations, managed care, utilization
In the current debate about how to control health care costs and improve quality of care, policy makers have been discussing the implications of the considerable geographic variations in health care spending and use (Pear 2009). Patterns of health care use vary substantially across areas of the United States (Wennberg and Gittelsohn 1973) even after controlling for differences in prices and population characteristics (see review in CBO 2008). Areas with higher spending per person have more intensive practice patterns and significantly greater use of “discretionary” services such as office visits, specialist consultations, and tests compared with lower-spending areas (Fisher et al. 2003a,b;).
However, additional spending and use are not related to better technical care, clinical outcomes ( Jencks et al. 2000; Fisher et al. 2003a,b; Jencks, Huff, and Cuerdon 2003; Baicker and Chandra 2004;), or physicians' self-perceived ability to provide high-quality care (Sirovich et al. 2006) across large areas. These findings are consistent for multiple clinical measures, including receipt of evidence-based services such as immunizations and outcomes such as mortality after acute myocardial infarction (Jencks et al. 2000; Fisher et al. 2003a,b; Jencks, Huff, and Cuerdon 2003; Baicker and Chandra 2004;).
However, there is little information about the relationship between treatment intensity and patient experiences with care. Knowing how spending and use are associated with patient experiences, such as the ease of obtaining needed care and being treated with respect by providers, is important to developing and evaluating health care policies (IOM 2001).
Some studies suggest that patient satisfaction is worse in high-use areas, but these relied upon limited measures of patient experiences with care and were restricted to a small sample of enrollees in fee-for-service (FFS) Medicare (Fisher et al. 2003a,b; Fowler et al. 2008;). Nonetheless, it is plausible that the association could go in either direction. In public opinion surveys, Americans place great value on having access to all the care that their providers think they need and fear changes that might restrict access (Blendon et al. 1998). Greater service use may also generate higher ratings of care (Davies and Ware 1988). Such preferences might cause beneficiaries in higher-intensity markets to give better overall ratings of care and their providers, especially in FFS where there are the fewest constraints on utilization of services. Furthermore, delivery of more services could enhance clinicians' knowledge of, and responsiveness to, patient needs and expectations and increase the likelihood of receiving recommended preventative care like vaccinations. High-intensity markets also have more physicians per person overall (Fisher et al. 2003a), potentially enabling easier access to care, shorter waiting times, and longer, less-hurried visits that facilitate better interactions with doctors and office staff.
Alternatively, high-intensity treatment may reflect an inefficient, poorly coordinated local delivery system. Higher-intensity markets have more specialists and fewer primary care providers per person than lower-intensity markets (Fisher et al. 2003a), which may impede access to primary care and foster overreliance on specialists. To accommodate demand, visits may be shortened and interactions with physicians and staff may suffer. An overburdened, uncoordinated system may also increase the likelihood of receiving unnecessary or harmful care. Thus, patients in high-use markets might report less favorable experiences accessing care, interacting with physicians and office staff, and obtaining basic preventative services.
Although Medicare Advantage (MA, Medicare's managed care program) plans could improve patient experiences by coordinating care and providing additional services made possible by higher Medicare reimbursement rates (Gold 2005), we expected that, overall, MA beneficiaries would report worse experiences than FFS beneficiaries in high-intensity areas because managed care restrictions on care would be felt most keenly there. The exception is receipt of flu and pneumonia vaccines, which MA plans have delivered more effectively overall than FFS (Landon et al. 2004).
The majority of Medicare beneficiaries are enrolled in the FFS program, but the growth of MA from 12 percent in 2003 to 22 percent of all Medicare beneficiaries in 2009 (KFF 2009) makes it increasingly important to understand how beneficiaries' experiences in both programs vary with intensity of service use. In this study, we examined whether more intensive use of services is associated with an array of Medicare beneficiary experiences with care, including the ease of accessing care, the quality of interactions with doctors and staff, and overall ratings of care and their providers, in both traditional FFS Medicare and MA.
METHODS
Overview
We examined the relationship between a market's intensity of service use and Medicare beneficiary experiences in 2003 in FFS and MA. Beneficiary experiences were from the CAHPS Medicare surveys of FFS and MA beneficiaries nationwide, which ask about getting needed care, getting care quickly, communication with their physicians, interactions with physician office staff, and receipt of selected preventative care (Goldstein et al. 2001). Intensity of service use in each market was measured by the End-of-Life Expenditure Index (EOL-EI) developed by researchers at Dartmouth Medical School (Fisher et al. 2003a,b;). This intensity index summarizes the market variation in Medicare spending that is not explained by market differences in illness or price. Because much end-of-life care is hospital based, the hospital referral region (HRR) is our unit of analysis. We calculated correlations between the HRR-level intensity index and HRR-level case-mix-adjusted mean CAHPS scores.
CAHPS Survey
The CAHPS surveys of Medicare beneficiaries were designed to assess beneficiaries' overall experiences with care and their experiences in specific areas, such as communication with their physicians and timely access to needed care. Administered to MA beneficiaries since 1997 and FFS beneficiaries since 2000, the CAHPS measures have undergone extensive psychometric testing to assure reliable measures of important dimensions of patient experiences with care; the development and testing of CAHPS have been detailed elsewhere (Schnaier et al. 1999; Zaslavsky, Zaborski, and Cleary 2000c; Zaslavsky et al. 2000a, b, 2001; Zaslavsky 2001; Zaslavsky and Cleary 2002; Hargraves, Hays, and Cleary 2003).
We analyzed 10 measures of beneficiaries' experiences with access and care delivery from the 2003 surveys: overall ratings of (1) doctor, (2) specialist, and (3) care; (4) the ability to get needed care, (5) get care quickly, and (6) being seen within 15 minutes of the scheduled appointment time; (7) their doctor's communication skills, (8) helpfulness of office staff; and receipt of (9) pneumococcal and (10) influenza vaccine (Table 1).
Table 1.
Description of 2003 CAHPS® Composites and Survey Items Used in Analysis
| Measures | Individual Items |
|---|---|
| Get needed care* | Since you joined Medicare, how much of a problem, if any, was it to get a personal doctor or nurse you are happy with? |
| In the last 6 months, how much of a problem, if any, was it to see a specialist that you needed to see? | |
| In the last 6 months, how much of a problem, if any, was it to get the care, tests, or treatment you or a doctor believed necessary? | |
| In the last 6 months, how much of a problem, if any, were delays in health care while you waited for approval from your health plan/Medicare? | |
| Get care quickly† | In the last 6 months, when you called during regular office hours, how often did you get the help or advice you needed? |
| In the last 6 months, when you needed care right away for an illness, injury, or condition, how often did you get care as soon as you wanted? | |
| In the last 6 months, not counting the times you needed health care right away, how often did you get an appointment for health care as soon as you wanted? | |
| Seen in 15 minutes† | In the last 6 months, how often were you taken to the exam room within 15 minutes of your appointment? |
| Doctor's communication† | In the last 6 months, how often did doctors or other health providers listen carefully to you? |
| In the last 6 months, how often did doctors or other health providers explain things in a ways you could understand? | |
| In the last 6 months, how often did doctors or other health providers show respect for what you had to say? | |
| In the last 6 months, how often did doctors or other health providers spend enough time with you? | |
| Helpful and courteous office staff† | In the last 6 months, how often did office staff at a doctor's office or clinic treat you with courtesy or respect? |
| In the last 6 months, how often were office staff at a doctor's office or clinic as helpful as you thought they would be? | |
| Receipt of flu shot‡ | Did you get a flu shot last year, at any time from September to December 2002? |
| Receipt of pneumonia shot‡ | Have you ever had a pneumonia shot? This shot is usually given only once or twice in a person's lifetime and is different than a flu shot. It is also called the pneumococcal vaccine |
| Overall ratings | |
| Doctor§ | Using any number from 0 to 10, where 0 is the worst personal doctor or nurse possible and 10 is the best personal doctor or nurse possible, what number would you use to rate your personal doctor or nurse? |
| Specialist§ | How would you rate the specialist you saw most often in the last 6 months, including a personal doctor if he or she is a specialist? Using any number from 0 to 10, where 0 is the worst specialist possible and 10 is the best specialist possible, what number would you use to rate the specialist? |
| Care§ | Using any number from 0 to 10, where 0 is the worst health care possible and 10 is the best health care possible, what number would you use to rate all your health care in the last 6 months? |
Scale:
Problem (1–3): a big problem, a small problem, not a problem.
Often (1–4): never, sometimes, usually, always.
Yes/No (1, 0): yes, no.
Global (1–10): worst possible (1) to best possible (10).
The overall ratings, being seen within 15 minutes, and vaccination measures are individual items. The others are composite measures previously developed and validated for public reporting of Medicare beneficiary experiences (Zaslavsky et al. 2002; Hargraves, Hays, and Cleary 2003;). All items were scaled so that higher scores indicate more favorable experiences and all items in a composite measure have the same response scale.
Survey Sample and Methods
The FFS survey was administered to a random sample of approximately 600 beneficiaries from each of 275 geographic strata usually comprised of contiguous groups of counties within a state with approximately equal numbers of FFS beneficiaries (RTI and RAND 2005). For the MA survey, a random sample of 600 noninstitutionalized beneficiaries was drawn from each MA contract in effect on July 1, 2003 and for the previous 2 years (or each geographically defined stratum of large contracts) (Goldstein et al. 2001). Beneficiaries sampled from contracts that had ceased activity before the survey and beneficiaries who had left their plan were excluded.
All sampled beneficiaries received the survey by mail with telephone follow-up for nonrespondents (Goldstein et al. 2001; RTI and RAND 2005;). Sampled beneficiaries were sent a letter from the Centers for Medicare and Medicaid Services explaining the purpose of the survey. Spanish-language surveys were sent upon request. Respondents were screened so that they only answered items for which they had relevant care experiences (e.g., only beneficiaries reporting an office visit in the past 6 months were asked about their experience in the doctor's office) (Zaslavsky, Zaborski, and Cleary 2002). This study was approved by the Harvard Medical School Committee on Human Subjects.
Market Definitions and Intensity Index
HRRs are based on patterns of referral for tertiary care, such as major cardiovascular surgery (Wennberg and Cooper 1996). Over 90 percent of all U.S. residents live in HRRs where >80 percent of hospitalizations occur within the HRR (Wennberg and Cooper 1996). Thus, HRRs define distinct areas within which patients' utilization is influenced by a common set of providers.
Our index of intensity of utilization, the 2003 EOL-EI, was calculated for each HRR as the average per capita age, sex, race, and price-adjusted spending on hospital and physician services for FFS Medicare beneficiaries in their last 6 months of life (Fisher et al. 2003a). Because these data were not available for managed care beneficiaries, we used the measure based on FFS beneficiaries to characterize the entire market. The 2003 index was the most recent available and directly corresponded to the time period of our survey.
The index was designed to isolate differences in spending due to variation in service use. It measures market differences in spending associated with overall treatment intensity in a market rather than differences in underlying illness levels or price. The EOL-EI is strongly related to service use in three chronic disease cohorts (acute myocardial infarction, colorectal cancer, and hip fracture) and a general Medicare population cohort, suggesting that the index is reflects general intensity of service use in an area (Fisher et al. 2003a).
People in higher-intensity markets use more “discretionary,” supply-sensitive services, including more frequent physician visits, specialist consultations, lab services, and make greater use of the hospital as a site of care than lower-intensity markets (Fisher et al. 2003a). Research using clinical vignettes has shown a propensity for greater use of these “discretionary” services by physicians in higher-intensity regions (Sirovich et al. 2005).
To assess the robustness of our findings, we also examined relationships between patient experiences and another measure of treatment intensity, the 2003 acute care index (ACI), defined as age-, sex-, race-, price-, and illness-adjusted spending for physician and hospital services in the first 12 months of follow-up for Medicare FFS beneficiaries with acute myocardial infarction, hip fracture, or colon cancer (Fisher et al. 2003a,b;).
Control Variables
CAHPS scores were adjusted for individual characteristics known to be associated with differences in reported experiences, including the beneficiary's age, education, general health status, general mental health status, interactions between age and region and general health status and region, and the use of a proxy to complete the CAHPS survey (Schnaier et al. 1999; Zaslavsky 2001;). Other control variables included federal region, MA penetration, and average Medicare payment. MA penetration in HRRs was calculated by weighting the September 2003 county-level MA penetration rate by the fraction of the HRR's older than 65 population each county represented in the 2000 U.S. Census. HRR payment levels were calculated as the average of each program's payments per person for the counties in each HRR, similarly weighted by population.
Statistical Analysis
We excluded beneficiaries under age 65 and those eligible for Medicaid (14.6 percent of CAHPS respondents) from the analysis because these groups have distinct coverage choices and care needs.
Our unit of analysis was the HRR. Unlike Medicare FFS, MA plans are not available in every market. Of the 306 HRRs nationwide, 199 had MA enrollment and at least 20 CAHPS MA respondents in 2003, representing 99.8 percent of all otherwise eligible MA enrollees; these are the MA markets used in analysis. HRRs were assigned to quintiles based on their intensity index; each quintile contains roughly equal numbers of HRRs (not beneficiaries). Unless the use of quintiles is specifically noted, all analyses and comparisons used the continuous intensity index.
We calculated the case-mix-adjusted mean of each of the CAHPS measures for each HRR using linear regression models (Zaslavsky et al. 2001). Composite measure scores were calculated as the average of all composite items, each item weighted equally (Zaslavsky et al. 2002). The HRR means were weighted to be representative of the corresponding populations: all beneficiaries in all 306 markets, and FFS beneficiaries and MA beneficiaries in the 199 markets with MA plans.
We first examined the association between intensity of service use and patient experiences by estimating correlations and linear regressions of HRR-level case-mix-adjusted CAHPS scores for each population. Controlling for federal region, HRRs' MA penetration, and HRRs' average total Medicare payments did not substantively change the regression results, so these variables were not included in the final model. We tested whether the regression relationships between the intensity index and HRR outcomes were significantly different for FFS and MA. We also calculated effect sizes, defined as the difference between the mean case-mix-adjusted CAHPS scores in the lowest- and highest-spending quintiles of HRRs divided by the pooled standard deviation within quintile. Finally, we repeated our analyses for the entire Medicare population (including beneficiaries under the age of 65 and receiving Medicaid), and substituting the ACI for the EOL-EI, to assess the robustness of our findings.
To determine whether the observed correlations were disproportionately influenced by HRRs in the highest-intensity quintile, we tested whether HRRs in this quintile fit a linear trend by rerunning the regression analyses with a dummy variable representing the highest-intensity quintile of markets. We then estimated correlations between the intensity index and the CAHPS measures for markets in the remaining (lower) quintiles of intensity. Analyses were performed with SAS software, version 9.0 (SAS Institute, Cary, NC).
RESULTS
In 2003, there were 120,974 and 135,757 respondents to the FFS (63.9 percent response rate) and MA (80.2 percent response rate) surveys, respectively, that met our inclusion criteria (Table 2). After weighting the data to be representative of the Medicare program nationally, roughly half of the study population was between 65 and 74 years old, just over half was female, about one-fifth had completed at least some college, one-third reported excellent or very good health, and just over 14 percent was enrolled in MA plans. High-intensity markets spent about 1.5 times the lowest-intensity markets and had more health care resources per capita: 1.17 times the number of physicians, 1.52 the number of specialists, and 1.30 times the hospital beds per person (Table 2). HRRs in the fifth quintile were concentrated in Texas, Pennsylvania, New York, New Jersey, Michigan, Illinois, Florida, and California.
Table 2.
Medicare Beneficiary and Hospital Referral Region Characteristics by Quintile of Service Use Intensity
| Q1 Lowest Use | Q2 | Q3 | Q4 | Q5 Highest Use | Total | |
|---|---|---|---|---|---|---|
| Beneficiary characteristics* | ||||||
| Medicare beneficiaries (over 65, no Medicaid) | 3,946,493 | 4,091,412 | 5,690,426 | 6,236,004 | 8,604,122 | 28,568,456 |
| Program (%) | ||||||
| FFS | 83.4 | 87.0 | 88.2 | 90.0 | 81.8 | 85.8 |
| Medicare Advantage | 16.6 | 13.1 | 11.8 | 10.4 | 18.2 | 14.2 |
| Age (%) | ||||||
| 65–74 | 50.2 | 51.2 | 50.5 | 52.0 | 49.3 | 50.5 |
| 75–84 | 38.1 | 37.4 | 38.2 | 37.7 | 39.0 | 38.2 |
| ≥85 | 11.8 | 11.3 | 11.3 | 10.3 | 11.6 | 11.3 |
| Sex (%) | ||||||
| Male | 44.0 | 43.1 | 43.7 | 43.8 | 43.3 | 43.6 |
| Female | 56.0 | 56.9 | 56.3 | 56.2 | 56.7 | 56.4 |
| Education (%) | ||||||
| High school graduate or less | 53.3 | 58.1 | 59.4 | 58.0 | 55.6 | 56.9 |
| At least some college | 43.2 | 38.2 | 36.6 | 37.7 | 39.9 | 39.0 |
| Missing | 3.5 | 3.7 | 4.0 | 4.2 | 4.5 | 4.1 |
| Health status (%) | ||||||
| Excellent or very good | 34.0 | 32.1 | 30.1 | 30.0 | 31.2 | 31.3 |
| Good | 37.6 | 36.3 | 36.6 | 34.9 | 36.5 | 36.3 |
| Fair or poor | 26.4 | 29.7 | 31.2 | 32.9 | 29.9 | 30.3 |
| Missing | 2.0 | 1.9 | 2.1 | 2.2 | 2.3 | 2.1 |
| Market characteristics | Ratio (highest:lowest) | |||||
| Number of HRRs | 61 | 62 | 61 | 61 | 61 | 306 |
| Intensity index (U.S.$) | 10,817 | 12,419 | 13,657 | 14,734 | 16,991 | 1.54 |
| FFS per capita Medicare spending (U.S.$) | 5,335 | 5,719 | 6,157 | 6,634 | 7,689 | 1.44 |
| Hospital beds per 1,000‡ | 2.3 | 2.7 | 2.8 | 2.9 | 3.0 | 1.30 |
| Physician supply per 100,000‡ | ||||||
| All physicians | 190.9 | 189.1 | 185.5 | 190.8 | 223.2 | 1.17 |
| Primary care physicians | 71.6 | 70.2 | 66.9 | 66.4 | 77.1 | 1.08 |
| Medical specialists | 20.4 | 20.3 | 21.3 | 23.4 | 31.1 | 1.52 |
| Surgeons | 39.1 | 39.8 | 39.9 | 41.6 | 46.9 | 1.20 |
| Other physicians | 59.7 | 58.8 | 57.4 | 59.3 | 68.1 | 1.14 |
| Medicare advantage penetration (%) | 10.3 | 8.2 | 8.0 | 7.0 | 11.6 | 1.13 |
Sample weighted to represent the study population nationally (Medicare beneficiaries, 65 years or older, not receiving Medicaid).
Hospital beds and physician supply are age, sex, race adjusted rates calculated as described in the 1999 Dartmouth Atlas of Health Care (Wennberg and Cooper 1999) for HRRS in a particular quintile.
For all (FFS and MA) beneficiaries across the 306 markets, problems with access to care, including how often beneficiaries were taken to the exam room within 15 minutes of a scheduled appointment (adjusted correlation [R]=−0.64, p<.001), getting care quickly (R=−0.47, p=.05), and getting care when needed (R=−0.12, p<.031) were more frequent in high-intensity areas than in low-intensity markets (Table 3). Beneficiaries in high-intensity markets also more frequently reported problems getting assistance from physician office staff (R=−0.48, p<.001) and with quality of communication with the physician (R=−0.10, p=.01) than those in low-intensity markets (Table 3). Beneficiaries in higher-intensity markets rated their personal physicians more highly than their counterparts in lower-intensity markets (R=+0.23, p<.001), but overall ratings of care and specialist were not significantly related to intensity. Finally, beneficiaries in higher-intensity markets reported receiving of flu (R=−0.46, p<.001) and pneumonia shots (R=−0.49, p<.001) less often (Table 3).
Table 3.
Correlations between 2003 Market Service Use Intensity and Reports of Medicare Beneficiary Experiences with Care*
| All HRRs (n=306) | Medicare MA HRRs (n=199) |
|||||
|---|---|---|---|---|---|---|
| All Beneficiaries† |
FFS Beneficiaries‡ |
MA Beneficiaries‡ |
||||
| Access | R | p-Value | R | p-Value | R | p-Value |
| Getting needed care | −0.12 | .031 | 0.05 | .92 | −0.33 | <.001 |
| Getting care quickly | −0.47 | .05 | −0.47 | <.001 | −0.49 | <.001 |
| Seen in 15 minutes | −0.64 | <.001 | −0.62 | <.001 | −0.59 | <.001 |
| Provider and staff interactions | ||||||
| Doctor's communication | −0.10 | .01 | −0.03 | .70 | −0.22 | .002 |
| Helpful and courteous office staff | −0.48 | <.001 | −0.40 | <.001 | −0.43 | <.001 |
| Preventative care | ||||||
| Pneumonia shot | −0.46 | <.001 | −0.44 | <.001 | −0.48 | <.001 |
| Flu shot | −0.49 | <.001 | −0.47 | <.001 | −0.42 | <.001 |
| Overall ratings | ||||||
| Personal physician | 0.23 | <.001 | 0.37 | <.001 | −0.11 | .13 |
| Specialist | 0.003 | .18 | 0.15 | .04 | −0.20 | <.001 |
| Care | 0.01 | .36 | 0.05 | .45 | −0.24 | <.001 |
Patient experiences were measured by CAHPS measures that were case-mix adjusted. Service use intensity was measured by the intensity index, which was adjusted for prices and local demographics (age, sex, and race).
Sample weighted to represent the study population nationally (Medicare beneficiaries, 65 or older, not receiving Medicaid).
Sample weighted to represent each program.
CAHPS, Consumer Assessments of Healthcare Providers and Systems; FFS, fee-for-service; HRR, hospital referral region; MA, Medicare Advantage.
Table 3 also shows analyses stratified by Medicare sector. Findings for FFS beneficiaries in the 199 markets with MA enrollment were similar to those in the combined analyses. As indicated by the correlations, effect sizes for differences between the highest and lowest spending markets for FFS beneficiaries were greatest for being taken to the exam room within 15 minutes of their appointment (2.47), how helpful office staff were (1.38), and overall rating of their personal physician (1.03) (Table 4).
Table 4.
Effect Size for Lowest versus Highest Quintiles of Service Use Intensity in Medicare MA HRRs*
| FFS |
Medicare MA |
|||||
|---|---|---|---|---|---|---|
| Mean CAHPS Score† |
Mean CAHPS Score† |
|||||
| Lowest Quintile Of Intensity (Q1) | Highest Quintile Of Intensity (Q5) | Effect Size* | Lowest Quintile Of Intensity (Q1) | Highest Quintile Of Intensity (Q5) | Effect Size* | |
| Patient experiences | ||||||
| Access | ||||||
| Getting needed care | 2.84 | 2.84 | 0.09 | 2.83 | 2.71 | −1.33 |
| Getting care quickly | 3.66 | 3.62 | −0.46 | 3.64 | 3.49 | −1.20 |
| Seen in 15 minutes | 2.91 | 2.58 | −2.47 | 2.98 | 2.59 | −2.07 |
| Provider and staff interactions | ||||||
| Doctor's communication | 3.64 | 3.63 | −0.27 | 3.64 | 3.57 | −0.68 |
| Helpful and courteous office staff | 3.80 | 3.74 | −1.38 | 3.80 | 3.67 | −1.47 |
| Preventative care | ||||||
| Pneumonia shot | 0.70 | 0.63 | −1.16 | 0.77 | 0.66 | −1.45 |
| Flu shot | 0.76 | 0.69 | −1.30 | 0.80 | 0.73 | −1.17 |
| Overall ratings | ||||||
| Personal physician | 8.73 | 8.89 | 1.03 | 8.77 | 8.70 | −0.29 |
| Specialist | 8.80 | 8.86 | 0.28 | 8.76 | 8.57 | −0.52 |
| Care | 8.93 | 8.93 | 0.03 | 8.85 | 8.61 | −0.76 |
Effect size is the difference between the mean case-mix-adjusted CAHPS scores in the lowest- and highest-spending quintiles divided by the pooled standard deviation within quintile. Positive sign indicates better performance in highest-spending quintile than lowest; negative sign indicates the opposite. The analysis is based on 40 HRRs each in the lowest- and highest-intensity quintiles.
Patient experiences were measured by CAHPS measures, which have been case-mix adjusted. Responses were weighted to represent each program, and the figures presented have been rounded to the nearest hundredth.
CAHPS, Consumer Assessments of Healthcare Providers and Systems; FFS, fee-for-service; HRR, hospital referral region; MA, Medicare Advantage.
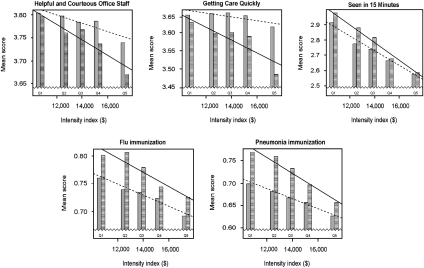
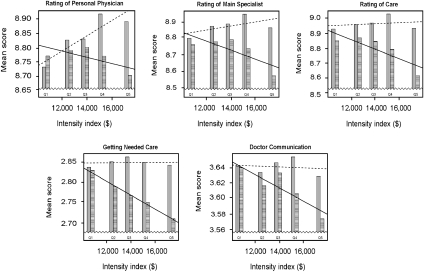
MA beneficiaries in higher-intensity markets, however, reported worse experiences than those in lower-intensity markets for almost every measure (Table 3 and Figures 1 and 2). Like FFS respondents, MA beneficiaries in higher-intensity markets had more difficulty getting care quickly (R=−0.33), being taken to the exam room within 15 minutes of their appointment (R=−0.59), and getting help and respectful treatment by office staff (R=−0.43) than their MA counterparts in lower-intensity markets (p<.0001 for all). Unlike FFS beneficiaries, however, MA beneficiaries in higher-intensity markets also reported lower overall ratings of their specialist (R=−0.20, p<.001) and care overall (R=−0.24, p<.001), as well as worse communication with their doctor (R=−0.22, p<.002) and more delays getting care while waiting for approval from their health plan (R=−0.33, p<.001) than MA beneficiaries in low-intensity markets. Effect sizes for differences between the highest- and lowest-spending quintiles for MA beneficiaries were greatest for being taken to the exam room within 15 minutes of their appointment (2.07), helpfulness of office staff (1.47), and getting needed care (1.33) (Table 4).
Figure 1.
Patient Reported Experiences Negatively Related to Intensity of Service Use in Medicare Advantage (MA) and Fee-for-Service (FFS)
Figure 2.
Patient Reported Experiences Negatively Related to Intensity of Service Use in Medicare Advantage (MA) But Not Fee-for-Service (FFS)
In general, the difference between the average FFS and MA beneficiary experience is larger in high-intensity markets than in lower-intensity markets, where patient-reported experiences are relatively similar (Figure 2). For almost all measures across all markets FFS performance is better than MA performance (Figure 1). The exceptions were, “How often were you taken to the exam room within 15 minutes of your appointment?” and receipt of pneumonia and flu vaccines; for these, MA beneficiaries report more favorable experiences than FFS beneficiaries across levels of intensity (Figure 2).
Sensitivity analysis revealed that beneficiaries in markets in the highest quintile of intensity reported significantly poorer experiences for five measures (overall ratings of personal physician, specialist, care, getting care quickly, and helpful and courteous office staff) than would be expected from the trend across the rest of the markets in one or both of the programs. This poor performance in the top quintile of markets does not appear to be due to a small set of outlying poorly scoring areas because standard deviations of area means were fairly similar across quintiles of intensity.
Correlations of patient experiences with the ACI were similar to those with the EOL-EI intensity index, although in some cases they were smaller. Including beneficiaries under the age of 65 and Medicaid eligibles yielded similar relationships between experiences and intensity of care with the exception of getting care quickly, whose correlations became insignificant among the overall Medicare population (R=−0.10, p=.071) and FFS beneficiaries in markets with MA (R=−0.10, p=.146).
DISCUSSION
At the heart of the national health care debate is how to improve quality and control spending. In this paper, we asked if the finding that more use is associated with worse clinical care and outcomes was also true from the patient's perspective. Theoretically, patients could have better care experiences in higher-intensity markets, but we found that higher service use was not associated with better care experiences, with the exception of higher overall ratings of their personal physician.
Access to care, interactions with office staff and physician communication were significantly worse in higher-intensity markets, and beneficiaries in these markets more frequently had to wait over 15 minutes past their scheduled appointment time at the physician's office and were less likely to report having received recommended vaccines. This is consistent with physicians' reports in high-intensity markets that they are less able to provide high-quality care to patients compared with physicians in lower-intensity markets (Sirovich et al. 2006).
The strong negative relationship between service use intensity and access to care measures could result from the increased provision of nonessential services in higher-intensity markets. This increased use may limit the availability of providers to deliver essential services, making it more difficult for beneficiaries to see physicians for routine care. Furthermore, there might be a greater mismatch between desired and provided services in higher-intensity areas because beneficiaries there expect to receive more services. At least for some measures, the negative effects associated with patterns of intense service use appear especially strong in the highest use markets, which may reflect larger gaps in beneficiary expectations, or particularly uncoordinated or stressed delivery systems that negatively affect all Medicare beneficiary experiences. This is especially important because the highest spending markets represent 30 percent of our study population and may provide the biggest opportunity to control costs.
As expected, higher intensity of service use was more strongly associated with worse reports of care experiences among MA beneficiaries than in FFS. In addition to worse access to care and interactions with office staff, MA beneficiaries in higher-intensity markets reported more problems getting care when needed and finding a satisfactory provider than MA beneficiaries in lower-intensity markets. Furthermore, MA beneficiaries reported worse patient experiences than their FFS counterparts in the same markets, except for delivery of flu and pneumonia vaccines, consistent with earlier research (Landon et al. 2004). These results are even more striking considering that MA enrollment is voluntary, and those who enroll are likely to be those who most value extra MA plan benefits relative to FFS freedom of choice. The differences in reported care experiences were small, but significant, in the low-intensity markets, and larger in high-intensity markets. This provides some insight into possible sources of previously identified state-to-state variations in patient experiences (Landon et al. 2004; Zaslavsky, Zaborski, and Cleary 2004;).
Patient reports may be particularly poor for MA beneficiaries in higher-intensity markets because MA plans entering “inefficient” markets may try to profit by reducing service use (Brown and Gold 1999; MedPAC 2001;), and high-intensity markets are characterized by greater use of “discretionary” services, making these areas an attractive target. If MA beneficiaries in high-intensity markets feel plan changes to manage or restrict care most keenly—compared with their own previous experience or that of their neighbors in FFS Medicare—they might report worse care, regardless of its technical quality. This difference in expectations could also explain why, unlike FFS beneficiaries, MA beneficiaries were not more satisfied with their personal provider in higher-intensity markets. Nonetheless, beneficiaries have been drawn to MA plans because they offered more generous benefits and lower premiums and cost-sharing than FFS Medicare or private supplemental coverage (Atherly, Dowd, and Feldman 2004; Gold et al. 2004;).
Our study has several limitations. First, the data used were from 2003. Since then, the MA program has expanded the array of plan choices available to beneficiaries to include, among others, private fee-for-service, preferred provider organizations, and prescription drug plans. We cannot extrapolate our findings to those enrolled in these alternative models, because 90 percent of Medicare-managed care beneficiaries nationwide were enrolled in health maintenance organization (HMO) plans in 2003 (KFF 2009).
Second, this paper assessed only some dimensions of health care quality. MA may outperform FFS on other dimensions. For example, our analyses and those by Landon et al. (2004) have found MA plans deliver preventative care at higher rates than FFS providers. Third, our data on service intensity were based on FFS use, but MA delivery patterns could differ. Because plans with exclusive provider relationships constitute a minority of managed care plans, Medicare beneficiaries likely share many of the same providers. Although we could not control for provider overlap, we found that FFS and MA experiences often diverge, suggesting that differences in practice patterns in the two programs may explain some of variation observed.
Fourth, CAHPS measures focus on reports about experiences with care and many are relatively objective, such as whether a patient was seen within 15 minutes of his or her scheduled appointment time and received flu and pneumonia vaccinations. However, many reports about care experiences might be influenced by expectations. The case-mix adjustment model removes such effects related to age, reported health status, and education, but some measures may still reflect differences in expectations to some extent. Fifth, we could not distinguish the roles of patient demand and underlying market and organizational factors in determining treatment intensity, although recent work indicates that patient preferences account for only a very small amount of area variation in use (Anthony et al. 2009). Sixth, we selected the intensity index over alternative utilization measures. The index is highly correlated with an HRR's average Medicare FFS (R=+0.80, p<.001) and MA payment levels (R=+0.61, p<.001), but it was designed to more effectively control for area differences in underlying illness to isolate spending variation linked to area practice patterns than other measures.
Finally, HRR-level associations might differ from those within HRRs. For instance, within an HRR, patients who use more services might report better experiences. Hence, our results should be interpreted as characterizing system-level associations at the geographical level relevant to inpatient care, not those for individual patients or smaller areas. We doubt that our findings are substantially confounded by variations in patient case-mix at this level. Our methods minimized potential confounding by studying Medicare beneficiaries, who by definition are all insured, excluding Medicaid eligibles and those under 65, and case-mix adjusting for factors known to be associated with differences in patient experiences (Schnaier et al. 1999; Zaslavsky et al. 2001;). Case-mix only accounts for a small portion of differences in patient experiences (Zaslavsky, Zaborski, and Cleary 2000c), so it is unlikely that additional adjustment would result in substantial changes. Further study of area characteristics associated with costs and quality might elucidate the reasons for the associations we found.
Our findings are important given policy makers' desire to improve the efficiency and quality of the Medicare program (Weems 2008; Pear 2009;). Under the current system, more Medicare spending has not been producing higher-quality care for beneficiaries on average. Our findings are consistent with the argument that high spending in some areas reflects wasteful and/or poorly coordinated care. Managed care is particularly unpopular (Robinson 2001) and more of the same is unlikely to improve care. The current alternative types of MA plans are less managed than HMOs and more generously reimbursed per enrollee than HMOs and FFS, suggesting that enrollment growth in these alternatives is unlikely to improve efficacy or reduce spending differences (MedPAC 2008).
In sum, our work and others' (Fisher et al. 2003a,b; Anthony et al. 2009;) suggest that higher use and poorer quality are rooted in local delivery system problems. The highest-intensity markets provide the biggest opportunity to control costs and improve quality of care. These areas reported the worst patient experiences and generate a disproportionate share of costs. Policy makers cannot rely on the current program structure to transform markets, and administratively cutting spending in high-intensity areas is likely to hurt quality and arouse intense opposition. More effective policy tools now receiving the most attention include payment reforms such as a bundled payments for care episodes; increasing the number of primary care providers; greater use of integrated organizations; development of accountable care organizations; adopting enhanced systems of primary care, like the medical home; and expanding the use of comparative effectiveness guidelines (Iglehart 2008a,b; Crosson 2009; Fisher et al. 2009; Mechanic and Altman 2009; Wilensky 2009;). Regardless of the options pursued, innovative Medicare policy and approaches to health care delivery are required to improve access to needed services while reducing wasteful and redundant care.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This work was supported by a contract (500-01-0020) from the Centers for Medicare & Medicaid Services to Westat/Harvard University. Jessica Mittler also received financial support from an Alfred P. Sloan Foundation dissertation fellowship. The authors gratefully acknowledge the technical assistance provided by Matthew Cioffi, Larry Zaborski, Kristen Bronner, and thoughtful feedback provided by participants in the Harvard Health Policy research seminar.
Disclosures: None.
Disclaimers: None.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Appendix SA2: Patient Reported Experiences by Intensity Index Quintiles in Fee-for-Service (FFS) and Medicare Advantage (MA), 2003.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- Anthony DL, Herndon MB, Gallagher PM, Barnato AE, Bynum JP, Gottlieb DJ, Fisher ES, Skinner JS. How Much Do Patients' Preferences Contribute to Resource Use? Health Affairs. 2009;28(3):864–73. doi: 10.1377/hlthaff.28.3.864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atherly A, Dowd BE, Feldman R. The Effect of Benefits, Premiums, and Health Risk on Health Plan Choice in the Medicare Program. Health Services Research. 2004;39(4, part I):847–64. doi: 10.1111/j.1475-6773.2004.00261.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baicker K, Chandra A. Medicare Spending, the Physician Workforce, and Beneficiaries' Quality of Care. Health Affairs W4. 2004:W184–97. doi: 10.1377/hlthaff.w4.184. Web Exclusive. [DOI] [PubMed] [Google Scholar]
- Blendon RJ, Brodie M, Benson JM, Altman DE, Levitt L, Hoff T, Hugick L. Understanding the Managed Care Backlash. Health Affairs. 1998;17(4):80–94. doi: 10.1377/hlthaff.17.4.80. [DOI] [PubMed] [Google Scholar]
- Brown RS, Gold MR. What Drives Medicare Managed Care Growth? Health Affairs. 1999;18(6):140–9. doi: 10.1377/hlthaff.18.6.140. [DOI] [PubMed] [Google Scholar]
- Congressional Budget Office (CBO). Geographic Variation in Health Care Spending. Washington, DC: Congressional Budget Office; 2008. [Google Scholar]
- Crosson FJ. Medicare: The Place to Start Delivery System Reform. Health Affairs. 2009;2009(28):w232–4. doi: 10.1377/hlthaff.28.2.w232. [DOI] [PubMed] [Google Scholar]
- Davies AR, Ware JE. Involving Consumers in Quality of Care Assessment. Health Affairs. 1988;7(1):33–48. doi: 10.1377/hlthaff.7.1.33. [DOI] [PubMed] [Google Scholar]
- Fisher ES, McClellan MB, Bertko J, Lieberman SM, Lee JJ, Lewis JL, Skinner JS. Fostering Accountable Health Care: Moving Forward in Medicare. Health Affairs. 2009;28(2):w219–31. doi: 10.1377/hlthaff.28.2.w219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher ES, Wennberg DE, Stukel TA, Gottlieb MS, Lucas FL, Pinder EL. The Implications of Regional Variations in Medicare Spending, Part 1: The Content, Quality, and Accessibility of Care. Annals of Internal Medicine. 2003a;138(4):273–88. doi: 10.7326/0003-4819-138-4-200302180-00006. [DOI] [PubMed] [Google Scholar]
- Fisher ES. The Implications of Regional Variations in Medicare Spending, Part 2: Health Outcomes and Satisfaction with Care. Annals of Internal Medicine. 2003b;138(4):288–99. doi: 10.7326/0003-4819-138-4-200302180-00007. [DOI] [PubMed] [Google Scholar]
- Fowler FJ, Gallagher PM, Anthony DL, Larsen K, Skinner JS. Relationship between Regional Per Capita Medicare Expenditures and Patient Perceptions of Quality of Care. Journal of the American Medical Association. 2008;299(20):2406–12. doi: 10.1001/jama.299.20.2406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold M. Private Plans in Medicare: Another Look. Health Affairs. 2005;24(5):1302–10. doi: 10.1377/hlthaff.24.5.1302. [DOI] [PubMed] [Google Scholar]
- Gold M, Achman L, Mittler J, Stevens B. Monitoring Medicare+Choice: What Have We Learned? Findings and Operational Lessons for Medicare Advantage. Washington, DC: Mathematica Policy Research; 2004. [Google Scholar]
- Goldstein E, Cleary PD, Langwell KM, Zaslavsky AM, Heller A. Medicare Managed Care CAHPS®: A Tool for Performance Improvement. Health Care Financing Review. 2001;22:101–7. [PMC free article] [PubMed] [Google Scholar]
- Hargraves JL, Hays RD, Cleary PD. Psychometric Properties of the Consumer Assessment of Health Plans Study (CAHPS®) 2.0 Adult Core Survey. Health Services Research. 2003;38(6, part 1):1509–27. doi: 10.1111/j.1475-6773.2003.00190.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iglehart JK. Medicare, Graduate Medical Education, and New Policy Directions. New England Journal of Medicine. 2008a;359(6):643–50. doi: 10.1056/NEJMhpr0803754. [DOI] [PubMed] [Google Scholar]
- Iglehart JK. No Place Like Home—Testing a New Model of Care Delivery. New England Journal of Medicine. 2008b;359(12):1200–2. doi: 10.1056/NEJMp0805225. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (IOM). Crossing the Quality Chasm: A New Health System for the 21st Century. Report Brief. Washington, DC: National Academy Press; 2001. [Google Scholar]
- Jencks SF, Cuerdon T, Burwen DR, Fleming B, Houck PM, Kussmaul AE, Nilasena DS, Ordin DL, Arday DR. The Quality of Medical Care Delivered to Medicare Beneficiaries: A Profile at State and National Levels. Journal of the American Medical Association. 2000;284(13):1670–6. doi: 10.1001/jama.284.13.1670. [DOI] [PubMed] [Google Scholar]
- Jencks SF, Huff ED, Cuerdon T. Change in the Quality of Medical Care Delivered to Medicare Beneficiaries, 1998–1999 to 2000–2001. Journal of the American Medical Association. 2003;289(3):305–12. doi: 10.1001/jama.289.3.305. [DOI] [PubMed] [Google Scholar]
- Kaiser Family Foundation (KFF). 2009. “Medicare Health and Prescription Drug Plan Tracker” [accessed July 22, 2009]. Available at http://www.kff.org/medicare/healthplantracker.
- Landon BE, Zaslavsky AM, Bernard SL, Cioffi MJ, Cleary PD. A National Comparison of the Performance of Traditional Medicare and Medicare Managed Care. Journal of the American Medical Association. 2004;291(14):1744–52. doi: 10.1001/jama.291.14.1744. [DOI] [PubMed] [Google Scholar]
- Mechanic D, Altman S. Payment Reform Options: Episode Payment Is a Good Place to Start. Health Affairs. 2009;28:w262–71. doi: 10.1377/hlthaff.28.2.w262. [DOI] [PubMed] [Google Scholar]
- Medicare Payment Advisory Commission (MedPAC). Report to Congress: Medicare in Rural America. Washington, DC: MedPAC; 2001. Bringing Medicare+Choice to Rural America; pp. 115–23. [Google Scholar]
- Medicare Payment Advisory Commission (MedPAC). 2008. Private FFS Plans in Medicare Advantage. Testimony of Mark Miller, Executive Director MedPAC, before the Committee on Finance, U.S. Senate, January 30.
- Pear R. 2009. “Health Care Spending Disparities Stir a Fight.”The New York Times, June 9.
- Research Triangle International (RTI) and RAND. 2005. Implementation of Medicare CAHPS®FFS Survey. Final Report for the 2003 Survey [accessed March 1, 2010]. Available at http://www.cms.hhs.gov/CAHPS/Downloads/03_2003FFSCAHPSDataCollectionMethodsRPT.pdf.
- Robinson JC. The End of Managed Care. Journal of the American Medical Association. 2001;285(20):2622–8. doi: 10.1001/jama.285.20.2622. [DOI] [PubMed] [Google Scholar]
- Schnaier JA, Sweeny SF, Williams VS, Kosiak B, Lubalin JS, Hays RD, Harris-Kojetin LD. Special Issues Addressed in the CAHPS® Survey of Medicare Managed Care Beneficiaries. Medical Care. 1999;37(3, suppl):69–78. doi: 10.1097/00005650-199903001-00008. [DOI] [PubMed] [Google Scholar]
- Sirovich BE, Gottlieb DJ, Welch HG, Fisher ES. Variation in the Tendency of Primary Care Physicians to Intervene. Archives of Internal Medicine. 2005;165(19):2252–6. doi: 10.1001/archinte.165.19.2252. [DOI] [PubMed] [Google Scholar]
- Sirovich BE. Regional Variations in Health Care Intensity and Physician Perceptions of Quality of Care. Annals of Internal Medicine. 2006;144(9):641–6. doi: 10.7326/0003-4819-144-9-200605020-00007. [DOI] [PubMed] [Google Scholar]
- Weems K. 2008. The Structure and Costs of the Medicare Advantage Program. Testimony of the Acting Administration Centers for Medicare & Medicaid Services before the House Ways & Means Subcommittee on Health, February 28.
- Wennberg JE, Cooper MM. The Quality of Medical Care in the United States: A Report on the Medicare Program. The Dartmouth Atlas of Health Care in the United States. Chicago: American Health Association Press; 1996. [PubMed] [Google Scholar]
- Wennberg JE. The Quality of Medical Care in the United States: A Report on the Medicare Program. The Dartmouth Atlas of Health Care in the United States. Chicago: American Health Association Press; 1999. [PubMed] [Google Scholar]
- Wennberg JE, Gittelsohn A. Small Area Variations in Health Care Delivery. Science. 1973;182:1102–8. doi: 10.1126/science.182.4117.1102. [DOI] [PubMed] [Google Scholar]
- Wilensky GR. The Policies and Politics of Creating a Comparative Clinical Effectiveness Research Center. Health Affairs. 2009;28(4):w719–29. doi: 10.1377/hlthaff.28.4.w719. [DOI] [PubMed] [Google Scholar]
- Zaslavsky AM. Statistical Issues in Reporting Quality Data: Small Samples and Case Mix Variation. International Journal of Quality in Health Care. 2001;13(6):481–8. doi: 10.1093/intqhc/13.6.481. [DOI] [PubMed] [Google Scholar]
- Zaslavsky AM, Beaulieu ND, Landon BE, Cleary PD. Dimensions of Consumer-Assessed Quality of Medicare Managed Care Health Plans. Medical Care. 2000a;38(2):162–74. doi: 10.1097/00005650-200002000-00006. [DOI] [PubMed] [Google Scholar]
- Zaslavsky AM, Cioffi MJ, Cleary PD, Ding L, Shaul JA, Zaborski LB. Adjusting Performance Measures to Ensure Equitable Plan Comparisons. Health Care Financing Review. 2001;22(3):109–26. [PMC free article] [PubMed] [Google Scholar]
- Zaslavsky AM, Cleary PD. Dimensions of Plan Performance for Sick and Healthy Members on the Consumer Assessments of Health Plans Study 2.0 Survey. Medical Care. 2002;40(10):951–64. doi: 10.1097/00005650-200210000-00012. [DOI] [PubMed] [Google Scholar]
- Zaslavsky AM, Landon BE, Beaulieu ND, Cleary PD. How Consumer Assessments of Managed Care Vary within and among Markets. Inquiry. 2000b;37(2):146–61. [PubMed] [Google Scholar]
- Zaslavsky AM, Shaul JA, Zaborski LB, Cioffi MJ, Cleary PD. Combining Health Plan Performance Indicators into Simpler Composite Measures. Health Care Financing Review. 2002;23(4):101–15. [PMC free article] [PubMed] [Google Scholar]
- Zaslavsky AM, Zaborski L, Cleary PD. Does the Effect of Respondent Characteristics on Consumer Assessments Vary across Health Plans? Medical Care Research and Review. 2000c;57:379–94. doi: 10.1177/107755870005700307. [DOI] [PubMed] [Google Scholar]
- Zaslavsky AM, Zaborski LB, Cleary PD. Factors Affecting Response Rates to the Consumer Assessment of Health Plans Survey. Medical Care Research and Review. 2002;57(3):485–99. doi: 10.1097/00005650-200206000-00006. [DOI] [PubMed] [Google Scholar]
- Zaslavsky AM. Plan, Geographical, and Temporal Variation of Consumer Assessments of Ambulatory Health Care. Health Services Research. 2004;39(5):1467–85. doi: 10.1111/j.1475-6773.2004.00299.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.