Abstract
Objective
To analyze nursing home utilization patterns in order to identify potential targeting criteria for transitioning residents back to the community.
Data Sources
Secondary data from minimum data set (MDS) assessments for an annual cohort of first-time admissions (N=24,648) to all Minnesota nursing homes (N=394) from July 2005 to June 2006.
Study Design
We conducted a longitudinal analysis from admission to 365 days. Major MDS variables were discharge status; resident's preference and support for community discharge; gender, age, and marital status; pay source; major diagnoses; cognitive impairment or dementia; activities of daily living; and continence.
Principal Findings
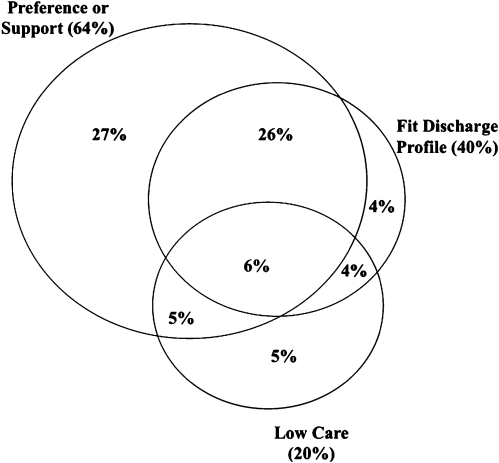
At 90 days the majority of residents showed a preference or support for community discharge (64 percent). Many had health and functional conditions predictive of community discharge (40 percent) or low-care requirements (20 percent). A supportive facility context, for example, emphasis on postacute care and consumer choice, increased transition rates.
Conclusions
A community discharge intervention could be targeted to residents at 90 days after nursing home admission when short-stay residents are at risk of becoming long-stay residents.
Keywords: Outcome, community care, consumer preference, length of stay, quality of care
Efforts are underway in Minnesota and other states to shift the balance of long-term care resources from institutional to community-based long-term care (Kaye, LaPlante, and Harrington 2009). States have been engaged for a number of years in preadmission screening programs and other initiatives aimed at diverting persons from nursing homes (Summer 2005). Recently, attention has been given to promoting community transitions for persons residing in nursing homes who wish to be in a community setting and who can reasonably be served there. The federal government's Money Follows the Person (MFP) Demonstration (CMS 2007) as well as many state-initiated programs have attempted to facilitate discharge from nursing home to community (Kasper and O'Malley 2006a,b;).
Minnesota is in the process of implementing a new Community Transitions Program to facilitate community transitions for short-stay nursing home residents who are at risk of becoming long-stay residents. The program will promote timely return to the community early in a resident's nursing home stay (e.g., 3 months after admission) and, if possible, before Medicaid conversion and personal or family resources are exhausted. An important component of the Community Transitions Program is a strategy for targeting residents for community discharge. We undertook this study to better understand the factors affecting community discharges and to design an operational targeting approach that could be based on readily available administrative data. Our objectives were to (1) select a targeting window or stage in a resident's nursing home stay that would be optimal for a community discharge intervention; (2) develop targeting criteria from resident characteristics indicating a high probability of community discharge, low nursing home resource requirements, and, perhaps most importantly, a preference for returning to the community and a family member or other person supportive of that preference; and (3) examine facility characteristics that affect transition to the community and may play a role in targeting. Data for the analysis come from Minimum Data Set (MDS) assessments, which are performed for all nursing home residents at admission and periodically thereafter.
TARGETING WINDOW
Most transitions in the current system of care, absent a transition intervention, occur early on in the resident's stay and result in discharge back to the community. Many nursing home residents are admitted for rehabilitation and/or recuperation or they are in the latter stages of a terminal illness; they either return to the community or die after a short stay in the facility. A relatively small proportion of admissions become long stays, remaining in the nursing home for months or years (Reschovsky 1998; Jones 2002; Kasper 2005; Gill et al. 2009;). The longer one remains in the nursing home, however, the less the likelihood of a community transition (Coughlin, McBride, and Liu 1990b; Mehdizadeh 2002; Chapin et al. 2009;). Ideally, the window for an intervention would be that period between the short and long stay. An untargeted intervention too early in the nursing home stay can lead to inefficiencies where residents and their caregivers may not need help and they would likely transition to the community on their own without an intervention (Newcomer, Kang, and Graham 2006). Long-stay residents may be difficult to transition if they have exhausted assets, settled into the institution, and broken off community ties. Less than 6 percent of Medicaid-eligible persons in nursing homes for 6 months or more transition to the community each year (Wenzlow and Lipson 2009).
PREDICTORS OF COMMUNITY DISCHARGE
Targeting for community transitions should also consider personal, health, and functional conditions that increase the probability of community discharge (Kasper 2005). Previous studies found that community discharge was most likely for residents who were younger (Murtaugh 1994; Mehr, Williams, and Fries 1997; Chapin et al. 1998;), male (Engle and Graney 1993; Murtaugh 1994;), non-Medicaid pay source (Engle and Graney 1993; Murtaugh 1994; Chapin et al. 1998;), continent (Murtaugh 1994), minimally dependent in ADLs (Nyman et al. 1989; Coughlin, McBride, and Liu 1990a; Engle and Graney 1993; Murtaugh 1994; Mehr, Williams, and Fries 1997;), cognitively intact or only mildly impaired (Coughlin, McBride, and Liu 1990a; Engle and Graney 1993; Chapin et al. 1998;), absent behavioral problems (Murtaugh 1994), and admitted with a hip or other fracture (Liu, McBride, and Coughlin 1994; Cumming, Klineberg, and Katelaris 1996;). We also would expect facilities admitting higher percentages of Medicare postacute residents or those receiving therapies to have higher community discharge rates (Kane et al. 1996; Arling, Williams, and Kopp 2000; Jette, Warren, and Wirtalla 2004;).
LOW CARE REQUIREMENTS
In addition, targeting should take into account residents with low need for nursing or other care resources who might be good candidates for community care (Buttar, Blaum, and Fries 2001). Mor et al. (2007) estimated the percentage of nursing home residents nationally and by state who were what they termed “low care”. They developed definitions of low care from the Resource Utilization Group (RUG-III) resident classification system (Fries et al. 1994; Arling et al. 2007;). Residents meeting their broad definition of low care are as follows: (a) fell into one the lowest RUG-III groups, that is, Impaired Cognition, Behavioral Problems, or Physical Function Reduced (Physical); and (b) were independent or required only minimal supervision with eating, transferring, bed mobility, or hygiene activities of daily living (ADLs). Narrowly defined low-care residents met the same ADL criteria but were restricted to the RUG Physical groups. In an annual admission cohort with stays of approximately 90 days, 8.4 percent of residents in Minnesota (5.2 percent nationally) met the narrow definition of low care and 15.3 percent met the broad definition (13.5 percent nationally). Among residents staying 90 days or more during the year, 7.7 percent in Minnesota (5.1 percent nationally) met the narrow definition and 12.4 percent the broad definition (11.8 percent nationally). Thus, Minnesota appears to be slightly higher than the national average in percentage of residents in low-care categories. Many of these residents could be candidates for community transitions.
PREFERENCES AND SUPPORT FOR COMMUNITY DISCHARGE
Probably the most important consideration in discharge from the nursing home is the resident's preference to return to the community and the availability of someone who supports that preference. Individuals' expectations about nursing home use and availability of formal and informal community support influence their risk of nursing home admission (Boaz and Muller 1994; Freedman 1996; Lindrooth, Hoerger, and Norton 2000; Gaugler, Kane, and Newcomer 2007;). Yet little research has been conducted into how these factors influence transitions back into the community or success in remaining there (Howell et al. 2007). A move to a nursing home may mean giving up community housing and supportive arrangements. The longer a person stays in a nursing home, the fewer community resources are likely to be intact (Kasper and O'Malley 2006a). Some persons entering nursing homes may have a clear intent for short or long stay, but many may be undecided. Once admitted, the length of the nursing home stay can be difficult to predict. The individual's health may improve or deteriorate; attitudes change; and family and community support systems fluctuate.
METHODS
Study Sample
We created an MDS analysis file of all first-time nursing home admissions (N=24,648) to Minnesota nursing facilities from July 1, 2005 to June 30, 2006. We excluded nursing home transfers (10 percent of all admissions) and persons with nursing home use in the prior 2 years (27 percent of all admissions). The first-time admission cohort was followed to the point of discharge or for a maximum of 365 days of residence in a nursing home. Discharge status taken from the MDS was collapsed into major categories: community discharge (private home/apartment with no home health services, private home/apartment with home health services, or board and care/assisted living), discharged to another institution (nursing facility, acute-care hospital, other facility, psychiatric hospital, MR/DD facility, rehabilitation hospital, or other), and deceased. Discharge status was missing for only 1.7 percent of admissions having a valid discharge date; these cases were excluded from the analysis.
Variables
Study variables came from admission, quarterly (90, 180, and 270 days), significant change or annual MDS assessments. They included age, gender, marital status, and living alone before admission as well as diagnoses and problem conditions such as Alzheimer's or dementia, psychiatric disorder (schizophrenia or anxiety disorder), depression, diabetes, hip fracture, cancer, end-stage disease, and bowel or bladder continence. The MDS was also used to group residents into major RUG-III categories of Extensive Services (Extensive), Rehabilitation, Special Care, and Clinically Complex, which served as general indicators of health conditions or service use (Fries et al. 1994). Dependency in ADLs was measured with the ADL long-form index, ranging from 0 (independent) to 28 (totally dependent) (Morris, Fries, and Morris 1999). Cognitive impairment was measured with the Cognitive Performance Scale (CPS) with a range of 0 (intact) to 6 (very severely impaired) (Morris et al. 1994). The problem behavior variable (scored yes or no) was based on one or more problem behaviors (resists care, verbally abusive, physically abusive, or socially inappropriate) exhibited at least weekly. The primary pay source for the per diem payment was assigned at each MDS assessment according to assessment type, MDS pay source check box, and presence of a Medicaid number. We also constructed facility-level variables that were aggregates of the resident-level variables: proportion of admissions on Medicare, from an acute-care hospital, having a preference to return to the community, and falling into a major RUG-III category of Extensive or Rehabilitation, indicating a need for postacute care.
Low care was defined as falling into one of the RUG-III groups with minimal ADL dependence, including residents who were cognitively impaired (IA1 or IA2) or had behavioral problems (BA1 or BA2) as well as residents without these conditions (PA1, PA2). Measures of community discharge preference and support were taken from MDS item Q1a –“Resident expresses/indicates preference to return to the community” (yes/no) and Q1b –“Resident has a support person who is positive toward discharge” (yes/no) measured at admission to the nursing home. Nursing home staff members were instructed in the MDS manual to “ask the resident directly” in answering items Q1a and Q1b; however, we do not know how much answers were influenced by staff's own assessment of the person's wishes or potential for discharge, family preferences, or degree of cognitive impairment or communication deficits displayed by the resident. Unfortunately, after the admission assessment, the MDS does not re-ask the questions about discharge preference or support until the annual assessment.
Facility-level variables were percentage admissions from acute-care hospitals (mean=78.5; SD=17.5; median=83.3); percentage of Medicare admissions (mean=71.6; SD=18.4; median=75.6); and percentage preference or support for discharge to the community (mean=78.3; SD=15.3; median=81.3).
Analysis
We first examined the admission sources, length of stay, and discharge status for the cohort. Second, we determined characteristics of residents at admission and those still in the nursing home at 90, 180, and 365 days. Third, we constructed multiple logistic regression models for identifying which resident or facility characteristics (i.e., admission source, age, marital status, living arrangement, diagnoses or conditions, pay source, and RUG-III groups) would be predictive of a resident's preference or support for returning to the community (scored 1=yes; 0=no) and subsequent discharge to the community within 90 days after admission (scored 1=community discharge; 0=remaining in the facility, nursing home transfer or other discharge status, or death). We also tested models for remaining in the nursing home (1=yes, 0=no) and multiple discharge statuses (score: 1=community discharge; 2=death; 3=other discharge status; or 4=remaining in the facility). Because residents were clustered within facilities, we estimated a hierarchical general linear (HGLM) model with a logit link function using HLM statistical software (Raudenbush and Bryk 2002; Raudenbush, Bryk, and Congdon 2002;). We tested a multilevel model (level 1=resident and level 2=facility) made up of a structural component containing resident and facility-level variables and a stochastic component with an error term representing the resident and facility residual terms. Prior research into discharge outcomes has not examined contextual effects with facility and patient-level variables considered simultaneously in a multilevel framework. We investigate, for example, if a Medicare or postacute resident is more likely to be discharged back to the community if the individual enters a facility that cares for a higher proportion of Medicare or postacute residents.
RESULTS
Admission Sources, Length of Stay, and Discharge Status
The first-time admission cohort varied in their admission sources, discharge status, and length of stay. The majority of admissions (87 percent) came from acute care hospitals. Smaller percentages of admission were from a private residence (9 percent), assisted living or board and care home (2 percent), or other source (2 percent). Most persons were discharged over the course of the year: 67 percent (16,441) were still in the facility at 14 days, 19 percent (4,549) were in the facility at 90 days, 13 percent (3,238) at 180 days, and 10 percent (2,481) at 1 year. Over two-thirds of discharges went to a private residence with home health (32 percent), private residence without home health (29 percent), or assisted living (8 percent). Nine percent of discharges went to another nursing home, 17 percent died, 4 percent went to an acute-care hospital, and 2 percent went to another discharge setting.
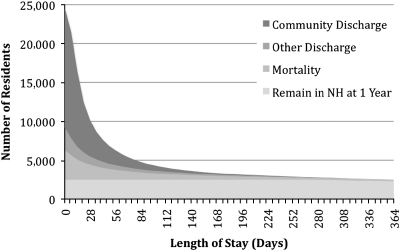
Discharges to the community were concentrated early in the nursing home stay (Figure 1). Eighty-five percent of the community discharges occurred within 30 days of admission, 10 percent were in 31–90 days, 4 percent in 91–180 days, and only 1 percent in 181–365 days. In contrast, 55 percent of deaths occurred in the first 30 days, 22 percent in 31–90 days, 11 percent in 91–180 days, and 12 percent in 181–365 days. At approximately 45 days the community discharge and mortality curves crossed over; the likelihood of mortality became increasingly greater than community discharge after that point.
Figure 1.
Number of Residents Remaining in the Nursing Home by Length of Stay and Discharge Status (n=24,648)
Characteristics of Residents at Admission, 90, 180, and 365 Days
Table 1 presents characteristics of all admissions and those remaining in the facility for 90, 180, and 365 days. The first set of variables was measured only at admission but reported for residents still remaining at 90, 180, and 365 days; the second set of variables was both measured and reported for residents at each length of stay. Members of the admission cohort were likely to be female, unmarried, living with someone else before admission, admitted from an acute-care setting and with Medicare paying the per diem. Their most prevalent conditions at admission were Alzheimer's or other forms of dementia, depression, behavioral problems, incontinence, diabetes, cancer, and hip fracture. Very high percentages of admissions preferred (84 percent) or had support for community discharge (69 percent). Having support was strongly associated with preference: 67 percent of residents had both preference and support for community discharge, 14 percent had neither preference nor support, 17 percent had preference without support, and only 2 percent had support without preference. Comparing all admissions with residents in the facility at 90, 180, or 365 days, the longer stay residents were much more likely to have had diagnoses of dementia or depression, moderate to severe cognitive impairment, behavioral problems, incontinence, low-care needs either broadly or narrowly defined, and to have converted to Medicaid. Longer stay residents were less likely to have preferred or had support for returning to the community, been admitted from an acute-care hospital or had Medicare as a per diem pay source.
Table 1.
Resident Characteristics for All Admissions and Those Still in the Nursing Home at 90, 180, and 365 Days
| Resident Characteristics | All Admissions (N=24,648) | Residents at 90 Days (n=4,549) | Residents at 180 Days (n=3,238) | Residents at 365 Days (n=2,483) |
|---|---|---|---|---|
| Measured at admission | ||||
| Female (%) | 61 | 62 | 64 | 66 |
| Not married (%) | 61 | 69 | 70 | 71 |
| Age (mean and SD) | 77.3 (12.7) | 80.1 (13.4) | 81.5 (12.6) | 82.6 (11.9) |
| Lived alone before admission (%) | 40 | 43 | 42 | 43 |
| Alzheimer's or dementia diagnosis (%) | 16 | 37 | 43 | 45 |
| History of MH or DD (%) | 6 | 8 | 8 | 7 |
| Schizophrenia, bipolar, anxiety (%) | 12 | 15 | 14 | 14 |
| Depression diagnosis (%) | 24 | 40 | 45 | 50 |
| Diabetes (%) | 26 | 25 | 24 | 25 |
| Cancer (%) | 14 | 11 | 9 | 8 |
| Hip fracture (%) | 7 | 5 | 3 | 3 |
| End-stage disease (%) | 3 | 3 | 2 | 2 |
| Prefer community discharge (Q1a) (%) | 84 | 60 | 55 | 52 |
| Support for community discharge (Q1b) (%) | 69 | 47 | 38 | 36 |
| Prefer or support for community discharge (%) | 86 | 64 | 58 | 56 |
| Prefer and support for community discharge (%) | 67 | 43 | 35 | 32 |
| Measured at each assessment | ||||
| Medicare per diem (%) | 77 | 28 | 5 | 5 |
| Medicaid per diem (%) | 7 | 35 | 50 | 58 |
| Other per diem (%) | 16 | 37% | 45 | 37 |
| Cognitive Performance Scale (CPS) score (range 0–6) (mean and SD) | 1.3 (1.5) | 2.3 (1.5) | 2.5 (1.5) | 2.6 (1.5) |
| Moderate to very severe cognitive impairment (%) | 24 | 50 | 55 | 59 |
| ADL scale (range=0–28) (mean and SD) | 13.3 (6.7) | 12.4 (8.1) | 12.4 (8.3) | 13.0 (8.3) |
| Incontinence (frequent or greater) (%) | 21 | 37 | 40 | 47 |
| Behavior problem at least weekly (%) | 14 | 28 | 31 | 32 |
| RUG extensive (%) | 46 | 5 | 4 | 3 |
| RUG rehabilitation (%) | 35 | 18 | 3 | 3 |
| RUG special (%) | 6 | 6 | 6 | 4 |
| RUG clinically complex (%) | 4 | 19 | 20 | 19 |
| RUG impaired cognition (%) | 3 | 15 | 18 | 18 |
| RUG behavioral (%) | 0 | 1 | 1 | 1 |
| RUG physical (%) | 6 | 36 | 47 | 52 |
| Low care requirements (%) | 3 | 20 | 24 | 23 |
Predictors of Preference for and Actual Community Discharge
Because preference and support for community discharge on admission had such a strong relationship to actual discharge, we wanted to determine what resident characteristics might be related to residents' preferences or support for returning to the community. Also, we wanted to determine the relationships between preferences or support for community discharge, other resident characteristics and actual community discharge. Because we anticipated that preferences or community discharge status might be related to facility characteristics, we included facility-level variables that were aggregates of resident-level variables. The postacute emphasis of the facility was represented by the proportion of admissions from acute-care hospital, with Medicare per diem, or falling into either of the higher RUG-III categories of Extensive or Rehabilitation that indicated postacute service need. We also hypothesized that facilities with a higher proportion of residents with a preference for or support for discharge to community would have higher discharge rates.
Table 2 shows results from HGLM models with correlates of the residents' preferences or support for community discharge at admission (yes=1, no=0). The sample consisted of all members of the admission cohort and all variables were measured at admission. Admissions from an acute-care hospital, with Medicare per diem, living alone prior to admission, in the RUG Extensive or Rehabilitation category, and with a hip fracture diagnosis were more likely to have a preference or support for community discharge. Admissions who were unmarried, older, receiving a Medicaid per diem, cognitively impaired and Alzheimer's or other dementia diagnosis, ADL dependent, incontinent, and suffering from cancer or an end-stage disease were less likely to have preference or support. Residents entering the facility in a low-care group were also less likely to prefer or have support for community discharge. In addition, admissions to facilities that admit a higher proportion of persons from acute-care hospitals were more likely to prefer or have support for community discharge. Finally, we found a significant interaction effect between resident and facility-level variables. Residents admitted from acute-care hospitals were more likely to prefer or have support for community discharge if they were admitted to a facility with a higher proportion of admissions from acute care.
Table 2.
HGLM Results for Resident's Preference or Support for Returning to the Community Based on Resident Characteristics at Nursing Home Admission (N=24,648)
| Coefficient | Odds Ratio | Confidence Interval | |
|---|---|---|---|
| Intercept | 2.32 | 10.15 | 9.24, 11.16 |
| Facility characteristic | |||
| Postacute facility (facility % of admissions from acute-care hospital) | 1.75 | 5.77 | 3.37, 9.87 |
| Resident characteristics and interactions | |||
| Resident admitted from acute care hospital | 0.94 | 2.56 | 2.28, 2.88 |
| Interaction: Postacute facility × resident admitted from acute care hospital | 1.94 | 6.95 | 3.76, 12.87 |
| Resident characteristics | |||
| Not married | −0.42 | 0.66 | 0.59, 0.74 |
| Age | −0.02 | 0.98 | 0.97, 0.98 |
| Live alone before admission | 0.16 | 1.18 | 1.05, 1.33 |
| Medicare | 0.47 | 1.60 | 1.40, 1.82 |
| Medicaid | −0.17 | 0.84 | 0.72, 0.99 |
| Alzheimer's or dementia diagnosis | −0.37 | 0.69 | 0.62, 0.77 |
| Cancer | −0.61 | 0.54 | 0.48, 0.60 |
| Hip fracture | 0.98 | 2.65 | 2.04, 3.45 |
| End-stage disease | −2.40 | 0.09 | 0.07, 0.11 |
| Cognitive Performance Scale (CPS) score | −0.45 | 0.64 | 0.62, 0.66 |
| ADL Long-Form Scale (range=0–28) | −0.05 | 0.95 | 0.94, 0.96 |
| Incontinent bowel or bladder (frequent or greater) | −0.38 | 0.68 | 0.61, 0.76 |
| RUG extensive | 0.60 | 1.82 | 1.60, 2.05 |
| RUG rehabilitation | 0.81 | 2.25 | 1.96, 2.58 |
| Low care | −0.62 | 0.54 | 0.43, 0.67 |
Note. All independent variables were statistically significant (p<.001). Results hierarchical general linear models (HGLM) with logit link function. Prefer or support for community discharge=1; do not prefer nor have support for community discharge=0. All independent variables were centered on their grand means.
The HGLM model for community discharge within 90 days after admission is presented in Table 3. Again, the sample consisted of the entire admission cohort with variables measured at admission. As we had anticipated preferring or having support to return to the community was a significant predictor of actual community discharge, even after controlling for other factors. Most of the same factors related to preference or support for community discharge were significantly related to actual discharge. Admission from an acute-care hospital, in the RUG Extensive or Rehabilitation category, and with a hip fracture diagnosis were more likely to be discharged to the community. Admissions who were unmarried, older, receiving Medicaid per diem, cognitively impaired or Alzheimer's or other dementia diagnosis, ADL dependent, incontinent, and with a psychiatric disorder, diabetes, cancer, or an end-stage disease diagnosis were less likely to be discharged to the community. Residents entering the facility in a low-care group were also less likely to be discharged to the community. Two facility-level variables were significant. A person was more likely to be discharged to the community if he or she entered a facility admitting a higher proportion of persons from acute-care hospitals and a facility where a higher proportion of admissions either preferred or had support for community discharge. Again, we found a significant interaction effect between resident- and facility-level variables. Residents who preferred or had support for community discharge were more likely to be discharged to the community if they were admitted to a facility with a high proportion of admissions preferring or having support for community discharge. We also tested multinomial models predicting community discharge, death, or remaining in the facility at 90 days. The same factors were significantly related to community discharge.
Table 3.
HGLM Results for Community Discharge within 90 Days Based on Resident Characteristics at Nursing Home Admission (N=24,648)
| Coefficient | Odds Ratio | Confidence Interval | |
|---|---|---|---|
| Intercept | 0.00 | 1.00 | 0.94, 1.08 |
| Facility characteristic | |||
| Postacute facility (facility % of admissions from acute-care hospital) | 0.83 | 2.28 | 1.36, 3.84 |
| Facility % of admissions with preference or support for returning to the community | 1.06 | 2.88 | 1.66, 4.98 |
| Resident characteristics and interactions | |||
| Resident prefer community discharge (Q1a) or support for community discharge (Q1b) | 2.18 | 8.89 | 7.75, 10.19 |
| Interaction: Facility % of admissions with preference or support × resident prefers or has support | 1.67 | 5.32 | 2.09, 13.58 |
| Resident admitted from acute care hospital | 0.44 | 1.55 | 1.37, 1.74 |
| Resident characteristics | |||
| Not married | −0.25 | 0.78 | 0.72, 0.85 |
| Age | 0.00 | 1.00 | 0.99, 1.00 |
| Medicare | 0.01 | 1.01 | 0.91, 1.12 |
| Medicaid | −0.46 | 0.63 | 0.54, 0.75 |
| Mental health diagnosis | −0.17 | 0.85 | 0.76, 0.94 |
| Alzheimer's or dementia diagnosis | −0.20 | 0.82 | 0.73, 0.92 |
| Diabetes | −0.21 | 0.81 | 0.75, 0.88 |
| Cancer | −0.58 | 0.56 | 0.51, 0.62 |
| Hip fracture | 0.29 | 1.34 | 1.17, 1.53 |
| End-stage disease | −1.36 | 0.26 | 0.19, 0.35 |
| Cognitive Performance Scale (CPS) score | −0.34 | 0.71 | 0.70, 0.74 |
| ADL Long-Form Scale (Range=0–28) | −0.08 | 0.92 | 0.92, 0.93 |
| Incontinent bowel or bladder (frequent or greater) | −0.47 | 0.62 | 0.57, 0.69 |
| RUG extensive | 0.42 | 1.52 | 1.36, 1.70 |
| RUG rehabilitation | 0.54 | 1.72 | 1.55, 1.90 |
| Low care | −0.77 | 0.46 | 0.38, 0.58 |
Notes. Results hierarchical general linear models (HGLM) with logit link function. community discharge=1; remain in facility, mortality, or other discharge=0. All independent variables were centered on their grand means.
Targeting Criteria
Drawing from prior research and the findings of our study, we selected three targeting criteria: preference or support for community discharge (Q1a or Q1b=yes), low-care requirements (RUG-III group IA1, IA2, BA1, BA2, PA1, PA2), and fitting a community discharge profile. The discharge profile was operationalized as the resident having a >50 percent likelihood of being discharged to the community within 90 days after admission. Conditional probability of community discharge was estimated from an HGLM model similar to the model described above with the following predictor variables all measured at admission: younger, married; Medicare per diem; admitted from an acute-care hospital; hip fracture; RUG Extensive or Rehabilitation category; minimal cognitive impairment (CPS); minimal ADL dependence (ADL dependency scale); continent; absent weekly behavioral problems; and absent a diagnosis of Alzheimer's or other dementia, depression, other mental disorder, diabetes, cancer, or end-stage disease. Details of the model are contained in Appendix SA2.
Targeting criteria were applied to the 4,549 residents in the admission cohort still in the nursing home at 90 days who presumably were at risk of becoming long-stay. Seventy-seven percent of residents met one or more of the three criteria. Sixty-four percent had preference or support for community discharge (at admission), 40 percent fit the community discharge profile (at admission), and 20 percent fell into the low-care category (at 90 days). Figure 2 shows the intersection of the three criteria. Although there was some overlap in targeting criteria, a sizeable proportion (36 percent) met only one criterion and the majority of these residents (27 percent) had preference or support but did not fit the profile or have low-care requirements. Thirty-two percent of residents (26+6 percent) met both the preference/support and profile criteria, 11 percent (6+5 percent) met the preference/support and low-care criteria, 10 percent (6+4 percent) met the discharge profile and low-care criteria, and only a small percentage (6 percent) met all three criteria.
Figure 2.
Percentage Meeting Targeting Criteria among Residents Still in the Facility at 90 Days after Admission (n=4,549)
DISCUSSION
Results from this study can inform the design of a program to transition residents from nursing home to community. A key question is when to initiate a community discharge intervention. Should it address long-stay residents who will be hard to relocate permanently but where a community discharge is clearly an accomplishment, or target residents earlier in their stays who are at risk of becoming long-stay residents? The nursing home population is dynamic. Over 80 percent of individuals in our annual admission cohort were discharged within 90 days of admission and only 10 percent remained in the facility at 1 year. Although two-thirds of discharges returned to the community, the probability of community discharge fell sharply during the first 90 days of an individual's nursing home stay when short-stay residents faced a substantial risk of becoming long-stay residents. We concluded that the optimum intervention window for community transitions would be between 90 and 120 days. This window allows for the large number of discharges before 90 days in the current system of care, while recognizing that with increasing length of stay the resident is more likely to break off ties to the community and become institutionalized. Transitioning residents during a 90–120 window should be less-resource intensive and should yield a higher success rate than MFPs' 180 days or more window. Moreover, private pay residents can be transitioned early in their stays perhaps avoiding costly Medicaid spend down.
Second, the program should be targeted to residents remaining in the facility despite preferring to return to the community and having a support person, variables we found to be strong predictors of community discharge. In addition, the program should target potentially long-stay residents whose characteristics predict community discharge. This profile includes having a preference or support for community discharge. The very high percentage (77 percent) of residents meeting one or more criteria bodes well for the success of community transitions, although it does not offer much targeting efficiency. A more efficient combination of criteria would be residents who: (a) had a preference or support and fit the community discharge profile (32 percent) or (b) had a preference or support and had low requirements (11 percent). This combination of criteria places primary importance on resident and family preferences while recognizing that the resident's health and functional status will influence long-term care decisions. We should note that only a small percentage of residents were low care at admission. Over half of the low-care admissions (52 percent) were admitted directly from the community and a majority (62 percent) expressed a preference or support for community discharge. These findings suggest that many of these individuals might have the potential for diversion to assisted living or home- and community-based services rather than entering nursing homes.
Third, we identified important contextual effects that can inform intervention program planning. People admitted to facilities with a higher proportion of postacute admissions were more likely to prefer returning to the community as well as actually doing so. In addition, residents admitted to facilities where other admissions shared their preferences or support had an increased likelihood of being discharged back to the community. Postacute facilities may attract persons who want to return to the community and have support to do so. Staff in these facilities might be more sensitive to resident preferences and, as a result, they may be more likely to assess and record a resident's preference or support for community discharge on the MDS. In addition, postacute facilities may place greater emphasis on restorative and rehabilitative care, resulting in greater success at community discharges. Also, these facilities might encourage among their residents and staff a culture of expectations for returning to the community. Being in a context where other residents expect to return to the community is likely to enhance one's own expectations, resulting in a successful transition. A community transition program should promote facility care practices and cultures aimed at restoring functional status, teaching self-management skills, and encouraging positive attitudes and support for community transitions.
Finally, we have shown that the MDS can be a valuable tool in targeting residents for a transition program. The MDS has recognized limitations. The MDS preference and support items are asked only at admission and annually thereafter. Updated ascertainment of preferences would be better. The preference determinations are subject to interpretation or even bias by facility staff, and MDS items lack information about family support capabilities and facility actions to promote discharge (Kane 2008; Nishita et al. 2008;). Some concerns will likely be addressed in MDS version 3.0 (scheduled for implementation October 2010), which requires facilities to directly ask residents preference and support questions on a quarterly basis (Saliba and Buchanan 2008). Furthermore, transition programs may face administrative challenges in gaining access to MDS data in a timely manner (Reinhard and Hendrickson 2006). We think realistically that the Medicaid program can obtain and process MDS assessments within 60 days of admission and send resident targeting reports to transitions counselors and nursing home discharge planners within 30 days after that. Targeted residents still in the facility at 90 days would be contacted to enquire about community discharge.
Much attention is focused on the federal MFP initiative being implemented in 31 states with U.S.$1.75 billion in federal funding. The Minnesota transition program employs a different design. Whereas MFP is restricted to longer stay Medicaid residents who have been in the nursing home for at least 6 months (Lipson and Williams 2009), the Minnesota program targets persons earlier in their stays (90–120 days) who are at risk of becoming long-stay residents, would likely remain in the facility without an intervention, and who have the potential for a successful transition. The Minnesota program also includes both Medicaid and private pay residents under the assumption that many private pay residents will eventually convert to Medicaid if they remain in the facility. Thus, the state can promote consumer choice and perhaps save future Medicaid funds by avoiding or delaying Medicaid conversion. We plan to evaluate the effectiveness of the Minnesota program, drawing comparisons where possible with MFP.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: Preliminary findings from this study were presented at the Annual Research Meeting of Academy Health, June 2007. The study was supported by a contract with the Minnesota Department of Human Services. Julie Bershadsky and Mark Woodhouse assembled the study data and ran much of the analysis. Robert Held, Christine Mueller, and Kathleen Abrahamson gave thoughtful comments on the study design and findings. The authors are responsible for any errors or omissions. The opinions expressed are solely those of the authors and not the Minnesota Department of Human Services or their other institutional affiliations.
Disclosures: None.
Disclaimers: None.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Appendix SA2: Targeting Model.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- Arling G, Kane RL, Mueller C, Lewis T. Explaining Direct Care Resource Use of Nursing Home Residents: Findings from Time Studies in Four States. Health Services Research. 2007;42(2):827–46. doi: 10.1111/j.1475-6773.2006.00627.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arling G, Williams AR, Kopp D. Therapy Use and Discharge Outcomes for Elderly Nursing Home Residents. Gerontologist. 2000;40(5):587–95. doi: 10.1093/geront/40.5.587. [DOI] [PubMed] [Google Scholar]
- Boaz RF, Muller CF. Predicting the Risk of “Permanent” Nursing Home Residence: The Role of Community Help as Indicated by Family Helpers and Prior Living Arrangements. Health Services Research. 1994;29(4):391–414. [PMC free article] [PubMed] [Google Scholar]
- Buttar A, Blaum C, Fries B. Clinical Characteristics and Six-Month Outcomes of Nursing Home Residents with Low Activities of Daily Living Dependency. Journals of Gerontology Series A, Biological Sciences and Medical Sciences. 2001;56(5):M292–7. doi: 10.1093/gerona/56.5.m292. [DOI] [PubMed] [Google Scholar]
- Chapin R, Baca B, Macmillan K, Rachlin R, Zimmerman M. Residential Outcomes for Nursing Facility Applicants Who Have Been Diverted: Where Are They 5 Years Later? Gerontologist. 2009;49(1):46–56. doi: 10.1093/geront/gnp009. [DOI] [PubMed] [Google Scholar]
- Chapin R, Wilkinson DS, Rachlin R, Levy M, Lindbloom R. Going Home: Community Reentry of Light Care Nursing Facility Residents Age 65 and Over. Journal of Health Care Finance. 1998;25(2):35–48. [PubMed] [Google Scholar]
- CMS. 2007. Money Follows the Person” [accessed on Decmeber 7 2007, 2007]. Available at http://www.cms.hhs.gov/DeficitReductionAct/20_MFP.asp.
- Coughlin TA, McBride TD, Liu K. Determinants of Transitory and Permanent Nursing Home Admissions. Medical Care. 1990a;28(7):616–31. doi: 10.1097/00005650-199007000-00007. [DOI] [PubMed] [Google Scholar]
- Coughlin TA. Determinants of Transitory and Permanent Nursing Home Admissions. Medical Care. 1990b;28(7):616–31. doi: 10.1097/00005650-199007000-00007. [DOI] [PubMed] [Google Scholar]
- Cumming RG, Klineberg R, Katelaris A. Cohort Study of Risk of Institutionalisation after Hip Fracture. Australian and New Zealand Journal of Public Health. 1996;20(6):579–82. doi: 10.1111/j.1467-842x.1996.tb01069.x. [DOI] [PubMed] [Google Scholar]
- Engle VF, Graney MJ. Predicting Outcomes of Nursing Home Residents—Death and Discharge Home. Journals of Gerontology. 1993;48(5):S 269–75. doi: 10.1093/geronj/48.5.s269. [DOI] [PubMed] [Google Scholar]
- Freedman VA. Family Structure and the Risk of Nursing Home Admission. Journals of Gerontology Series B, Psychological Sciences and Social Sciences. 1996;51(2):S61–9. doi: 10.1093/geronb/51b.2.s61. [DOI] [PubMed] [Google Scholar]
- Fries BE, Schneider DP, Foley WJ, Gavazzi M, Burke R, Cornelius E. Refining a Case-Mix Measure for Nursing Homes: Resource Utilization Groups (RUG-III) Medical Care. 1994;32(7):668–85. doi: 10.1097/00005650-199407000-00002. [DOI] [PubMed] [Google Scholar]
- Gaugler JE, Kane RL, Newcomer R. Resilience and Transitions from Dementia Caregiving. Journals of Gerontology Series B, Psychological Sciences and Social Sciences. 2007;62(1):P38–44. doi: 10.1093/geronb/62.1.p38. [DOI] [PubMed] [Google Scholar]
- Gill TM, Gahbauer EA, Han L, Allore HG. Functional Trajectories in Older Persons Admitted to a Nursing Home with Disability after an Acute Hospitalization. Journal of American Geriatric Society. 2009;57(2):195–201. doi: 10.1111/j.1532-5415.2008.02107.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howell S, Silberberg M, Quinn WV, Lucas JA. Determinants of Remaining in the Community after Discharge: Results from New Jersey's Nursing Home Transition Program. Gerontologist. 2007;47(4):535–47. doi: 10.1093/geront/47.4.535. [DOI] [PubMed] [Google Scholar]
- Jette DU, Warren RL, Wirtalla C. Rehabilitation in Skilled Nursing Facilities: Effect of Nursing Staff Level and Therapy Intensity on Outcomes. American Journal of Physical and Medical Rehabilitation. 2004;83(9):704–12. doi: 10.1097/01.phm.0000137312.06545.d0. [DOI] [PubMed] [Google Scholar]
- Jones A. The National Nursing Home Survey: 1999 Summary. Vital and Health Statistics – Series 13: Data From the National Health Survey. 2002;13(152):1–116. [PubMed] [Google Scholar]
- Kane RA. Providing Structured Opportunities for Nursing Home Residents to Choose Community Care. Journal of American Geriatric Society. 2008;56(1):163–5. doi: 10.1111/j.1532-5415.2007.01560.x. [DOI] [PubMed] [Google Scholar]
- Kane RL, Chen Q, Blewett LA, Sangl J. Do Rehabilitative Nursing Homes Improve the Outcomes of Care? Journal of American Geriatric Society. 1996;44(5):545–54. doi: 10.1111/j.1532-5415.1996.tb01440.x. [DOI] [PubMed] [Google Scholar]
- Kasper J. 2005. Who Stays and Who Goes Home: Using National Data on Nursing Home Discharges and Long-Stay Residents to Draw Implications for Nursing Home Transition Programs. Kaiser Commission on Medicaid and the Uninsured.
- Kasper J, O'Malley M. 2006a. Nursing Home Transition Programs: Perspectives of Medicaid Care Planners. Kaiser Commission on Medicaid and the Uninsured.
- Kasper J. 2006b. Nursing Home Transition Programs: Perspectives of State Medicaid Officials. Kaiser Commission on Medicaid and the Uninsured.
- Kaye HS, LaPlante MP, Harrington C. Do Noninstitutional Long-Term Care Services Reduce Medicaid Spending? Health Affairs (Millwood) 2009;28(1):262–72. doi: 10.1377/hlthaff.28.1.262. [DOI] [PubMed] [Google Scholar]
- Lindrooth RC, Hoerger TJ, Norton EC. Expectations among the Elderly about Nursing Home Entry. Health Services Research. 2000;35(5, part 2):1181–202. [PMC free article] [PubMed] [Google Scholar]
- Lipson DJ, Williams SR. Implications for State Program Features for Attaining MFP Goals. National Evaluation of the Money Follows the Person (MFP) Demonstration Grant Program: Reports from the Field. I. Princeton, NJ.: Mathematica Policy Research; 2009. [Google Scholar]
- Liu K, McBride T, Coughlin T. Risk of Entering Nursing Homes for Long Versus Short Stays. Medical Care. 1994;32(4):315–27. doi: 10.1097/00005650-199404000-00001. [DOI] [PubMed] [Google Scholar]
- Mehdizadeh SA. Health and Long-Term Care Use Trajectories of Older Disabled Women. Gerontologist. 2002;42(3):304–14. doi: 10.1093/geront/42.3.304. [DOI] [PubMed] [Google Scholar]
- Mehr DR, Williams BC, Fries BE. Predicting Discharge Outcomes of VA Nursing Home Residents. Journal of Aging and Health. 1997;9(2):244–65. doi: 10.1177/089826439700900206. [DOI] [PubMed] [Google Scholar]
- Mor V, Zinn J, Gozalo P, Feng Z, Intrator O, Grabowski DC. Prospects for Transferring Nursing Home Residents to the Community. Health Affairs (Millwood) 2007;26(6):1762–71. doi: 10.1377/hlthaff.26.6.1762. [DOI] [PubMed] [Google Scholar]
- Morris JN, Fries BE, Mehr DR, Hawes C, Phillips C, Mor V, Lipsitz LA. MDS Cognitive Performance Scale. Journal of Gerontology: Medical Sciences. 1994;49(4):M174–82. doi: 10.1093/geronj/49.4.m174. [DOI] [PubMed] [Google Scholar]
- Morris JN, Fries BE, Morris SA. Scaling ADLs within the MDS. Journals of Gerontology Series A, Biological Sciences and Medical Sciences. 1999;54(11):M546–53. doi: 10.1093/gerona/54.11.m546. [DOI] [PubMed] [Google Scholar]
- Murtaugh CM. Discharge Planning in Nursing Homes. Health Services Research. 1994;28(6):751–69. [PMC free article] [PubMed] [Google Scholar]
- Newcomer R, Kang T, Graham C. Outcomes in a Nursing Home Transition Case-Management Program Targeting New Admissions. Gerontologist. 2006;46(3):385–90. doi: 10.1093/geront/46.3.385. [DOI] [PubMed] [Google Scholar]
- Nishita CM, Wilber KH, Matsumoto S, Schnelle JF. Transitioning Residents from Nursing Facilities to Community Living: Who Wants to Leave? Journal of American Geriatric Society. 2008;56(1):1–7. doi: 10.1111/j.1532-5415.2007.01566.x. [DOI] [PubMed] [Google Scholar]
- Nyman JA, Cyphert ST, Russell DW, Wallace RB. The Ratio of Impaired Elderly in the Community to Those in Nursing Homes in Two Rural Iowa Counties. Medical Care. 1989;27(10):920–7. doi: 10.1097/00005650-198910000-00002. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and Data Analysis Methods. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- Raudenbush SW, Bryk AS, Congdon RT. HLM [computer program]. Version 5 (release) Lincolnwood, IL: Scientific Software International; 2002. [Google Scholar]
- Reinhard SC, Hendrickson L. Money Follows the Person: States' Progress in Using the Minimum Data Set (MDS) to Facilitate Nursing Home Transition. New Brunswick, NJ: Rutgers Center for State Health Policy; 2006. [Google Scholar]
- Reschovsky JD. The Demand for Post-Acute and Chronic Care in Nursing Homes. Medical Care. 1998;36(4):475–90. doi: 10.1097/00005650-199804000-00004. [DOI] [PubMed] [Google Scholar]
- Saliba D, Buchanan J. Development and Validation of a Revised Nursing Home Assessment Tool: MDS 3.0. Baltimore: Centers for Medicare and Medicaid Services; 2008. [Google Scholar]
- Summer L. 2005. Strategies to Keep Consumers Needing Long-Term Care in the Community and Out of Nursing Facilities. Kaiser Commission on Medicaid and the Uninsured, pp. 35.
- Wenzlow AT, Lipson DJ. Transitioning Medicaid Enrollees from Institutions to the Community: Number of People Eligible and Number of Transitions Targeted Under MFP. National Evaluation of the Money Follows the Person (MFP) Demonstration Grant Program: Reports from the Field. I. Princeton, NJ: Mathematica Policy Research; 2009. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.