Abstract
Objective
To assess the impact of state Medicaid wage pass-through policy on direct-care staffing levels in U.S. nursing homes.
Data Sources
Online Survey Certification and Reporting (OSCAR) data, and state Medicaid nursing home reimbursement policies over the period 1996–2004.
Study Design
A fixed-effects panel model with two-step feasible-generalized least squares estimates is used to examine the effect of pass-through adoption on direct-care staff hours per resident day (HPRD) in nursing homes.
Data Collection/Extraction Methods
A panel data file tracking annual OSCAR surveys per facility over the study period is linked with annual information on state Medicaid wage pass-through and related policies.
Principal Findings
Among the states introducing wage pass-through over the study period, the policy is associated with between 3.0 and 4.0 percent net increases in certified nurse aide (CNA) HPRD in the years following adoption. No discernable pass-through effect is observed on either registered nurse or licensed practical nurse HPRD.
Conclusions
State Medicaid wage pass-through programs offer a potentially effective policy tool to boost direct-care CNA staffing in nursing homes, at least in the short term.
Keywords: Medicaid, wage pass-through, direct-care staff, nursing homes
Two decades after the landmark legislation of the Nursing Home Reform Act as part of the Omnibus Budget Reconciliation Act of 1987, substandard quality of care in the nation's nursing homes—despite incremental improvements—continues to be a widespread concern (Wiener, Freiman, and Brown 2007). Among others, inadequate staffing has frequently been blamed for this sorry state of affairs. Indeed, a cumulative body of evidence emerging from the research literature has consistently linked low staffing levels to poor quality of nursing home care (Centers for Medicare & Medicaid Services 2000, 2001; Bostick et al. 2006).
The demand for more, and better trained, direct-care staff in nursing homes has increasingly been met with serious recruitment and retention problems, attributable to a variety of factors, including low wages, few benefits, difficult working conditions, lack of career ladders, and as a result, low job satisfaction and high turnover among these staff (Scanlon 2001; Super 2002; Smith and Baughman 2007;). In response, recent government and private initiatives have sought to address impediments in recruiting and retaining direct-care workers. Although many of these initiatives are multifaceted, some focus specifically on improving direct-care workers' wages and benefits.
From a policy perspective, targeting direct-care wages and benefits is particularly relevant to nursing homes where a high proportion of care is already publicly funded, mostly by Medicaid. In virtually all states, Medicaid nursing home reimbursement rates are considerably lower than Medicare or private-pay rates, and reportedly, often below the actual costs of care provided (BDO Seidman 2007). In effect, state Medicaid reimbursement policy, by imposing a third-party payer constraint, limits nursing homes' financial resources and flexibility in setting wages and benefits. With wages for nurse aides barely above the minimum wage and scanty benefits, nursing homes are essentially competing with fast food restaurants and other low-wage service sectors for their entry-level direct-care staff (Scanlon 2001).
In recent years, Medicaid programs in a growing number of states have experimented with a wage pass-through policy, which earmarks additional funds for the explicit purpose of increasing compensation for direct-care workers in long-term care. States adopting a wage pass-through policy generally require that a certain portion of the Medicaid reimbursement increase be devoted to staffing, through enhancing direct-care wages or benefits or increasing the number of staff. States have generally used two approaches to its implementation—by designating either a set dollar amount per staff hour (or patient day), or a certain percentage of a reimbursement increase to be used for wages/benefits (North Carolina Division of Facility Services 2000). In practice, however, the formulation and mechanisms of a wage pass-through vary widely from state to state, as do accountability procedures in place to monitor provider compliance (North Carolina Division of Facility Services 1999; Paraprofessional Healthcare Institute 2003;).
Despite increased popularity of wage pass-through as a state policy tool, little is currently known about its effectiveness in achieving the intended goals—to boost direct-care staffing and reduce vacancies and turnover. The lack of formal evaluations of wage pass-through is due in part to the paucity of data. After all, wage pass-through is still a relatively new concept for most states, with the majority of existing programs introduced only within the past decade. Michigan is an exception as one of the few early adopters, with a wage pass-through in place for nursing homes since 1990 (North Carolina Division of Facility Services 2000). Longitudinal data from Michigan indicate that between 1990 and 1998, the nurse aide turnover rate declined from 75 to 67 percent, which the state attributes to wage pass-through (Scanlon 2001). The Michigan data also reveal a large, cumulative impact of wage pass-through on actual nurse aide wages by 2000 (Walker, Angelotti, and Patterson 2000). However, a 2000 follow-up survey of 16 states with a wage pass-through in 1999 reported mixed results regarding the impact of pass-through on aide recruitment and retention (North Carolina Division of Facility Services 2000). This mixture of empirical evidence has led a recent analysis of state wage pass-through programs to conclude that data currently available do not clearly support the efficacy of such programs (Paraprofessional Healthcare Institute 2003).
For nursing home policy makers, researchers, and consumer advocates concerned about staffing issues, an important question remains unanswered as to whether Medicaid wage pass-through has ultimately translated into increases in actual direct-care staffing levels, which are key to the quality of nursing home care. To our knowledge, no research so far has attempted to address this issue, which, obviously, has significant policy implications. The limited information currently available on state wage pass-through programs is fragmented and has been neither updated frequently enough nor extended to the most recent years, despite calls for continuously tracking state policy changes and initiatives in this area (North Carolina Division of Facility Services 2000). Another limitation of the extant data on state wage pass-through policies is the ambiguity in regards to the specific providers to which a wage pass-through is applied. For instance, a wage pass-through may be proposed specifically to target certified nurse aides (CNAs) in skilled nursing facilities in one state, or personal care assistants in home care settings in another state, or both in still other states—a differentiation in program features that has largely been blurred in most of the ongoing discussions about wage pass-through.
In a recently conducted survey of state Medicaid nursing home reimbursement policies, we collected longitudinal data on wage pass-through from all the 48 continental U.S. states covering a 9-year period from 1996 to 2004. Our survey is designed specifically to capture Medicaid wage pass-through programs targeting direct-care staff in nursing homes, and to our knowledge, the resulting data are the most current and comprehensive available. Combining these state policy data with a national longitudinal file of nursing homes for the same period, we seek in this paper to address the following question: Has the introduction of Medicaid wage pass-through increased direct-care staffing in U.S. nursing homes?
METHODS
Data Sources
The primary source of data for this study is the Online Survey Certification and Reporting (OSCAR) system from 1996 to 2004. The OSCAR contains facility-level information, including staffing, organizational characteristics, and aggregate resident conditions, for all Medicare/Medicaid-certified nursing homes in the United States. The OSCAR data are self-reported by each facility during periodic inspections by the state, which occur on average about once a year.
We track each facility over time and create a longitudinal data file with repeated annual surveys per facility. If multiple surveys exist for the same facility in a given year, only the one closest to year end is retained. Our study excludes hospital-based facilities, which primarily serve short-stay, postacute Medicare patients and often provide staffing centrally through the affiliated hospital. Nursing homes located in rural areas are also excluded because their labor market varies markedly from that of urban facilities (Intrator et al. 2005; Feng et al. 2008;). We further exclude the small number of facilities located in Alaska, Hawaii, the District of Columbia, and other U.S. territories.
Annual information about state Medicaid wage pass-through and other nursing home payment policies from 1996 to 2004, including average Medicaid rates and the use of case-mix reimbursement, are collected by the authors through an ongoing survey of state Medicaid offices, as described elsewhere (Grabowski et al. 2004, 2008). Relevant time-varying characteristics of the local nursing home market are obtained from the county-level Area Resource File.
Dependent Variable
The dependent variable is defined annually per facility, as the total average direct-care staff hours per resident day (HPRD), separately for CNAs, licensed practical nurses (LPNs), and registered nurses (RNs). For each staffing measure, observations with HPRD values >12 or beyond the 99th percentile (whichever threshold is lower) in the respective aggregate distribution are treated as outliers and trimmed from the analysis. The dependent variable is logged (natural log) for the multivariate regression analysis (detailed below), implying that the coefficient estimates can be interpreted as the percent change in staffing HPRD in response to a unit change in a particular independent variable of interest.
Independent Variables
State Policies
The key state policy variable of interest is the Medicaid wage pass-through to nursing homes. Exploiting timing to adoption, we create an ordinal pass-through policy variable with baseline: (1) preadoption, (2) year of adoption, (3) first year after adoption (with policy still in effect), (4) second or subsequent years after adoption (with policy still in effect), and (5) policy repealed. Observations in the first category are used as the reference/control group, and those in the remaining categories are coded as four dummy variables. We hypothesize that nursing homes in states that introduced wage pass-through over the study period will experience an increase in direct-care staffing levels in the postadoption period, ceteris paribus, compared with the preadoption period or to facilities in states without exposure to the policy. Moreover, this coding scheme permits the assessment of nonlinear policy effects: that is, a new policy may not reach its full impact until some lapse from its initial adoption, and this impact may dwindle thereafter, particularly when the policy is repealed.
In addition, we control for two important variables related to Medicaid nursing home reimbursement. One is the annual state-average Medicaid payment rate, which is inflation adjusted to 2004 dollars (centered at overall mean, with U.S.$10 increment) using the annual Consumer Price Index published by the Bureau of Labor Statistics. The other relates to the use of case-mix-adjusted reimbursement, measured by a dummy variable indicating the presence of a case-mix payment system in a given state and year.
Market Conditions
As in most previous studies, we use the county as a proxy for the nursing home market, which is a reasonable approximation given patterns of funding and resident origin (Grabowski 2008). We include the average number of empty beds per nursing home in the county as an indicator of market competition. To control for variations in local demand and supply factors related to the nursing workforce, we include the number of RNs and LPNs per hospital bed, number of nursing home beds per capita, and Medicare managed care penetration rate. Furthermore, hospital wage index (standardized, with one standard deviation increment) is included to control for regional differences in the purchasing power of Medicaid payments and the price of medical and nursing services.
Facility Characteristics
To account for differences in resident case mix, we include an acuity index derived from OSCAR, which combines a range of activity of daily living dependencies and special treatment measures for all residents in each facility (Feng et al. 2006). Other characteristics include whether the facility has a nurse practitioner or physician assistant, whether an Alzheimer's unit is available, and the percent of Medicaid residents.
Statistical Analysis
Taking advantage of the panel data, we begin with a conventional, facility fixed-effects model approach, which controls for any fixed facility-specific omitted variables that may be correlated with direct-care staffing levels. This modeling approach implicitly purges the unobserved and potentially confounded cross-sectional heterogeneity by relying on the within-facility variation in the covariates over time and using facilities that did not experience a change as a control for unrelated time-series variation (Grabowski 2004; Feng et al. 2006;). In addition, we include calendar year dummies in the model to capture the overall trends in direct-care staffing levels in nursing homes.
The fixed-effects approach using panel data returns consistent estimates under the assumption that the errors are independently distributed. However, this may be too strong an assumption because the residual components are unlikely to be independent among each other for facilities within the same state. Furthermore, we would expect that the unobserved shocks influencing nursing home staffing would be serially correlated over time within states. Hence, a fixed-effects regression that does not account for clustering and the serial correlation problem will lead to inefficient estimates and inference problems.
A general solution is to cluster observations at the state level as suggested by Bertrand, Duflo, and Mullainathan (2004). This procedure constructs an error structure from the data and returns a consistent estimate robust to the clustering and serial correlation problems. However, the obtained standard errors (SEs) are potentially inefficient as it does not purge the underlying serial correlation but simply adopts a heterogeneity robust procedure in constructing the error structure. Another fundamental problem with this procedure is that estimates are inconsistent if state-level shocks are correlated with facility-level nursing home characteristics, which is very likely in our data. Consequently, a fixed-effects regression with SEs clustered at the state level may result in biased estimates and misleading policy effects.
Thus, in this analysis, we implement a two-step feasible-generalized least squares (FGLS) estimation procedure originally proposed by Hansen (2007) and slightly modified in Foster and Lee (2009) for simpler application. The basic idea of this procedure is as follows: the first step nets out facility-level variation in the dependent variable to return the component that varies with state-level variables, that is, state policies. The second step is a GLS procedure at the state level using this estimated component as the dependent variable. Assuming that the underlying state-year shock follows an AR(1) process, we obtain an unbiased estimate of the autoregressive (AR) coefficient and perform an autocorrelation-adjusted regression. The first step estimates are robust to the clustering problem and the possible correlation between facility variables and state-year level shocks. The second step deals with the serial-correlation problem. The efficiency gain amounts to a 30–50 percent decrease in SEs depending on panel length and the underlying AR structure of the shocks, as documented in Foster and Lee (2009).
Briefly, the procedure involves the following steps: (i) take deviations from the means of facility-level outcomes and covariates, regress outcome deviations on the facility-level covariate deviations using state-year fixed effects, and retrieve estimates of the state-year fixed effects; (ii) regress state-year fixed effects on state policy variables and state fixed effects (this returns the two-step ordinary least squares [OLS] estimates which do not account for the serial correlation problem), and compute the AR(1) parameter from autocorrelation of difference residuals using the method of moments; and (iii) run the final FGLS model by first differencing the data from its mean and then ρ-differencing (i.e., differencing the variables by one-period lag multiplied by the AR(1) coefficient) and reweighting (the first observation) using the estimated AR(1) parameter, with Huber-White robust SEs clustered at the state level.
Applying the procedure above, we carry out two separate sets of models. The first includes only those facilities in states that introduced wage pass-through during the period of 1996–2004, utilizing observations within the same state that are not exposed to the policy as a control. The second set of models includes facilities from both adopter and nonadopter states, with observations from the latter included in the control group. If systematic and significant differences emerge from the two sets of model specifications, this would suggest that those adopter states and nonadopter states differ in important ways along observed or unobserved attributes, or both. If so, inference about the policy effects should be made with caution.
RESULTS
Our state policy survey indicates that in 1996, only two states (California and Michigan) had a wage pass-through policy in place. In the 8-year period that followed, 21 additional states introduced wage pass-through, including 1 state in 1998 (Minnesota), 3 states in 1999 (Delaware, South Carolina, and Wisconsin), 6 states in 2000 (Kansas, Maine, Montana, Texas, Virginia, and Vermont), 3 states in 2001 (North Dakota, Rhode Island, and Wyoming), 5 states in 2002 (Arizona, Florida, Massachusetts, Maryland, and New York), 2 states in 2003 (Louisiana and South Dakota), and 1 state in 2004 (Georgia). Because some of these states have “bounced” in and out of a pass-through policy over the study period, the total number of states with a pass-through in effect varies annually (see Table SA1 for details). Nevertheless, the general trend has been a significant increase in pass-through adoption among the states, from just 2 states in 1996 to 10 by 2004.
Descriptive statistics on study variables, including means and standard deviations for continuous variables and percentages for categorical variables, are reported in Table 1, separately for facilities in the 21 pass-through adopter states and facilities in nonadopter states. Excluded here and from the analyses that follow are the two early adopters, California and Michigan, which began pass-through in 1986 and 1990, respectively. The reason is that no data from the preadoption period are observed in these two states, and given our interest in comparing staffing differences before and postpass-through adoption, it would be inappropriate to include them in either the “treatment” or control group. All variables are time varying, pursuant to a fixed-effects model specification. In the multivariate regression model, all continuous variables on the right-hand side of the equation are centered at the overall mean.
Table 1.
Description of Study Variables, Aggregated over 1996–2004
| Pass-through: Adopter States | Pass-through: Nonadopter States | |
|---|---|---|
| Mean (SD) or Percentage | Mean (SD) or Percentage | |
| Dependent variables | ||
| CNA HPRD | 2.13 (0.87) | 2.09 (0.93) |
| LPN HPRD | 0.73 (0.44) | 0.70 (0.45) |
| RN HPRD | 0.34 (0.34) | 0.40 (0.35) |
| State policies | ||
| Wage pass-through | ||
| Preadoption (reference) (%) | 56.1 | 100 |
| Year of adoption (%) | 11.5 | — |
| 1st year after adoption (%) | 10.1 | — |
| 2nd and subsequent years after adoption (%) | 13.7 | — |
| Policy repealed (%) | 8.6 | |
| CPI-adjusted Medicaid payment rate (2004 dollar) | 123.42 (31.92) | 119.58 (23.65) |
| Case-mix reimbursement (%) | 75.8 | 64.7 |
| Facility characteristics | ||
| Acuity index | 11.0 (1.5) | 10.9 (1.6) |
| Nurse practitioner/physician assistant (%) | 28.5 | 19.4 |
| Alzheimer's unit (%) | 18.4 | 20.7 |
| Percent Medicaid | 65.9 (23.3) | 62.7 (24.2) |
| Market (county) conditions | ||
| Average number of empty beds per nursing home | 14.4 (7.5) | 15.8 (7.9) |
| RNs per hospital bed | 1.36 (0.50) | 1.46 (0.41) |
| LPNs per hospital bed | 0.19 (0.11) | 0.17 (0.11) |
| Nursing home beds per 1,000 elders | 52.2 (20.0) | 56.0 (16.4) |
| Managed care penetration rate (%) | 15.4 (13.3) | 14.2 (12.4) |
| Area wage index | 1.01 (0.15) | 0.99 (0.11) |
| Number of observations | 31,648 | 37,094 |
CNA, certified nurse aide; CPI, consumer price index; HPRD, hours per resident day; LPN, licensed practical nurse; RN, registered nurse; SD, standard deviation.
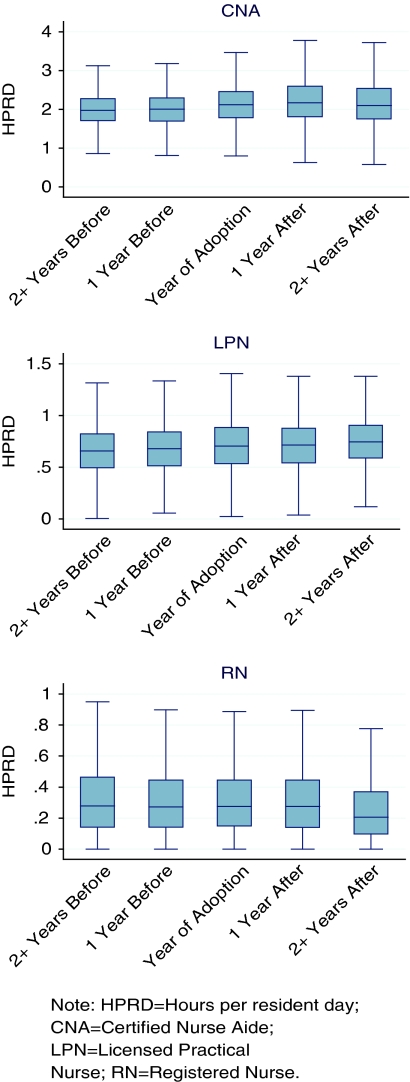
In Figure 1, we use box plots to illustrate aggregate changes in direct-care CNA, LPN, and RN staffing levels in nursing homes from the 21 adopter states, by timing to pass-through introduction (which varies by state, as described above). The box plots reveal a noticeable jump in CNA staffing levels in the year of and 1 year after pass-through adoption but a much smaller increase in subsequent years, as compared with levels in the preadoption period. A continuous increase in the postrelative to preadoption period is observed in LPN staffing levels. The trend in RN staffing is distinct: there seems to be little change in the year of and the first year after adoption, followed by a dip in subsequent years. However, it is important to note that these aggregate staffing changes are due in part to the pass-through policy and partly to the overall time trends in staffing levels. To net out the policy effect, we now turn to multivariate analysis using a fixed-effects panel model with two-step FGLS estimates, beginning with results from the 21 adopter states only, as reported in Table 2.
Figure 1.
Change in Direct-Care Staffing Levels in Nursing Homes in 21 States Introducing Wage Pass-through during 1996–2004
Table 2.
The Effect of Introducing Medicaid Wage Pass-through on Direct-Care Staffing Levels in Nursing Homes in 21 Pass-through Adopter States, 1996–2004
| CNA |
LPN |
RN |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| 2nd Step‡ |
2nd Step‡ |
2nd Step‡ |
|||||||
| 1st Step† (1) OLS | (2) OLS | (3) FGLS | 1st Step† (1) OLS | (2) OLS | (3) FGLS | 1st Step† (1) OLS | (2) OLS | (3) FGLS | |
| Wage pass-through§: | |||||||||
| Year of adoption | 0.0334*** | 0.0288* | 0.0301** | 0.0218 | 0.0254 | 0.0268 | 0.0171 | 0.0208 | 0.0233 |
| (0.0107) | (0.0153) | (0.0126) | (0.0238) | (0.0359) | (0.0319) | (0.0264) | (0.0373) | (0.0373) | |
| 1st year after adoption | 0.0444*** | 0.0428*** | 0.0399*** | 0.0272 | 0.0214 | 0.0226 | 0.0255 | 0.0305 | 0.0297 |
| (0.0144) | (0.0136) | (0.0134) | (0.0179) | (0.0327) | (0.0297) | (0.0322) | (0.0424) | (0.0408) | |
| 2nd/subsequent years | 0.0144 | 0.0149 | 0.0279* | 0.0127 | 0.0629 | 0.0728 | −0.0651 | −0.0134 | −0.0116 |
| (0.0193) | (0.0142) | (0.0141) | (0.0269) | (0.0490) | (0.0436) | (0.0395) | (0.0655) | (0.0623) | |
| Policy repealed | 0.0016 | 0.0163 | 0.0268** | 0.0573* | 0.0463 | 0.0506 | −0.1506** | −0.0864 | −0.0821 |
| (0.0281) | (0.0220) | (0.0125) | (0.0319) | (0.0425) | (0.0329) | (0.0550) | (0.0590) | (0.0566) | |
| Medicaid payment rate | 0.0093 | −0.0025 | −0.0012 | 0.0268 | 0.0469** | 0.0414** | 0.0051 | 0.0023 | 0.0024 |
| (0.0152) | (0.0101) | (0.0079) | (0.0159) | (0.0167) | (0.0167) | (0.0091) | (0.0101) | (0.0093) | |
| Case-mix reimbursement | −0.0442 | −0.0284 | −0.0164 | −0.0341 | −0.0176 | −0.0075 | 0.1118** | 0.1088 | 0.1110* |
| (0.0317) | (0.0207) | (0.0131) | (0.0341) | (0.0371) | (0.0281) | (0.0535) | (0.0712) | (0.0621) | |
| Facility fixed effects | Yes | Yes | Yes | ||||||
| State fixed effects | Yes | Yes | Yes | ||||||
| Year fixed effects | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Cluster (state) | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Number of observations | 30,377 | 189 | 189 | 30,473 | 189 | 189 | 30,548 | 189 | 189 |
In all first-step OLS models, the following time-varying covariates are controlled for—at the facility level: acuity index, employment of a nurse practitioner or physician assistant, having an Alzheimer's unit, and percent Medicaid; at the county level: average number of empty beds per nursing home, number of RNs per hospital bed, number of LPNs per hospital bed, number of nursing home beds per 1,000 population 65+, Medicare-managed care penetration rate, and wage index.
In all second-step models, variables are ρ-differenced after being demeaned.
Reference category=preadoption.
Statistical significance:
p<.10.
p<.05.
p<.01.
Numbers in parentheses are robust standard errors.
We start with a baseline, conventional differences-in-differences model including facility and year fixed effects (column 1 under each outcome, Table 2). This model reveals a positive coefficient on CNA staffing during the year of pass-through adoption (β=0.0334, p<.01), a larger positive coefficient in the first year after adoption (β=0.0444, p<.01), and statistically insignificant coefficients in subsequent years (with or without the policy still in effect). For LPNs, all first-step, baseline coefficients associated with pass-through are positive but statistically insignificant (at 5 percent level). For RNs, the coefficients for the year of and first year after pass-through adoption are positive but statistically insignificant; they turn negative for the second and subsequent years after adoption, especially after the policy is repealed (β=−0.1506, p<.05). By and large, these patterns persist in the second-step OLS models (column 2 under each outcome), with the point estimate for repealing pass-through on RNs reduced by nearly half and lost in statistical significance.
Results from the final two-step FGLS model (column 3 under each outcome) indicate that the point estimates of pass-through effects on CNAs remain robust and significant: β=0.0301 (p<.05) for the year of adoption, β=0.0399 (p<.01) for the first year after adoption, β=0.0279 (p<.10) for the second and subsequent years after adoption, and β=0.0268 (p<.05) following the repealing of pass-through. No significant pass-through effect on either LPN or RN staffing is detected in the final FGLS models.
We replicate all models from Table 2 in a pooled analysis based on data from all states (excluding California and Michigan), with results reported in Table 3. As shown, the pass-through effects are washed out for CNAs, with point estimates reduced substantially. For RNs, although the first-step baseline model reveals some significant and positive pass-through impact immediately following policy adoption and a negative effect after repealing the policy, none of these associations are of statistical significance in the final FGLS model. No pass-through effect on LPNs is observed.
Table 3.
The Effect of Introducing Medicaid Wage Pass-through on Direct-Care Staffing Levels in Nursing Homes in All States (Excluding California and Michigan), 1996–2004
| CNA |
LPN |
RN |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| 2nd Step‡ |
2nd Step‡ |
2nd Step‡ |
|||||||
| 1st Step† (1) OLS | (2) OLS | (3) FGLS | 1st Step† (1) OLS | (2) OLS | (3) FGLS | 1st Step† (1) OLS | (2) OLS | (3) FGLS | |
| Wage pass-through:§ | |||||||||
| Year of adoption | 0.0289 | 0.0121 | 0.0170 | 0.0028 | 0.0086 | 0.0122 | 0.0553*** | 0.0451 | 0.0469 |
| (0.0187) | (0.0150) | (0.0121) | (0.0211) | (0.0327) | (0.0291) | (0.0185) | (0.0292) | (0.0329) | |
| 1st year after adoption | 0.0421 | 0.0233 | 0.0214 | 0.0040 | 0.0066 | 0.0074 | 0.0596* | 0.0567* | 0.0482 |
| (0.0275) | (0.0173) | (0.0158) | (0.0180) | (0.0266) | (0.0235) | (0.0297) | (0.0324) | (0.0309) | |
| 2nd/subsequent years | 0.0193 | −0.0082 | 0.0023 | −0.0175 | 0.0555 | 0.0607 | −0.0324 | 0.0012 | −0.0024 |
| (0.0314) | (0.0214) | (0.0186) | (0.0312) | (0.0431) | (0.0404) | (0.0330) | (0.0399) | (0.0358) | |
| Policy repealed | 0.0033 | −0.0030 | 0.0040 | 0.0299 | 0.0264 | 0.0312 | −0.0975** | −0.0725 | −0.0670 |
| (0.0173) | (0.0197) | (0.0169) | (0.0327) | (0.0312) | (0.0272) | (0.0443) | (0.0433) | (0.0406) | |
| Medicaid payment rate | 0.0120 | 0.0008 | 0.0003 | 0.0086 | 0.0210** | 0.0206** | −0.0077 | 0.0010 | 0.0038 |
| (0.0079) | (0.0058) | (0.0044) | (0.0074) | (0.0091) | (0.0080) | (0.0088) | (0.0077) | (0.0076) | |
| Case-mix reimbursement | −0.0004 | −0.0082 | 0.0028 | −0.0421* | −0.0109 | −0.0076 | −0.0173 | 0.0145 | 0.0175 |
| (0.0168) | (0.0188) | (0.0166) | (0.0210) | (0.0203) | (0.0161) | (0.0343) | (0.0320) | (0.0293) | |
| Facility fixed effects | Yes | Yes | Yes | ||||||
| State fixed effects | Yes | Yes | Yes | ||||||
| Year fixed effects | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Cluster (state) | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Number of observations | 66,263 | 414 | 414 | 66,551 | 414 | 414 | 66,560 | 414 | 414 |
In all first-step OLS models, the following time-varying covariates are controlled for—at the facility level: acuity index, employment of a nurse practitioner or physician assistant, having an Alzheimer's unit, and percent Medicaid; at the county level: average number of empty beds per nursing home, number of RNs per hospital bed, number of LPNs per hospital bed, number of nursing home beds per 1,000 population 65+, Medicare managed care penetration rate, and wage index.
In all second-step models, variables are ρ-differenced after being demeaned.
Reference category=Preadoption (including states that have never adopted pass-through throughout).
Statistical significance:
p<.10.
p<.05.
p<.01.
Numbers in parentheses are robust standard errors.
DISCUSSION
Our estimates indicate that among the states introducing wage pass-through during the period of 1996–2004, its implementation is associated with between 3.0 and 4.0 percent net increase in CNA HPRD in the years following policy adoption. In absolute terms, these estimates would amount to roughly an additional 27–36 minutes of CNA care per patient per week in a typical nursing home receiving wage pass-through payments. These staffing gains, arguably, are fairly moderate vis-à-vis the escalating acuity of nursing home residents (Feng et al. 2006).
Nevertheless, the finding of this positive relationship should be reassuring to state policy makers and advocates long concerned about inadequate staffing in nursing homes. The substantiation of this relationship through a rigorously designed two-step FGLS fixed-effects panel model approach provides evidence of the potential effectiveness, in the short run at least, of using Medicaid wage pass-through payments to boost direct-care staffing in nursing homes. In light of this finding, the rapid diffusion of wage pass-through programs among the states in recent years is an encouraging development. States that currently have not had a wage pass-through policy in place should perhaps consider the adoption of such a policy.
We observe a significant increase in CNA staffing immediately following pass-through adoption within 21 states that introduced pass-through over the study period, and this increase persists, although at a slower rate, even after the policy is repealed; this positive relationship no longer holds, however, in a pooled analysis including facilities from nonadopter states. One possible explanation is that when all observations from the nonadopter states are lumped in the control group the chances for detecting a policy impact have been lowered considerably, in the presence of a concurrent secular trend of increasing CNA staffing in homes across all states (which may not be fully captured by year fixed effects), particularly in those nonadopter states. It may also be the case that adding these other states increases the variance of the estimates, thereby reducing the ability to detect a difference in those states implementing the policy.
On the other hand, our final FGLS estimates suggest that although RN staffing levels do not increase significantly following pass-through adoption, they do not drop significantly, either, even after the policy is repealed. This finding is noteworthy considering the fact that there has been a continuous, counteracting trend of declining RN staffing levels in both adopter and nonadopter states throughout the study period (Feng et al. 2008). We suspect that without the pass-through policy in effect, RN staffing might have dropped more precipitously than otherwise. Furthermore, in conjunction of significant increases in CNA staffing following pass-through adoption, the finding of no significant drop in RN staffing due to the policy may suggest that there is little substitution of less skilled staff for more skilled staff going on in facilities receiving pass-through payments.
Our results also suggest that the positive effects of wage pass-through on CNAs are mostly manifest in the first 2 years of initial adoption, after which the staffing gains due to the policy diminish considerably. This raises the question as to whether such programs can be a sustainable policy vehicle to address the chronic problem of staffing shortage in nursing homes. Moreover, our state data indicate some level of instability in the provision of wage pass-through as characterized by not infrequent swings between adopting and subsequently rescinding the policy. Combined, these findings suggest that the observed staffing gains following pass-through adoption may signal some incremental benefits of a piecemeal policy shock rather than a long-term solution to nursing home staffing problems.
The costs of wage pass-through to Medicaid programs should also be considered. In a time of prolonged economic downturn, states face increased fiscal pressures and many have already or are proposing to cut their Medicaid nursing home budgets. These cuts will further constrain states' ability to initiate a wage pass-through policy or sustain an existing one. In practice, a related concern is whether nursing homes in states with a wage pass-through in place will actually put the earmarked Medicaid dollars toward hiring more direct-care staff or improving wages/benefits for current staff. Concerns have already been raised in recent state audits that many facilities may have failed to pass the Medicaid dollars on to their direct-care workers or otherwise misused the pass-through funds (Trewyn 2001; Carlson 2003;). Thus, it remains a challenge to effectively monitor the implementation of wage pass-through to make sure that the funds are spent as intended. Furthermore, to the extent that actual pass-through dollars have been diverted from investment in direct-care staff, the pass-through impact on staffing as observed in this study may have been underestimated.
Our study has several potential limitations. First, the possibility of policy endogeneity may exist and should not be overlooked. That is, the adoption of wage pass-through by certain states may be purposeful action internally driven by political, economic, and fiscal conditions or in response to consumer concerns within the state, which are unobservable and not captured in our analysis. Estimates of the policy impact may be biased if the forces that lead to policy shifts are not accounted for (Besley and Case 2000). Hence, inference about the pass-through policy effects on the basis of our findings should be made with caution. Further research may be necessary to identify and better understand those state-specific idiosyncratic factors underlying the choice of a pass-through policy.
Second, due to data constraints we could not assess the pass-through impact on direct-care staff wages, turnover, or retention. Based on panel data from the 1996 to 2001 Surveys of Income and Program Participation, a recent analysis by Baughman and Smith (2007) reports that Medicaid wage pass-through was associated with a significant 7 percent increase in wages for direct-care workers. Future research may consider using more recent, national longitudinal data to assess the impact of wage pass-through on direct-care staff wages in nursing homes using additional data sources, such as the U.S. Census Bureau's Longitudinal Employment and Household Dynamics data that provide information on worker wages and turnover on a quarterly basis. More definitive empirical evidence is needed to determine whether wage pass-through can effectively achieve these intended goals.
In addition, limitations of our study data should also be noted. Without rigorous external audits, the facility self-reported OSCAR data are prone to errors, which potentially may have biased our results despite all data-cleaning efforts. Furthermore, although we use timing to policy change to capture the nonlinear pass-through effects, other features of the policy should also be explored, such as the formulation and generosity of actual payments. There is a need as well to better understand the complexity of and substantial cross-state variations in existing pass-through programs, as is the case with other Medicaid nursing home payment policies, perhaps through a series of detailed case studies (Miller et al. 2009). Despite these limitations, this study represents an important first step toward unraveling the pass-through impact on staffing based on national longitudinal data. Thus, findings reported here provide the basis to inform ongoing discussions and additional research in this area. Lastly, a related yet unanswered, question pertains to whether the staffing gains associated with wage pass-through have in turn improved the quality of patient care, an important issue for further investigation.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This work was supported by the National Institute on Aging grants R01-AG026465 and P01-AG027296, both to Vincent Mor (PI). We appreciate the assistance of Nancy Grossman in the collection of state policy data analyzed in this paper. Preliminary results from an earlier draft of this paper were presented at the 61st Annual Scientific Meeting of the Gerontological Society of America, November 21–25, 2008, National Harbor, MD.
Disclosures: None.
Disclaimers: None.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Table SA1: Medicaid Pass-through Policy Changes in States That Ever Adopted the Policy, 1996–2004.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- Baughman R, Smith K. 2007. The Labor Market for Direct Care Workers. Working Paper. Federal Reserve Bank of Boston, New England Public Policy Center.
- BDO Seidman. A Report on Shortfalls in Medicaid Funding for Nursing Home Care. BDO Seidman; 2007. Available at http://www.ahcancal.org/research_data/funding/Documents/2007%20Medicaid%20Shortfall%20Report.pdf[accessed on March 9, 2010] [Google Scholar]
- Bertrand M, Duflo E, Mullainathan S. How Much Should We Trust Differences-in-Differences Estimates? Quarterly Journal of Economics. 2004;119(1):249–75. [Google Scholar]
- Besley T, Case A. Unnatural Experiments? Estimating the Incidence of Endogenous Policies. The Economic Journal. 2000;110(467):672–94. [Google Scholar]
- Bostick JE, Rantz MJ, Flesner MK, Riggs CJ. Systematic Review of Studies of Staffing and Quality in Nursing Homes. Journal of the American Medical Directors Association. 2006;7(6):366–76. doi: 10.1016/j.jamda.2006.01.024. [DOI] [PubMed] [Google Scholar]
- Carlson E. Payment Due: California's Leaky System to Improve the Wages of Nursing Home Employees. Los Angeles, CA: National Senior Citizens Law Center; 2003. [Google Scholar]
- Centers for Medicare and Medicaid Services. Report to Congress: Appropriateness of Minimum Nurse Staffing Ratios in Nursing Homes, Phase I. Baltimore, MD: Centers for Medicare and Medicaid Services: 2000. [Google Scholar]
- Centers for Medicare & Medicaid Services. Report to Congress: Appropriateness of Minimum Nurse Staffing Ratios in Nursing Homes, Phase II. Baltimore, MD: Centers for Medicare and Medicaid Services: 2001. [Google Scholar]
- Feng Z, Grabowski DC, Intrator O, Mor V. The Effect of State Medicaid Case-Mix Payment on Nursing Home Resident Acuity. Health Services Research. 2006;41(4, part 1):1317–36. doi: 10.1111/j.1475-6773.2006.00545.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng Z, Grabowski DC, Intrator O, Zinn J, Mor V. Medicaid Payment Rates, Case-Mix Reimbursement, and Nursing Home Staffing-1996–2004. Medical Care. 2008;46(1):33–40. doi: 10.1097/MLR.0b013e3181484197. [DOI] [PubMed] [Google Scholar]
- Foster A, Lee YS. 2009. Staffing Subsidies and the Quality of Care in Nursing Homes—FGLS Estimates: How to Effectively Double the Number of States in Your Analysis. Working Paper. Providence, RI: Department of Economics, Brown University.
- Grabowski DC. A Longitudinal Study of Medicaid Payment, Private-Pay Price and Nursing Home Quality. International Journal of Health Care Finance Economics. 2004;4(1):5–26. doi: 10.1023/b:ihfe.0000019258.29496.03. [DOI] [PubMed] [Google Scholar]
- Grabowski DC. The Market for Long-Term Care Services. Inquiry. 2008;45(1):58–74. doi: 10.5034/inquiryjrnl_45.01.58. [DOI] [PubMed] [Google Scholar]
- Grabowski DC, Feng Z, Intrator O, Mor V. Health Affairs (Millwood) 2004. Recent Trends in State Nursing Home Payment Policies; pp. W-4: 363–73. [DOI] [PubMed] [Google Scholar]
- Grabowski DC. Medicaid Nursing Home Payment and the Role of Provider Taxes. Medical Care Research Review. 2008;65(4):514–27. doi: 10.1177/1077558708315968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen CB. Generalized Least Squares Inference in Panel and Multilevel Models with Serial Correlation and Fixed Effects. Journal of Econometrics. 2007;140(2):670–94. [Google Scholar]
- Intrator O, Feng Z, Mor V, Gifford D, Bourbonniere M, Zinn J. The Employment of Nurse Practitioners and Physician Assistants in U.S. Nursing Homes. Gerontologist. 2005;45(4):486–95. doi: 10.1093/geront/45.4.486. [DOI] [PubMed] [Google Scholar]
- Miller EA, Mor V, Grabowski DC, Gozalo PL. The Devil's in the Details: Trading Policy Goals for Complexity in Medicaid Nursing Home Reimbursement. Journal of Health Politics, Policy, and Law. 2009;34(1):93–135. doi: 10.1215/03616878-2008-993. [DOI] [PubMed] [Google Scholar]
- North Carolina Division of Facility Services. Comparing State Efforts to Address the Recruitment and Retention of Nurse Aide and Other Paraprofessional Aide Workers. Raleigh, NC: North Carolina Division of Facility Services; 1999. [Google Scholar]
- North Carolina Division of Facility Services. Results of a Follow-Up Survey to States on Wage Supplements for Medicaid and Other Public Funding To Address Aide Recruitment and Retention In Long-Term Care Settings. Raleigh, NC: North Carolina Division of Facility Services; 2000. [Google Scholar]
- Paraprofessional Healthcare Institute. 2003. State Wage Pass-Through Legislation: An Analysis. Workforce Strategies: No. 1. Prepared for the Office of Disability, Aging and Long-Term Care Policy and Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services.
- Scanlon WJ. Nursing Workforce: Recruitment and Retention of Nurses and Nurse Aides Is a Growing Concern. Washington, DC: U.S. General Accounting Office; 2001. [Google Scholar]
- Smith K, Baughman R. 2007. “Caring for America's Aging Population: A Profile of the Direct-Care Workforce.” Monthly Labor Review, September, 20–6.
- Super N. Who Will Be There to Care? The Growing Gap between Caregiver Supply and Demand. Washington, DC: The George Washington University; 2002. [Google Scholar]
- Trewyn P. Audit Says Nursing Homes Didn't Pass through Wage Increases. The Business Journal of Milwaukee. 2001 February 2, 2001, p. 2. [Google Scholar]
- Walker JS, Angelotti S, Patterson D. Medicaid Funding for Nursing Home Services: A Historical Perspective. Lansing, MI: Michigan Senate Fiscal Agency; 2000. [Google Scholar]
- Wiener JM, Freiman MP, Brown D. 2007. Nursing Home Care Quality: Twenty Years after the Omnibus Budget Reconciliation Act of 1987. Commissioned by the Kaiser Family Foundation.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.