Abstract
Objective
To determine how reliance on Veterans Affairs (VA) for medical care among veterans enrolled in Medicare is affected by medical conditions, access, and patient characteristics.
Data Sources/Study Setting
Department of Veterans Affairs.
Study Design
We examined reliance on the VA for inpatient, outpatient, and overall medical care among all VA users in fiscal years 2003 and 2004 who were also enrolled in Medicare. We calculated the marginal effects of patient factors on VA reliance using fractional logistic regression; we also analyzed overall VA reliance separately for under-65 and age-65+ groups. The primary focus of this analysis was the relationship between aggregated condition categories (ACCs), which represent medical conditions, and reliance on the VA.
Principal Findings
Mean VA reliance was significantly higher in the under-65 population than in the age-65+ group (0.800 versus 0.531). Lower differential distance to the VA, and higher VA-determined priority for health care, predicted higher VA reliance. Most individual ACCs were negatively associated with VA reliance, though substance abuse and mental health disorders were significantly associated with increased reliance on VA care. Conditions of the eyes and ears/nose/throat had positive marginal effect on VA reliance for the under 65, while diabetes was positive for age 65+. Among inpatients, veterans with ACCs for mental health conditions, eye conditions, amputations, or infectious and parasitic conditions had higher likelihood of a VA hospitalization than inpatients without these conditions.
Conclusions
Many dually enrolled Veterans use both Medicare and VA health care. Age, accessibility, and priority level for VA services have a clear relationship with VA reliance. Because dual use is common, coordination of care among health care settings for such patients should be a policy priority.
Keywords: Access to health care, veterans, Medicare, health services research, health services
The Veterans Affairs (VA) Health Care System is the largest integrated health care system in the United States, with a medical care and research budget of U.S.$32.5 billion in fiscal year (FY) 2005. More than 5.4 million veterans received care in the VA in FY 2005. Although the Veterans Health Administration (VHA) has the responsibility to provide comprehensive medical care to veterans, many veterans have multiple options for medical care and may choose to use other health systems in addition to or instead of the VA. Medicare is one such alternative to the VA system. In FY 1999, 35 percent of veterans qualified for Medicare coverage due to age (65 and older), and 7 percent of veterans (who were younger than 65 years) were eligible for Medicare through Social Security Disability benefits, for a total of 42 percent of Veterans having Medicare eligibility (VA Information Resource Center 2003).
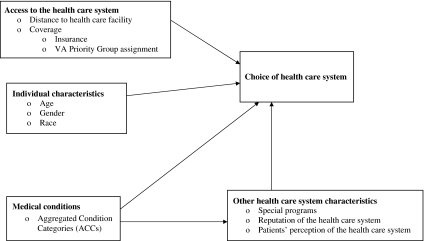
Previous research shows that dually enrolled veterans make use of VA health care as well as non-VA health care under Medicare financing, possibly in a complementary manner (Shen et al. 2003; Rosen et al. 2005; Keyhani et al. 2007;). There are a number of factors that may affect an individual's choice about where to obtain health care when there is more than one option. Figure 1 illustrates a conceptual model of possible factors affecting patients' selection of a health care system. Our framework posits that access to a health care system, individual demographic characteristics, individual medical conditions, and health care system attributes will affect decisions about health system use.
Figure 1.
Factors Influencing Choice of Health Care System
Specific aspects of access to a health care system include distance to health care facilities and coverage in the system. Research has found that the further the distance to the nearest VA hospital or clinic, the less likely it is that veterans will come to the VA for medical, surgical, or primary care (Burgess and DeFiore 1994; Mooney et al. 2000; Hynes et al. 2007;). Further distance from VA facilities also predicted lower utilization of VA transplant care (Weeks and West 2007), mental health and substance abuse (MH/SA) services (McCarthy et al. 2007; Carey et al. 2008;), and stroke care among dually enrolled veterans (Shen et al. 2008). For MH/SA services, Carey et al. (2008) found that as the distance to VA facilities increased, VA expenditures decreased, and a complementary result is seen for reduced access to Medicare facilities (Carey et al. 2008). Because health care under Medicare financing can be obtained in more locations than VA care (due to the limited number of VA facilities), residence in a rural versus urban setting may also be a determinant of where veterans receive their health care.
Regarding the coverage aspect of access, the amount of out-of-pocket costs that an individual faces may also affect choice of health care system. A study by Shen et al. (2003) showed that dually enrolled veterans who have private Medicare supplemental insurance (Medigap) are more likely to use Medicare than the VA. In the VA setting, priority level for services (assigned based on the veteran's severity of service-connected disabilities and income level) is a proxy for coverage and out-of-pocket cost, and higher priority veterans (those who face less in out-of-pocket expenses) have been shown to be more likely to rely on the VA for health care (Hynes et al. 2007).
The choice of whether to obtain VA versus non-VA health care may also be affected by specific medical conditions, and thus need for treatment of these conditions. Studies of dually eligible veterans have found that the majority of VA users hospitalized for acute myocardial infarction (Wright et al. 1997, 1999) and stroke (Shen et al. 2008) were admitted to Medicare hospitals, rather than VA hospitals, for their initial care. Over 80 percent of coronary revascularization procedures done for dually eligible veterans in New York during 1999 and 2000 were performed outside of the VA system (Weeks et al. 2006). In addition, Medicare-eligible veterans obtain the vast majority (86 percent) of solid-organ (liver, kidney, and heart) transplants through Medicare coverage, rather than within the VA health care system (Weeks and West 2007). On the other hand, for less acute conditions, over 94 percent of dually enrolled veterans with a MH/SA diagnosis use VA MH/SA services, while fewer than 28 percent of these veterans use Medicare for MH/SA services (Carey et al. 2008). Such prior research in this area lends credence to the notion that decisions about health care use may be driven by particular ailments. However, the extent to which various medical conditions concurrently influence VA versus Medicare use has not been comprehensively studied.
Therefore, in the present study we examine the effect of a variety of factors on the proportion of care obtained from the VA (VA Reliance) among veterans enrolled in both the VA and Medicare. Our research is an important advance over previous research in a number of ways. First, we include all dually enrolled users of the VA health system, rather than restricting our focus to a specific disease or treatment, and we explore the association of health care system reliance with a comprehensive set of disease conditions as classified by aggregated condition categories (ACCs). Our cost calculations on the Medicare side include patient out-of-pocket and supplemental insurance payments; this reflects the higher cost sharing that Medicare users face and which are also part of the system costs. We include demographic and access variables—including gender, differential distance between VA and non-VA facilities, and VA priority level—that may contribute to use of one or both settings, and we examine the interaction between these factors and the ACCs. Finally, our study separately considers the younger Medicare-disabled and the Medicare-elderly populations, as individual characteristics, illness conditions, and patterns of utilization are different for these groups.
METHODS
Patient Population and Data Sources
We identified a cohort of veterans who were VA users and also enrolled in fee-for-service (FFS) Medicare. All veterans who had inpatient or outpatient VA or Fee basis use (for care paid by the VA in non-VA settings) in FY 2003 and 2004 in VA priority groups 1–8 were included. The patients were identified as VA users in the VA Allocation Resource Center's Adjusted Decision Support System file and the VHA Assistant Deputy Under Secretary for Health Monthly Enrollment file or Fee basis file. These records were matched against the VA Information Resource Center's VA Medicare-merged dataset (VA Information Resource Center 2003) for that period (October 2002–September 2004), resulting in a cohort of 2,077,773 VA participants who were also Medicare enrollees in FY 2003 and FY 2004. The Institutional Review Board for Baylor College of Medicine and the Michael E. DeBakey VA Medical Center approved this study. We applied several exclusion criteria to the initial cohort. First, veterans who had missing VA priority group classification were excluded; however, this number was quite small—245. We also excluded veterans with missing or unusable diagnostic data, generally resulting from invalid International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] codes (266 patients) and those who died in FY 2003 or FY 2004 (103,011). Finally, we excluded patients with missing (701) zip codes and patients whose zip codes were outside of the 50 states and District of Columbia (30,420 patients). One patient was excluded because of recorded age ≤17. Applying these exclusion criteria yielded a final cohort of 1,943,129 veterans.
Outcome Variables
Our primary outcome of interest was reliance on VA health care, calculated as the veteran's VA costs divided by his or her combined VA and Medicare costs for FY, expressed as a proportion from 0 to 1. The Medicare program requires extensive cost-sharing by patients, sometimes borne by supplemental insurance. To capture comprehensive costs of Medicare services, we included the patient out-of-pocket and supplemental insurance payments; these data are available in the Medicare claims files. We examined three types of reliance: a measure of overall VA reliance representing all health care use; a measure using only outpatient (ambulatory) care costs; and one for inpatient care, broken down based on locations of hospitalization (in VA only, in Medicare only, and in both settings).
The extent of VA service use was determined by examining the VA National Patient Care database (NPCD) and Fee basis (services from non-VA providers but paid for by VA) files for all inpatient and outpatient services during the respective FYs. For inpatient care, both acute and extended care stays were included. We obtained health care use costs from the VA Health Economics Resource Center (HERC) inpatient and outpatient Average Cost Datasets (ACDs) for VA Care (Phibbs et al. 2003; Wagner, Chen, and Barnett 2003;). HERC developed these patient-level databases by combining VA cost and utilization data with external (primarily Medicare) relative value weights. The HERC ACDs provide externally valid cost data that are reliable for use in comparisons across VA facilities and VA regional networks, as well as between VA and non-VA settings. Our measures of VA reliance also included VA pharmacy costs, which were taken from the VA Decision Support System files. Outpatient VA reliance was calculated using the same data sources, though excluding costs associated with inpatient stays. Overall and outpatient reliance measures are examined as continuous proportions between and including 0 and 1. Inpatient reliance was coded as a categorical variable with three values: VA-only inpatient use, Medicare-only inpatient use, and both VA and Medicare inpatient use.
We determined use of Medicare services with Medicare FFS claims files. Specifically, for inpatient care we searched the Medicare provider and analysis review file and physician/supplier claims that were concurrent (±1 day) with inpatient stays. For outpatient care, we used the outpatient, carrier (physician/supplier), home health, Hospice and Durable Medical Equipment Standard Analytic files (SAFs). We used an algorithm provided by CMS' Research Data Assistance Center to calculate the Medicare provider payment. This payment is essentially the sum of three components: the payment made by Medicare, the payment made by the beneficiary (co-insurance and deductibles), and any payment made by a primary payer.
Independent Variables
We obtained data on patient age, gender, and death events from the VA vital status file. Because race data are incomplete in VA databases, we obtained race information from Medicare enrollment databases.
Differential Distance between Nearest VA and Nearest Non-VA Hospital
As a differential measure of a veteran's access to VA versus non-VA medical care, we constructed the following differential distance measure: (distance from patient's zip code to the nearest VA Medical Center [VAMC] zip code) minus (distance from patient's zip code to the nearest non-VA Medicare-participating hospital zip code). Differential distance measures have been used in previous research of veteran access to health care (Maciejewski et al. 2007; Brahmajee et al. 2008;) to capture excess distance between a VA hospital and a (generally nearer) non-VA hospital. To carry out this calculation, we first obtained each patient's zip code from Medicare denominator files. We then obtained a list of all VAMCs and their zip codes from the VA Station Tracking database as well as a list of all Medicare hospitals and their zip codes from the Medicare Point-Of-Service (POS) file, excluding hospitals specializing in care of veterans, active military, children, or women. To determine the distance to the nearest VAMC for each valid patient zip code, the distances between that zip code (excluding those outside the United States) and all VAMC-containing zip codes were first calculated using an algorithm, based on the inverse tangent Haversine formula, provided by the VAHERC (2009). The least of these distances was then accepted as the distance to the nearest VAMC. The distance to the nearest Medicare Hospital was calculated similarly, though testing all Medicare hospital-containing zip codes. The variable was categorized into differential distance intervals (<5, 5–19, 20–39, 40–59, 60+miles) due to the nonlinear nature of the relationship between distance and VA reliance. The interval <5 miles included the negative differential distances, that is, the cases where the nearest VAMC is closer to the patient than the nearest Medicare hospital; an examination of the relationship between a negative differential distance and VA reliance revealed that this relationship was similar to the 0–5-mile differential distance.
Priority
Each veteran enrolled in the VA health care system is assigned a priority level. Priority levels range from 1 to 8 and are assigned based on the veteran's severity of service-connected disabilities and income level (veterans Health Administration 2007). Veterans in priority categories 7–8 do not have a service-connected disability, and they pay a co-payment for VA services. Veterans with priority levels 1–6 have some measure of service-connected disability or have low income. For our analyses, we divided veterans into four categories based on priority level: priority 7–8 (reference); priority 5 (low income); priority 2, 3, and 6 (low to moderate disability); and priority 1 and 4 (high disability).
Disease Conditions
We categorized health conditions using a diagnosis-based risk adjustment methodology developed and licensed by the DxCG Company (Ellis et al. 1996). In the Diagnostic Cost Group algorithm, >15,000 ICD-9-CM codes are partitioned into 545 clinically specific groups called DxGroups. These DxGroups are clustered into condition categories according to similarities in clinical condition and resource use. Condition categories that are related and affect the same organ system are then arranged hierarchically to create 184 hierarchical condition categories (HCCs). Patients are assigned the most severe condition they have within a hierarchy. In previous work, we have shown that this methodology has strong clinical validity in the VA population, with risk of mortality increasing monotonically with more severe diagnostic categories (Petersen et al. 2005). The DxCG software also provides ACCs, which are groups of HCCs that encompass certain disease groups such as diabetes or certain organ systems such as the cerebrovascular system. A patient may have more than one ACC, and most do. As ACCs indicate occurrence of a specific disease group, they are not mutually exclusive categories.
The ICD-9-CM codes contributing to the ACCs were combined from both the VA and Medicare sources: the VA NPCD and Fee basis files as well as Medicare claims files. We excluded five ACCs from our analyses either because of rarity in the VA (pregnancy-related, neonates, and developmental disability) or because the ACC did not represent a clinical condition, but rather a loosely defined nonclinical ‘catchall’ category for a minor issue or case history (ill-defined symptoms/conditions, screening/history).
Data Analysis
We calculated the mean VA reliance score within each of the demographic and distance categories and each of 26 ACCs. We also calculated the prevalence of each condition among dual users and users of the VA alone. Finally, we used two types of regression models, described below, to predict the effect of each ACC on VA reliance adjusting for age, gender, race, priority level, and our differential distance variable.
Because our outcome variables for overall reliance and outpatient reliance are fractions between, and including, 0 and 1, we could not use either ordinary least squares linear regression or log-odds procedures. With ordinary least squares linear regression, predicted values from the regression are not restricted to the 0–1 interval. In the case of modeling the log-odds ratio, if any outcome variable takes on the value of 0 or 1 with positive probability, an adjustment has to be made before computing the log-odds ratio. In addition, beyond this, it is problematic to recover the expected values of the fractional outcome variable. Thus, in our analysis of overall and outpatient reliance measures, we used a regression model developed by Papke and Wooldridge (1996). This model, known as the fractional logistic model, is used widely in economics research to model proportions (Fairris and Pedace 2004; Hendershott and Pryce 2006; Mann and Powers 2007;). Kieschnick and McCullough (2003) have identified this model, which uses a quasi-maximum likelihood estimation procedure, as the most suitable method for general use across disciplines when the outcome is a proportion.
The basic equation for this model is
where xi is a vector of covariates and β the corresponding vector of parameters. This model allows the dependent variable y to take on the values between and including 0 and 1, and the predicted values lie on the open interval (0,1). Papke and Wooldridge (1996) found that the parameter estimates can be consistently estimated regardless of the distribution of the dependent variable. We present the marginal effect and standard error of each covariate, a common presentation for the fractional logistic model (Kieschnick and McCullough 2003). The marginal effect of a categorical independent variable is the estimated amount that the VA reliance would change if that independent variable changed from 0 to 1, with the other independent variables held at their mean values.
We conducted separate analyses to estimate the effect of ACCs and other patient characteristics on overall VA reliance and VA outpatient reliance. Both analyses used the fractional logistic model and were conducted using Stata version 10 (StataCorp LP, College Station, TX, 2007). For overall VA reliance we analyzed data from the population described above (N=1,943,129) and estimated the effects of patient characteristics separately for patients under 65 who qualified for Medicare, and patients aged 65 and older, as these populations are clinically distinct. To predict outpatient VA reliance as a function of ACCs and other variables, we applied the fractional logistic model to the subset of the population with at least one outpatient episode (N=1,942,290) using outpatient VA reliance as the dependent variable.
To predict the effect of patient characteristics on inpatient stays, we conducted multinomial logistic regression analysis using SAS version 9.1 (SAS Institute Inc., Cary, NC, 2002). All patients included in this analysis (N=731,227) had at least one inpatient stay in at least one of the settings. We estimated the effects of ACCs and other characteristics on a categorical variable with three values: VA-only inpatient use, Medicare-only inpatient use, and both VA and Medicare inpatient use. Medicare-only use was the reference group for the analysis. This modeling technique, which has been used in previous research (Hynes et al. 2007), is more appropriate for inpatient use because only 10 percent of the hospitalized patients had inpatient use in both systems.
We also examined 12 pairs of ACCs with the clinical potential for interaction effects. Most of these pairs are notable for co-occurring in patients with multiple chronic illnesses, while others included ACCs indicative of an acute illness (e.g., cardio-respiratory arrest) paired with a chronic condition ACC (e.g., diabetes).
Finally, we examined interactions of age and distance, age and the substance abuse ACC, and age and the mental health ACC. Because the sample is actually a large population, the interactions are significant, but the parameter effects are less than the main effects. In view of the large number of main effects, these interaction results did not appear to add additional insight and are not shown.
RESULTS
Table 1 displays the demographic, access, and clinical condition characteristics, along with mean VA reliance, of the two dual enrollee populations: under age 65, who qualify for Medicare through disability; and age 65 and older. Approximately one-sixth (16.8 percent) of the full cohort were under age 65. Not surprisingly, patients were predominantly male (95.1 percent of the under 65 group and 98.2 percent of the 65+ group, but still significantly different at p<.001). Differential distance categories were distributed similarly in both populations. However, the two populations differed with respect to several characteristics, including race. While 19.5 percent of the under-65 group were black, black veterans comprised only 7.6 percent of the 65+ group (p<.001). The under-65 population also had a larger proportion of high disability priority classification (48.4 percent) than did the older population (12.9 percent, p<.001). While the priority 7–8 veterans accounted for only 7.1 percent of the under-65 group, they comprised 37.5 percent of the 65+ population (p<.001). Some of the clinical conditions, represented by ACCs, also differed in the two cohorts. For example, the under-65 group had three times the percentage of substance abuse occurrence (43.6 percent versus 13.4 percent, p<.001) as that of the 65+ veterans. Similarly, the proportion of under-65 patients with the mental health ACC (67.9 percent) is over twice that in the age-65+ veterans (29.0 percent, p<.001). The proportion of patients with the liver ACC was 14.6 percent in the under-65 group, but only 7.0 percent in the 65+ cohort (p<.001). However, the malignant neoplasm ACC occurred in a much higher proportion of 65+ veterans (36.3 percent) than in under-65 patients (17.7 percent, p<.001).
Table 1.
Characteristics and Mean VA Reliance for FY04 Dual VA-Medicare Users
| Age under 65 |
Age 65+ |
|||
|---|---|---|---|---|
| Variable | N (%) | Mean VA Reliance | N (%) | Mean VA Reliance |
| Total | 325,622 (100) | 0.800 | 1,617,507 (100) | 0.531 |
| Male | 309,557 (95.1) | 0.800 | 1,587,729 (98.2) | 0.530 |
| Female | 16,065 (4.9) | 0.811 | 29,778 (1.8) | 0.553 |
| Black | 63,461 (19.5) | 0.810 | 123,114 (7.6) | 0.737 |
| Non-black | 262,161 (80.5) | 0.798 | 1,494,393 (92.4) | 0.514 |
| Priority 7–8: non-disabled, copayment required | 23,279 (7.1) | 0.658 | 607,190 (37.5) | 0.406 |
| Priority 5: low income | 105,315 (32.3) | 0.773 | 562,487 (34.8) | 0.622 |
| Priority 1, 4: high disability | 157,653 (48.4) | 0.843 | 208,323 (12.9) | 0.632 |
| Priority 2, 3, 6: low/moderate disability | 39,375 (12.1) | 0.785 | 239,507 (14.8) | 0.544 |
| Differential distance*: <5 miles | 67,908 (20.9) | 0.863 | 281,322 (17.4) | 0.648 |
| Differential distance: 5–19 miles | 77,109 (23.7) | 0.824 | 367,545 (22.7) | 0.547 |
| Differential distance: 20–39 miles | 58,887 (18.1) | 0.789 | 317,644 (19.6) | 0.508 |
| Differential distance: 40–59 miles | 49,576 (15.2) | 0.764 | 257,762 (15.9) | 0.495 |
| Differential distance: 60+ miles | 72,142 (22.2) | 0.750 | 393,234 (24.3) | 0.473 |
| Age: <65 years | — | — | — | — |
| Age: 65–74 years | — | — | 743,944 (46.0) | 0.599 |
| Age: 75+ years | — | — | 873,563 (54.0) | 0.473 |
| Indicator for presence of ACC† | ||||
| ACC01: infectious and parasitic | 100,691 (30.9) | 0.744 | 559,104 (34.6) | 0.467 |
| ACC02: malignant neoplasm | 57,660 (17.7) | 0.732 | 587,736 (36.3) | 0.443 |
| ACC03: benign/in situ neoplasm | 32,764 (10.1) | 0.762 | 262,847 (16.3) | 0.460 |
| ACC04: diabetes | 105,818 (32.5) | 0.750 | 568,510 (35.1) | 0.503 |
| ACC05: nutritional and metabolic | 236,647 (72.7) | 0.772 | 1,342,537 (83.0) | 0.498 |
| ACC06: liver | 47,445 (14.6) | 0.716 | 113,289 (7.0) | 0.355 |
| ACC07: gastrointestinal | 180,159 (55.3) | 0.755 | 999,719 (61.8) | 0.470 |
| ACC08: musculoskeletal and connective | 240,259 (73.8) | 0.778 | 1,241,039 (76.7) | 0.493 |
| ACC09: hematological | 67,239 (20.6) | 0.647 | 532,159 (32.9) | 0.398 |
| ACC10: cognitive disorders | 35,542 (10.9) | 0.713 | 203,326 (12.6) | 0.410 |
| ACC11: substance abuse | 142,012 (43.6) | 0.788 | 215,976 (13.4) | 0.577 |
| ACC12: mental | 221,227 (67.9) | 0.808 | 469,622 (29.0) | 0.517 |
| ACC14: neurological | 114,722 (35.2) | 0.748 | 424,389 (26.2) | 0.450 |
| ACC15: cardio-respiratory arrest | 18,479 (5.7) | 0.503 | 116,799 (7.2) | 0.281 |
| ACC16: heart | 233,142 (71.6) | 0.766 | 1,467,249 (90.7) | 0.514 |
| ACC17: cerebro-vascular | 44,140 (13.6) | 0.667 | 404,424 (25.0) | 0.398 |
| ACC18: vascular | 76,577 (23.5) | 0.664 | 645,747 (39.9) | 0.416 |
| ACC19: lung | 135,001 (41.5) | 0.710 | 782,997 (48.4) | 0.442 |
| ACC20: eyes | 179,893 (55.2) | 0.798 | 1,197,479 (74.0) | 0.501 |
| ACC21: ears, nose, and throat | 194,942 (59.9) | 0.795 | 957,256 (59.2) | 0.493 |
| ACC22: urinary system | 90,288 (27.7) | 0.691 | 702,536 (43.4) | 0.424 |
| ACC23: genital system | 89,981 (27.6) | 0.749 | 805,282 (49.8) | 0.462 |
| ACC25: skin and subcutaneous | 144,396 (44.3) | 0.768 | 925,092 (57.2) | 0.479 |
| ACC26: injury, poisoning, complications | 144,545 (44.4) | 0.720 | 716,158 (44.3)‡ | 0.426 |
| ACC29: transplants, openings, amputations | 12,890 (4.0) | 0.674 | 50,231 (3.1) | 0.424 |
| Presence of selected ACC comorbidity pairs | ||||
| ACCs 4, 6: diabetes+liver | 17,351 (5.3) | 0.639 | 48,623 (3.0) | 0.333 |
| ACCs 4, 15: diabetes+cardio-respiratory arrest | 9,365 (2.9) | 0.474 | 54,742 (3.4) | 0.265 |
| ACCs 4, 16: diabetes+heart | 95,269 (29.3) | 0.736 | 548,287 (33.9) | 0.496 |
| ACCs 4, 17: diabetes+cerebro-vascular | 19,629 (6.0) | 0.617 | 172,071 (10.7) | 0.379 |
| ACCs 4, 20: diabetes+eyes | 78,157 (24.0) | 0.762 | 475,605 (29.4) | 0.499 |
| ACCs 4, 22: diabetes+urinary | 39,231 (12.1) | 0.640 | 288,599 (17.8) | 0.409 |
| ACCs 4, 29: diabetes+transplants, openings, amputations | 6,003 (1.8) | 0.635 | 22,546 (1.4) | 0.414 |
| ACCs 11, 12: substance abuse+mental health | 110,919 (34.1) | 0.794 | 85,419 (5.3) | 0.552 |
| ACCs 16, 17: heart+cerebro-vascular | 39,168 (12.0) | 0.648 | 392,813 (24.3) | 0.392 |
| ACCs 16, 18: heart+vascular | 68,172 (21.0) | 0.645 | 622,077 (38.5) | 0.408 |
| ACCs 17, 18: cerebro-vascular+vascular | 20,616 (6.3) | 0.564 | 251,180 (15.5) | 0.341 |
| ACCs 20, 22: urinary+eyes | 56,007 (17.2) | 0.695 | 550,793 (34.1) | 0.409 |
Distance to the nearest VA Medical Center minus the distance to the nearest non-VA Medicare-participating hospital; greater positive values suggest the patient lives closer to a non-VA Medicare hospital.
ACCs are not mutually exclusive; most veterans have multiple HCCs.
Difference in proportion of population with the variable not significant at p<.001. All differences in VA reliance means were significant at p<.001.
ACC, aggregated condition category; VA, Veterans Affairs.
Mean VA reliance was dramatically higher in the under-65 group than in the older population for all the characteristics we studied. Mean overall VA reliance in the under-65 group was 0.800, while it was 0.531 in the 65+ group (p<.001). Within the 65+ group, mean VA reliance was higher for ages 65–74 (0.599) compared with that of veterans age 75 and older (0.473, p<.001). The only characteristic where mean VA reliance was somewhat similar in both age groups was in the black racial category, with mean VA reliance of 0.810 in the under-65 population and 0.737 in the 65+ group (but still significantly different at p<.001).
Within both groups, we observed variation in mean VA reliance by ACC indicators as well as other covariates. Consistent with previous work (Hynes et al. 2007), we found that proximity to the VA and VA priority levels indicative of lower income and higher disability were associated with increased VA reliance. With respect to ACCs, MH/SA conditions are associated with relatively high VA reliance (mental health in the under-65 group (0.808 versus 0.800 overall), and substance abuse in the 65+ group (0.577 compared with the overall 0.531), while cardio-respiratory arrest is associated with relatively low VA reliance (0.503 in the younger group, and 0.281 in the age 65+ cohort). In the pairs of comorbid conditions that we assessed, only the combined MH/SA in the 65+ cohort was higher than the overall reliance, with a mean VA reliance of 0.552.
Table 2 shows the distribution of the disease groups and other categories among dual users and users of the VA alone. The VA-only users are more likely than the dual users to be black, to qualify for the low-income or high disability priority categories, and to be younger than 65, reflecting the role of the VA as a safety-net type of health care provider. Again, the MH/SA ACCs are found in higher percentages among VA-only users than among dual users; these are the only ACCs that are more prevalent in the VA-only user subgroup. All differences in prevalence between dual users and VA-only users are statistically significant.
Table 2.
Prevalence of Variables among Dual Users and Users of VA Alone
| Variable | N (%) among Dual Users | N (%) among Users of VA Alone |
|---|---|---|
| Total | 1,553,340 | 389,789* |
| Male | 1,518,555 (97.8) | 378,731 (97.2) |
| Female | 34,785 (2.2) | 11,058 (2.8) |
| Black | 113,588 (7.3) | 72,987 (18.7) |
| Non-black | 1,439,752 (92.7) | 316,802 (81.3) |
| Priority 7–8: | 581,339 (37.4) | 49,130 (12.6) |
| Priority 5: low income | 498,747 (32.1) | 169,055 (43.4) |
| Priority 1, 4: high disability | 249,097 (16.0) | 116,879 (30.0) |
| Priority 2, 3, 6: low/moderate disability | 224,157 (14.4) | 54,725 (14.0) |
| Differential distance: <5 miles† | 236,291 (15.2) | 112,939 (29.0) |
| Differential distance: 5–19 miles | 338,355 (21.8) | 106,299 (27.3) |
| Differential distance: 20–39 miles | 311,349 (20.0) | 65,182 (16.7) |
| Differential distance: 40–59 miles | 262,400 (16.9) | 44,938 (11.5) |
| Differential distance: 60+ miles | 404,945 (26.1) | 60,431 (15.5) |
| Age: <65 years | 189,537 (12.2) | 136,085 (34.9) |
| Age: 65–74 years | 588,494 (37.9) | 155,450 (39.9) |
| Age: 75+ years | 775,309 (49.9) | 98,254 (25.2) |
| ACC01: infectious and parasitic | 565,623 (36.4) | 94,172 (24.2) |
| ACC02: malignant neoplasm | 562,387 (36.2) | 83,009 (21.3) |
| ACC03: benign/in situ neoplasm | 259,617 (16.7) | 35,994 (9.2) |
| ACC04: diabetes | 562,272 (36.2) | 112,056 (28.8) |
| ACC05: nutritional and metabolic | 1,317,693 (84.8) | 261,491 (67.1) |
| ACC06: liver | 137,779 (8.9) | 22,955 (5.9) |
| ACC07: gastrointestinal | 1,005,109 (64.7) | 174,769 (44.8) |
| ACC08: musculoskeletal and connective | 1,239,017 (79.8) | 242,281 (62.2) |
| ACC09: hematological | 539,934 (34.8) | 59,464 (15.3) |
| ACC10: cognitive disorders | 215,182 (13.9) | 23,686 (6.1) |
| ACC11: substance abuse | 258,712 (16.7) | 99,276 (25.5) |
| ACC12: mental | 537,185 (34.6) | 153,664 (39.4) |
| ACC14: neurological | 460,807 (29.7) | 78,304 (20.1) |
| ACC15: cardio-respiratory arrest | 129,237 (8.3) | 6,041 (1.6) |
| ACC16: heart | 1,404,251 (90.4) | 296,140 (76.0) |
| ACC17: cerebro-vascular | 406,129 (26.2) | 42,435 (10.9) |
| ACC18: vascular | 647,814 (41.7) | 74,510 (19.1) |
| ACC19: lung | 803,949 (51.8) | 114,049 (29.3) |
| ACC20: eyes | 1,157,068 (74.5) | 220,304 (56.5) |
| ACC21: ears, nose, and throat | 962,581 (62.0) | 189,617 (48.7) |
| ACC22: urinary system | 705,774 (45.4) | 87,050 (22.3) |
| ACC23: genital system | 783,713 (50.5) | 111,550 (28.6) |
| ACC25: skin and subcutaneous | 916,486 (59.0) | 153,002 (39.3) |
| ACC26: injury, poisoning, complications | 763,861 (49.2) | 96,842 (24.8) |
| ACC29: transplants, openings, amputations | 54,711 (3.5) | 8,410 (2.2) |
| Presence of selected ACC comorbidity pairs | ||
| ACCs 4, 6: diabetes+liver | 59,199 (3.8) | 6,775 (1.7) |
| ACCs 4, 15: diabetes+cardio-respiratory arrest | 61,823 (4.0) | 2,284 (0.6) |
| ACCs 4, 16: diabetes+heart | 542,516 (34.9) | 101,040 (25.9) |
| ACCs 4, 17: diabetes+cerebro-vascular | 176,700 (11.4) | 15,000 (3.9) |
| ACCs 4, 20: diabetes+eyes | 466,436 (30.0) | 87,326 (22.4) |
| ACCs 4, 22: diabetes+urinary | 296,808 (19.1) | 31,022 (8.0) |
| ACCs 4, 29: diabetes+transplants, openings, amputations | 25,246 (1.6) | 3,303 (0.9) |
| ACCs 11, 12: substance abuse+mental health | 139,942 (9.0) | 56,396 (14.5) |
| ACCs 16, 17: heart+cerebro-vascular | 393,797 (25.4) | 38,184 (9.8) |
| ACCs 16, 18: heart+vascular | 624,075 (40.2) | 66,174 (17.0) |
| ACCs 17, 18: cerebro-vascular+vascular | 255,606 (16.5) | 16,190 (4.2) |
| ACCs 20, 22: urinary+eyes | 550,189 (35.4) | 56,611 (14.5) |
All differences in proportion of population with the variable were significant at p<.001.
Distance to the nearest VA Medical Center minus the distance to the nearest non-VA Medicare-participating hospital; greater positive values suggest the patient lives closer to a non-VA Medicare hospital.
ACC, aggregated condition category; VA, Veterans Affairs.
In Table 3 are the results of the fractional logistic regression analysis for overall VA reliance as represented by the marginal effects of the independent variables. These results suggest that most individual ACCs had a negative association with the proportion of total health care costs attributed to VA care. In the under-65 model, only the mental health, eyes, and the ears/nose/throat ACCs had positive effect on VA reliance, while the substance abuse and the skin ACCs were nonsignificant, indicating that these were some of the few situations where clinical condition groups were more strongly associated with VA reliance than with the other factors we assessed. In the older cohort, the Diabetes ACC was positive, as were infectious/parasitic, MH/SA ACCs. The relative marginal effects suggest that other covariates, such as priority group and distance, have stronger influence than the ACCs in predicting the level of VA reliance in this age group.
Table 3.
Fractional Logistic Regression of Overall VA Reliance as a Function of ACCs, Adjusted for Age, Sex, Race, VA Priority Group, and Differential Distance between Nearest VAMC and Nearest Medicare Hospital
| Under 65 |
Age 65+ |
|||
|---|---|---|---|---|
| Variable | Marginal Effect | Robust SE | Marginal Effect | Robust SE |
| Male (reference group) | — | — | — | — |
| Female | 0.006 | 0.0020 | 0.023 | 0.0021 |
| Non-black (reference group) | — | — | — | |
| Black | −0.016 | 0.0012 | 0.121 | 0.0012 |
| Priority 7, 8 (reference group) | — | — | — | — |
| Priority 5 (low income) | 0.077 | 0.0014 | 0.211 | 0.0006 |
| Priority 1, 4 (high disability) | 0.142 | 0.0016 | 0.269 | 0.0007 |
| Priority 2, 3, 6 (low/moderate disability) | 0.076 | 0.0013 | 0.157 | 0.0008 |
| Differential distance: <5 miles (reference) | — | — | — | — |
| Differential distance: 5–19 miles | −0.045 | 0.0016 | −0.079 | 0.0010 |
| Differential distance: 20–39 miles | −0.083 | 0.0019 | −0.121 | 0.0010 |
| Differential distance: 40–59 miles | −0.109 | 0.0020 | −0.149 | 0.0010 |
| Differential distance: 60+ miles | −0.124 | 0.0018 | −0.174 | 0.0009 |
| Age≥75 | — | — | −0.066 | 0.0006 |
| ACC01: infectious and parasitic | −0.004 | 0.001 | 0.003 | 0.0006 |
| ACC02: malignant neoplasm | −0.016 | 0.0012 | −0.092 | 0.0006 |
| ACC03: benign/in situ neoplasm | −0.025 | 0.0015 | −0.081 | 0.0008 |
| ACC04: diabetes | −0.004 | 0.001 | 0.011 | 0.0006 |
| ACC05: nutritional and metabolic | −0.025 | 0.0011 | −0.086 | 0.0008 |
| ACC06: liver | −0.040 | 0.0013 | −0.096 | 0.0011 |
| ACC07: gastrointestinal | −0.029 | 0.0009 | −0.048 | 0.0006 |
| ACC08: musculoskeletal and connective | −0.027 | 0.0011 | −0.069 | 0.0007 |
| ACC09: hematological | −0.061 | 0.0013 | −0.078 | 0.0006 |
| ACC10: cognitive disorders | −0.024 | 0.0015 | −0.045 | 0.0009 |
| ACC11: substance abuse | 0.001* | 0.0009 | 0.042 | 0.0009 |
| ACC12: mental | 0.020 | 0.0010 | 0.039 | 0.0006 |
| ACC14: neurological | −0.021 | 0.0010 | −0.024 | 0.0007 |
| ACC15: cardio-respiratory arrest | −0.106 | 0.0023 | −0.154 | 0.0012 |
| ACC16: heart | −0.036 | 0.0011 | −0.061 | 0.0010 |
| ACC17: cerebro-vascular | −0.046 | 0.0014 | −0.079 | 0.0007 |
| ACC18: vascular | −0.046 | 0.0012 | −0.072 | 0.0006 |
| ACC19: lung | −0.069 | 0.0010 | −0.083 | 0.0006 |
| ACC20: eyes | 0.032 | 0.0010 | −0.041 | 0.0007 |
| ACC21: ears, nose, and throat | 0.009 | 0.0010 | −0.018 | 0.0006 |
| ACC22: urinary system | −0.048 | 0.0011 | −0.068 | 0.0006 |
| ACC23: genital system | −0.017 | 0.001 | −0.062 | 0.0006 |
| ACC25: skin and subcutaneous | −0.001* | 0.0009 | −0.024 | 0.0006 |
| ACC26: injury, poisoning, complications | −0.080 | 0.0010 | −0.091 | 0.0006 |
| ACC29: transplants, openings, amputations | −0.007 | 0.0022 | −0.011 | 0.0018 |
| Selected ACC comorbidity pairs† | ||||
| ACCs 4, 6: diabetes+liver | −0.010 | 0.0024 | 0.000* | 0.0023 |
| ACCs 4, 15: diabetes+cardio-respiratory arrest | 0.017 | 0.0029 | 0.003* | 0.0024 |
| ACCs 4, 16: diabetes+heart | −0.012 | 0.0032 | −0.013 | 0.0029 |
| ACCs 4, 17: diabetes+cerebro-vascular | −0.005* | 0.0023 | −0.010 | 0.0013 |
| ACCs 4, 20: diabetes+eyes | 0.026 | 0.0018 | 0.085 | 0.0015 |
| ACCs 4, 22: diabetes+urinary | 0.002* | 0.0019 | 0.002* | 0.0012 |
| ACCs 4, 29: diabetes+transplants, openings, amputations | 0.016 | 0.0039 | 0.016 | 0.0035 |
| ACCs 11, 12: substance abuse+mental health | −0.011 | 0.0020 | −0.013 | 0.0018 |
| ACCs 16, 17: heart+cerebro-vascular | −0.007* | 0.0040 | −0.020 | 0.0036 |
| ACCs 16, 18: heart+vascular | −0.015 | 0.0033 | −0.039 | 0.0027 |
| ACCs 17, 18: cerebro-vascular+vascular | −0.005* | 0.0024 | 0.003* | 0.0013 |
| ACCs 20, 22: urinary+eyes | 0.008 | 0.0018 | 0.047 | 0.0013 |
Note: Presented are marginal effects.
Not significant at p<.01
These pairs were tested for interaction effects, in sequential models, with the single ACCs and the demographic and access covariates. Rather than show the results of each model, we present the marginal effect of the pairs in this table.
ACC, aggregated condition category; SE, standard error; VA, Veterans Affairs; VAMC, VA Medical Center.
The results of the outpatient VA reliance analysis (Table 4) were consistent with our findings for correlates of overall VA reliance in veterans older than 65 (outpatient VA reliance was not analyzed separately by age group, though veterans older than 65 composed the majority of the cohort). The data presented in Table 4 (left column) represent the marginal effects for each variable. Again, MH/SA disorders were associated with greater reliance on the VA for outpatient care. To a lesser extent, infectious and parasitic diseases (e.g., HIV/AIDS) and diabetes were also associated with increased reliance on VA outpatient care.
Table 4.
Regression Results of Inpatient and Outpatient Use as a Function of ACCs, Adjusted for Sex, Race, VA Priority Group, Differential Distance between Nearest VAMC and Nearest Medicare Hospital, and Age
| Outpatient Analysis: Fractional Logistic Regression: Marginal Effects |
Inpatient Analysis (N=731,227) Odds Ratios from Multinomial Logistic Regression (Referent Outcome Is Stays in Medicare Only) |
|||
|---|---|---|---|---|
| Outpatient Reliance N=1,942,290 |
||||
| Variable | Marginal Effect | Robust SE | VA Inpatient Stay Only N=191,093 | VA+Medicare Stays N=81,581 |
| Male (reference) | — | — | — | — |
| Female | 0.011 | 0.0015 | 1.215 | 1.231 |
| Non-black (reference) | — | — | — | — |
| Black | 0.078 | 0.0009 | 1.523 | 1.799 |
| Priority 7–8: (reference) | — | — | — | — |
| Priority 5: low income | 0.182 | 0.0005 | 5.572 | 4.503 |
| Priority 1, 4: high disability | 0.222 | 0.0005 | 9.48 | 7.521 |
| Priority 2, 3, 6: low/moderate disability | 0.133 | 0.0006 | 4.224 | 3.643 |
| Distance: <5 miles (reference) | — | — | — | — |
| Distance: 5–19 miles | −0.067 | 0.0008 | 0.531 | 0.648 |
| Distance: 20–39 miles | −0.105 | 0.0008 | 0.342 | 0.495 |
| Distance: 40–59 miles | −0.130 | 0.0009 | 0.257 | 0.435 |
| Distance: 60+ miles | −0.152 | 0.0008 | 0.194 | 0.375 |
| Age: <65 years | 0.085 | 0.0008 | 1.471 | 1.51 |
| Age: 65–74 (reference) | — | — | — | — |
| Age: 75+ years | −0.061 | 0.0005 | 0.676 | 0.779 |
| ACC01: infectious and parasitic | 0.002 | 0.0005 | 1.046 | 1.249 |
| ACC02: malignant neoplasm | −0.092 | 0.0005 | 0.911 | 0.788 |
| ACC03: benign/in situ neoplasm | −0.080 | 0.0007 | 0.75 | 0.691 |
| ACC04: diabetes | 0.014 | 0.0005 | 0.967 | 1.052 |
| ACC05: nutritional and metabolic | −0.062 | 0.0006 | 0.598 | 0.889 |
| ACC06: liver | −0.065 | 0.0009 | 0.653 | 0.998* |
| ACC07: gastrointestinal | −0.033 | 0.0005 | 0.865 | 1.151 |
| ACC08: musculoskeletal and connective | −0.059 | 0.0006 | 0.675 | 0.807 |
| ACC09: hematological | −0.057 | 0.0005 | 0.739 | 1.165 |
| ACC10: cognitive disorders | −0.022 | 0.0007 | 0.77 | 1.464 |
| ACC11: substance abuse | 0.044 | 0.0006 | 1.222 | 1.818 |
| ACC12: mental | 0.039 | 0.0005 | 1.158 | 1.578 |
| ACC14: neurological | −0.025 | 0.0005 | 0.896 | 1.077 |
| ACC15: cardio-respiratory arrest | −0.076 | 0.0010 | 0.436 | 1.135 |
| ACC16: heart | −0.040 | 0.0008 | 0.666 | 0.922 |
| ACC17: cerebro-vascular | −0.052 | 0.0006 | 0.658 | 0.969 |
| ACC18: vascular | −0.051 | 0.0005 | 0.762 | 1.071 |
| ACC19: lung | −0.058 | 0.0005 | 0.606 | 1.108 |
| ACC20: eyes | −0.035 | 0.0005 | 1.056 | 0.889 |
| ACC21: ears, nose, and throat | −0.018 | 0.0005 | 0.904 | 0.869 |
| ACC22: urinary system | −0.055 | 0.0005 | 0.882 | 1.24 |
| ACC23: genital system | −0.056 | 0.0005 | 0.744 | 0.767 |
| ACC25: skin and subcutaneous | −0.032 | 0.0005 | 1.009* | 1.021 |
| ACC26: injury, poisoning, complications | −0.076 | 0.0005 | 0.774 | 1.242 |
| ACC29: transplant/opening/amputation | −0.013 | 0.0013 | 1.211 | 1.3 |
| Selected ACC comorbidity pairs† | ||||
| ACCs 4, 6: diabetes+liver | 0.941 | 0.901 | ||
| ACCs 4, 15: diabetes+cardio-respiratory arrest | 0.901 | 0.953 | ||
| ACCs 4, 16: diabetes+heart | 0.824 | 1.005* | ||
| ACCs 4, 17: diabetes+cerebro-vascular | 0.911 | 0.996* | ||
| ACCs 4, 20: diabetes+eyes | 1.340 | 1.227 | ||
| ACCs 4, 22: diabetes+urinary | 0.945 | 1.054 | ||
| ACCs 4, 29: diabetes+transplants, openings, amputations | 1.070 | 1.031* | ||
| ACCs 11, 12: substance abuse+mental health | 0.864 | 1.066 | ||
| ACCs 16, 17: heart+cerebro-vascular | 0.692 | 0.918* | ||
| ACCs 16, 18: heart+vascular | 0.668 | 0.943* | ||
| ACCs 17, 18: cerebro-vascular+vascular | 0.819 | 0.895 | ||
| ACCs 20, 22: urinary+eyes | 0.840 | 0.986* | ||
Not significant at p<.01.
These pairs were tested for interaction effects, in sequential models with the single ACCs and the demographic and access covariates. Rather than show the results of each model, we present the marginal effect of the pairs in this table.
ACC, aggregated condition category; SE, standard error; VA, Veterans Affairs; VAMC, VA Medical Center.
Our analysis of inpatient care examined whether patient characteristics were associated with the likelihood of receiving inpatient care within the VA system only, under Medicare only, or in both settings. Twenty-six percent of the cohort had an inpatient stay during the study period. Roughly two-thirds of the veterans (63 percent) with any inpatient stays received their inpatient care solely through Medicare, 26 percent received inpatient care solely in the VA, and 11 percent had inpatient care in both the VA and Medicare. Patients with the ACC for transplants or amputations were more likely to have inpatient care in the VA only (odds ratio=1.21, 95 percent CI: 1.18–1.24; reference group Medicare only). A separate analysis of HCC occurring in Medicare and the VA suggests that this result is driven by amputations (results not shown). The likelihood of having an inpatient stay only in the VA was also >1 and statistically significant for patients with ACCs for infectious and parasitic disorders (OR=1.05, 95 percent CI: 1.03–1.10.); substance abuse (OR=1.22, 95 percent CI: 1.20–1.24); mental health disorders (OR=1.16, 95 percent CI: 1.14–1.17); and eye disorders (OR=1.06, 95 percent CI: 1.04–1.07). The other ACCs (a higher number of condition groups) were more likely to be associated with patients who had stays in Medicare only, and particularly those who had stays in both the VA and Medicare. We examined the 12 comorbidity pairs for interactions in the inpatient analysis as well. The diabetes+eyes pair was more likely to receive inpatient care in the VA only (OR=1.34, 95 percent CI: 1.30–1.38), as was the diabetes+transplants/openings/amputations pair (OR=1.07, 95 percent CI: 1.01–1.13), compared with the Medicare-only inpatients.
DISCUSSION
We investigated the relationship between patient clinical characteristics and use of VA health care services among Medicare-enrolled veterans, controlling for other factors that might affect choices about where to obtain care. Unlike much of the prior work in this topic, we focused upon the full spectrum of clinical conditions rather than specific diseases or procedures, and we assessed all Medicare eligible veterans regardless of age. We also used a novel statistical method, fractional logistic regression, to answer our scientific questions. Our goal was to evaluate whether patients' health conditions explained variation in the extent of health care reliance on the VA versus Medicare-financed services, beyond that which could be explained by other factors such as age, gender, race, distance to the nearest VAMC, and VA-determined priority for health care services.
Our results confirm and extend those of other investigators who have assessed utilization of VA services by dually enrolled veterans (Borowsky and Cowper 1999; Rosen et al. 2005; Hynes et al. 2007;). Examining more recent data on VA/Medicare dual enrollees, we confirm the findings of Hynes and colleagues that VA priority group and distance to VA care are influential factors in reliance on the VA. We further examined the full spectrum of medical conditions that may play a role in reliance. Like Rosen and colleagues, we examined ACCs across both systems as indicators of health conditions; we took an added step of incorporating the ACCs in a modeling approach, and using a novel technique that has not been widely applied to health services research questions. Another relatively unique contribution is that we studied patients under 65, and we showed that they have different patterns of care and health care needs than elderly dually enrolled veterans.
In this cohort of dual VA-Medicare enrollees, we found that outpatient VA reliance was greater for women, for black patients, and for those in VA priority categories indicative of severe service-connected disability or low income. As differential distance to a VA facility, relative to the nearest Medicare hospital, increased, outpatient reliance on the VA decreased monotonically. Those veterans with substance abuse and mental health disorders had greater reliance on VA outpatient care, and also on inpatient care in the VA (both the VA-only and VA+ Medicare inpatient care). These results are consistent with the observation that the VA provides a large quantity of MHSA care. We further found that diseases of the eyes, ears, nose, and throat were significantly associated with greater VA reliance in the under-65 group but with lower VA reliance in those patients 65 and above. The diabetes and infectious and parasitic disease ACCs were correlates of increased VA reliance only in the older group.
Indeed, the population of veterans who are dually enrolled in Medicare and the VA is composed of two very disparate groups: those veterans under the age of 65 who are Medicare eligible due to disability (disability-eligible), and those 65 years or older who are Medicare eligible through age (age-eligible). The former population is, by definition, more disabled and therefore may also use more—and different kinds—of health care than those veterans who are age-eligible. In our separate analyses of overall reliance for these two populations, we find differences in the magnitude of the effect of factors that affect choice of health care setting. For both populations, priority categories of disability and low income are predictors of increased reliance on the VA. We note that, while the marginal effect of disability priority categories is smaller in the under-65 veterans, this finding may be due to the fact that the under-65 population is already disabled. In both groups, ACCs associated with acute, critical care, such as cardio-respiratory arrest, are predictors of notably lower VA reliance (hence, higher Medicare reliance); these are conditions where the patients likely have less or virtually no choice in health care setting and may be taken to the nearest hospital by emergency transport. The nearest hospital in such a situation is not likely to be a VA hospital.
In terms of clinical characteristics, Medicare-age-eligible veterans show a substantially larger marginal effect of increased VA reliance from diagnoses of substance abuse or mental health conditions than do their under-65 counterparts. This finding may reflect the fact that typical under-65 veterans are already more likely to have substance abuse or mental health conditions.
The younger veterans under the age of 65 who fall into the ACC for eye problems have greater reliance on the VA, whereas their age 65 and older counterparts have less reliance on the VA. As the VA provides specialized care in blind rehabilitation, younger blind veterans may be relying heavily on the VA for this service. The co-occurrence of some pairs of chronic condition ACCs does not have as great of an influence on VA reliance as more acute conditions. Our findings suggest that while some illness conditions (e.g., substance abuse and mental health problems, cardio-respiratory arrest) have a significant influence on where a veteran obtains the bulk of health care, other factors more fundamental to VA eligibility or access (such as VA priority group or distance to VA care) may be the strongest drivers of VA reliance.
The higher prevalence of ACCs observed in dual users versus VA-only users illustrates findings from other research (Rosen et al. 2005; Byrne et al. 2006;) that dual users have more diagnoses recorded than those who use the VA exclusively, and that more diagnoses overall are recorded in Medicare settings. This may reflect, to varying degrees, a disparity in coding incentive behavior between Medicare and the VA, but also perhaps less complicated disease patterns in VA-only users. Our prior work (Byrne et al. 2006) suggested that the higher proportion of diagnoses in Medicare could be partially attributed to veterans who use the VA primarily for pharmacy services.
This study has several limitations. First, we could not measure the cost of outpatient prescription drugs under the Medicare program. Although until recently FFS Medicare did not pay for pharmaceuticals, these costs are nevertheless associated with patient out-of-pocket costs in that setting and therefore ideally should be included in our reliance measure. Because different clinical conditions are likely to entail different pharmaceutical costs, the Medicare costs may be underestimated by the lack of prescription information. Second, we were not able to assess non-FFS Medicare users, and these individuals may exhibit different patterns of use than those individuals who are enrolled in FFS Medicare. Third, ideally our cost data would have included copayments to the VA paid by veterans in Priority 7 and 8, as a complement to the Medicare copayment data. However, patient-level copayment data are not available in VA administrative data sources. Because we cannot include the copayments in VA costs, we might be underestimating the effect of Priority 7 or 8 status on reliance. Because VA copayments generally constitute a smaller proportion of total costs than do Medicare copayments, however, we do not believe the study's overall conclusions are affected by this fact. Fourth, although we have diagnoses from both VA and Medicare databases, our analysis cannot specify where the care for different conditions was provided. In previous work (Byrne et al. 2006), we documented little overlap in recorded diagnoses across the two databases, and therefore can speculate that the diagnoses being recorded in each do reflect the care that is provided. However, future research is needed to confirm this assertion. Fifth, because the VA and Medicare are in a somewhat unique complementary situation, our results may not be generalizable to other health care systems. However, the methods could be applied to other arenas in which patients have a choice between two systems of care. Sixth, although we have data on use of health care for our population under both the Medicare and VA systems, it is possible that veterans in our cohort are accessing health care under other systems as well. Veterans with private insurance or Medicaid may be receiving non-VA/non-Medicare health services. Thus, although we can assess the VA-Medicare balance of care, Veterans may be receiving additional care that is not captured in our data. Lastly, the choice of health care setting by individuals who have access to more than one system may also be a factor of specific characteristics of the health care systems, including but not limited to special programs or facilities (e.g., transplantation facilities, rehabilitation programs), the reputation of the health care system, and patients' subjective perception of the systems (Figure 1). Also, the VA and non-VA care differ in the mix of services offered, such as differing levels of long-term care and rehabilitation, which makes utilization comparisons a challenge; hence, the cost comparisons presented here may be a somewhat simplistic reflection of “reliance.” Little research has examined these potential factors directly, and in this study as well we are limited by data in our ability to address these factors. Nevertheless, our study is a comprehensive examination of many of the factors affecting choice of health care setting.
In summary, accessibility and priority level for VA health care services have a clear relationship with VA reliance. Medicare-enrolled veterans with mental illness, substance abuse, or amputations have greater reliance on VA care. Veterans who are Medicare eligible due to disability show differences from their age-eligible counterparts in factors that affect reliance. Finally, the results found here have implications for policy, across both the VA and Medicare. Based on previous research, veterans who are dual users of VA and Medicare are likely to be using complementary services from the two systems (Shen et al. 2003; Rosen et al. 2005; Byrne et al. 2006;). In some cases, for example, mental health and spinal cord rehabilitation, the VA may offer enhanced coverage. Hence, veterans may be making rational choices that result in a comprehensive “benefits package” between Medicare and VA health care service options. This research also confirms that veterans who use Medicare as well as the VA are recording higher levels of services (Hynes et al. 2007; Keyhani et al. 2007;), suggesting that these dual users have a higher illness burden than those veterans who use only one system. Moreover, continuity of care for dually enrolled veterans is a particular concern, notably in conditions (e.g., diabetes) where care is sought in both settings. It is important that clinicians are aware of all comorbid conditions of patients, so that appropriate risks and benefits of treatment may be considered. Indeed, it is critically important that the health care for these veterans be coordinated between the two systems so that high-quality care is delivered, and that unneeded duplication of services is avoided.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The authors are grateful to Degang Wang, Ph.D., for statistical analysis; LeChauncy Woodard, M.D., M.P.H., for clinical input into the design and analysis; and Supicha Sookanan Chitwood, M.P.H., for logistical and administrative support. This research was conducted with support from a VA contract (Project XVA 33-102) at the request of Veterans Integrated Service Networks 12 and 23. This work was supported in part by the Houston VA HSR&D Center of Excellence (HFP 90-020). Dr. Petersen was a Robert Wood Johnson Foundation Generalist Physician Scholar (grant no. 045444) at the time that this work was conducted, and an American Heart Association Established Investigator Awardee (grant no. 0540043N). Dr. Byrne holds a National Cancer Institute career development award (K07 CA101812).
Disclosures: None.
Disclaimers: None.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- Borowsky SJ, Cowper DC. Dual Use of VA and Non-VA Primary Care. Journal of General Internal Medicine. 1999;14(5):274–80. doi: 10.1046/j.1525-1497.1999.00335.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brahmajee KN, Lux X, Vaughan-Sarrazin MS, Cram P. Coronary Revascularization at Specialty Cardiac Hospitals and Peer General Hospitals in Black Medicare Beneficiaries. Circulation Cardiovascular Quality and Outcomes. 2008;1(2):116–22. doi: 10.1161/CIRCOUTCOMES.108.800086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgess JF, Jr., DeFiore DA. The Effect of Distance to VA Facilities on the Choice and Level of Utilization of VA Outpatient Services. Social Science and Medicine. 1994;39(1):95–104. doi: 10.1016/0277-9536(94)90169-4. [DOI] [PubMed] [Google Scholar]
- Byrne MM, Kuebeler M, Pietz K, Petersen LA. Effect of Using Information from Only One System for Dually Eligible Health Care Users. Medical Care. 2006;44(8):768–73. doi: 10.1097/01.mlr.0000218786.44722.14. [DOI] [PubMed] [Google Scholar]
- Carey K, Montez-Rath ME, Rosen AK, Christiansen CL, Loveland S, Ettner SL. Use of VA and Medicare Services by Dually Eligible Veterans with Psychiatric Problems. Health Services Research. 2008;43(4):1164–83. doi: 10.1111/j.1475-6773.2008.00840.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis RP, Pope GC, Iezzoni L, Ayanian JZ, Bates DW, Burstin H, Ash AS. Diagnosis-Based Risk Adjustment for Medicare Capitation Payments. Health Care Financing Review. 1996;17(3):101–28. [PMC free article] [PubMed] [Google Scholar]
- Fairris D, Pedace R. The Impact of Minimum Wages on Job Training: An Empirical Exploration with Establishment Data. Southern Economic Journal. 2004;70(3):566–83. [Google Scholar]
- Hendershott PH, Pryce G. The Sensitivity of Homeowner Leverage to the Deductibility of Home Mortgage Interest. Journal of Urban Economics. 2006;60(1):50–68. [Google Scholar]
- Hynes DM, Koelling K, Stroupe K, Arnold N, Mallin K, Sohn MW, Weaver FM, Manheim L, Kok L. Veterans' Access to and Use of Medicare and Veterans Affairs Health Care. Medical Care. 2007;45(3):214–23. doi: 10.1097/01.mlr.0000244657.90074.b7. [DOI] [PubMed] [Google Scholar]
- Keyhani S, Ross JS, Hebert P, Dellenbaugh C, Penrod JD, Siu AL. Use of Preventive Care by Elderly Male Veterans Receiving Care through the Veterans Health Administration, Medicare Fee-for-Service, and Medicare HMO Plans. American Journal of Public Health. 2007;97(12):2179–85. doi: 10.2105/AJPH.2007.114934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kieschnick R, McCullough BD. Regression Analysis of Variates Observed on (0,1): Percentages, Proportions and Fractions. Statistical Modelling. 2003;3(3):193–213. [Google Scholar]
- Maciejewski ML, Perkins M, Li Y, Chapko M, Fortney JC, Liu C. Utilization and Expenditures of Veterans Obtaining Primary Care in Community Clinics and VA Medical Centers: An Observational Cohort Study. BMC Health Services Research. 2007;7:56. doi: 10.1186/1472-6963-7-56. Available at http://www.biomedcentral.com/1472-6963/7/56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann SV, Powers EA. Determinants of Bond Tender Premiums and the Percentage Tendered. Journal of Banking and Finance. 2007;31(3):547–66. [Google Scholar]
- McCarthy JF, Blow JF, Valenstein M, Fischer EP, Owen RR, Barry KL, Hudson TJ, Ignacio RV. Veterans Affairs Health System and Mental Health Treatment Retention among Patients with Serious Mental Illness: Evaluating Accessibility and Availability Barriers. Health Services Research. 2007;42(3, part 1):1042–60. doi: 10.1111/j.1475-6773.2006.00642.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mooney C, Zwanzinger J, Phibbs CS, Schmitt S. Is Travel Distance a Barrier to Veterans' Use of VA Hospitals for Medical Surgical Care? Social Science and Medicine. 2000;50(12):1743–55. doi: 10.1016/s0277-9536(99)00414-1. [DOI] [PubMed] [Google Scholar]
- Papke LE, Wooldridge JM. Econometric Methods for Fractional Response Variables with an Application to 401 (K) Plan Participation Rates. Journal of Applied Econometrics. 1996;11(6):619–32. [Google Scholar]
- Petersen LA, Pietz K, Woodard LD, Byrne M. Comparison of the Predictive Validity of Diagnosis-Based Risk Adjusters for Clinical Outcomes. Medical Care. 2005;43(1):61–7. [PubMed] [Google Scholar]
- Phibbs CS, Bhandari A, Yu W, Barnett PG. Estimating the Costs of VA Ambulatory Care. Medical Care Research and Review. 2003;60(3, suppl):54S–73S. doi: 10.1177/1077558703256725. [DOI] [PubMed] [Google Scholar]
- Rosen AK, Gardner J, Montez M, Loveland S, Hendricks A. Dual-System Use: Are There Implications for Risk Adjustment and Quality Assessment? American Journal of Medical Quality. 2005;20(4):182–94. doi: 10.1177/1062860605275791. [DOI] [PubMed] [Google Scholar]
- Shen Y, Findley PA, Maney M, Pogach L, Crystal S, Rajan M, Findley TW. Department of Veterans Affairs-Medicare Dual Beneficiaries with Stroke: Where Do They Get Care? Journal of Rehabilitation Research and Development. 2008;45(1):43–51. doi: 10.1682/jrrd.2006.07.0081. [DOI] [PubMed] [Google Scholar]
- Shen Y, Hendricks A, Zhang S, Kazis LE. VHA Enrollees' Health Care Coverage and Use of Care. Medical Care Research and Review. 2003;60(2):253–67. doi: 10.1177/1077558703060002007. [DOI] [PubMed] [Google Scholar]
- StataCrop. Stata Statistical Software: Release 10. College Station, TX: StataCrop LP; 2007. [Google Scholar]
- VA Health Economics Resource Center (HERC). Patient Incurred Cost—How Do I Estimate Travel Costs? 2009. [accessed on June 18, 2009]. Available at http://www.herc.research.va.gov/resources/faq_h02.asp.
- VA Information Resource Center (VIREC) 2003. “Research Findings from the VA Medicare Data Merge Initiative: Veterans Enrollment, Access and Use of Medicare and VA Health Services.” (XVA 69-001). [accessed on September 30, 2009] Report to the under Secretary for Health, Department of Veterans Affairs. Available at http://www1.va.gov/VHAPUBLICATIONS/VIEWPUBLICATION.asp?pub_ID=1611.
- Veterans Health Administration. VHA Enrollment Determinations. VHA Handbook 1601A.03. Washington, DC: VHA; 2007. [Google Scholar]
- Wagner TH, Chen S, Barnett PG. Using Average Cost Methods to Estimate Encounter-Level Costs for Medical-Surgical Stays in the VA. Medical Care Research and Review. 2003;60(3, suppl):15S–36S. doi: 10.1177/1077558703256485. [DOI] [PubMed] [Google Scholar]
- Weeks WB, Bott DM, Bazos DA, Campbell SL, Lombardo R, Racz MJ, Hannan EL, Wright SM, Fisher ES. Veterans Health Administration Patients' Use of the Private Sector for Coronary Revascularization in New York: Opportunities to Improve Outcomes by Directing Care to High-Performance Hospitals. Medical Care. 2006;44(6):519–26. doi: 10.1097/01.mlr.0000215888.20004.5e. [DOI] [PubMed] [Google Scholar]
- Weeks WB, West AN. Where Do Veterans Health Administration Patients Obtain Heart, Liver and Kidney Transplants? Military Medicine. 2007;172(11):1154–9. doi: 10.7205/milmed.172.11.1154. [DOI] [PubMed] [Google Scholar]
- Wright SM, Daley J, Fisher ES, Thibault GE. Where Do Elderly Veterans Obtain Care for Acute Myocardial Infarction: Department of Veterans Affairs or Medicare? Health Services Research. 1997;31(6):739–54. [PMC free article] [PubMed] [Google Scholar]
- Wright SM, Petersen LA, Lamkin RP, Daley J. Increasing Use of Medicare Services by Veterans with Acute Myocardial Infarction. Medical Care. 1999;37(6):529–37. doi: 10.1097/00005650-199906000-00002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.